The Effect of a Secondary Task on Kinematics during Turning in Parkinson’s Disease with Mild to Moderate Impairment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
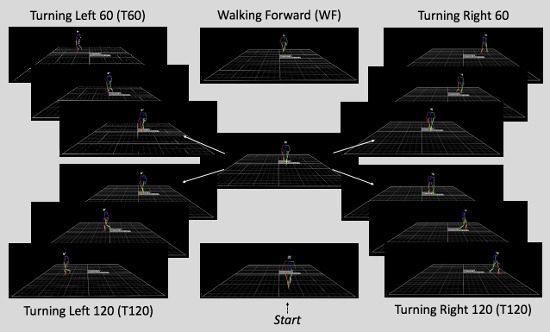
2.2. Experimental Procedures
2.3. Data Reduction
2.4. Data Analysis
3. Results
3.1. Cognitive Task
3.2. Spatiotemporal Parameters
4. Discussion
4.1. Effects on Gait Variables: A Task Comparison
4.2. Effects on Gait Variables: A Direction Comparison
4.3. Effects on Gait Variables: Cognitive Task and Mechanical Task
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- De Lau, L.M.; Breteler, M.M. Epidemiology of Parkinson’s disease. Lancet Neurol. 2016, 5, 525–535. [Google Scholar] [CrossRef]
- Kelly, V.E.; Eusterbrock, A.J.; Shumway-Cook, A. A review of dual-task walking deficits in people with Parkinson’s disease: Motor and cognitive contributions, mechanisms, and clinical implications. Parkinsonism Disord. 2012, 2012, 918719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cummings, J.L. Intellectual impairment in Parkinson’s disease: Clinical, pathological, and biochemical correlates. J. Ger. Psychiatry Neurol. 1988, 1, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Creaby, M.W.; Cole, M.H. Gait characteristics and falls in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Related Disord. 2018, 57, 1–8. [Google Scholar] [CrossRef]
- Kelly, V.E.; Eusterbrock, A.J.; Shumway-Cook, A. The effects of instructions on dual-task walking and cognitive task performance in people with Parkinson’s disease. Parkinsonism Dis. 2012. [Google Scholar] [CrossRef]
- Nocera, J.R.; Roemmich, R.; Elrod, J.; Atlmann, L.J.P.; Hass, C.J. Effects of cognitive task on gait initiation in Parkinson disease: Evidence of motor prioritization? J. Rehabil. Res. Develop. 2013, 50, 699–708. [Google Scholar] [CrossRef]
- Rochester, L.; Galna, B.; Lord, S.; Burn, D. The nature of dual-task interference during gait in incident Parkinson’s disease. Neuroscience 2014, 265, 83–94. [Google Scholar] [CrossRef]
- Morris, M.E.; Iansek, R.; Matyas, T.A.; Summers, J.J. Stride length regulation in Parkinson’s disease: Normalization strategies and underlying mechanisms. Brain 1996, 119, 551–568. [Google Scholar] [CrossRef]
- Morris, M.E.; Huxham, F.; McGinley, J.; Dodd, K.; Iansek, R. The biomechanics and motor control of gait in Parkinson disease. Clin. Biomech. 2001, 16, 459–470. [Google Scholar] [CrossRef]
- Canning, C.G. The effect of directing attention during walking under dual task conditions in Parkinson’s disease. Parkinsonism Relat. Disord. 2005, 11, 95–99. [Google Scholar] [CrossRef]
- Plotnik, M.; Dagan, Y.; Gurevich, T.; Giladi, N.; Hausdorff, J.M. Effects of cognitive function on gait and dual tasking abilities in patients with Parkinson’s disease suffering from motor response fluctuations. Exp. Brain Res. 2011, 208, 169–179. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, S.; Morris, M.E.; Iansek, R. Dual task interference during gait in people with Parkinson disease: Effects of motor versus cognitive secondary tasks. Phys. Ther. 2002, 82, 888–897. [Google Scholar] [CrossRef] [PubMed]
- Rochester, L.; Hetherington, V.; Jones, D.; Nieuwboer, A.; Willems, A.; Kwakkel, G.; van Wegen, E. Attending to the task: Interference effects of functional tasks on walking in Parkinson’s disease and the roles of cognition, depression, fatigue and balance. Arch. Phys. Med. Rehab. 2004, 85, 1578–1585. [Google Scholar] [CrossRef] [PubMed]
- Brauer, S.G.; Morris, M.E. Can people with Parkinson’s disease improve dual tasking when walking? Gait Posture 2010, 31, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.A.; de Bruin, N.; Doan, J.B.; Suchowersky, O.; Hu, B. Novel challenges to gait in Parkinson’s disease: The effect of concurrent music in single and dual task contexts. Arch. Phys. Med. Rehab. 2009, 90, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Salazar, R.D.; Ren, X.; Ellis, T.; Toraif, N.; Barthelemy, O.J.; Neargarder, S.; Cronin-Golomb, A. Dual tasking in Parkinson’s disease: Cognitive consequences while walking. Neuropsychology 2016, 31, 613–623. [Google Scholar] [CrossRef]
- Campbell, C.M.; Rowse, J.L.; Ciol, M.A.; Shumway-Cook, A. The effect of cognitive demand on timed up and Go performance in older adults with and without Parkinson disease. Neurol. Rep. 2003, 27, 2–7. [Google Scholar] [CrossRef]
- Camicioli, R.; Oken, B.S.; Sexton, G.; Kaye, J.A.; Nutt, J.G. Verbal fluency task affects gait in Parkinson’s disease with motor freezing. J. Geriatr. Psych. Neurol. 1998, 11, 181–185. [Google Scholar] [CrossRef]
- Galletly, R.; Brauer, S.G. Does the type of concurrent task affect preferred and cued gait in people with Parkinson’s disease. Austr. J. Physiother. 2005, 51, 175–180. [Google Scholar] [CrossRef] [Green Version]
- Lapointe, L.L.; Stierwalt, J.A.G.; Maitland, C.G. Talking with walking: Cognitive loading and injurious falls in Parkinson’s disease. Intern. J. Speech-Lang. Pathol. 2010, 12, 445–459. [Google Scholar] [CrossRef]
- Stegemoller, E.L.; Wilson, J.P.; Hazamy, A.; Shelly, M.C.; Okun, M.S.; Altmann, L.P.; Hass, C.J. Associations between cognitive and gait performance during single- and dual-task walking in people with Parkinson disease. Phys. Ther. 2014, 94, 757–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yogev, G.; Giladi, N.; Peretz, C.; Springer, S.; Simon, E.S.; Hausdorff, J.M. Dual tasking, gait rhythmicity, and Parkinson’s disease: Which aspects of gait are attention demanding? Eur. J. Neurosci. 2005, 22, 1248–1256. [Google Scholar] [CrossRef] [PubMed]
- Wild, L.B.; de Lima, D.B.; Balardin, J.B.; Rizzi, L.; Giacobbo, B.L.; Oliveira, H.B.; de Lima, A.; Peyre-Tartaruga, L.A.; Rieder, C.R.; Bromberg, E. Characterization of cognitive and motor performance during dual-tasking in healthy older adults and patients with Parkinson’s disease. J. Neurol. 2013, 260, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.; Perlmutter, J.S.; Earhart, G.M. A kinematic and electromyographic analysis of turning in people with Parkinson disease. Neurorehabil. Neural Repair 2009, 23, 166–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stack, E.; Jupp, K.; Ashburn, A. Developing methods to evaluate how people with Parkinson’s disease turn 180°: An activity frequently associated with falls. Disab. Rehabil. 2004, 26, 478–484. [Google Scholar] [CrossRef]
- Stack, E.L.; Ashburn, A.M.; Jupp, K.E. Strategies used by people with Parkinson’s disease who report difficulty turning. Parkinson. Relat. Disord. 2006, 12, 87–92. [Google Scholar] [CrossRef]
- Adamson, M.B.; Gilmore, G.; Stratton, T.W.; Baktash, N.; Jog, M.S. Medication status and dual tasking on turning strategies in Parkinson disease. J. Neurol. Sci. 2019, 396, 206–212. [Google Scholar] [CrossRef]
- Chou, P.; Lee, S. Turning deficits in people with Parkinson’s disease. Tzu Chi Med. J. 2013, 25, 200–202. [Google Scholar] [CrossRef]
- Vaugoyeau, M.; Viallet, F.; Mesure, S.; Massion, J. Coordination of axial rotation and step execution: Deficits in Parkinson’s disease. Gait Posture 2003, 18, 150–157. [Google Scholar] [CrossRef]
- Crenna, P.; Carpinella, I.; Rabuffetti, M.; Calabrese, E.; Mazzoleni, P.; Nemni, R.; Ferrarin, M. The association between impaired turning and normal straight walking in Parkinson’s disease. Gait Posture 2007, 26, 172–178. [Google Scholar] [CrossRef]
- Willems, A.M.; Nieuwboer, A.; Chavret, F.; Desloovere, K.; Dom, R.; Rochester, L.; Kwakkel, G.; van Wegen, E.; Jones, D. Turning in Parkinson’s disease patients and controls: The effect of auditory cues. Mov. Disord. 2007, 22, 1871–1878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mellone, S.; Mancini, M.; King, L.A.; Horak, F.B.; Chiari, L. The quality of turning in Parkinson’s disease: A compensatory strategy to prevent postural instability? J. Neuroeng Rehabil. 2016, 13, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertoli, M.; Della Croce, U.; Cereatti, A.; Mancini, M. Objective measures to investigate turning impairments and freezing of gait in people with Parkinson’s disease. Gait Posture 2019, 74, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Encarna Micó-Amigo, M.; Kingma, I.; Heinzel, S.; Nussbaum, S.; Heger, T.; Lummel, R.C.V.; Dieën, J.H.V. Dual vs. Single Tasking during Circular Walking: What Better Reflects Progression in Parkinson’s Disease? Front. Neurol. 2019. [Google Scholar] [CrossRef]
- Spildooren, J.; Vercruysse, S.; Desloovere, K. Freezing of gait in Parkinson’s disease: The impact of dual-tasking and turning. Mov. Disord. 2010, 25, 2563–2570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayot, M.; Dujardin, K.; Tard, C.; Defebvre, L.; Bonnet, C.T.; Allart, E.; Delval, A. The interaction between cognition and motor control: A theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning. Clin. Neurophys. 2018, 48, 361–375. [Google Scholar] [CrossRef]
- Hackney, M.E.; Earhart, G.M. The effects of a secondary task on forward and backward walking in Parkinson disease. Neurorehabil. Neural Repair 2010, 24, 97–106. [Google Scholar] [CrossRef] [Green Version]
- Patla, A.E.; Prentice, S.D.; Robinson, C.; Neufeld, J. Visual control of locomotion: Strategies for changing direction and for going over obstacles. J. Exp. Psychol. 1991, 17, 603–634. [Google Scholar] [CrossRef]
- Hughes, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef] [Green Version]
- Schenkman, M.L.; Clark, K.; Xie, T.; Kuchibhatla, M.; Shinberg, M.; Ray, L. Spinal movement and performance of a standing reach task in participants with and without Parkinson disease. Phys. Ther. 2001, 81, 1400–1411. [Google Scholar] [CrossRef]
- Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease. The Unified Parkinson’s Disease Rating Scale (UPDRS): Status and recommendations. Mov. Disord. 2003, 18, 738–750. [Google Scholar] [CrossRef] [PubMed]
- Peyre-Tartaruga, L.A.; Monteiro, E.P. A new integrative approach to evaluate pathological gait: Locomotor rehabilitation index. Clin. Transl. Degener. Dis. 2016, 1, 86–90. [Google Scholar] [CrossRef]
- Woollacott, M.; Shumway-Cook, A. Attention and the control of posture and gait: A review of an emerging area of research. Gait Posture 2002, 16, 1–14. [Google Scholar] [CrossRef]
- Plotnik, M.; Giladi, N.; Hausdorff, J.M. Bilateral coordination of gait and Parkinson’s disease: The effects of dual tasking. J. Neurol. Neurosurg. Psych. 2009, 80, 347–350. [Google Scholar] [CrossRef]
- Hausdorff, J.M.; Balash, J.; Giladi, N. Effects of cognitive challenge on gait variability in patients with Parkinson’s disease. J. Geriatr. Psych. Neurol. 2003, 16, 53–58. [Google Scholar] [CrossRef] [PubMed]
- De Melo Roiz, R.; Avezedo Cacho, E.W.; Macedo Pazinatto, M.; Guimaraes Reis, J.; Cliquet, A.; Barasnevicius-Quagliato, E.M.A. Gait analysis comparing Parkinson’s disease with healthy elderly subjects. Arq. Neuropsiquiatr. 2010, 68, 81–86. [Google Scholar] [CrossRef]
- Sofuwa, O.; Nieuwboer, A.; Desloovere, K.; Willems, A.M.; Chavret, F.; Jonkers, I. Quantitative gait analysis in Parkinson’s disease: Comparison with a healthy control group. Arch. Phys. Med. Rehabil. 2005, 86, 1007–1013. [Google Scholar] [CrossRef] [Green Version]
- Taylor, M.J.D.; Dadbnichki, P.; Strike, S.C. A three-dimensional biomechanical comparison between turning strategies during the stance phase of walking. Hum. Mov. Sci. 2005, 24, 558–573. [Google Scholar] [CrossRef]
- Segal, A.; Orendurff, M.; Flick, K.; Berge, J.; Klute, G. Ankle biomechanics during a spin turn. In Proceedings of the 28th Annual Meeting of the American Society of Biomechanics, Boulder, CO, USA, 15 July 2004; p. 168. [Google Scholar]
- Xu, D.; Chow, J.W.; Wang, Y.T. Effects of turn angle and pivot foot on lower extremity kinetics during walk and turn actions. J Appl. Biomech. 2006, 22, 74–79. [Google Scholar] [CrossRef]





| Subject No. | Age (yrs) | Sex | Body Mass (kg) | Body Height (m) | BMI (kg·m−2) | Disease Duration (yrs) | Y&H Score | UPDRS Score | MMSE | Medication | Side of Appearance of the First Motor Symptom |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PD1 | 77 | F | 80 | 1.64 | 29.74 | 4 | 1 | 26 | 29 | Levodopa/carbidopa | Left |
| PD2 | 66 | F | 63 | 1.58 | 25.24 | 4 | 3 | 37 | 27 | Levodopa/carbidopa | Left |
| PD3 | 71 | M | 70 | 1.70 | 24.22 | 3 | 1 | 24 | 28 | Levodopa/benserazide | Right |
| PD4 | 59 | M | 65 | 1.70 | 22.49 | 9 | 1 | 26 | 29 | Levodopa/carbidopa | Left |
| PD5 | 67 | M | 80 | 1.66 | 29.03 | 3 | 1 | 30 | 26 | Levodopa/carbidopa | Right |
| PD6 | 67 | M | 80 | 1.77 | 25.54 | 6 | 1 | 30 | 28 | Levodopa/benserazide | Left |
| PD7 | 63 | F | 55 | 1.59 | 21.76 | 1 | 1 | 23 | 29 | Levodopa/benserazide | Right |
| PD8 | 77 | M | 82 | 1.88 | 23.20 | 8 | 1 | 25 | 24 | Levodopa/carbidopa | Right |
| PD9 | 67 | M | 93 | 1.78 | 29.35 | 7 | 2 | 32 | 25 | Levodopa/carbidopa | Left |
| Stance Time (s) | Swing Time (s) | |||||
| Walking Direction | CR | PDNA | PDA | CR | PDNA | PDA |
| WF_ST | 0.72 ± 0.05 | 0.74 ± 0.12 a | 0.74 ± 0.18 c,l | 0.33 ± 0.03 | 0.33 ± 0.04 | 0.33 ± 0.02 a |
| T60_ST | 0.73 ± 0.07 a | 0.76 ± 0.13 a,h,m | 0.75 ± 0.12 b,g | 0.33 ± 0.04 | 0.33 ± 0.04 | 0.35 ± 0.03 |
| T120_ST | 0.75 ± 0.07 b | 0.78 ± 0.14 b,h,m | 0.78 ± 0.14 c,l,g | 0.33 ± 0.04 | 0.35 ± 0.03 | 0.35 ± 0.03 |
| WF_DT | 0.75 ± 0.07 m | 0.80 ± 0.12 a,m | 0.78 ± 0.11 c,l | 0.33 ± 0.04 | 0.34 ± 0.04 | 0.35 ± 0.05 a |
| T60_DT | 0.78 ± 0.11 a | 0.84 ± 0.14 a | 0.82 ± 0.14 b | 0.33 ± 0.03 | 0.34 ± 0.04 | 0.35 ± 0.04 |
| T120_DT | 0.81 ± 0.11 b,m | 0.85 ± 0.14 b,m | 0.83 ± 0.13 c,l | 0.34 ± 0.04 | 0.35 ± 0.05 | 0.37 ± 0.06 |
| Stride Time (s) | Cadence (Stride·min−1) | |||||
| Walking Direction | CR | PDNA | PDA | CR | PDNA | PDA |
| WF_ST | 1.05 ± 0.08 a | 1.07 ± 0.12 a,n | 1.08 ± 0.12 b,m | 114.79 ± 8.68 a | 113.55 ± 12.27 c,n | 112.74 ± 11.91 b,d,m |
| T60_ST | 1.06 ± 0.11 a | 1.09 ± 0.12 a,h | 1.10 ± 0.12 b | 113.77 ± 10.01 a | 111.35 ± 12.10 c,i | 109.92 ± 11.32 b,d |
| T120_ST | 1.08 ± 0.11 a | 1.14 ± 0.14 c,n,h | 1.13 ± 0.13 a,m | 112.16 ± 9.96 b | 106.90 ± 12.98 a,i,n | 107.04 ± 12.10 a,m |
| WF_DT | 1.09 ± 0.10 a,l | 1.13 ± 0.11 a,n | 1.13 ± 0.12 b,n | 110.94 ± 10.08 a,m | 106.76 ± 10.79 c,n | 106.79 ± 10.92 b,m |
| T60_DT | 1.11 ± 0.13 a | 1.18 ± 0.13 a | 1.18 ± 0.13 b | 108.88 ± 12.57 a,g | 102.94 ± 11.55 c | 103.04 ± 11.02 b |
| T120_DT | 1.14 ± 0.12 a,l | 1.20 ± 0.15 c,n | 1.20 ± 0.14 a,n | 105.84 ± 10.87 b,g,m | 101.00 ± 12.46 a,n | 101.44 ± 11.97 a,m |
| Step Frequency (Hz) | Stride Length (m) | Walking Speed (m·s−1) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Walking Direction | CR | PDNA | PDA | CR | PDNA | PDA | CR | PDNA | PDA |
| WF_ST | 0.95 ± 0.08 a | 0.95 ± 0.10 c,n | 0.94 ± 0.10 b,m | 1.34 ± 0.10 a,n,#,° | 1.23 ± 0.14 b,n,# | 1.24 ± 0.14 c,n,° | 1.28 ± 0.12 c,m,#,° | 1.17 ± 0.21 b,f,n,# | 1.17 ± 0.21 b,e,n,° |
| T60_ST | 0.95 ± 0.08 a | 0.93 ± 0.10 c,h | 0.92 ± 0.10 b | 1.33 ± 0.08 b,h,#,° | 1.20 ± 0.14 b,i,# | 1.23 ± 0.16 c,i,° | 1.26 ± 0.12 c,i,#,° | 1.06 ± 0.17 f,i,# | 1.06 ± 0.18 e,i,° |
| T120_ST | 0.93 ± 0.08 b | 0.89 ± 0.11 a,h,n | 0.89 ± 0.10 a,m | 1.24 ± 0.07 a,h,n,#,° | 1.05 ± 0.13 i,n,# | 1.05 ± 0.11 i,n,° | 1.15 ± 0.12 b,i,m,#,° | 0.95 ± 0.15 i,n,# | 0.95 ± 0.14 i,n,° |
| WF_DT | 0.92 ± 0.08 a,m | 0.89 ± 0.09 c,n | 0.89 ± 0.09 b,m | 1.27 ± 0.06 a,n,#,° | 1.14 ± 0.12 b,n,# | 1.15 ± 0.13 c,n,° | 1.18 ± 0.10 c,n,#,° | 1.09 ± 0.17 b,d,n,# | 1.11 ± 0.18 b,n,° |
| T60_DT | 0.91 ± 0.10 a,g | 0.86 ± 0.10 c | 0.86 ± 0.09 b | 1.26 ± 0.07 b,i,#,° | 1.14 ± 0.15 b,i,# | 1.14 ± 0.15 c,i,° | 1.14 ± 0.15 c,i,#,° | 1.03 ± 0.18 d,i,# | 1.06 ± 0.17 i,° |
| T120_DT | 0.88 ± 0.09 b,g,m | 0.84 ± 0.10 a,n | 0.84 ± 0.10 a,m | 1.18 ± 0.08 a,i,n,#,° | 1.02 ± 0.16 i,n,# | 1.01 ± 0.16 i,n,° | 1.04 ± 0.14 b,i,n,#,° | 0.89 ± 0.16 i,n,# | 0.89 ± 0.14 i,n,° |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nardello, F.; Bertoli, E.; Bombieri, F.; Bertucco, M.; Monte, A. The Effect of a Secondary Task on Kinematics during Turning in Parkinson’s Disease with Mild to Moderate Impairment. Symmetry 2020, 12, 1284. https://0-doi-org.brum.beds.ac.uk/10.3390/sym12081284
Nardello F, Bertoli E, Bombieri F, Bertucco M, Monte A. The Effect of a Secondary Task on Kinematics during Turning in Parkinson’s Disease with Mild to Moderate Impairment. Symmetry. 2020; 12(8):1284. https://0-doi-org.brum.beds.ac.uk/10.3390/sym12081284
Chicago/Turabian StyleNardello, Francesca, Emanuele Bertoli, Federica Bombieri, Matteo Bertucco, and Andrea Monte. 2020. "The Effect of a Secondary Task on Kinematics during Turning in Parkinson’s Disease with Mild to Moderate Impairment" Symmetry 12, no. 8: 1284. https://0-doi-org.brum.beds.ac.uk/10.3390/sym12081284