Health-Related Quality of Life, Family Conflicts and Fear of Injecting: Perception Differences between Preadolescents and Adolescents with Type 1 Diabetes and Their Mothers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting and Procedure
2.3. Participants and Study Size
2.4. Variables
2.5. Measures
2.5.1. Diabetes Quality of Life for Youth-Short Form (DQOL-SF)
2.5.2. Revised Diabetes Family Conflict Scale (DFCS-R)
2.5.3. Diabetes Fear of Injecting Questionnaire (D-FISQ)
2.5.4. Diabetes Information
2.6. Statistical Methods and Bias
3. Results
3.1. Descriptive Data of Participants
3.2. Quality of Life and Family Conflicts of Patients and Their Mothers Compared with Norms
3.3. Comparison between Patients’ and Their Mothers’ Reports on Patient’s Fear of Injecting and Family Conflicts
3.4. Factors Associated with Patient’s Quality of Life
3.5. Factors Associated with Mother’s Family Conflict Score
4. Discussion
5. Limitations, Future Implications and Clinical Suggestions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patterson, C.C.; Karuranga, S.; Salpea, P.; Saeedi, P.; Dahlquist, G.; Soltesz, G.; Ogle, G.D. Worldwide estimates of incidence, prevalence and mortality of type 1 diabetes in children and adolescents: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Prac. 2019, 157, 107842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonder-Frederick, L.A.; Cox, D.J.; Ritterband, L.M. Diabetes and behavioral medicine: The second decade. J. Consult. Clin. Psychol. 2002, 70, 611–625. [Google Scholar] [CrossRef] [PubMed]
- Vaid, B.E.; Lansing, A.H.; Stanger, C. Problems with Self-Regulation, Family Conflict, and Glycemic Control in Adolescents Experiencing Challenges with Managing Type 1 Diabetes. J. Pediatr. Psychol. 2018, 43, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.J.; Holmbeck, G.; Iannotti, R.J.; McKay, S.V.; Lochrie, A.; Volkening, L.K.; Laffel, L. Dyadic measures of the parent–child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Fam. Syst. Health 2009, 27, 141–152. [Google Scholar] [CrossRef]
- Berg, C.A.; Butner, J.E.; Butler, J.M.; King, P.S.; Hughes, A.E.; Wiebe, D.J. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychol. 2013, 32, 719–728. [Google Scholar] [CrossRef]
- Berg, C.A.; Queen, T.; Butner, J.E.; Turner, S.L.; Lansing, A.H.; Main, A.; Anderson, J.H.; Thoma, B.C.; Winnick, J.B.; Wiebe, D.J. Adolescent Disclosure to Parents and Daily Management of Type 1 Diabetes. J. Pediatr. Psychol. 2017, 42, 75–84. [Google Scholar] [CrossRef] [Green Version]
- Marker, A.M.; Noser, A.E.; Clements, M.A.; Patton, S.R. Shared Responsibility for Type 1 Diabetes Care Is Associated with Glycemic Variability and Risk of Glycemic Excursions in Youth. J. Pediatr. Psychol. 2018, 43, 61–71. [Google Scholar] [CrossRef]
- Young, M.T.; Lord, J.H.; Patel, N.J.; Gruhn, M.A.; Jaser, S.S. Good Cop, Bad Cop: Quality of Parental Involvement in Type 1 Diabetes Management in Youth. Curr. Diabetes Rep. 2014, 14, 546. [Google Scholar] [CrossRef] [Green Version]
- Wiebe, D.J.; Chow, C.M.; Palmer, D.L.; Butner, J.; Butler, J.M.; Osborn, P.; Berg, C.A. Developmental Processes Associated with Longitudinal Declines in Parental Responsibility and Adherence to Type 1 Diabetes Management Across Adolescence. J. Pediatr. Psychol. 2014, 39, 532–541. [Google Scholar] [CrossRef]
- Helgeson, V.S.; Reynolds, K.A.; Siminerio, L.; Escobar, O.; Becker, M.D. Parent and Adolescent Distribution of Responsibility for Diabetes Self-care: Links to Health Outcomes. J. Pediatr. Psychol. 2008, 33, 497–508. [Google Scholar] [CrossRef] [Green Version]
- Powers, M.A.; Richter, S.A.; Ackard, D.M.; Craft, C. Diabetes Distress Among Persons with Type 1 Diabetes: Associations with Disordered Eating, Depression, and Other Psychological Health Concerns. Diabetes Educ. 2017, 43, 105–113. [Google Scholar] [CrossRef]
- Carroll, N.C.; Vittrup, B. Type 1 Diabetes in Adolescence: Considerations for Mental Health Professionals. J. Child Adolesc. Couns. 2020, 6, 137–148. [Google Scholar] [CrossRef]
- Delamater, A.M.; De Wit, M.; McDarby, V.; Malik, J.A.; Hilliard, M.E.; Northam, E.; Acerini, C.L. ISPAD Clinical Practice Consensus Guidelines 2018: Psychological care of children and adolescents with type 1 diabetes. Pediatr. Diabetes 2018, 19, 237–249. [Google Scholar] [CrossRef]
- Egede, L.E.; Dismuke, C.E. Serious Psychological Distress and Diabetes: A Review of the Literature. Curr. Psychiatry Rep. 2012, 14, 15–22. [Google Scholar] [CrossRef]
- Laffel, L.M.B.; Connell, A.; Vangsness, L.; Goebel-Fabbri, A.; Mansfield, A.; Anderson, B.J. General Quality of Life in Youth with Type 1 Diabetes: Relationship to patient management and diabetes-specific family conflict. Diabetes Care 2003, 26, 3067–3073. [Google Scholar] [CrossRef] [Green Version]
- Hilliard, M.E.; Holmes, C.S.; Chen, R.; Maher, K.; Robinson, E.; Streisand, R. Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychol. 2013, 32, 388–396. [Google Scholar] [CrossRef]
- Hood, K.K.; Butler, D.A.; Anderson, B.J.; Laffel, L.M.B. Updated and Revised Diabetes Family Conflict Scale. Diabetes Care 2007, 30, 1764–1769. [Google Scholar] [CrossRef] [Green Version]
- Iturralde, E.; Rausch, J.R.; Weissberg-Benchell, J.; Hood, K.K. Diabetes-Related Emotional Distress Over Time. Pediatrics 2019, 143, e20183011. [Google Scholar] [CrossRef]
- Fu, A.Z.; Qiu, Y.; Radican, L. Impact of fear of insulin or fear of injection on treatment outcomes of patients with diabetes. Curr. Med. Res. Opin. 2009, 25, 1413–1420. [Google Scholar] [CrossRef]
- Mollema, E.D.; Snoek, F.J.; Pouwer, F.; Heine, R.J.; Van Der Ploeg, H.M. Diabetes Fear of Injecting and Self-Testing Questionnaire: A psychometric evaluation. Diabetes Care 2000, 23, 765–769. [Google Scholar] [CrossRef] [Green Version]
- Cemeroglu, A.P.; Can, A.; Davis, A.T.; Cemeroglu, O.; Kleis, L.; Daniel, M.S.; Bustraan, J.; Koehler, T.J. Fear of Needles in Children with Type 1 Diabetes Mellitus on Multiple Daily Injections and Continuous Subcutaneous Insulin Infusion. Endocr. Prac. 2015, 21, 46–53. [Google Scholar] [CrossRef]
- Al Hayek, A.A.; Robert, A.A.; Babli, S.; Almonea, K.; Al Dawish, M.A. Fear of Self-Injecting and Self-Testing and the Related Risk Factors in Adolescents with Type 1 Diabetes: A Cross-Sectional Study. Diabetes Ther. 2017, 8, 75–83. [Google Scholar] [CrossRef] [Green Version]
- Simmons, J.H.; McFann, K.K.; Brown, A.C.; Rewers, A.; Follansbee, D.; Temple-Trujillo, R.E.; Klingensmith, G.J. Reliability of the Diabetes Fear of Injecting and Self-Testing Questionnaire in Pediatric Patients with Type 1 Diabetes. Diabetes Care 2007, 30, 987–988. [Google Scholar] [CrossRef] [Green Version]
- Hanas, R. Reducing injection pain in children and adolescents with diabetes: A review of indwelling catheters. Pediatr. Diabetes 2004, 5, 102–111. [Google Scholar] [CrossRef]
- Howe, C.J.; Ratcliffe, S.J.; Tuttle, A.; Dougherty, S.; Lipman, T.H. Needle Anxiety in Children with Type 1 Diabetes and Their Mothers. MCN Am. J. Matern. Nurs. 2011, 36, 25–31. [Google Scholar] [CrossRef]
- Tremolada, M.; Bonichini, S.; Piovan, V.; Pastore, N.; Mazzoldi, M. Psychological Well-being in Parents of Paediatric Patients with TD1. Role of Family Conflict and Parental Fear of Children’s Self-injecting on Their Glycaemic Control and Psychological Well-being. Br. J. Educ. Soc. Behav. Sci. 2017, 19, 1–13. [Google Scholar] [CrossRef]
- Moreira, H.; Frontini, R.; Bullinger, M.; Canavarro, M.C. Family Cohesion and Health-Related Quality of Life of Children with Type 1 Diabetes: The Mediating Role of Parental Adjustment. J. Child Fam. Stud. 2014, 23, 347–359. [Google Scholar] [CrossRef]
- Grey, M.; Boland, E.A.; Yu, C.; Sullivan-Bolyai, S.; Tamborlane, W.V. Personal and Family Factors Associated with Quality of Life in Adolescents with Diabetes. Diabetes Care 1998, 21, 909–914. [Google Scholar] [CrossRef]
- Wagner, V.M.; Müller-Godeffroy, E.; Von Sengbusch, S.; Häger, S.; Thyen, U. Age, metabolic control and type of insulin regime influences health-related quality of life in children and adolescents with type 1 diabetes mellitus. Eur. J. Pediatr. 2005, 164, 491–496. [Google Scholar] [CrossRef]
- Hvidøre Study Group on Childhood Diabetes; Skinner, T.C.; Hoey, H.; McGee, H.M.; Skovlund, S.E. A short form of the Diabetes Quality of Life for Youth questionnaire: Exploratory and confirmatory analysis in a sample of 2,077 young people with type 1 diabetes mellitus. Diabetologia 2006, 49, 621–628. [Google Scholar] [CrossRef]
- Weissberg-Benchell, J.; Nansel, T.; Holmbeck, G.; Chen, R.; Anderson, B.; Wysocki, T.; Laffel, L. Generic and Diabetes-specific Parent–Child Behaviors and Quality of Life Among Youth with Type 1 Diabetes. J. Pediatr. Psychol. 2009, 34, 977–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinger, K.; O’Donnell, K.A.; Ritholz, M.D. Adolescent views of diabetes-related parent conflict and support: A focus group analysis. J. Adolesc. Health 2001, 29, 330–336. [Google Scholar] [CrossRef] [Green Version]
- Williams, L.B.; Laffel, L.M.B.; Hood, K.K. Diabetes-specific family conflict and psychological distress in paediatric Type 1 diabetes. Diabet. Med. 2009, 26, 908–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, M.J.; Gagliardino, J.J.; Gray, L.J.; Khunti, K.; Mohan, V.; Hughes, R. Real-world factors affecting adherence to insulin therapy in patients with Type 1 or Type 2 diabetes mellitus: A systematic review. Diabet. Med. 2013, 30, 512–524. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.H.; Kim, J.H. Time in Range from Continuous Glucose Monitoring: A Novel Metric for Glycemic Control. Diabetes Metab. J. 2020, 44, 828–839. [Google Scholar] [CrossRef] [PubMed]
- Savin, K.L.; Hamburger, E.R.; Monzon, A.D.; Patel, N.J.; Perez, K.M.; Lord, J.H.; Jaser, S.S. Diabetes-specific family conflict: Informant discrepancies and the impact of parental factors. J. Fam. Psychol. 2018, 32, 157–163. [Google Scholar] [CrossRef]
- Rybak, T.M.; Ali, J.S.; Berlin, K.S.; Klages, K.L.; Banks, G.G.; Kamody, R.C.; Ferry, R.J.; Alemzadeh, R.; Diaz-Thomas, A.M. Patterns of Family Functioning and Diabetes-Specific Conflict in Relation to Glycemic Control and Health-Related Quality of Life Among Youth with Type 1 Diabetes. J. Pediatr. Psychol. 2017, 42, 40–51. [Google Scholar] [CrossRef] [Green Version]
- Campbell, M.J.S.; Wang, J.; Cheng, Y.; Cogen, F.R.; Streisand, R.; Monaghan, M. Diabetes-specific family conflict and responsibility among emerging adults with type 1 diabetes. J. Fam. Psychol. 2019, 33, 788–796. [Google Scholar] [CrossRef]
- McLenon, J.; Rogers, M.A.M. The fear of needles: A systematic review and meta-analysis. J. Adv. Nurs. 2019, 75, 30–42. [Google Scholar] [CrossRef] [Green Version]
- Birnie, K.A.; Noel, M.; Parker, J.A.; Chambers, C.T.; Uman, L.S.; Kisely, S.R.; McGrath, P.J. Systematic Review and Meta-Analysis of Distraction and Hypnosis for Needle-Related Pain and Distress in Children and Adolescents. J. Pediatr. Psychol. 2014, 39, 783–808. [Google Scholar] [CrossRef] [Green Version]
- Willemsen, H.; Chowdhury, U.; Briscall, L. Needle Phobia in Children: A Discussion of Aetiology and Treatment Options. Clin. Child Psychol. Psychiatry 2002, 7, 609–619. [Google Scholar] [CrossRef]
- Nansel, T.R.; Iannotti, R.J.; Simons-Morton, B.G.; Cox, C.; Plotnick, L.P.; Clark, L.M.; Zeitzoff, L. Diabetes Personal Trainer Outcomes: Short-term and 1-year outcomes of a diabetes personal trainer intervention among youth with type 1 diabetes. Diabetes Care 2007, 30, 2471–2477. [Google Scholar] [CrossRef] [Green Version]
- McMurtry, C.M.; Taddio, A.; Noel, M.; Antony, M.M.; Chambers, C.T.; Asmundson, G.J.G.; Riddell, R.P.; Shah, V.; Macdonald, N.E.; Rogers, J.; et al. Exposure-based Interventions for the management of individuals with high levels of needle fear across the lifespan: A clinical practice guideline and call for further research. Cogn. Behav. Ther. 2016, 45, 217–235. [Google Scholar] [CrossRef] [Green Version]
- Peyrot, M.; Rubin, R.R. Behavioral and Psychosocial Interventions in Diabetes: A conceptual review. Diabetes Care 2007, 30, 2433–2440. [Google Scholar] [CrossRef] [Green Version]
- Missotten, L.C.; Luyckx, K.; Seiffge-Krenke, I. Family Climate of Adolescents with and without Type 1 Diabetes: Longitudinal Associations with Psychosocial Adaptation. J. Child Fam. Stud. 2013, 22, 344–354. [Google Scholar] [CrossRef]
| Socio-Demographic Variable | Range/Levels | N | % |
|---|---|---|---|
| Gender | Male | 50 | 49 |
| Female | 52 | 51 | |
| Age | Preadolescents (range: 10–14 years) | 48 | 47.1 |
| Adolescents (15–19 years) | 54 | 52.9 | |
| Mean | SD | ||
| HbA1c | Range: 5.5–11.1 | 7.6 | 1 |
| Time from diagnosis (years) | Range: 0–15 | 7.9 | 4 |
| Socio-Demographic Variable | Range/Levels | Mean | SD |
|---|---|---|---|
| Age | Range: 27–63 years | 46.9 | 6.2 |
| N | % | ||
| Relationship status | Married | 76 | 74.5 |
| Divorced/Separated | 18 | 17.7 | |
| Cohabitant | 6 | 5.9 | |
| Single parent | 1 | 1 | |
| Missing | 1 | 1 | |
| Perceived economic condition | Insufficient | 8 | 7.8 |
| Sufficient | 28 | 27.5 | |
| Adequate | 39 | 38.2 | |
| Good | 25 | 24.5 | |
| Optimal | 2 | 2 | |
| Level of education | Primary school | 1 | 1 |
| Lower secondary school | 40 | 39.2 | |
| Upper secondary school | 43 | 42.2 | |
| University Degree | 14 | 13.7 | |
| Ph.D. or Master’s degree | 4 | 3.9 |
| Variable | Typology | Mean | SD | Minimum–Maximum |
|---|---|---|---|---|
| D-FISQ patients | FSI | 1.3 | 2.3 | 0–12 |
| FST | 1.6 | 2.6 | 0–13 | |
| D-FISQ patients global score | FSI + FST | 2.3 | 4.2 | 0–22 |
| D-FISQ mothers’ reports on their own experience of injecting (N = 54 for FSI and 48 for FST) | FSI | 1.4 | 2.7 | 0–12 |
| FST | 1.5 | 3.5 | 0–21 | |
| D-FISQ mothers global score | FSI + FST | 3.7 | 5.9 | 0–32 |
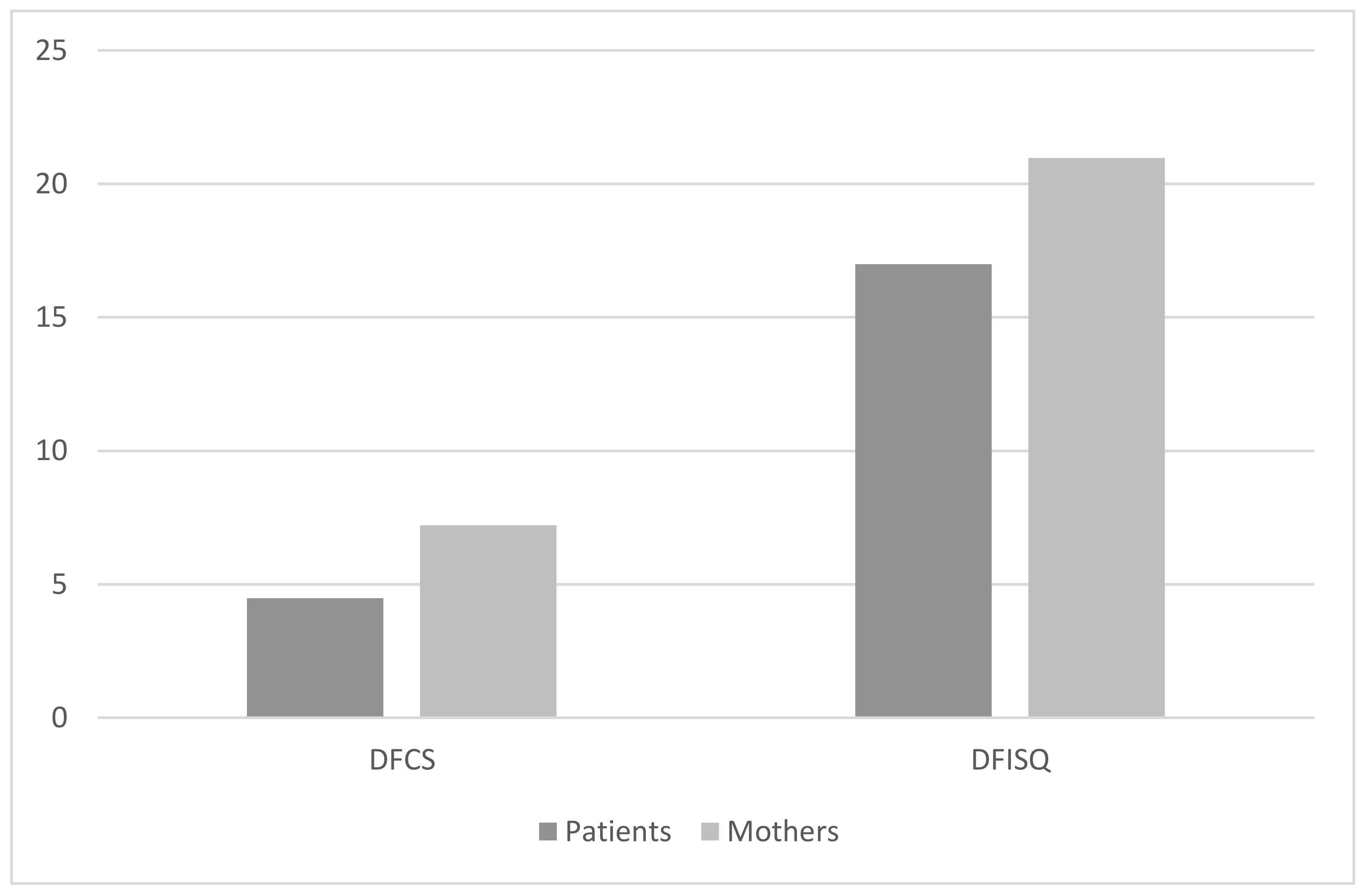
| DFCS patients | 17 | 10.6 | 0–49 | |
| DFCS mothers | 21 | 11.6 | 0–54 | |
| DQOLY | 16.3 | 7.2 | 3–34 |
| Variable | DFISQ_Self | DFISQ_Mother | DFCS_Patient | DFCS_Mother | DQOLY | DQOLY_Impact | DQOLY_Worries |
|---|---|---|---|---|---|---|---|
| Gender | rho = 0.02 p = 0.8 | rho = −0.01 p = 0.9 | rho = −0.1 p = 0.2 | rho = 0.09 p = 0.3 | rho =0.05 p = 0.6 | rho = −0.02 p = 0.8 | rho = 0.1 p = 0.3 |
| Patient’s Age | rho = −0.07 p = 0.4 | rho = −0.3 ** p = 0.001 | rho = −0.03 p = 0.8 | rho = −0.09 p = 0.3 | rho = 0.2 * p = 0.013 | rho = 0.1 p = 0.1 | rho = 0.3 * p = 0.005 |
| HbA1c | rho = 0.009 p = 0.3 | rho = 0.1 p = 0.3 | rho = 0.03 p = 0.8 | rho = 0.1 p = 0.2 | rho = 0.05 p = 0.6 | rho = 0.02 p = 0.8 | rho = 0.07 p = 0.5 |
| Time from diagnosis | rho = −0.06 p = 0.5 | rho = −0.1 p = 0.2 | rho = 0.09 p = 0.3 | rho = 0.1 p = 0.1 | rho = 0.1 p = 0.2 | rho = −0.012 p = 0.9 | rho = 0.2 * p = 0.03 |
| Mother’s age | rho = −0.11 p = 0.2 | rho = −0.3 ** p = 0.004 | RHO = 0.1 p = 0.3 | rho = −0.1 p = 0.2 | rho = 0.1 p = 0.1 | rho = 0.2 p = 0.07 | rho = 0.06 p = 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tremolada, M.; Cusinato, M.; Bonichini, S.; Fabris, A.; Gabrielli, C.; Moretti, C. Health-Related Quality of Life, Family Conflicts and Fear of Injecting: Perception Differences between Preadolescents and Adolescents with Type 1 Diabetes and Their Mothers. Behav. Sci. 2021, 11, 98. https://0-doi-org.brum.beds.ac.uk/10.3390/bs11070098
Tremolada M, Cusinato M, Bonichini S, Fabris A, Gabrielli C, Moretti C. Health-Related Quality of Life, Family Conflicts and Fear of Injecting: Perception Differences between Preadolescents and Adolescents with Type 1 Diabetes and Their Mothers. Behavioral Sciences. 2021; 11(7):98. https://0-doi-org.brum.beds.ac.uk/10.3390/bs11070098
Chicago/Turabian StyleTremolada, Marta, Maria Cusinato, Sabrina Bonichini, Arianna Fabris, Claudia Gabrielli, and Carlo Moretti. 2021. "Health-Related Quality of Life, Family Conflicts and Fear of Injecting: Perception Differences between Preadolescents and Adolescents with Type 1 Diabetes and Their Mothers" Behavioral Sciences 11, no. 7: 98. https://0-doi-org.brum.beds.ac.uk/10.3390/bs11070098






