Root Canal Morphology of the Permanent Mandibular Incisors by Cone Beam Computed Tomography: A Systematic Review
Abstract
:1. Introduction
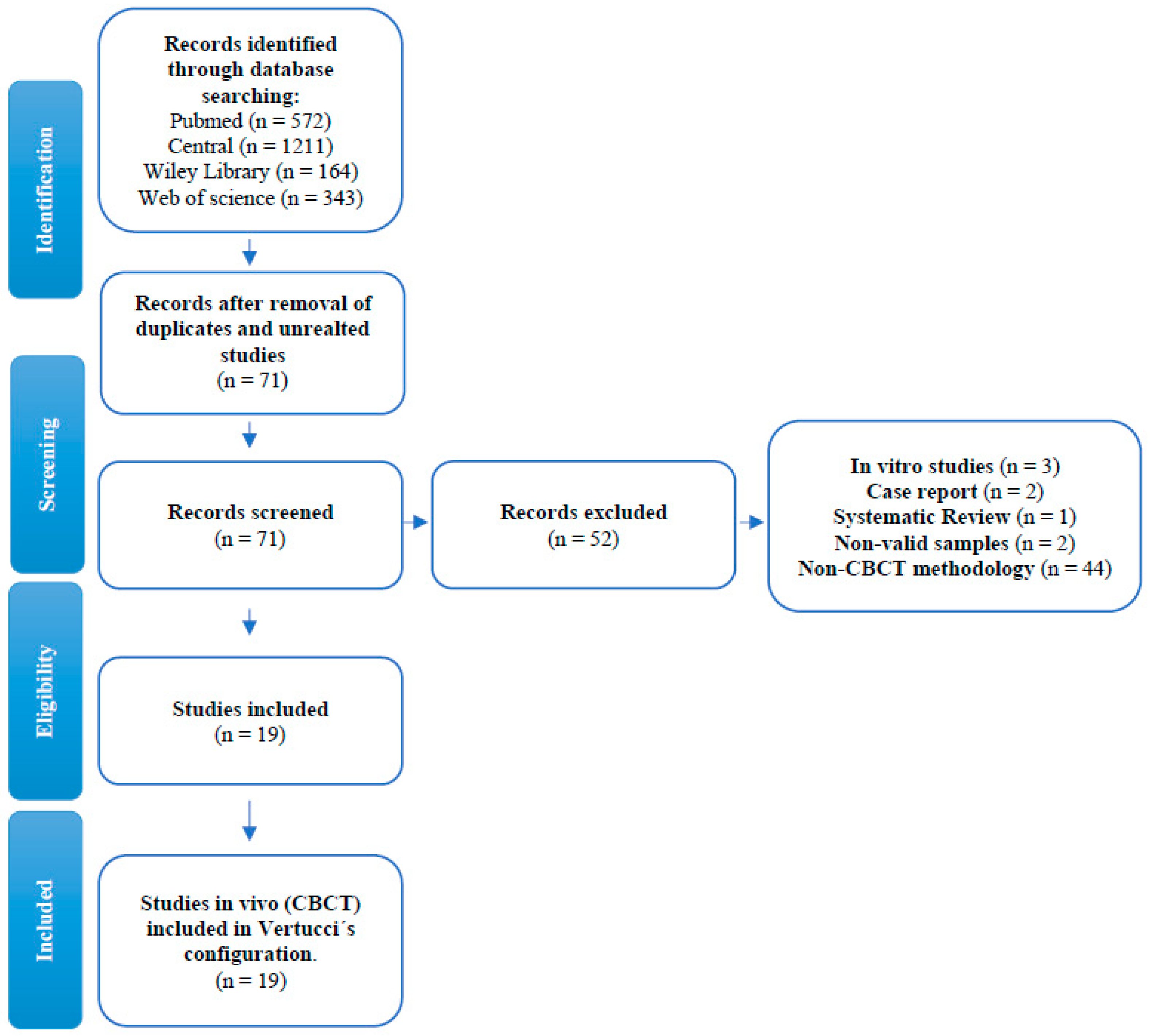
2. Methods
2.1. Protocols
2.2. Search Method for the Identification of Studies
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction and Analysis
2.5. Quality of the Reports of the Included Studies
3. Results
3.1. Characteristics of the Studies
3.2. Quality of the Reports of the Included Studies
3.3. Synthesis of Studies Included
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CBCT | Cone-Beam Computed Tomography |
| µ-CT | Micro-Computed Tomography |
| FOV | Field of View |
References
- Kucher, M.; Dannemann, M.; Modler, N.; Haim, D.; Hannig, C.; Weber, M.-T. Continuous Measurement of Three-Dimensional Root Canal Curvature Using Cone-Beam Computed and Micro-Computed Tomography: A Comparative Study. Dent. J. 2020, 8, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vertucci, F.J. Root canal anatomy of the human permanent teeth. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 589–599. [Google Scholar] [CrossRef]
- Naoum, H.J.; Chandler, N.P.; Love, R. Conventional versus Storage Phosphor-Plate Digital Images to Visualize the Root Canal System Contrasted with a Radiopaque Medium. J. Endod. 2003, 29, 349–352. [Google Scholar] [CrossRef]
- Assadian, H.; Dabbaghi, A.; Gooran, M.; Eftekhar, B.; Sharifi, S.; Shams, N.; Najvani, A.D.; Tabesh, H. Accuracy of CBCT, Digital Radiography and Cross-Sectioning for the Evaluation of Mandibular Incisor Root Canals. Iran. Endod. J. 2016, 11, 106–110. [Google Scholar] [PubMed]
- Gilles, J.; Reader, A. An SEM investigation of the mesiolingual canal in human maxillary first and second molars. Oral Surg. Oral Med. Oral Pathol. 1990, 70, 638–643. [Google Scholar] [CrossRef]
- Nogueira, B.M.L.; Fagundes, N.C.F.; Menezes, T.O.D.A.; Lima, R.R.; Brandão, J.M.D.S. Root and Canal Morphology of Permanent Mandibular Incisors. Int. J. Odontostomatol. 2017, 11, 95–100. [Google Scholar] [CrossRef] [Green Version]
- Baxter, S.; Jablonski, M.; Hülsmann, M. Cone-beam-computed-tomography of the symmetry of root canal anatomy in mandibular incisors. J. Oral Sci. 2020, 62, 180–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolf, T.G.; Stiebritz, M.; Boemke, N.; Elsayed, I.; Paqué, F.; Wierichs, R.J.; Briseño-Marroquín, B. 3-dimensional Analysis and Literature Review of the Root Canal Morphology and Physiological Foramen Geometry of 125 Mandibular Incisors by Means of Micro–Computed Tomography in a German Population. J. Endod. 2020, 46, 184–191. [Google Scholar] [CrossRef]
- Ahmed, H.M.A.; Versiani, M.A.; De-Deus, G.; Dummer, P.M.H. A new system for classifying root and root canal morphology. Int. Endod. J. 2016, 50, 761–770. [Google Scholar] [CrossRef] [Green Version]
- Patel, S.; Brown, J.; Semper, M.; Abella, F.; Mannocci, F.; Dummer, P.M.H. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics. Int. Endod. J. 2019, 52, 1675–1678. [Google Scholar] [CrossRef] [Green Version]
- Martins, J.N.; Marques, D.; Silva, E.J.N.L.; Caramês, J.; Versiani, M.A. Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review. J. Endod. 2019, 45, 372–386.e4. [Google Scholar] [CrossRef] [PubMed]
- Von Arx, T. Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Int. Endod. J. 2005, 38, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Baruwa, A.O.; Martins, J.N.; Meirinhos, J.; Pereira, B.; Gouveia, J.; Quaresma, S.A.; Monroe, A.; Ginjeira, A. The Influence of Missed Canals on the Prevalence of Periapical Lesions in Endodontically Treated Teeth: A Cross-sectional Study. J. Endod. 2019, 46, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.P.L.; Nardello, L.C.L.; Fernandes, F.S.; Bruno, F.P.; Paz, L.R.; Iglecias, E.F.; Honório, H.M.; Mayer, M.P.A.; Gavini, G.; Pinheiro, E.T. Effects of Contemporary Irrigant Activation Schemes and Subsequent Placement of an Interim Dressing on Bacterial Presence and Activity in Root Canals Associated with Asymptomatic Apical Periodontitis. J. Clin. Med. 2020, 9, 854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, J.N.; Gu, Y.; Marques, D.; Francisco, H.; Caramês, J. Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-beam Computed Tomography. J. Endod. 2018, 44, 1096–1104. [Google Scholar] [CrossRef] [Green Version]
- Sert, S.; Bayirli, G.S. Evaluation of the Root Canal Configurations of the Mandibular and Maxillary Permanent Teeth by Gender in the Turkish Population. J. Endod. 2004, 30, 391–398. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Martins, J.N.; Kishen, A.; Marques, D.; Silva, E.J.N.L.; Caramês, J.; Mata, A.; Versiani, M.A. Preferred Reporting Items for Epidemiologic Cross-sectional Studies on Root and Root Canal Anatomy Using Cone-beam Computed Tomographic Technology: A Systematized Assessment. J. Endod. 2020, 46, 915–935. [Google Scholar] [CrossRef]
- Sroczyk-Jaszczyńska, M.; Kołecki, J.; Lipski, M.; Puciło, M.; Wilk, G.; Falkowski, A.; Kot, K.; Nowicka, A. A study of the symmetry of roots and root canal morphology in mandibular anterior teeth using cone-beam computed tomographic imaging in a Polish population. Folia Morphol. 2015. [Google Scholar] [CrossRef] [Green Version]
- Mashyakhy, M. Anatomical analysis of permanent mandibular incisors in a Saudi Arabian population: An in vivo cone-beam computed tomography study. Niger. J. Clin. Pr. 2019, 22, 1611–1616. [Google Scholar] [CrossRef]
- Mirhosseini, F.; Tabrizizadeh, M.; Nateghi, N.; Rad, E.S.; Derafshi, A.; Ahmadi, B.; Daneshvar, M. Evaluation of Root Canal Anatomy in Mandibular Incisors Using CBCT Imaging Technique in an Iranian Population. J. Dent. 2019, 20, 24–29. [Google Scholar]
- Pan, J.Y.Y.; Parolia, A.; Chuah, S.R.; Bhatia, S.; Mutalik, S.; Pau, A. Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health 2019, 19, 14. [Google Scholar] [CrossRef] [PubMed]
- Valenti-Obino, F.; Di Nardo, D.; Quero, L.; Miccoli, G.; Gambarini, G.; Testarelli, L.; Galli, M. Symmetry of root and root canal morphology of mandibular incisors: A cone-beam computed tomography study in vivo. J. Clin. Exp. Dent. 2019, 11, e527–e533. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-C.; Cheng, W.-C.; Weng, P.-W.; Chung, M.-P.; Su, C.-C.; Chiang, H.-S.; Tsai, Y.-W.C.; Chung, C.-H.; Shieh, Y.-S.; Huang, R.-Y. The Presence of Distolingual Root in Mandibular First Molars Is Correlated with Complicated Root Canal Morphology of Mandibular Central Incisors: A Cone-beam Computed Tomographic Study in a Taiwanese Population. J. Endod. 2018, 44, 711–716.e1. [Google Scholar] [CrossRef]
- Saati, S.; Shokri, A.; Foroozandeh, M.; Poorolajal, J.; Mosleh, N. Root Morphology and Number of Canals in Mandibular Central and Lateral Incisors Using Cone Beam Computed Tomography. Braz. Dent. J. 2018, 29, 239–244. [Google Scholar] [CrossRef]
- Shemesh, A.; Kavalerchik, E.; Levin, A.; Ben Itzhak, J.; Levinson, O.; Lvovsky, A.; Solomonov, M. Root canal morphology evaluation of central and lateral mandibular incisors using cone-beam computed tomography in a Israeli population. J. Endod. 2018, 44, 51–55. [Google Scholar] [CrossRef] [Green Version]
- Verma, G.R.; Bhadage, C.; Bhoosreddy, A.R.; Vedpathak, P.R.; Mehrotra, G.P.; Nerkar, A.C.; Bhandari, A.; Chaubey, S. Cone Beam Computed Tomography Study of Root Canal Morphology of Permanent Mandibular Incisors in Indian Subpopulation. Pol. J. Radiol. 2017, 82, 371–375. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, E.J.N.L.; De Castro, R.W.Q.; Nejaim, Y.; Silva, A.I.V.; Haiter-Neto, F.; Silberman, A.; Cohenca, N. Evaluation of root canal configuration of maxillary and mandibular anterior teeth using cone beam computed tomography: An in-vivo study. Quintessence Int. 2016, 47, 19–24. [Google Scholar]
- Zhou, Z.; Yang, Z.; Lu, K.; Wang, F.; Li, Y.; Zhengyan, Y.; Keke, L.; Fei, W.; Yueheng, L.; Zhi, Z. Cone-beam computed tomography study of the root and canal morphology of mandibular permanent anterior teeth in a Chongqing population. Ther. Clin. Risk Manag. 2015, 12, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Geduk, G.; Deniz, Y.; Eroğlu, E.; Zengin, A. Cone-beam computed tomography study of root canal morphology of permanent mandibular incisors in a Turkish sub-population. J. Oral Maxillofac. Radiol. 2015, 3, 7. [Google Scholar] [CrossRef]
- Altunsoy, M.; Ok, E.; Nur, B.G.; Aglarci, O.S.; Gungor, E.; Colak, M. A cone-beam computed tomography study of the root canal morphology of anterior teeth in a Turkish population. Eur. J. Dent. 2014, 8, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Ma, Y.; Yang, L.; Chen, X.; Zhang, X.; Wang, Y. A Study of the Root Canal Morphology of Mandibular Anterior Teeth Using Cone-beam Computed Tomography in a Chinese Subpopulation. J. Endod. 2014, 40, 1309–1314. [Google Scholar] [CrossRef]
- Lin, Z.; Hu, Q.; Wang, T.; Ge, J.; Liu, S.; Zhu, M.; Wen, S. Use of CBCT to investigate the root canal morphology of mandibular incisors. Surg. Radiol. Anat. 2014, 36, 877–882. [Google Scholar] [CrossRef]
- Liu, J.; Luo, J.; Dou, L.; Yang, D. CBCT study of root and canal morphology of permanent mandibular incisors in a Chinese population. Acta Odontol. Scand. 2013, 72, 26–30. [Google Scholar] [CrossRef]
- Aminsobhani, M.; Sadegh, M.; Meraji, N.; Razmi, H.; Kharazifard, M.J. Evaluation of the root and canal morphology of mandibular permanent anterior teeth in a Iranian population by cone-beam computed tomography. J. Dent. 2013, 10, 358–366. [Google Scholar]
- Ghamari, M.; Mollashahi, N.F.; Salarpour, M.; Mousavi, E.; Kazemian, K.; Moudi, E.; Arab, S. Evaluation of the relationship between crown size and root canal morphology of mandibular incisors by cone beam computed tomography (CBCT). Electron. Physician 2017, 9, 5001–5007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neelakantan, P.; Subbarao, C.; Subbarao, C.V. Comparative Evaluation of Modified Canal Staining and Clearing Technique, Cone-Beam Computed Tomography, Peripheral Quantitative Computed Tomography, Spiral Computed Tomography, and Plain and Contrast Medium-enhanced Digital Radiography in Studying Root Canal Morphology. J. Endod. 2010, 36, 1547–1551. [Google Scholar] [CrossRef]
- Kajan, Z.D.; Taramsari, M.; Khosravifard, N.; Kanani, M. Accuracy of Cone-beam Computed Tomography in Comparison with Standard Method in Evaluating Root Canal Morphology: An In Vitro Study. Iran. Endod. J. 2018, 13, 181–187. [Google Scholar]
- Monsarrat, P.; Arcaute, B.; Peters, O.A.; Maury, E.; Telmon, N.; Georgelin- Gurgel, M.; Maret, D. Internationalships in the variability of root canal anatomy among the permanent teeth: A full- mouth approach by cone-beam CT. PLoS ONE 2016, 20, 11. [Google Scholar]
- Tiku, A.M.; Kalaskar, R.R.; Damle, S.G. An unusual presentation of all the mandibular anterior teeth with two root canals—A case report. J. Indian Soc. Pedod. Prev. Dent. 2005, 23, 204. [Google Scholar] [CrossRef]
- Bauman, R.; Scarfe, W.; Clark, S.; Morelli, J.; Scheetz, J.; Farman, A. Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensions. Int. Endod. J. 2011, 44, 752–758. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Marques, D.; Leal Silva, E.J.N.; Caramês, J.; Mata, A.; Versiani, M.A. In Influence of demographic factors on the prevalence of a second root canal in mandibular anterior teeth—A systematic review and meta-analysis of cross-sectional studies using cone beam computed tomography. Arch. Oral Biol. 2020, 116, 104749. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Dawood, A.; Ford, T.P.; Whaites, E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int. Endod. J. 2007, 40, 818–830. [Google Scholar] [CrossRef]
- Brown, J.; Jacobs, R.; Levring Jäghagen, E.; Lindh, C.; Baksi, G.; Schulze, D. Basic training requirements for the use of dental CBCT by dentists: A position paperprepared by the European Academy of Dentomaxillofacial Radiology. Dentomaxillofac. Radiol. 2014, 43, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Martins, J.N.; Alkhawas, M.-B.A.; Altaki, Z.; Bellardini, G.; Berti, L.; Boveda, C.; Chaniotis, A.; Flynn, D.; Gonzalez, J.A.; Kottoor, J.; et al. Worldwide Analyses of Maxillary First Molar Second Mesiobuccal Prevalence: A Multicenter Cone-beam Computed Tomographic Study. J. Endod. 2018, 44, 1641–1649. [Google Scholar] [CrossRef]
- De Pablo, O.V.; Estevez, R.; Sánchez, M.P.; Heilborn, C.; Cohenca, N. Root Anatomy and Canal Configuration of the Permanent Mandibular First Molar: A Systematic Review. J. Endod. 2010, 36, 1919–1931. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Marques, D.; Silva, E.J.N.L.; Caramês, J.; Mata, A.; Versiani, M.A. Prevalence of C-shaped canal morphology using cone beam computed tomography—A systematic review with meta-analysis. Int. Endod. J. 2019, 52, 1556–1572. [Google Scholar] [CrossRef]
- Milani, A.S.; Shahi, S.; Sergiz, Y.; Nezafati, S.; Lotfi, M.; Rahimi, S. Prevalence of two root canals in human mandibular anterior teeth in an Iranian population. Indian J. Dent. Res. 2013, 24, 234. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, S.H.G.; De Moraes, L.C.; Faig-Leite, H.; Camargo, S.E.A.; Camargo, C.H.R. In vitro incidence of root canal bifurcation in mandibular incisors by radiovisiography. J. Appl. Oral Sci. 2009, 17, 234–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Study/Year | n | Country | 2nd Root Canal | Vertucci | Other Outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | Others | |||||
| Baxter et al./2020 [7] | 604 CI 604 LI | Germany | 22.6% 24.3% | 76.1% 76.6% | 22% 21.3% | - | 0.6% 1% | 1.1% 1% | - | - | 0.2% 0.1% | Symmetry: Type I: 77% (CI), 77% (LI); Rest of types: 17.5% (CI), 20.5% (LI). |
| Sroczyk et al./2019 [19] | 212 CI 208 LI | Poland | 34.1% 31.8% | 65.4% 67.2% | 1% 0.9% | 26.4% 25% | - 0.5% | 5.3% 3.9% | - | 1% - | 0.9% 2.5% | Symmetry: Type I: 54.86% (CI), 56.12% (LI). Rest of types: 23.53% (CI), 19,19% (LI). |
| Mashyakhy et al./2019 [20] | 410 CI 412 LI | Saudi Arabia | 26.3% 30.8% | 73.7% 69.2% | - | 26.3% 29.8% | - | - 1% | - | - | - | Symmetry: 91.2% (CI), 85.8% (LI). |
| Mirhosseini et al./2019 [21] | 330 CI 351 LI | Iran | 23.9% 35% | 76.1% 65% | 0% 0.6% | 15.8% 15.7% | 0.6% 0.9% | 7.6% 17.8% | - | - | - | % 2nd root canal: LI > CI |
| Pan et al./2019 [22] | 408 CI 400 LI | Malaysia | 5.1% 12.3% | 94.9% 87.8% | - | 1% 3.7% | 0.3% | 4.1% 8.2% | - | - | - | - |
| Valenti-Obino et al./2019 [23] | 487 CI 491 LI | Italy | 45% 43% | 55% 57% | 34.3% 35.7% | 9.3% 6.9% | 0.6% - | - | - | 0.8% 0.4% | - | Symmetry: 44.6% (CI), 44.8% (LI). |
| Martins et al./2018 [15] | 240 CI 240 LI 1203 CI 1234 LI | China Portugal | 0.4% 5% 27.4% 29.9% | 99.6% 95% 72.6% 70.1% | - 2.9% 2.4% 6.1% | 0.4% 0.8% 24% 23.1% | - - 0.1% - | - 1.3% 0.3% 0.2% | - - - - | - - 0.5% 0.2% | - - 0.1% 0.3% | The Asian group have a higher prevalence of Vertucci type I configuration compared to the white ethnic group. |
| Wu et al./2018 [24] | 800 CI | Taiwan | 15.6% | 84.4% | - | 13.5% | 2.1% | - | - | - | Correlation between complicated root canal CI-DLR in PMFM. | |
| Saati et al./2018 [25] | 207 CI 207 LI | Iran | 15.5% 21.8% | 54.5% 56.5% | - | 34.2% 26.1% | - | 11.3% 17.4% | - | - | - | - |
| Shemesh et al./2018 [26] | 1472 CI 1508 LI | Israel | 40.5% 37.9% | 59.5% 62.1% | 4% 4.3% | 33.7% 31.9% | 0.8% 0.4% | 0.5% 0.5% | - | - | 1.5% 0.8% | Symmetry: 69.8% (CI), 68.7% (LI). |
| Verma et al./2017 [27] | 400 CI 400 LI | India | 31.8% 35% | 68.3% 65% | 11% 13.2% | 15.3% 15.2% | 1.7% 3.0% | 3.7% 3.6% | - | - | - | % 2nd root canal: LI > CI |
| Da Silva et al./2016 [28] | 200 CI 200 LI | Brazil | 35.5% 39.5% | 64.5% 60.5% | - 0.5% | 18% 25.5% | - - | 14.5% 12% | 0.5% - | 2.5% 1.5% | - | - |
| Zhengyan et al./2016 [29] | 3375 CI 3257 LI | China | 3.8% 10.6% | 96.2% 89.4% | 0.1% 1% | 2.7% 7.7% | 0.1% 0.3% | 0.7% 1.2% | - | - | 0.2% 0.4% | 2nd root canal > LI women |
| Geduk et al./2015 [30] | 1438 I | Turkey | 3.6% | 64.4% | 15.2% | 19.4% | 0.2% | 0.8% | - | - | - | 2nd root canal > 41–50 years |
| Altunsoy et al./2014 [31] | 1582 CI 1603 LI | Turkey | 15.3% 19.2% | 84.4% 80.2% | 0.4% 1.3% | 0.8% 1.0% | 4.3% 5.4% | 10.1% 12.1% | - | - | - | 2nd root canal: men > women |
| Han et al./2014 [32] | 1286 CI 1294 LI | China | 15.7% 27.4% | 84.3% 72.6% | 3.4% 4.0% | 6.5% 15.5% | 1.2% 2.3% | 3.9% 5.1% | - 0.2% | 0.3% 0.2% | 0.4% 0.1% | IL > IC. Distance apex-root canal bifurcation: 6–12 mm. |
| Lin et al./2014 [33] | 706 CI 706 LI | China | 10.9% 25.5% | 89.1% 74.5% | 2.4% 3.7% | 6.2% 19.3% | 1.7% 2.1% | 0.6% 0.4% | - | - | - | Symmetry: 95.2% (CI), 93.8% (LI).2nd root canal: LI > CI |
| Liu et al./2014 [34] | 786 CI 785 LI | China | 8.9% 17.5% | 91.1% 82.5% | 2.0% 3.9% | 5.3% 10.4% | 1.3% 2.8% | 0.3% 0.3% | - | - | - | - |
| Aminsobhani et al./2013 [35] | 632 CI 614 LI | Iran | 27.3% 29.4% | 72.7% 70.6% | 11.3% 7.1% | 4.7% 3.7% | 7.7% 15.4% | 3.6% 3.2% | - | - | - | AV: 21.3 ± 0.10 (CI), 21.9 ± 0.13 (LI). No gender difference |
| Study/Year | Country | % 2nd Root Canal | CBCT Model | Voxel Size | FOV | Settings CBCT | Software Visualization |
|---|---|---|---|---|---|---|---|
| Baxter et al./2020 [7] | Germany | 23.45% | Galaxis Galileo (Sirona, Bensheim, Germany) | 0.3 mm | 15 cm3 | 85 Kv/5–7 mA/ | - |
| Sroczyk et al./2019 [19] | Poland | 32.9% | Cranex 3D (Soredex, Tuusula, Finland) | - | - | - | Horos |
| Mashyakhy/2019 [20] | Saudi Arabia | 28.55% | 3D Accuitomo 170 (Morita, Kyoto, Japan) | 0.25 mm | - | 90 Kv/5–8 mA/17.5 s. | Morita’s i-Dixel 3D |
| Mirhosseini et al./2019 [21] | Iran | 23.9% | Planmeca ProMax 3D (Planmeca, Helsinki, Finland) | 0.2 mm | 100 × 70 × 50 mm | 90 Kv/10 mA/14 s. | Planmeca Romexis |
| Pan et al./2019 [22] | Malaysia | 17.4% | KaVo 3D eXam (Imaging Sciences International, Hatfield, PA, USA) | 0.25 mm | - | 120 kV/5 mA/26.9 s. | eXam Vision |
| Valenti-obino et al./2019 [23] | Italy | 44% | GXDP-500 system (Gendex Dental, Biberach, Germany) | 0.2 mm | 13 × 9 × 13 cm | 90 kV/7 mA/23 s. | Horos |
| Martins et al./2018 [15] | China | 2.7% | Kodak 9500 (Carestream, Atlanta, GA) | 0.2 mm | Full arch. | 90 kV/10 mA/10.8 s. | CS 900 3D imaging |
| Martins et al./2018 [15] | Portugal | 28.6% | Planmeca ProMax 3D (Planmeca, Helsinki, Finland) | 0.2 mm | Full arch | 80 kV/15 mA/12.0 s. | Planmeca Romexis |
| Wu et al./2018 [24] | Taiwan | 15.6% | NewTom 5G (QR, Verona, Italy) | - | Full arch | 110 kV/11.94 mA/7 s. | - |
| Shemesh et al./2018 [25] | Israel | 39.2% | Asahi Alioth (Asahi Roentgen IND, Kyoto, Japan) | 0.155 mm | 80 × 80 mm | 85 kV/6 mA | OnDemand 3D |
| Saati et al./2018 [26] | Iran | 18.6% | NewTom 5G (QR, Verona, Italy) | 0.25 mm | - | 110 kV/2.5–6.7 mA/12 s. | NNT Viewer |
| Verma et al./2017 [27] | India | 33.5% | Galaxis Galileo (Sirona, Bensheim, Germany) | - | - | 98 kV/5–15 mA | - |
| Da Silva et al./2016 [28] | Brazil | 37.5% | i-CAT (Imaging Sciences International, Hatfield, PA, USA) | 0.2 mm | - | 120 kV/7 mA/40 s. | i-CAT |
| Zhengyan et al./2016 [29] | China | 7.2% | - | 0.125 mm | - | 120 kV/5 mA/9–18 s. | i-CAT |
| Geduk et al./2015 [30] | Turkey | 3.6% | Galaxis Galileo (Sirona, Bensheim, Germany) | - | - | 98 kV/15–30 mA | SIDEXIS XG |
| Altunsoy et al./2014 [31] | Turkey | 17.3% | i-CAT (Imaging Sciences International, Hatfield, PA, USA) | 0.3 mm | - | 120 kV/9–14 mA/6 s. | - |
| Han et al./2014 [32] | China | 21.7% | Galaxis Galileo (Sirona, Bensheim, Germany) | 0.125 mm | - | 85 kV/35.0 mA/2–6 s. | SIDEXIS XG |
| Lin et al./2014 [33] | - | - | - | - | - | - | |
| Liu et al./2014 [34] | China | 13.2% | i-CAT (Imaging Sciences International, Hatfield, PA, USA) | - | - | 120 kV/5 mA/9–18 s. | eXam Vision |
| Aminsobhani et al./2013 [35] | Irán | 28.35% | Planmeca ProMax 3D (Planmeca, Helsinki, Finland) | - | - | - | Planmeca Romexis |
| Section and Item | n | (%) |
|---|---|---|
| 1. Title | 19 | 100 |
| Introduction | ||
| 2. Keywords | 19 | 100 |
| 3. Aim | 19 | 100 |
| Methods | ||
| 4. Participants (in vivo assessment) | 19 | 100 |
| 5. CBCT | 19 | 100 |
| 6. Morphology concept and assessed teeth (variables) | 19 | 100 |
| 7. Assessment | 19 | 100 |
| 8. Observers | 13 | 68.4 |
| 9. Potential sources of bias | 15 | 78.9 |
| 10. Final simple size | 15 | 78.9 |
| 11. Reliability | 9 | 47.4 |
| 12. Statistical analysis | 13 | 68.4 |
| 13. Ethics Committee | 13 | 78.9 |
| Results | ||
| 14. Primary outcomes | 19 | 100 |
| 15. Other analysis | 15 | 78.9 |
| 16. Visual documentation support | 16 | 84.2 |
| Discussion | ||
| 17. Outcomes interpretation | 19 | 100 |
| 18. Strength and limitations | 6 | 31.5 |
| 19. Generalizability | 19 | 100 |
| 20. Future research | 4 | 21.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrero-Hernández, S.; López-Valverde, N.; Bravo, M.; Valencia de Pablo, Ó.; Peix-Sánchez, M.; Flores-Fraile, J.; Ramírez, J.M.; Macedo de Sousa, B.; López-Valverde, A. Root Canal Morphology of the Permanent Mandibular Incisors by Cone Beam Computed Tomography: A Systematic Review. Appl. Sci. 2020, 10, 4914. https://0-doi-org.brum.beds.ac.uk/10.3390/app10144914
Herrero-Hernández S, López-Valverde N, Bravo M, Valencia de Pablo Ó, Peix-Sánchez M, Flores-Fraile J, Ramírez JM, Macedo de Sousa B, López-Valverde A. Root Canal Morphology of the Permanent Mandibular Incisors by Cone Beam Computed Tomography: A Systematic Review. Applied Sciences. 2020; 10(14):4914. https://0-doi-org.brum.beds.ac.uk/10.3390/app10144914
Chicago/Turabian StyleHerrero-Hernández, Silvia, Nansi López-Valverde, Manuel Bravo, Óliver Valencia de Pablo, Manuel Peix-Sánchez, Javier Flores-Fraile, Juan Manuel Ramírez, Bruno Macedo de Sousa, and Antonio López-Valverde. 2020. "Root Canal Morphology of the Permanent Mandibular Incisors by Cone Beam Computed Tomography: A Systematic Review" Applied Sciences 10, no. 14: 4914. https://0-doi-org.brum.beds.ac.uk/10.3390/app10144914






