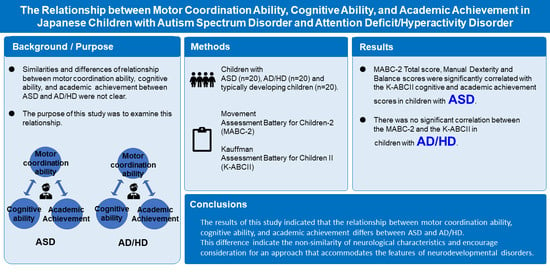
The Relationship between Motor Coordination Ability, Cognitive Ability, and Academic Achievement in Japanese Children with Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Instruments
2.3.1. Movement Assessment Battery for Children-2 (MABC-2)
2.3.2. The Japanese Version of the Kauffman Assessment Battery for Children-Second Edition (K-ABCII)
2.3.3. Autism Spectrum Screening Questionnaire (ASSQ)
2.3.4. Pervasive Developmental Disorders Autism Society Japan Rating Scale (PARS-TR)
2.3.5. ADHD Rating Scale-IV (ADHD RS-IV)
2.4. Statistical Analysis
3. Results
3.1. Motor Coordination Ability
3.2. Correlation between Motor Coordination Ability and Cognitive Ability/Academic Achievement
4. Discussion
4.1. Motor Coordination Ability
4.2. Correlation between Motor Coordination Ability and Cognitive Ability
4.3. Correlation between Motor Coordination Ability and Academic Achievement
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Saito, M.; Hirota, T.; Sakamoto, Y.; Adachi, M.; Takahashi, M.; Osato-Kaneda, A.; Kim, Y.S.; Leventhal, B.; Shui, A.; Kato, S.; et al. Prevalence and cumulative incidence of autism spectrum disorders and the patterns of co-occurring neurodevelopmental disorders in a total population sample of 5-year-old children. Mol. Autism 2020, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Kadesjö, B.; Gillberg, C. The Comorbidity of ADHD in the General Population of Swedish School-age Children. J. Child Psychol. Psychiatry Allied Discip. 2001, 42, 487–492. [Google Scholar] [CrossRef]
- van der Fels, I.M.J.; te Wierike, S.C.M.; Hartman, E.; Elferink-Gemser, M.T.; Smith, J.; Visscher, C. The relationship between motor skills and cognitive skills in 4–16 year old typically developing children: A systematic review. J. Sci. Med. Sport 2015, 18, 697–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asonitou, K.; Koutsouki, D.; Charitou, S. Motor skills and cognitive abilities as a precursor of academic performance in children with and without DCD. Procedia-Soc. Behav. Sci. 2010, 5, 1702–1707. [Google Scholar] [CrossRef] [Green Version]
- Macdonald, K.; Milne, N.; Orr, R.; Pope, R. Relationships between Motor Proficiency and Academic Performance in Mathematics and Reading in School-Aged Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 1603. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, V.R.; Ribeiro ML, S.; Melo, T.; de Tarso Maciel-Pinheiro, P.; Guimarães, T.T.; Araújo, N.B.; Ribeiro, S.; Deslandes, A.C. Motor coordination correlates with academic achievement and cognitive function in children. Front. Psychol. 2016, 7, 318. [Google Scholar] [CrossRef] [Green Version]
- Higashionna, T.; Iwanaga, R.; Tokunaga, A.; Nakai, A.; Tanaka, K.; Nakane, H.; Tanaka, G. Relationship between motor coordination, cognitive abilities, and academic achievement in Japanese children with neurodevelopmental disorders. Hong Kong J. Occup. Ther. 2017, 30, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Alloway, T.P. Working memory, reading, and mathematical skills in children with developmental coordination disorder. J. Exp. Child Psychol. 2007, 96, 20–36. [Google Scholar] [CrossRef] [Green Version]
- Pieters, S.; Desoete, A.; Van Waelvelde, H.; Vanderswalmen, R.; Roeyers, H. Mathematical problems in children with developmental coordination disorder. Res. Dev. Disabil. 2012, 33, 1128–1135. [Google Scholar] [CrossRef]
- Lukito, S.; Norman, L.; Carlisi, C.; Radua, J.; Hart, H.; Simonoff, E.; Rubia, K. Comparative meta-analyses of brain structural and functional abnormalities during cognitive control in attention-deficit/hyperactivity disorder and autism spectrum disorder. Psychol. Med. 2020, 50, 894–919. [Google Scholar] [CrossRef]
- Hirata, S.; Kita, Y.; Yasunaga, M.; Suzuki, K.; Okumura, Y.; Okuzumi, H.; Hosobuchi, T.; Kokubun, M.; Inagaki, M.; Nakai, A. Applicability of the Movement Assessment Battery for Children-Second Edition (MABC-2) for Japanese children aged 3–6 years: A preliminary investigation emphasizing internal consistency and factorial validity. Front. Psychol. 2018, 9, 1452. [Google Scholar] [CrossRef] [PubMed]
- Kita, Y.; Suzuki, K.; Hirata, S.; Sakihara, K.; Inagaki, M.; Nakai, A. Applicability of the Movement Assessment Battery for Children-Second Edition to Japanese children: A study of the Age Band 2. Brain Dev. 2016, 38, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.; Sugden, D.A.; Barnett, A.L. Movement Assessment Battery for Children-2, 2nd ed.; The Psychological Corporation: San Antonio, TX, USA, 2007; ISBN 978-0-7491-3608-6. [Google Scholar]
- Kaufman, A.S. Kaufman Assessment Battery for Children, (KABC-II); AGS Publishing: Circle Pines, MN, USA, 2004. [Google Scholar] [CrossRef] [Green Version]
- Posserud, M.B.; Lundervold, A.J.; Gillberg, C. Validation of the Autism Spectrum Screening Questionnaire in a Total Population Sample. J. Autism Dev. Disord. 2009, 39, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Tani, I.; Yukihiro, R.; Adachi, J.; Hara, K.; Ogasawara, M.; Inoue, M.; Kamio, Y.; Nakamura, K.; Uchiyama, T.; et al. Validation of an interview-based rating scale developed in Japan for pervasive developmental disorders. Res. Autism Spectr. Disord. 2012, 6, 1265–1272. [Google Scholar] [CrossRef]
- Green, D.; Charman, T.; Pickles, A.; Chandler, S.; Loucas, T.; Simonoff, E.; Baird, G. Impairment in movement skills of children with autistic spectrum disorders. Dev. Med. Child Neurol. 2009, 51, 311–316. [Google Scholar] [CrossRef]
- Whyatt, C.P.; Craig, C.M. Motor skills in children aged 7–10 years, diagnosed with autism spectrum disorder. J. Autism Dev. Disord. 2012, 42, 1799–1809. [Google Scholar] [CrossRef]
- Kadesjö, B.; Gillberg, C. Attention deficits and clumsiness in Swedish 7-year-old children. Dev. Med. Child Neurol. 1998, 40, 796–804. [Google Scholar] [CrossRef]
- Watemberg, N.; Waiserberg, N.; Zuk, L.; Lerman-Sagie, T. Developmental coordination disorder in children with attention-deficit-hyperactivity disorder and physical therapy intervention. Dev. Med. Child Neurol. 2007, 49, 920–925. [Google Scholar] [CrossRef]
- McAuliffe, D.; Pillai, A.S.; Tiedemann, A.; Mostofsky, S.H.; Ewen, J.B. Dyspraxia in ASD: Impaired coordination of movement elements. Autism Res. 2017, 10, 648–652. [Google Scholar] [CrossRef] [Green Version]
- Gizzonio, V.; Avanzini, P.; Campi, C.; Orivoli, S.; Piccolo, B.; Cantalupo, G.; Tassinari, C.A.; Rizzolatti, G.; Fabbri-Destro, M. Failure in Pantomime Action Execution Correlates with the Severity of Social Behavior Deficits in Children with Autism: A Praxis Study. J. Autism Dev. Disord. 2015, 45, 3085–3097. [Google Scholar] [CrossRef]
- MacNeil, L.K.; Mostofsky, S.H. Specificity of dyspraxia in children with autism. Neuropsychology 2012, 26, 165–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bramham, J.; Ambery, F.; Young, S.; Morris, R.; Russell, A.; Xenitidis, K.; Asherson, P.; Murphy, D. Executive functioning differences between adults with attention deficit hyperactivity disorder and autistic spectrum disorder in initiation, planning and strategy formation. Autism 2009, 13, 245–264. [Google Scholar] [CrossRef] [PubMed]
- Mostofsky, S.H.; Dubey, P.; Jerath, V.K.; Jansiewicz, E.M.; Goldberg, M.C.; Denckla, M.B. Developmental dyspraxia is not limited to imitation in children with autism spectrum disorders. J. Int. Neuropsychol. Soc. 2006, 12, 314–326. [Google Scholar] [CrossRef] [Green Version]
- Miller, M.; Chukoskie, L.; Zinni, M.; Townsend, J.; Trauner, D. Dyspraxia, motor function and visual-motor integration in autism. Behav. Brain Res. 2014, 269, 95–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corbett, B.A.; Constantine, L.J.; Hendren, R.; Rocke, D.; Ozonoff, S. Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Res. 2009, 166, 210–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartman, E.; Houwen, S.; Scherder, E.; Visscher, C. On the relationship between motor performance and executive functioning in children with intellectual disabilities. J. Intellect. Disabil. Res. 2010, 54, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Sinzig, J.; Morsch, D.; Bruning, N.; Schmidt, M.H.; Lehmkuhl, G. Inhibition, flexibility, working memory and planning in autism spectrum disorders with and without comorbid ADHD-symptoms. Child Adolesc. Psychiatry Ment. Health 2008, 2, 4. [Google Scholar] [CrossRef] [Green Version]
- Minshew, N.J.; Goldstein, G.; Taylor, H.G.; Siegel, D.J. Academic Achievement in High Functioning Autistic Individuals. J. Clin. Exp. Neuropsychol. 1994, 16, 261–270. [Google Scholar] [CrossRef]
- Miller, L.E.; Burke, J.D.; Troyb, E.; Knoch, K.; Herlihy, L.E.; Fein, D.A. Preschool predictors of school-age academic achievement in autism spectrum disorder. Clin. Neuropsychol. 2017, 31, 382–403. [Google Scholar] [CrossRef] [Green Version]
- De Smet, H.J.; Baillieux, H.; De Deyn, P.P.; Mariën, P.; Paquier, P. The cerebellum and language: The story so far. Folia Phoniatr. Logop. 2007, 59, 165–170. [Google Scholar] [CrossRef]
- Desmond, J.E.; Fiez, J.A. Neuroimaging studies of the cerebellum: Language, learning and memory. Trends Cogn. Sci. 1998, 2, 355–362. [Google Scholar] [CrossRef]
- Dinkel, P.J.; Willmes, K.; Krinzinger, H.; Konrad, K.; Koten, J.W. Diagnosing developmental dyscalculia on the basis of reliable single case FMRI methods: Promises and limitations. PLoS ONE 2013, 8, e83722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, P.; Weingart, D.; Bonner, T.; Watson, B.; Park, M.T.M.; Sharp, W.; Lerch, J.P.; Chakravarty, M.M. Defining the neuroanatomic basis of motor coordination in children and its relationship with symptoms of attention-deficit/hyperactivity disorder. Psychol. Med. 2016, 46, 2363–2373. [Google Scholar] [CrossRef] [PubMed]
- Polderman, T.J.C.; Huizink, A.C.; Verhulst, F.C.; van Beijsterveldt, C.E.M.; Boomsma, D.I.; Bartels, M. A genetic study on attention problems and academic skills: Results of a longitudinal study in twins. J. Can. Acad. Child Adolesc. Psychiatry 2011, 20, 22–34. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pmc/articles/PMC3024720/ (accessed on 1 April 2022). [PubMed]
- Schmiedeler, S.; Schneider, W. Attention-Deficit hyperactivity disorder (ADHD) in the early years: Diagnostic issues and educational relevance. Clin. Child Psychol. Psychiatry 2014, 19, 460–475. [Google Scholar] [CrossRef] [PubMed]
| ASD (n = 20) Mean (SD) | AD/HD (n = 20) Mean (SD) | t | p | |
|---|---|---|---|---|
| ASSQ | 22.0 (10.5) | 15.0 (8.8) | 2.28 | 0.03 * |
| PARS-TR | 23.1 (11.1) | 15.1 (8.9) | 2.48 | 0.02 * |
| ADHD RS-IV | 22.0 (9.9) | 23.9 (9.6) | −0.61 | 0.55 |
| K-ABCII Cognitive ability | ||||
| Sequential processing | 96.6 (16.7) | 84.8 (12.8) | 2.94 | <0.01 ** |
| Simultaneous processing | 101.0 (16.1) | 99.2 (12.2) | 0.40 | 0.69 |
| Planning | 105.0 (14.5) | 92.6 (15.8) | 2.59 | <0.01 ** |
| Learning | 107.0 (16.3) | 103.6 (13.9) | 0.72 | 0.48 |
| Total | 102.6 (15.8) | 92.0 (13.0) | 2.33 | 0.03 * |
| K-ABCII Academic achievement | ||||
| Knowledge | 101.8 (15.2) | 94.5 (12.5) | 1.65 | 0.11 |
| Reading | 101.6 (18.2) | 92.1 (15.0) | 1.80 | 0.08 |
| Writing | 97.3 (19.5) | 89.1 (18.0) | 1.34 | 0.19 |
| Arithmetic | 96.9 (15.9) | 93.4 (15.9) | 0.70 | 0.49 |
| Total | 99.7 (16.7) | 90.3 (16.9) | 1.77 | 0.08 |
| ASD (n = 20) Mean (SD) | AD/HD (n = 20) Mean (SD) | Typically Developing (n = 20) Mean (SD) | |
|---|---|---|---|
| Manual Dexterity | 9.2 (3.6) a | 10.5 (2.7) | 12.4 (3.0) |
| Aiming & Catching | 7.3 (3.5) a | 9.0 (3.0) | 10.8 (3.4) |
| Balance | 10.3 (3.5) a | 10.6 (2.6) b | 13.5 (1.9) |
| Total | 8.8 (3.4) a | 10.2 (2.6) b | 13.0 (2.4) |
| Sequential Processing | Simultaneous Processing | Planning | Learning | Total Cognitive Ability | |
|---|---|---|---|---|---|
| ASD | |||||
| Manual Dexterity | 0.07 | 0.58 ** | 0.65 ** | 0.32 | 0.51 * |
| Aiming & Catching | 0.03 | 0.27 | 0.10 | −0.11 | 0.11 |
| Balance | −0.02 | 0.34 | 0.41 | 0.36 | 0.36 |
| Total MABC-2 | 0.08 | 0.55 * | 0.55 ** | 0.29 | 0.49 * |
| AD/HD | |||||
| Manual Dexterity | 0.42 | 0.25 | 0.34 | 0.15 | 0.42 |
| Aiming & Catching | −0.18 | 0.09 | −0.14 | 0.01 | −0.09 |
| Balance | 0.26 | 0.29 | −0.08 | 0.14 | 0.23 |
| Total MABC-2 | 0.25 | 0.15 | 0.04 | 0.11 | 0.20 |
| Knowledge | Reading | Writing | Arithmetic | Total Academic Achievement | |
|---|---|---|---|---|---|
| ASD | |||||
| Manual Dexterity | 0.26 | 0.24 | 0.53 | 0.59 * | 0.52 |
| Aiming & Catching | −0.05 | 0.09 | 0.48 | 0.38 | 0.26 |
| Balance | −0.34 | 0.14 | 0.75 ** | 0.61 * | 0.31 |
| Total MABC-2 | −0.03 | 0.17 | 0.75 ** | 0.67 * | 0.46 |
| AD/HD | |||||
| Manual Dexterity | 0.35 | 0.10 | 0.33 | 0.22 | 0.26 |
| Aiming & Catching | −0.04 | −0.29 | −0.09 | −0.12 | −0.18 |
| Balance | 0.11 | −0.03 | 0.02 | 0.05 | 0.34 |
| Total MABC-2 | 0.17 | −0.04 | 0.14 | 0.06 | 0.07 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Higashionna, T.; Iwanaga, R.; Tokunaga, A.; Nakai, A.; Tanaka, K.; Tanaka, G. The Relationship between Motor Coordination Ability, Cognitive Ability, and Academic Achievement in Japanese Children with Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder. Brain Sci. 2022, 12, 674. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci12050674
Higashionna T, Iwanaga R, Tokunaga A, Nakai A, Tanaka K, Tanaka G. The Relationship between Motor Coordination Ability, Cognitive Ability, and Academic Achievement in Japanese Children with Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder. Brain Sciences. 2022; 12(5):674. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci12050674
Chicago/Turabian StyleHigashionna, Takuya, Ryoichiro Iwanaga, Akiko Tokunaga, Akio Nakai, Koji Tanaka, and Goro Tanaka. 2022. "The Relationship between Motor Coordination Ability, Cognitive Ability, and Academic Achievement in Japanese Children with Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder" Brain Sciences 12, no. 5: 674. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci12050674