Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
- the researchers’ University and/or hospitals’ emails and official websites and social media profiles (Facebook) of the following institutions: Medical University of Lodz, Central Teaching Hospital of the Medical University of Lodz, as well as University Hospital WAM-CSW
- social media profile of “Porozumienie Rezydentów”—one of the biggest organizations that gathers Polish HCWs
2.2. Measurement Tools
2.3. Data Collection
2.4. Sample Size Calculation and Statistical Analysis
3. Results
3.1. Study Group
3.2. Experiences with COVID-19 and the Related Anxiety
3.3. Vaccination-Related Experiences and Anxiety
3.4. Mental Well-Being According to the DASS-21 Questionnaire
3.5. Factors Influencing Pro-Vaccination Attitudes
4. Discussion
4.1. Attitude to the Risk Associated with SARS-CoV-2 Pandemic
4.2. Willingness to Get Vaccinated
4.3. Concerns about COVID-19 Vaccination and Conspiracy Theories
4.4. Factors Influencing Positive Attitudes towards Vaccination
4.5. Comparison between the Present and Previous Study on Medical and Non-Medical Students
5. Conclusions
6. Strength and Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lastrucci, V.; Lorini, C.; Del Riccio, M.; Gori, E.; Chiesi, F.; Sartor, G.; Zanella, B.; Boccalini, S.; Bechini, A.; Puggelli, F.; et al. SARS-CoV-2 Seroprevalence Survey in People Involved in Different Essential Activities during the General Lock-Down Phase in the Province of Prato (Tuscany, Italy). Vaccines 2020, 8, 778. [Google Scholar] [CrossRef] [PubMed]
- Khuroo, M.S.; Khuroo, M.; Khuroo, M.S.; Sofi, A.A.; Khuroo, N.S. COVID-19 Vaccines: A Race Against Time in the Middle of Death and Devastation! J. Clin. Exp. Hepatol. 2020, 10, 610–621. [Google Scholar] [CrossRef] [PubMed]
- Pfizer-BioNTech COVID-19 Vaccine Frequently Asked Questions|FDA. Available online: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/pfizer-biontech-covid-19-vaccine-frequently-asked-questions (accessed on 21 December 2020).
- Dini, G.; Toletone, A.; Sticchi, L.; Orsi, A.; Bragazzi, N.L.; Durando, P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum. Vaccin. Immunother. 2018, 14, 772–789. [Google Scholar] [CrossRef] [Green Version]
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical students and SARS-CoV-2 vaccination: Attitude and behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef] [PubMed]
- Bartoszek, A.; Walkowiak, D.; Bartoszek, A.; Kardas, G. Mental Well-Being (Depression, Loneliness, Insomnia, Daily Life Fatigue) during COVID-19 Related Home-Confinement—A Study from Poland. Int. J. Environ. Res. Public Health 2020, 17, 7417. [Google Scholar] [CrossRef] [PubMed]
- Power/Sample Size Calculator. Available online: https://www.stat.ubc.ca/~rollin/stats/ssize/b2.html (accessed on 5 February 2021).
- Rosner, B. Fundamentals of Biostatistics; Jaypee Brothers Medical Publishers (P) Ltd.: New Delhi, India, 2016; ISBN 9788180618147. [Google Scholar]
- Gabryelska, A.; Sochal, M.; Turkiewicz, S.; Białasiewicz, P. Relationship between HIF-1 and Circadian Clock Proteins in Obstructive Sleep Apnea Patients—Preliminary Study. J. Clin. Med. 2020, 9, 1599. [Google Scholar] [CrossRef]
- Sochal, M.; Małecka-Panas, E.; Gabryelska, A.; Talar-Wojnarowska, R.; Szmyd, B.; Krzywdzińska, M.; Białasiewicz, P. Determinants of Sleep Quality in Inflammatory Bowel Diseases. J. Clin. Med. 2020, 9, 2921. [Google Scholar] [CrossRef] [PubMed]
- Esprit, A.; de Mey, W.; Bahadur Shahi, R.; Thielemans, K.; Franceschini, L.; Breckpot, K. Neo-Antigen mRNA Vaccines. Vaccines 2020, 8, 776. [Google Scholar] [CrossRef]
- Zheng, C.; Hafezi-Bakhtiari, N.; Cooper, V.; Davidson, H.; Habibi, M.; Riley, P.; Breathnach, A. Characteristics and transmission dynamics of COVID-19 in healthcare workers at a London teaching hospital. J. Hosp. Infect. 2020, 106, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Hunter, E.; Price, D.A.; Murphy, E.; van der Loeff, I.S.; Baker, K.F.; Lendrem, D.; Lendrem, C.; Schmid, M.L.; Pareja-Cebrian, L.; Welch, A.; et al. First experience of COVID-19 screening of health-care workers in England. Lancet 2020, 395, e77–e78. [Google Scholar] [CrossRef]
- Di Martino, G.; Di Giovanni, P.; Di Girolamo, A.; Scampoli, P.; Cedrone, F.; D’Addezio, M.; Meo, F.; Romano, F.; Di Sciascio, M.B.; Staniscia, T. Knowledge and Attitude towards Vaccination among Healthcare Workers: A Multicenter Cross-Sectional Study in a Southern Italian Region. Vaccines 2020, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Kabamba Nzaji, M.; Kabamba Ngombe, L.; Ngoie Mwamba, G.; Banza Ndala, D.B.; Mbidi Miema, J.; Luhata Lungoyo, C.; Lora Mwimba, B.; Cikomola Mwana Bene, A.; Mukamba Musenga, E. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic Obs. Res. 2020, 11, 103–109. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus Disease (COVID-19) Dashboard|WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 5 February 2021).
- Sotgiu, G.; Dobler, C.C. Social stigma in the time of coronavirus disease 2019. Eur. Respir. J. 2020, 56, 2002461. [Google Scholar] [CrossRef]
- Iyengar, K.P.; Ish, P.; Upadhyaya, G.K.; Malhotra, N.; Vaishya, R.; Jain, V.K. COVID-19 and mortality in doctors. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1743–1746. [Google Scholar] [CrossRef]
- Shreffler, J.; Huecker, M.; Petrey, J. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West. J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. medRxiv 2020. [Google Scholar] [CrossRef]
- Pradhan, D.; Biswasroy, P.; Kumar Naik, P.; Ghosh, G.; Rath, G. A Review of Current Interventions for COVID-19 Prevention. Arch. Med. Res. 2020, 51, 363–374. [Google Scholar] [CrossRef]
- Georgiou, N.; Delfabbro, P.; Balzan, R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Pers. Individ. Dif. 2020, 166, 110201. [Google Scholar] [CrossRef]
- Duplaga, M. The Determinants of Conspiracy Beliefs Related to the COVID-19 Pandemic in a Nationally Representative Sample of Internet Users. Int. J. Environ. Res. Public Health 2020, 17, 7818. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, J.; Yang, Y.; Wang, Z.; Wang, G.; Hashimoto, K.; Zhang, K.; Liu, H. Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID-19. Brain Behav. Immun. Health 2020, 4, 100064. [Google Scholar] [CrossRef]
- Bagcchi, S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020, 20, 782. [Google Scholar] [CrossRef]
- Pierwszy Miesiąc Szczepień Przeciw Covid-19 za Nami—Szczepienie Przeciwko COVID-19—Portal Gov.pl. Available online: https://www.gov.pl/web/szczepimysie/pierwszy-miesiac-szczepien-przeciw-covid-19-za-nami?fbclid=IwAR0C77xsqDP9nLJeAOSdDmehlJFq0wKBZBBTRXm3gBcM0VVfCLl7T7mIhrU (accessed on 5 February 2021).
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020, 1. [Google Scholar] [CrossRef] [PubMed]
- Feleszko, W.; Lewulis, P.; Czarnecki, A.; Waszkiewicz, P. Flattening the Curve of COVID-19 Vaccine Rejection—An International Overview. Vaccines 2021, 9, 44. [Google Scholar] [CrossRef]
- Narodowy Program Szczepień Przeciw COVID-19—Szczepienie Przeciwko COVID-19—Portal Gov.pl. Available online: https://www.gov.pl/web/szczepimysie/narodowy-program-szczepien-przeciw-covid-19 (accessed on 5 February 2021).
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Groenewoud, R.; Rachor, G.S.; Asmundson, G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020, 11, 575950. [Google Scholar] [CrossRef]
- Davidson, M. Vaccination as a cause of autism—myths and controversies. Dialogues Clin. Neurosci. 2017, 19, 403–407. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 1–8. [Google Scholar] [CrossRef]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef] [PubMed]
- Jolley, D.; Paterson, J.L. Pylons ablaze: Examining the role of 5G COVID-19 conspiracy beliefs and support for violence. Br. J. Soc. Psychol. 2020, 59, 628–640. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Waite, F.; Rosebrock, L.; Petit, A.; Causier, C.; East, A.; Jenner, L.; Teale, A.-L.; Carr, L.; Mulhall, S.; et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, B.L.; Felter, E.M.; Chu, K.H.; Shensa, A.; Hermann, C.; Wolynn, T.; Williams, D.; Primack, B.A. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook. Vaccine 2019, 37, 2216–2223. [Google Scholar] [CrossRef] [PubMed]
- Pivetti, M.; Melotti, G.; Mancini, C. Vaccines and autism: A preliminary qualitative study on the beliefs of concerned mothers in Italy. Int. J. Qual. Stud. Health Well-Being 2020, 15, 1754086. [Google Scholar] [CrossRef] [Green Version]
- Kata, A. A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine 2010, 28, 1709–1716. [Google Scholar] [CrossRef]
- Goertzel, T. Conspiracy theories in science. EMBO Rep. 2010, 11, 493–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef] [PubMed]
- Michno, D.A.; Tan, J.; Adelekan, A.; Konczalik, W.; Woollard, A.C.S. How can we help? Medical students’ views on their role in the COVID-19 pandemic. J. Public Health 2021, 1–11. [Google Scholar] [CrossRef]
- Szmyd, B.; Rogut, M.; Białasiewicz, P.; Gabryelska, A. The impact of glucocorticoids and statins on sleep quality. Sleep Med. Rev. 2021, 55, 101380. [Google Scholar] [CrossRef]
| Healthcare Workers | Control Group | p-Value | |||
|---|---|---|---|---|---|
| Doctors | Administrative | Total | |||
| Total; n | 252 (10.96%) | 135 (5.87%) | 387 | 1913 (83.17%) | Not applicable |
| Male; n (%) | 71 (28.17%) | 51 (37.78%) | 122 (31.52%) | 1208 (63.15%) |
p
< 0.001
*, *, *, * |
| Mean age |
29.87 (SD = 6.99) |
34.26 (SD = 9.97) |
31.39 (SD = 8.42) | 26.94 (SD = 9.05) |
p
< 0.001
*, *, -, * |
| Healthcare Workers n (%) | Control Group n (%) | p-Value | |||
|---|---|---|---|---|---|
| Doctors | Administrative | Total | |||
| Previous SARS-CoV-2 infection | 54 (21.43%) | 9 (6.67%) | 63 (16.28%) | 159 (8.31%) | <0.001 *, -, *, * |
| Tested for SARS-CoV-2 | 188 (74.60%) | 43 (31.85%) | 231 (59.69%) | 418 (21.85%) | <0.001 *, *, *, * |
| Tested for SARS-CoV-2 ^: PCR: | |||||
| Nose | 89 (35.32%) | 17 (12.59%) | 106 (27.39%) | 126 (6.59%) | <0.001 *, *, *, * |
| Mouth | 34 (13.49%) | 6 (4.44%) | 40 (10.34%) | 79 (4.13%) | <0.001 *, -, *, * |
| Mouth and nose | 77 (30.56%) | 16 (11.85%) | 93 (24.03%) | 150 (7.84%) | <0.001 *, -, *, * |
| Quick antigen test | 40 (15.87%) | 7 (5.19%) | 47 (12.14%) | 51 (2.67%) | <0.001 *, -, *, * |
| ELISA | 35 (13.89%) | 10 (7.41%) | 45 (11.63%) | 60 (3.14%) | <0.001 *, *, -, * |
| Family member with confirmed SARS-CoV-2 infection | 170 (67.46%) | 69 (51.11%) | 239 (61.76%) | 1047 (54.73%) | <0.001 *, -, *, - |
| Family member deceased in the course of COVID-19 | 16 (6.35%) | 4 (2.96%) | 20 (5.17%) | 122 (6.38%) | 0.362 |
| How often do you visit elderly family members: | |||||
| Never | 56 (22.22%) | 25 (18.52%) | 81 (20.93%) | 354 (18.5%) | 0.413 |
| <1×/month | 102 (40.48%) | 46 (34.07%) | 148 (38.24%) | 653 (34.13%) | 0.130 |
| 1–2×/month | 52 (20.63%) | 19 (14.07%) | 71 (18.35%) | 369 (19.29%) | 0.428 |
| 3–10×/month | 30 (11.9%) | 27 (20.00%) | 57 (14.73%) | 303 (15.84%) | 0.178 |
| >10×/month | 10 (3.97%) | 17 (12.59%) | 27 (6.98%) | 213 (11.13%) | <0.001 *, -, *, * |
| Fear of contracting SARS-CoV-2 on a 10-point scale: | |||||
| General | 6 (3–7) | 5 (3–7) | 5 (3–7) | 4 (2–6) | <0.001 *, *, -, * |
| After illness | 5 (3–7) | 4 (2–6) | 5 (3–6.25) | 3 (2–5) | 0.151 |
| Main COVID-19-related concerns ^ | |||||
| Health or academic problems | 62 (24.60%) | 24 (17.78%) | 86 (22.22%) | 329 (17.20%) | 0.008 *, -, -, * |
| Health deterioration | 143 (56.75%) | 71 (52.59%) | 214 (55.30%) | 842 (44.01%) | <0.001 *, -, -, * |
| Post-COVID syndrome | 124 (49.21%) | 62 (45.93%) | 186 (48.06%) | 855 (44.69%) | 0.407 |
| Health deterioration in family members | 184 (73.02%) | 88 (65.19%) | 272 (70.28%) | 1069 (55.88%) | <0.001 *, *, -, * |
| Social stigma | 5 (1.98%) | 7 (5.19%) | 12 (3.10%) | 159 (8.31%) | <0.001 *, *, -, * |
| How concerned are you about passing on the disease to your relatives on a scale of 0–10? | |||||
| Overall | 8 (7–9) | 7 (4–8) | 8 (6–9) | 6 (3–8) | <0.001 *, -, *, * |
| After recovering from COVID | 2 (0–3) | 2 (2–4) | 2 (0.5–3) | 4 (1–7) | <0.001 *, -, -, * |
| Healthcare Workers | Control Group | p-Value | |||
|---|---|---|---|---|---|
| Doctors | Administrative | Total | |||
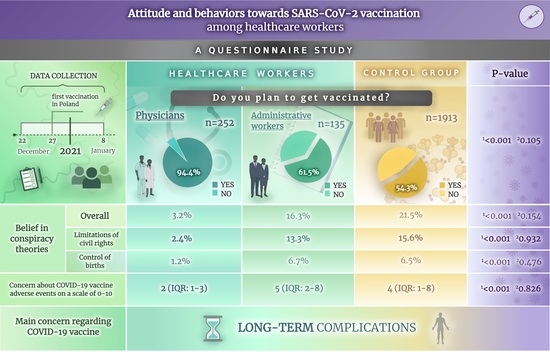
| Do you plan to get vaccinated? | |||||
| Yes—overall | 238 (94.44%) | 83 (61.48%) | 321 (82.95%) | 1039 (54.31%) | <0.001 *, -, *, * |
| As soon as possible | 223 (88.49%) | 62 (45.93%) | 285 (73.64%) | 561 (29.33%) | <0.001 *, *, *, * |
| At some point in the future | 15 (5.95%) | 21 (15.56%) | 36 (9.30%) | 478 (24.99%) | <0.001 *, *, *, * |
| No | 14 (5.56%) | 52 (38.52%) | 66 (17.05%) | 873 (45.64%) | <0.001 *, -, *, * |
| I do not know | 3 (1.19%) | 20 (14.81) | 23 (5.94%) | 380 (19.86%) | <0.001 *, -, *, * |
| How much are you worried about vaccination side effects on a scale of 0–10? | |||||
| Overall | 2 (1–3) | 5 (2–8) | 2 (1–5) | 4 (1–8) | <0.001 *, -, *, * |
| After previous SARS-CoV-2 infection | 2 (0–3) | 2 (2–4) | 2 (0.5–3) | 4 (1–7) | <0.001 *, *, -, * |
| What concerns you the most about getting vaccination? ^ | |||||
| Severe hypersensitivity reaction | 26 (10.32%) | 10 (7.41%) | 36 (9.30%) | 141 (7.37%) | 0.280 |
| Fever and malaise | 34 (13.49%) | 24 (17.78%) | 58 (14.99%) | 247 (12.91%) | 0.332 |
| Swelling and reddening around point of injection | 13 (5.16%) | 6 (4.44%) | 19 (4.91%) | 106 (5.54%) | 0.914 |
| Long-term complications | 81 (32.14%) | 60 (44.44%) | 141 (36.43%) | 847 (44.28%) | <0.001 *, -, *, * |
| Conspiracy theories (overall): | 8 (3.17%) | 22 (16.3%) | 30 (7.75%) | 411 (21.48%) | <0.001 *, -, *, * |
| Microchip injection | 0 (0%) | 5 (3.7%) | 5 (1.29%) | 127 (6.64%) | <0.001 *, -, *, * |
| Belief that herd immunity does not exist | 2 (0.79%) | 3 (2.22%) | 5 (1.29%) | 59 (3.08%) | 0.051 |
| Limitation of civil rights | 6 (2.38%) | 18 (13.33%) | 24 (6.2%) | 299 (15.63%) | <0.001 *, -, *, * |
| Control of births by vaccine manufacturers | 3 (1.19%) | 9 (6.67%) | 12 (3.10%) | 124 (6.48%) | <0.001 *, -, *, * |
| Autism | 0 (0%) | 8 (5.93%) | 8 (2.07%) | 80 (4.18%) | 0.003 *, -, *, - |
| Have you ever experienced any vaccination side effects? | 63 (25%) | 20 (14.81%) | 83 (21.45%) | 267 (13.96%) | <0.001 *, -, -, * |
| If so, which one of the following ^: | |||||
| Local reaction | 53 (21.03%) | 13 (6.63%) | 66 (17.05%) | 131 (6.85%) | <0.001 *, -, -, * |
| Fever, malaise | 40 (15.87%) | 12 (8.89%) | 52 (13.44%) | 171 (8.94%) | <0.001 *, -, -, * |
| Severe reaction | 0 (0%) | 2 (1.48%) | 2 (0.52%) | 16 (0.84%) | 0.623 |
| Long-term side effects | 0 (0%) | 3 (2.22%) | 3 (0.78%) | 30 (1.57%) | 0.256 |
| Has anyone from your family experienced any side effects of vaccines? | 69 (27.38%) | 28 (20.74%) | 97 (25.06%) | 360 (18.82%) | 0.001 *, -, -, * |
| If so, which one of the following ^: | |||||
| Local reaction | 52 (20.63%) | 14 (10.37%) | 66 (17.05%) | 137 (7.16%) | <0.001 *, -, *, * |
| Fever, malaise | 51 (20.24%) | 18 (13.33%) | 69 (17.83%) | 219 (11.45%) | <0.001 *, -, -, * |
| Severe reaction | 4 (1.53%) | 6 (4.44%) | 10 (2.58%) | 56 (2.93%) | 0.416 |
| Long-term side effects | 1 (0.40%) | 5 (3.7%) | 6 (1.55%) | 57 (2.98%) | 0.040 *, -, *, - |
| Past medical history of mandatory vaccinations: | Complete vs. rest <0.001 *, -, *, * | ||||
| Complete | 248 (98.41%) | 116 (85.93%) | 364 (96.06%) | 1685 (88.08%) | |
| Incomplete | 4 (1.59%) | 14 (10.37%) | 18 (4.65%) | 201 (10.51%) | |
| None | 0 (0%) | 5 (3.7%) | 5 (1.29%) | 27 (1.41%) | |
| Past medical history of recommended vaccinations, n (%) | 195 (77.38%) | 40 (29.63%) | 235 (60.72%) | 598 (31.26%) | <0.001 *, -, *, * |
| Healthcare Workers | Control Group | p-Value | |||
|---|---|---|---|---|---|
| Doctors | Administrative | Total | |||
| Depression | 5 (2–9) | 5 (2–9) | 6 (3–13) | 4 (2–9) | <0.001 *, *, -, * |
| Anxiety | 3 (1–6) | 3 (1–6) | 3 (1–6) | 2 (1–5) | 0.633 |
| Stress | 6 (3.5–10.5) | 6 (4–11) | 6 (3–11) | 7 (4–12) | 0.640 |
| OR | 95%CI | p-Value | |
|---|---|---|---|
| Intercept | 0.537 | 0.463–0.622 | <0.001 |
| Depression | 0.973 | 0.953–0.992 | 0.008 |
| Anxiety | 0.984 | 0.954–1.013 | 0.280 |
| Stress | 1.049 | 1.022–1.075 | <0.001 |
| Binary Logistic Regression Model | |||
|---|---|---|---|
| OR | 95%CI | p-Value | |
| Intercept | 1.049 | 0.527–2.088 | 0.891 |
| Sex (male) | 0.890 | 0.631–1.255 | 0.508 |
| Family member with confirmed SARS-CoV-2 infection (Yes) | 1.281 | 0.925–1.771 | 0.135 |
| Family member deceased in the course of COVID-19 (Yes) | 0.807 | 0.388–1.675 | 0.566 |
| Past medical history of recommended vaccinations (Yes) | 2.082 | 1.453–2.982 | <0.001 |
| Age (years) | 1.013 | 0.997–1.029 | 0.095 |
| The fear of COVID-19 (0–10) | 1.560 | 1.429–1.701 | <0.001 |
| The fear of passing on the disease to relatives (0–10) | 1.306 | 1.219–1.398 | <0.001 |
| The fear of vaccination side-effects (0–10) | 0.564 | 0.531–0.598 | <0.001 |
| Depression | 1.050 | 1.011–1.089 | 0.011 |
| Stress | 0.964 | 0.923–1.006 | 0.096 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines 2021, 9, 218. https://0-doi-org.brum.beds.ac.uk/10.3390/vaccines9030218
Szmyd B, Karuga FF, Bartoszek A, Staniecka K, Siwecka N, Bartoszek A, Błaszczyk M, Radek M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines. 2021; 9(3):218. https://0-doi-org.brum.beds.ac.uk/10.3390/vaccines9030218
Chicago/Turabian StyleSzmyd, Bartosz, Filip Franciszek Karuga, Adrian Bartoszek, Katarzyna Staniecka, Natalia Siwecka, Agnieszka Bartoszek, Maciej Błaszczyk, and Maciej Radek. 2021. "Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland" Vaccines 9, no. 3: 218. https://0-doi-org.brum.beds.ac.uk/10.3390/vaccines9030218