Kidney Function as a Determinant of HDL and Triglyceride Concentrations in the Australian Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Laboratory Methods
2.3. Data Preparation and Analysis
3. Results
3.1. Patient Characteristics
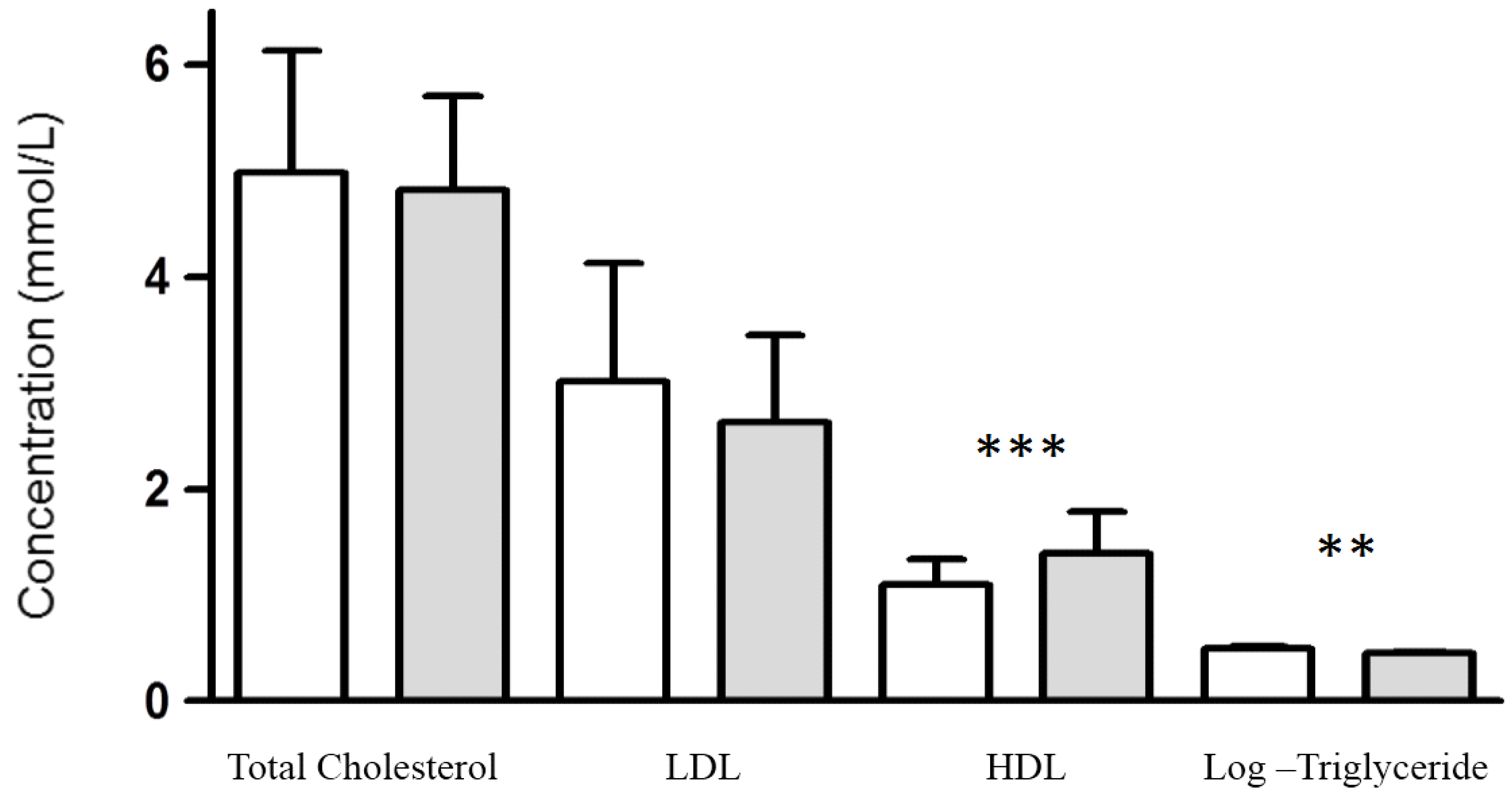
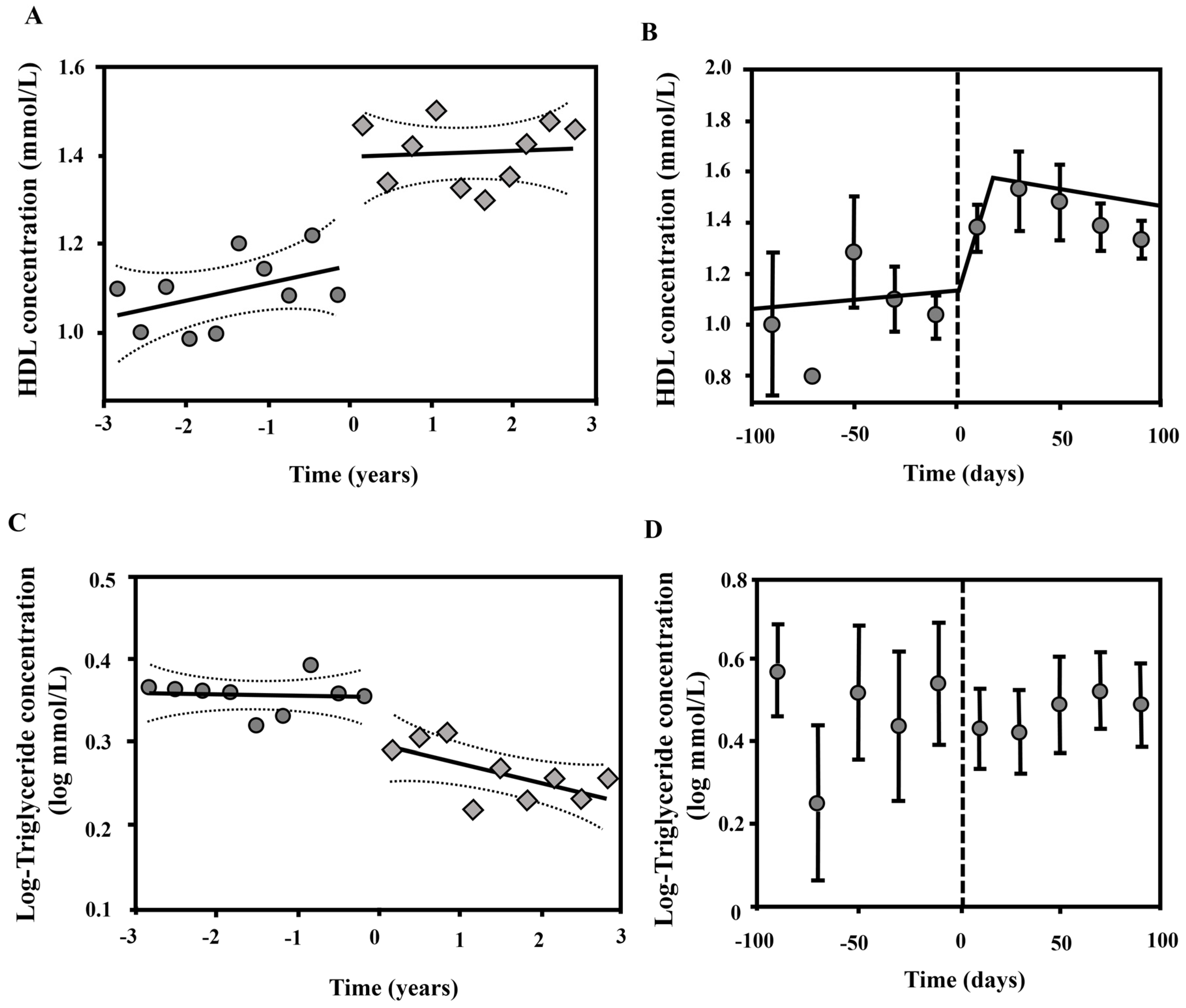
3.2. Effect of Kidney Function on Plasma Lipoprotein Concentrations
4. Discussion
Author Contributions
Conflicts of Interest
Abbreviations
| CKD | Chronic kidney disease |
| CVD | Cardiovascular disease |
| eGFR | Estimated glomerular filtration rate |
| ESKD | End stage kidney disease |
| HDL | High density lipoprotein |
| LDL | Low density lipoprotein |
References
- Meguid El Nahas, A.; Bello, A.K. Chronic kidney disease: The global challenge. Lancet 2005, 365, 331–340. [Google Scholar] [PubMed]
- Chadban, S.J.; Briganti, E.M.; Kerr, P.G.; Dunstan, D.W.; Welborn, T.A.; Zimmet, P.Z.; Atkins, R.C. Prevalence of kidney damage in Australian adults: The AusDiab kidney study. J. Am. Soc. Nephrol. 2003, 14, S131–S138. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- Meier-Kriesche, H.U.; Schold, J.D.; Srinivas, T.R.; Reed, A.; Kaplan, B. Kidney transplantation halts cardiovascular disease progression in patients with end-stage renal disease. Am. J. Transplant. 2004, 4, 1662–1668. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, R.A.; Ashby, V.B.; Milford, E.L.; Ojo, A.O.; Ettenger, R.E.; Agodoa, L.Y.; Held, P.J.; Port, F.K. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 1999, 341, 1725–1730. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; He, J.; Astor, B.C.; Folsom, A.R.; Coresh, J. Traditional and nontraditional risk factors predict coronary heart disease in chronic kidney disease: Results from the atherosclerosis risk in communities study. J. Am. Soc. Nephrol. 2005, 16, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Magnus, P.; Beaglehole, R. The real contribution of the major risk factors to the coronary epidemics: Time to end the “only-50%” myth. Arch. Intern. Med. 2001, 161, 2657–2660. [Google Scholar] [CrossRef] [PubMed]
- Sarnak, M.J.; Coronado, B.E.; Greene, T.; Wang, S.R.; Kusek, J.W.; Beck, G.J.; Levey, A.S. Cardiovascular disease risk factors in chronic renal insufficiency. Clin. Nephrol. 2002, 57, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Kwan, B.C.; Kronenberg, F.; Beddhu, S.; Cheung, A.K. Lipoprotein metabolism and lipid management in chronic kidney disease. J. Am. Soc. Nephrol. 2007, 18, 1246–1261. [Google Scholar] [CrossRef] [PubMed]
- Muntner, P.; Coresh, J.; Smith, J.C.; Eckfeldt, J.; Klag, M.J. Plasma lipids and risk of developing renal dysfunction: The atherosclerosis risk in communities study. Kidney Int. 2000, 58, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D. Dyslipidemia of chronic renal failure: The nature, mechanisms, and potential consequences. Am. J. Physiol. Renal Physiol. 2006, 290, F262–F272. [Google Scholar] [CrossRef] [PubMed]
- Bergmeyer, H.U.; Scheibe, P.; Wahlefeld, A.W. Optimization of methods for aspartate aminotransferase and alanine aminotransferase. Clinical. Chem. 1978, 24, 58–73. [Google Scholar]
- Keyser, J.W. Rapid estimation of albumin and total protein in small amounts of blood serum. Clin. Chem. Acta 1962, 7, 299–300. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [PubMed]
- Rikitake, K.; Oka, I.; Makoto, A.N.D.O.; Yoshimoto, T.; Tsuru, D. Creatinine Amidohydrolase (Creatininase) from Pseudomonas putida. Purification and some properties. J. Biochem. 1979, 86, 1109–1117. [Google Scholar]
- Klotzsch, S.G.; McNamara, J.R. Triglyceride measurements: A review of methods and interferences. Clin. Chem. 1990, 36, 1605–1613. [Google Scholar] [PubMed]
- Wearne, J.T. A note on urea estimation by diacetyl monoxime. J. Clin. Pathol. 1958, 11, 367. [Google Scholar] [CrossRef] [PubMed]
- Widdowson, G.M.; Penton, J.R. Determination of serum or plasma glucose on the “AutoAnalyzer II” by use of the hexokinase reaction. Clin. Chem. 1972, 18, 299–300. [Google Scholar] [PubMed]
- Blum, C.B.; Levy, R.I.; Eisenberg, S.; Hall, M., III; Goebel, R.H.; Berman, M. High density lipoprotein metabolism in man. J. Clin. Investig. 1977, 60, 795–807. [Google Scholar] [CrossRef] [PubMed]
- Manitpisitkul, W.; McCann, E.; Lee, S.; Weir, M.R. Drug interactions in transplant patients: What everyone should know. Curr. Opin. Nephrol. Hypertens. 2009, 18, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Aker, S.; Ivens, K.; Grabensee, B.; Heering, P. Cardiovascular risk factors and diseases after renal transplantation. Int. Urol. Nephrol. 1998, 30, 777–788. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D.; Moradi, H. Mechanisms of dyslipidemia of chronic renal failure. Hemodial. Int. 2006, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Harper, C.R.; Jacobson, T.A. Managing dyslipidemia in chronic kidney disease. J. Am. Coll. Cardiol. 2008, 51, 2375–2384. [Google Scholar] [CrossRef] [PubMed]
- Rosenson, R.S. Functional assessment of HDL: Moving beyond static measures for risk assessment. Cardiovasc. Drugs Ther. 2011, 24, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Tchernof, A.; Moorjani, S.; Cantin, B.; Dagenais, G.R.; Lupien, P.J.; Després, J.P. Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men. Prospective results from the Quebec Cardiovascular Study. Circulation 1997, 95, 69–75. [Google Scholar] [CrossRef] [PubMed]

| Risk Factor | eGFR (mL/min/1.73 m2) | p Trend | |||
|---|---|---|---|---|---|
| >60 | 30–60 | 15–30 | <15 | ||
| Diabetes mellitus (%) | 21.6 | 37.6 | 35.8 | 32.8 | ns |
| Hypertension (%) | 42.1 | 70.5 | 69.6 | 69.1 | <0.0001 |
| Smoking | |||||
| Current (%) | 10.8 | 22.0 | 8.8 | 15.1 | ns |
| Former (%) | 17.2 | 44.4 | 33.3 | 21.1 | ns |
| Total cholesterol (mmol/L) | 4.99 ± 1.36 | 4.96 ± 2.04 | 4.36 ± 1.46 | 4.26 ± 1.10 | <0.0001 |
| LDL (mmol/L) | 2.99 ± 1.07 | 2.88 ± 1.48 | 2.42 ± 1.28 | 2.33 ± 0.87 | <0.0001 |
| HDL (mmol/L) | 1.21 ± 0.39 | 1.10 ± 0.37 | 1.01 ± 0.37 | 1.02 ± 0.28 | <0.0001 |
| log-Triglycerides (log-mmol/L) | 0.40 ± 0.14 | 0.43 ± 0.14 | 0.47 ± 0.14 | 0.48 ± 0.12 | <0.0001 |
| Serum albumin (g/L) | 35.6 ± 6.0 | 34.9 ± 6.9 | 32.6 ± 7.8 | 33.5 ± 4.5 | 0.006 |
| Medication use | |||||
| Statin (%) | 27.5 | 33.8 | 46.1 | 81.3 | <0.0001 |
| Fibrate (%) | 2.0 | 2.5 | 2.9 | 2.0 | ns |
| Ezetimibe (%) | 0.9 | 3.4 | 1.5 | 2.0 | ns |
| Age (years) | 51.1 |
| Gender (M/F) | 36/24 |
| Hypertension (%) | 95.0 |
| Diabetes mellitus (%) | 33.3 |
| Smoking | |
| Former (%) | 20.0 |
| Current (%) | 8.3 |
| Lipid lowering | |
| Statin (%) | 95.0 |
| Fibrates (%) | 0.0 |
| Ezetimibe (%) | 1.6 |
| Immunosuppressant | |
| Predniosolone (%) | 98.3 |
| Mycophenolate (%) | 96.7 |
| Tacrolimus (%) | 81.7 |
| Cyclosporin (%) | 11.7 |
| Sirolimus (%) | 4.0 |
| Azathiopurine (%) | 4.0 |
| Lefluonamide (%) | 2.0 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, M.; Ray, U.; Yu, R.; Hudspeth, A.; Smillie, M.; Jordan, N.; Bartle, J. Kidney Function as a Determinant of HDL and Triglyceride Concentrations in the Australian Population. J. Clin. Med. 2016, 5, 35. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm5030035
Thompson M, Ray U, Yu R, Hudspeth A, Smillie M, Jordan N, Bartle J. Kidney Function as a Determinant of HDL and Triglyceride Concentrations in the Australian Population. Journal of Clinical Medicine. 2016; 5(3):35. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm5030035
Chicago/Turabian StyleThompson, Michael, Udayan Ray, Richard Yu, Andrew Hudspeth, Michael Smillie, Neville Jordan, and Janet Bartle. 2016. "Kidney Function as a Determinant of HDL and Triglyceride Concentrations in the Australian Population" Journal of Clinical Medicine 5, no. 3: 35. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm5030035





