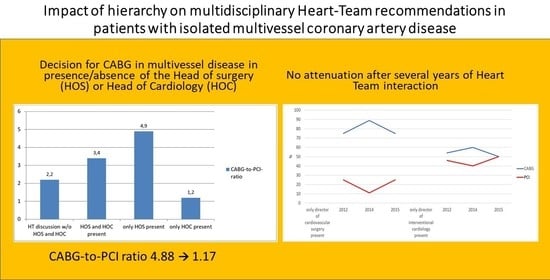
Impact of Hierarchy on Multidisciplinary Heart-Team Recommendations in Patients with Isolated Multivessel Coronary Artery Disease
Abstract
:1. Introduction
2. Methods
Statistical Analysis
3. Results
Application of the American College of Cardiology “Appropriate Use Criteria” and “SYNTAX Score II”
4. Discussion
4.1. Implications for Daily Practice
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviation
| CAD | coronary artery disease |
| CABG | coronary artery bypass grafting |
| PCI | percutaneous coronary intervention |
| HT | heart team |
| SYNTAX | SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery |
References
- Yadava, O.P. Heart team concept—A reality or a platonic illusion. Indian Heart J. 2017, 9, 681–683. [Google Scholar] [CrossRef] [PubMed]
- Kesson, E.M. Effects of a multidisciplinary team working on breast cancer survival. Br. Med. J. 2012, 344, e2718. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Kaul, S.; Mack, M. The rationale for heart-team decision-making for patients with stable, complex coronary artery disease. Eur. Heart J. 2013, 32, 2510–2518. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Calhoon, J.H.; Dehmer, G.J. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients with Stable Ischemic Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 2017, 69, 2212–2241. [Google Scholar] [PubMed]
- Long, J.; Luckraz, H.; Thekkudan, J.; Maher, A.; Norell, M. Heart team discussion in managing patients with coronary artery disease: Outcome and reproducibility. Interact. Cardiovasc. Thorac. Surg. 2012, 14, 594–598. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.K.; Luckraz, H.; Aktuerk, D. How does the ‘Heart Team’ decision get enacted for patients with coronary artery disease? Heart Asia 2014, 6, 31–33. [Google Scholar] [CrossRef]
- Ohlow, M.A.; Farah, A.; Kuntze, T.; Lauer, B. Patients’ preferences for coronary bypass grafting or staged percutaneous coronary intervention in multi-vessel coronary artery disease. Int. J. Clin. Pract. 2018, 72, e13056. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.; Morice, M.C.; Kappetein, A.P. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Kolbe, M.; Grande, B.; Marty, A. Making Heart Team discussions work. Struct. Heart 2019, 3, 100–103. [Google Scholar] [CrossRef]
- Farooq, V.; van Klaveren, D.; Steyerberg, E.W. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: Development and validation of SYNTAX score II. Lancet 2013, 381, 639–650. [Google Scholar] [CrossRef]
- Gulati, R.; Rihal, C.S. The SYNTAX trial: A perspective. Circ. Cardiovasc. Interv. 2009, 2, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Kappetein, A.P.; Dawkins, K.D.; Mohr, F.W. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease: Insights from the SYNTAX run-in phase. Eur. J. Cardiothorac. Surg. 2006, 4, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Health at a Glance-2015. OECD Indicators. Available online: http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm (accessed on 28 November 2018).
- Ko, D.T.; Tu, J.V.; Samadashvili, Z. Temporal trends in the use of percutaneous coronary intervention and coronary artery bypass surgery in New York State and Ontario. Circulation 2010, 121, 2635–2644. [Google Scholar] [CrossRef] [PubMed]
- Denvir, M.A.; Pell, J.P.; Lee, A.J. Variations in clinical decision-making between cardiologists and cardiac surgeons; a case for management by multidisciplinary teams? J. Cardiothorac. Surg. 2006, 1, 2. [Google Scholar] [CrossRef]
- Kahan, J.P.; Park, R.E.; Leape, L.L.; Bernstein, S.J.; Hilborne, L.H.; Parker, L.; Brook, R.H. Variations by specialty in physicians’ ratings of the appropriateness and necessity of indications for procedures. Med. Care 1996, 34, 512–523. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekharan, D.P.; Taggart, D.P. Informed consent for interventions in stable coronary artery disease: Problems, etiologies, and solutions. Eur. J. Cardiothorac. Surg. 2011, 39, 912–917. [Google Scholar] [CrossRef] [PubMed]
- Milne, J.; Greenfield, D.; Braithwaite, J. An ethnographic investigation of junior doctors’ capacities to practice interprofessionally in three teaching hospitals. J. Interprof. Care 2015, 29, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J.; Clay-Williams, R.; Vecellio, E. The basis of clinical tribalism, hierarchy and stereotyping: A laboratory-controlled teamwork experiment. BMJ Open 2016, 6, e012467. [Google Scholar] [CrossRef] [PubMed]
- Tajik, P.; Rengerink, K.O.; Mol, B.W.; Bossuyt, P.M. SYNTAX II score. Lancet 2013, 381, 1899. [Google Scholar] [CrossRef]
- Thuijs, D.F.; Kappetein, A.P.; Serruys, P.; Mohr, P.W.; Morice, M.C.; Mack, M.J.; Holmes, D.R., Jr.; Curzen, P.N.; Davierwala, P.; Noack, T.; et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicenter randomized controlled SYNTAX trial. Lancet 2019. [Google Scholar] [CrossRef]
- Meyer, E. Being the Boss in Brussels, Boston and Beijing. Available online: https://hbr.org/2017/07/being-the-boss-in-brussels-boston-and-beijing (accessed on 4 April 2019).




| Variable | HOS Present (n = 54) | HOC Present (n = 38) | HOC and HOS Present (n = 24) | Neither HOC nor HOS Present (n = 85) | p-Value |
|---|---|---|---|---|---|
| Age (years) | 70.1 ± 9.6 | 69.3 ± 9.1 | 70.9 ± 10.1 | 70.5 ± 8.9 | 0.87 |
| Male | 43 (79.6) | 34 (89.5) | 19 (79.2) | 69 (81.2) | 0.61 |
| Comorbidities | |||||
| Body-mass-index (kg/m2) | 28 ± 8.3 | 28 ± 4.6 | 31.4 ± 7.1 | 29.6 ± 7.2 | 0.69 |
| Hypertension requiring therapy | 36 (66.7) | 31 (81.6) | 17 (70.8) | 65 (79.3) | 0.54 |
| Active cigarette smoking | 4 (7.4) | 12 (31.6) | 4 (16.7) | 26 (30.6) | 0.006 |
| Hyperlipidemia | 14 (25.9) | 22 (57.9) | 13 (54.2) | 36 (42.4) | 0.01 |
| History of cardiac surgery | 3 (5.6) | 4 (10.5) | 2 (8.3) | 10 (11.8) | 0.67 |
| History of PCI | 8 (14.8) | 13 (34.2) | 15 (60.0) | 18 (21.2) | <0.001 |
| PAD | 18 (33.3) | 10 (26.3) | 3 (12.5) | 10 (11.8) | 0.01 |
| Chronic renal dysfunction | 8 (14.8) | 5 (13.2) | 4 (16.7) | 10 (11.8) | 0.92 |
| COPD | 1 (1.9) | 4 (10.5) | 1 (4.2) | 7 (8.2) | 0.77 |
| History of stroke/TIA | 4 (7.4) | 2 (5.3) | 1 (4.2) | 3 (3.5) | 0.49 |
| LV-EF (%) | 54 ± 9.9 | 51 ± 13 | 49.4 ± 14.8 | 48.9 ± 13.7 | 0.08 |
| Variable | HOS Present (n = 54) | HOC Present (n = 38) | Neither HOC nor HOS Present (n = 85) | p-Value |
| Diabetes mellitus | 20 (37.0) | 17 (44.7) | 42 (49.4) | 0.56 |
| eGFR (mL/min/1.73 m2) | 47.3 | 44.9 | 48.2 | 0.89 |
| 3 vessels with lesions ≥ 50% | 52 (96.3) | 33 (86.8) | 78 (91.7) | 0.37 |
| 2 vessels with LM/proximal LAD | 2 (3.7) | 3 (7.9) | 4 (4.7) | 0.75 |
| Unprotected LM | 0 (0.0) | 2 (5.3) | 3 (3.5) | 0.47 |
| EuroSCORE II (points) | 3.4 ± 2.0 | 4.6 ± 12 | 4.7 ± 7.9 | 0.23 |
| SYNTAX score (points) | 28 ± 8.3 | 27 ± 8.4 | 27.9 ± 10.1 | 0.81 |
| Decision for CABG/PCI Appropriate According to | ||||
| ACC appropriate use criteria | ||||
| Rarely appropriate care | 2/50 (4.0) | 5/33 (15.2) | 10/76 (13.2) | 0.17 |
| May be appropriate care | 16/50 (32.0) | 7/33 (21.2) | 21/76 (27.6) | 0.56 |
| Appropriate care | 32/50 (64.0) | 21/33 (63.6) | 45/76 (59.2) | 0.83 |
| SYNTAX score II calculation | 44/50 (88.0) | 32/33 (97.0) | 63/76 (82.9) | 0.09 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdulrahman, M.; Alsabbagh, A.; Kuntze, T.; Lauer, B.; Ohlow, M.A. Impact of Hierarchy on Multidisciplinary Heart-Team Recommendations in Patients with Isolated Multivessel Coronary Artery Disease. J. Clin. Med. 2019, 8, 1490. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm8091490
Abdulrahman M, Alsabbagh A, Kuntze T, Lauer B, Ohlow MA. Impact of Hierarchy on Multidisciplinary Heart-Team Recommendations in Patients with Isolated Multivessel Coronary Artery Disease. Journal of Clinical Medicine. 2019; 8(9):1490. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm8091490
Chicago/Turabian StyleAbdulrahman, Mohamed, Alaa Alsabbagh, Thomas Kuntze, Bernward Lauer, and Marc A. Ohlow. 2019. "Impact of Hierarchy on Multidisciplinary Heart-Team Recommendations in Patients with Isolated Multivessel Coronary Artery Disease" Journal of Clinical Medicine 8, no. 9: 1490. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm8091490