Mechanical Evaluation of the Stability of One or Two Miniscrews under Loading on Synthetic Bone
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measurements
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
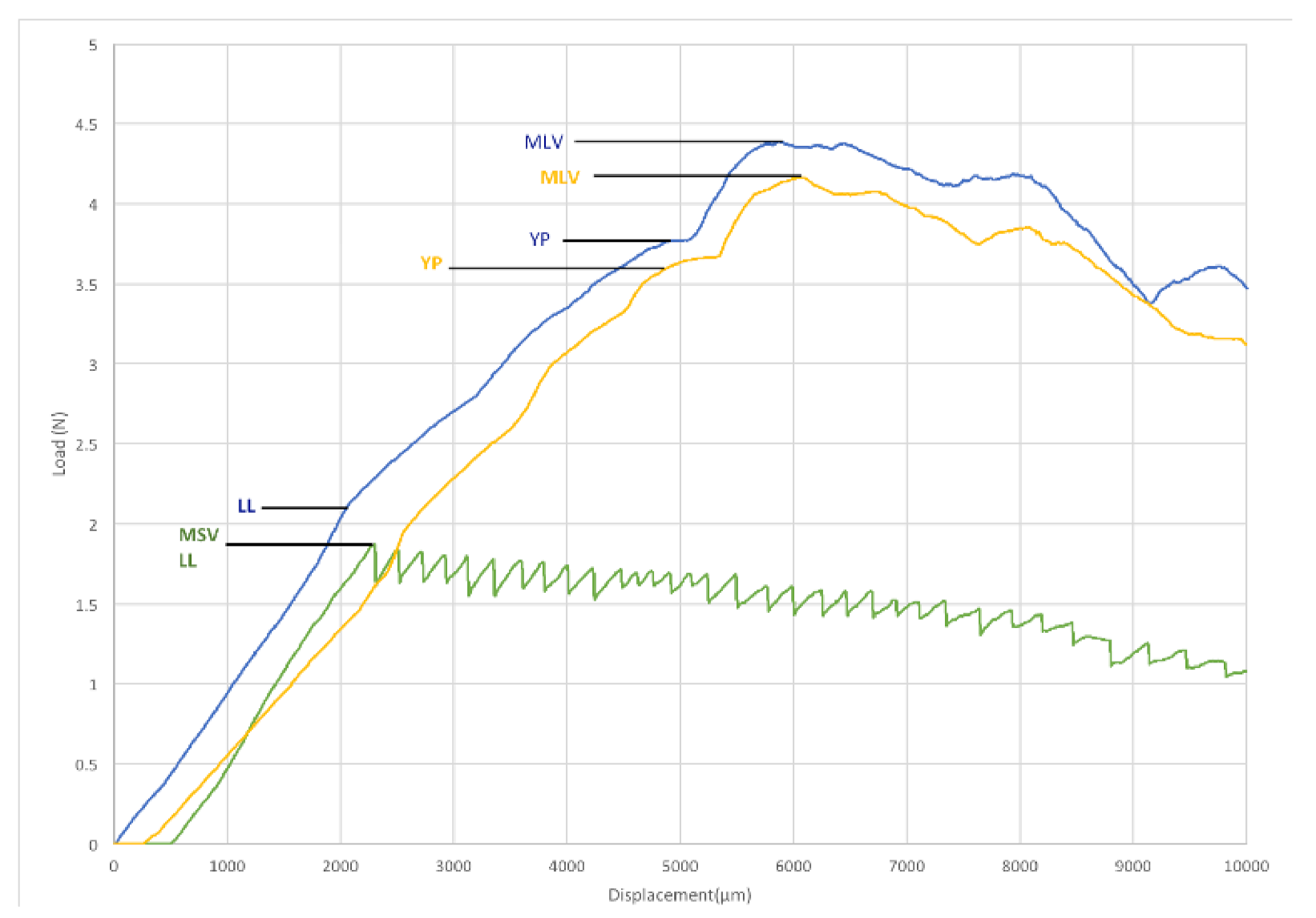
- a two-TAD system is on average stiffer than a one-TAD system under orthodontic loading;
- a one-TAD loses stability before reaching the YL of the TMA-archwire;
- the highest MLVs can be reached only with a two-TAD system; and the MLVs depends strictly on the archwire material in the two-TAD system.
Author Contributions
Funding
Conflicts of Interest
References
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.-M.; Takano-Yamamoto, T. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am. J. Orthod. Dentofacial. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Kuang, S.-H.; Wu, C.-H. Factors associated with the stability of mini-implants for orthodontic anchorage: A study of 414 samples in Taiwan. J. Oral Maxillofac. Surg. 2009, 67, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.-Y.; Kil, J.-K.; Yoon, T.-M.; Hwang, C.-J. Miniscrew stability evaluated with computerized tomography scanning. Am. J. Orthod. Dentofacial. Orthop. 2010, 137, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Migliorati, M.; Signori, A.; Silvestrini-Biavati, A. Temporary anchorage device stability: An evaluation of thread shape factor. Eur. J. Orthod. 2012, 34, 582–586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, C.-M.; Watanabe, K.; Tsatalis, A.E.; Lee, D.; Zheng, F.; Kyung, H.-M.; Deguchi, T.; Kim, D.-G. Evaluations of miniscrew type-dependent mechanical stability. Clin. Biomech. 2019, 69, 21–27. [Google Scholar] [CrossRef]
- Chang, Z.-C.J.; Chen, Y.-J.; Tung, Y.-Y.; Chiang, Y.-Y.; Lai, E.H.-H.; Chen, W.-P.; Lin, C.-P. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jeong, Y.; Pittman, J.; Deguchi, T.; Johnston, W.M.; Fields, H.W.; Kim, D.-G. Primary stability and viscoelastic displacement of mini-implant system under loading. Clin. Biomech. 2017, 41, 28–33. [Google Scholar] [CrossRef]
- Gupta, N.; Kotrashetti, S.M.; Naik, V. A comparitive clinical study between self tapping and drill free screws as a source of rigid orthodontic anchorage. J. Maxillofac. Oral Surg. 2012, 11, 29–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chopra, S.S.; Chakranarayan, A. Clinical evaluation of immediate loading of titanium orthodontic implants. Med. J. Armed Forces India 2015, 71, 165–170. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.-J.; Chang, H.-H.; Lin, H.-Y.; Lai, E.H.-H.; Hung, H.-C.; Yao, C.-C.J. Stability of miniplates and miniscrews used for orthodontic anchorage: Experience with 492 temporary anchorage devices. Clin. Oral Implants Res. 2008, 19, 1188–1196. [Google Scholar] [CrossRef]
- Wilmes, B.; Rademacher, C.; Olthoff, G.; Drescher, D. Parameters affecting primary stability of orthodontic mini-implants. J. Orofac. Orthop. Fortschritte Kieferorthopadie 2006, 67, 162–174. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M.A. Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 577–595. [Google Scholar] [CrossRef] [PubMed]
- Uesugi, S.; Kokai, S.; Kanno, Z.; Ono, T. Stability of secondarily inserted orthodontic miniscrews after failure of the primary insertion for maxillary anchorage: Maxillary buccal area vs midpalatal suture area. Am. J. Orthod. Dentofacial. Orthop. 2018, 153, 54–60. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.Y.; Mimi, Y.; Tak, C.M.; Chiong, F.K.W.; Chew, W.H. A study of success rate of miniscrew implants as temporary anchorage devices in Singapore. Int. J. Dent. 2015, 2015, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Cho, K.-C.; Baek, S.-H. Effects of predrilling depth and implant shape on the mechanical properties of orthodontic mini-implants during the insertion procedure. Angle Orthod. 2012, 82, 618–624. [Google Scholar] [CrossRef] [Green Version]
- Chaimanee, P.; Suzuki, B.; Suzuki, E.Y. “Safe Zones” for miniscrew implant placement in different dentoskeletal patterns. Angle Orthod. 2011, 81, 397–403. [Google Scholar] [CrossRef]
- Di Leonardo, B.; Ludwig, B.; Lisson, J.A.; Contardo, L.; Mura, R.; Hourfar, J. Insertion torque values and success rates for paramedian insertion of orthodontic mini-implants: A retrospective study. J. Orofac. Orthop. Fortschritte Kieferorthopadie 2018, 79, 109–115. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Barberis, F.; Schiavetti, I.; Dalessandri, D.; Benedicenti, S.; Biavati, A.S. Torque loss after miniscrew placement: An in-vitro study followed by a clinical trial. Open Dent. J. 2016, 10, 251–260. [Google Scholar] [CrossRef] [Green Version]
- Cozzani, M.; Nucci, L.; Lupini, D.; Dolatshahizand, H.; Fazeli, D.; Barzkar, E.; Naeini, E.; Jamilian, A. The ideal insertion angle after immediate loading in Jeil, Storm, and Thunder miniscrews: A 3D-FEM study. Int. Orthod. 2020, 18, 503–508. [Google Scholar] [CrossRef]
- Villela, H.M.; Filho, M.V.; Valdrighi, H.C.; Santamaria, M., Jr.; de Menezes, C.C.; Filho, M.V.; Vedovello, M. Evaluation of miniscrew angulation in the posterior maxilla using cone-beam computed tomographic image. Dent. Press J. Orthod. 2018, 23, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, H.; Deguchi, T.; Hasegawa, M.; Ito, M.; Kim, S.; Takano-Yamamoto, T. Orthodontic miniscrew failure rate and root proximity, insertion angle, bone contact length, and bone density: Failure factors for orthodontic miniscrew. Orthod. Craniofac. Res. 2013, 16, 44–55. [Google Scholar] [CrossRef]
- Bertl, K.; Domic, D.; Hirtler, L.; Heimel, P.; Esfandeyari, A.; Stavropoulos, A.; Ulm, C. Micro-CT evaluation of the cortical bone micro-architecture in the anterior and posterior maxilla and the maxillary sinus floor. Clin. Oral Investig. 2019, 23, 1453–1459. [Google Scholar] [CrossRef] [Green Version]
- Brosh, T.; Yekaterina, B.-E.; Pilo, R.; Shpack, N.; Geron, S. Can cone beam CT predict the hardness of interradicular cortical bone? Head Face Med. 2014, 10, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liou, E.J.W.; Pai, B.C.J.; Lin, J.C.Y. Do miniscrews remain stationary under orthodontic forces? Am. J. Orthod. Dentofacial. Orthop. 2004, 126, 42–47. [Google Scholar] [CrossRef]
- Nguyen, M.V.; Codrington, J.; Fletcher, L.; Dreyer, C.W.; Sampson, W.J. Influence of cortical bone thickness on miniscrew microcrack formation. Am. J. Orthod. Dentofacial. Orthop. 2017, 152, 301–311. [Google Scholar] [CrossRef]
- Rossi, M.; Bruno, G.; De Stefani, A.; Perri, A.; Gracco, A. Quantitative CBCT evaluation of maxillary and mandibular cortical bone thickness and density variability for orthodontic miniplate placement. Int. Orthod. 2017, 15, 610–624. [Google Scholar] [CrossRef]
- Derton, N.; Perini, A.; Mutinelli, S.; Gracco, A. Mandibular molar uprighting using mini-implants: Different approaches for different clinical cases—Two case reports. Orthod. Art. Pract. Dentofac. Enhanc. 2012, 13, 138–145. [Google Scholar]
- Yang, Y.; He, C.; Dianyu, E.; Yang, W.; Qi, F.; Xie, D.; Shen, L.; Peng, S.; Shuai, C. Mg bone implant: Features, developments and perspectives. Mater. Des. 2020, 185, 108259. [Google Scholar] [CrossRef]
- Su, Y.-H.; Peng, B.-Y.; Wang, P.-D.; Feng, S.-W. Evaluation of the implant stability and the marginal bone level changes during the first three months of dental implant healing process: A prospective clinical study. J. Mech. Behav. Biomed. Mater. 2020, 110, 103899. [Google Scholar] [CrossRef] [PubMed]


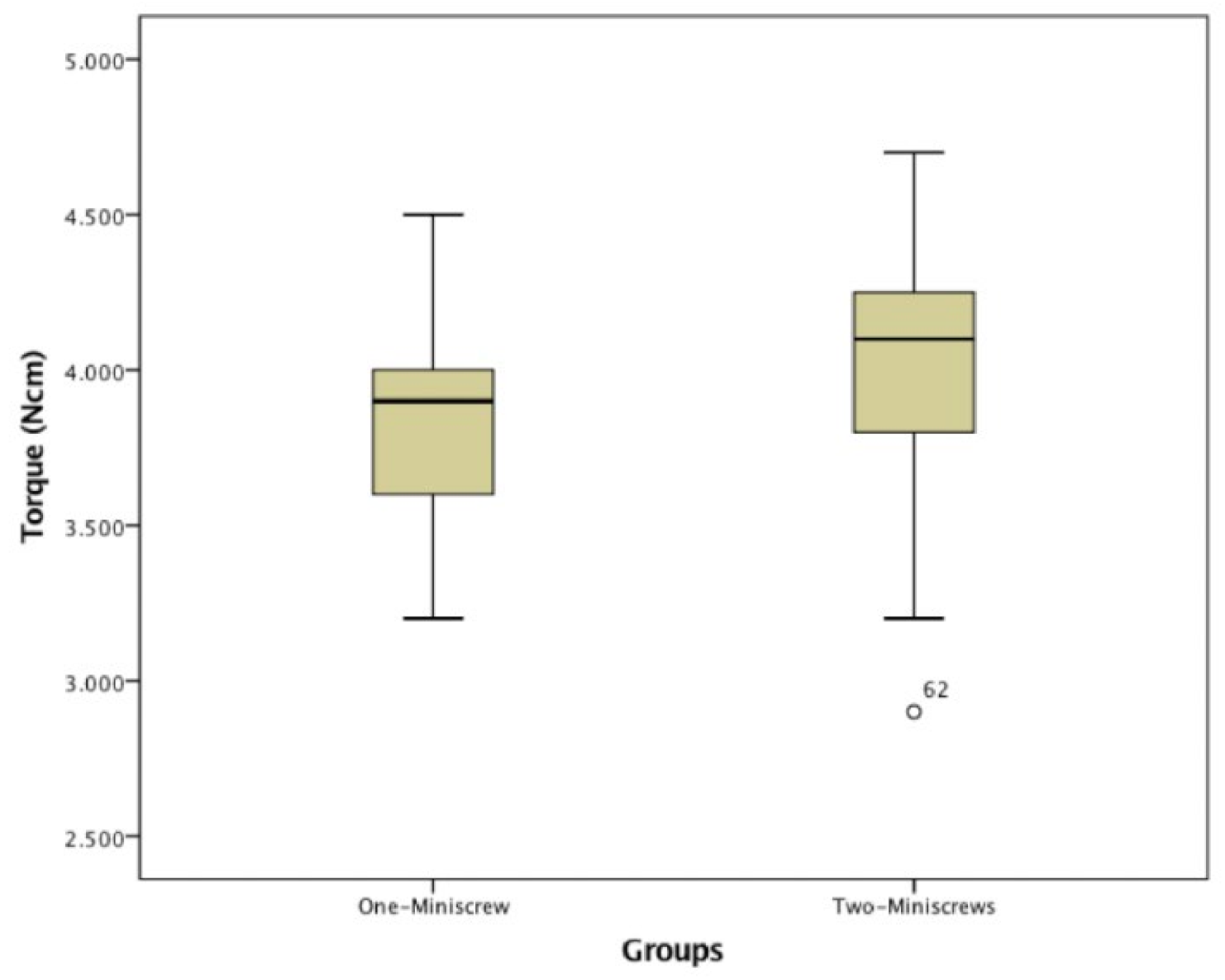

| One-Miniscrew (23) | Two-Miniscrews (44) | ||||
|---|---|---|---|---|---|
| Mean Value | SD | Mean Value | SD | p | |
| Insertion Torque (Ncm) | 3.870 | 0.388 | 4.014 | 0.399 | 0.089 |
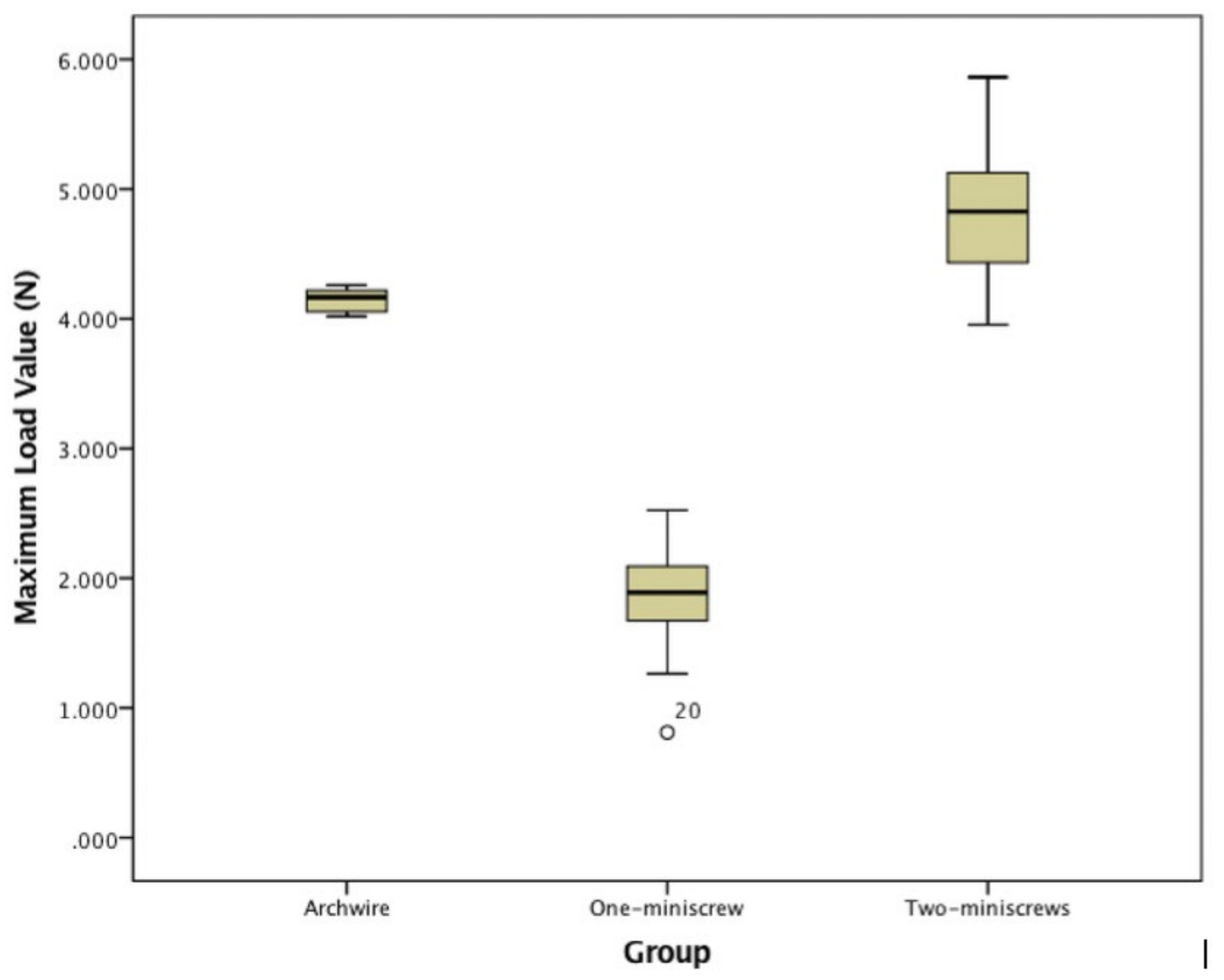
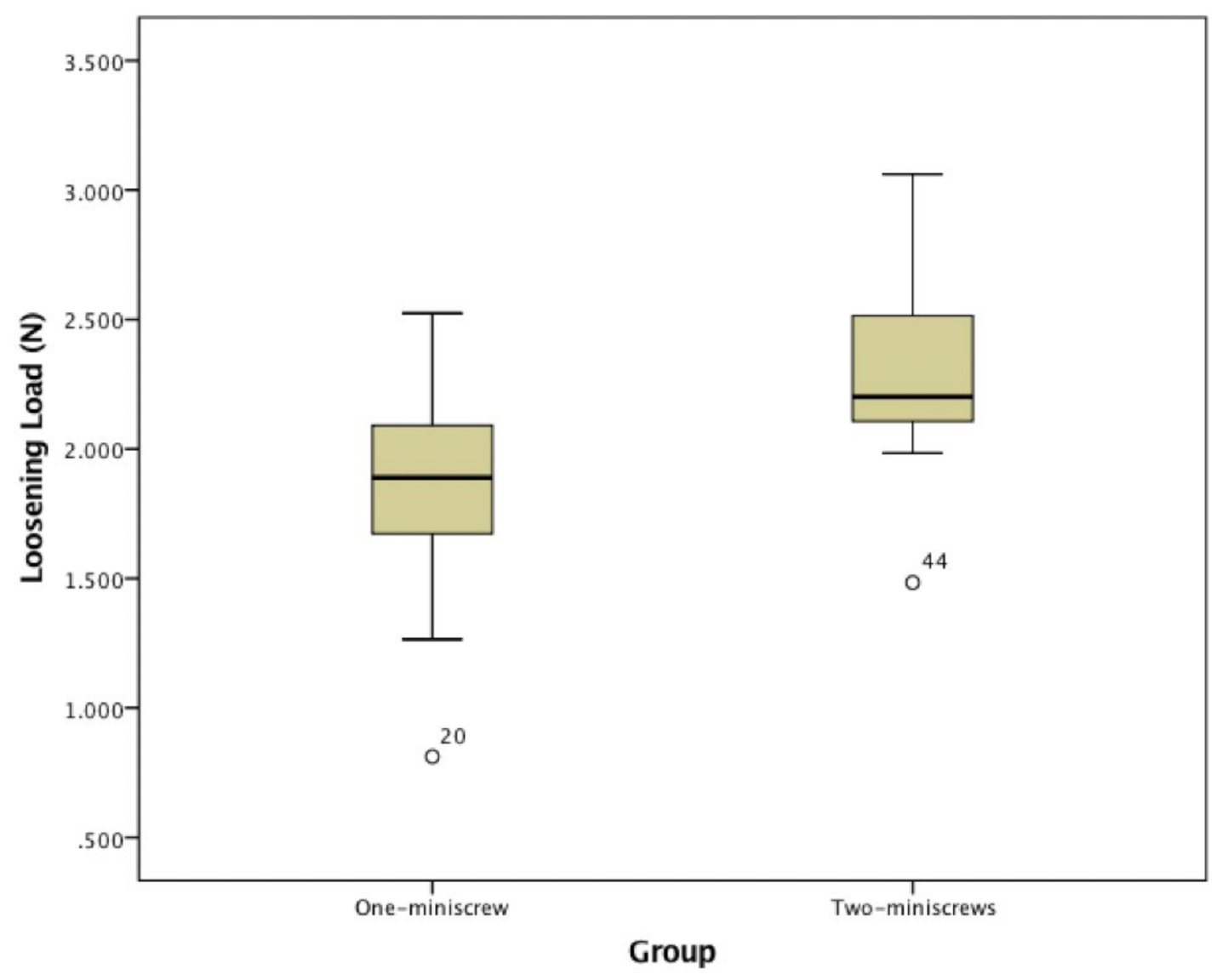
| One-Miniscrew (23 Singles) | Two-Miniscrews (22 Couples) | Archwire Only | |||||
|---|---|---|---|---|---|---|---|
| Mean Value | SD | Mean Value | SD | Mean Value | SD | p | |
| Yield (N) | NA | NA | 4.189 N | ±0.390 N | 3.652 N | ±0.064 N | 0.000 |
| Maximum Load Value (N) | 1.871 N | ±0.318 N | 4.843 N | ±0.515 N | 4.150 N | ±0.086 N | 0.000 |
| Loosening Load (N) | 1.871 N | ±0.318N | 2.294 N | ±0.333 N | NA | NA | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pradal, A.; Nucci, L.; Derton, N.; De Felice, M.E.; Turco, G.; Grassia, V.; Contardo, L. Mechanical Evaluation of the Stability of One or Two Miniscrews under Loading on Synthetic Bone. J. Funct. Biomater. 2020, 11, 80. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb11040080
Pradal A, Nucci L, Derton N, De Felice ME, Turco G, Grassia V, Contardo L. Mechanical Evaluation of the Stability of One or Two Miniscrews under Loading on Synthetic Bone. Journal of Functional Biomaterials. 2020; 11(4):80. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb11040080
Chicago/Turabian StylePradal, Andrea, Ludovica Nucci, Nicola Derton, Maria Elena De Felice, Gianluca Turco, Vincenzo Grassia, and Luca Contardo. 2020. "Mechanical Evaluation of the Stability of One or Two Miniscrews under Loading on Synthetic Bone" Journal of Functional Biomaterials 11, no. 4: 80. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb11040080





