Implant Placement Following Crestal Sinus Lift with Sequential Drills and Osteotomes: Five Years after Final Loading Results from a Retrospective Study
Abstract
:1. Introduction
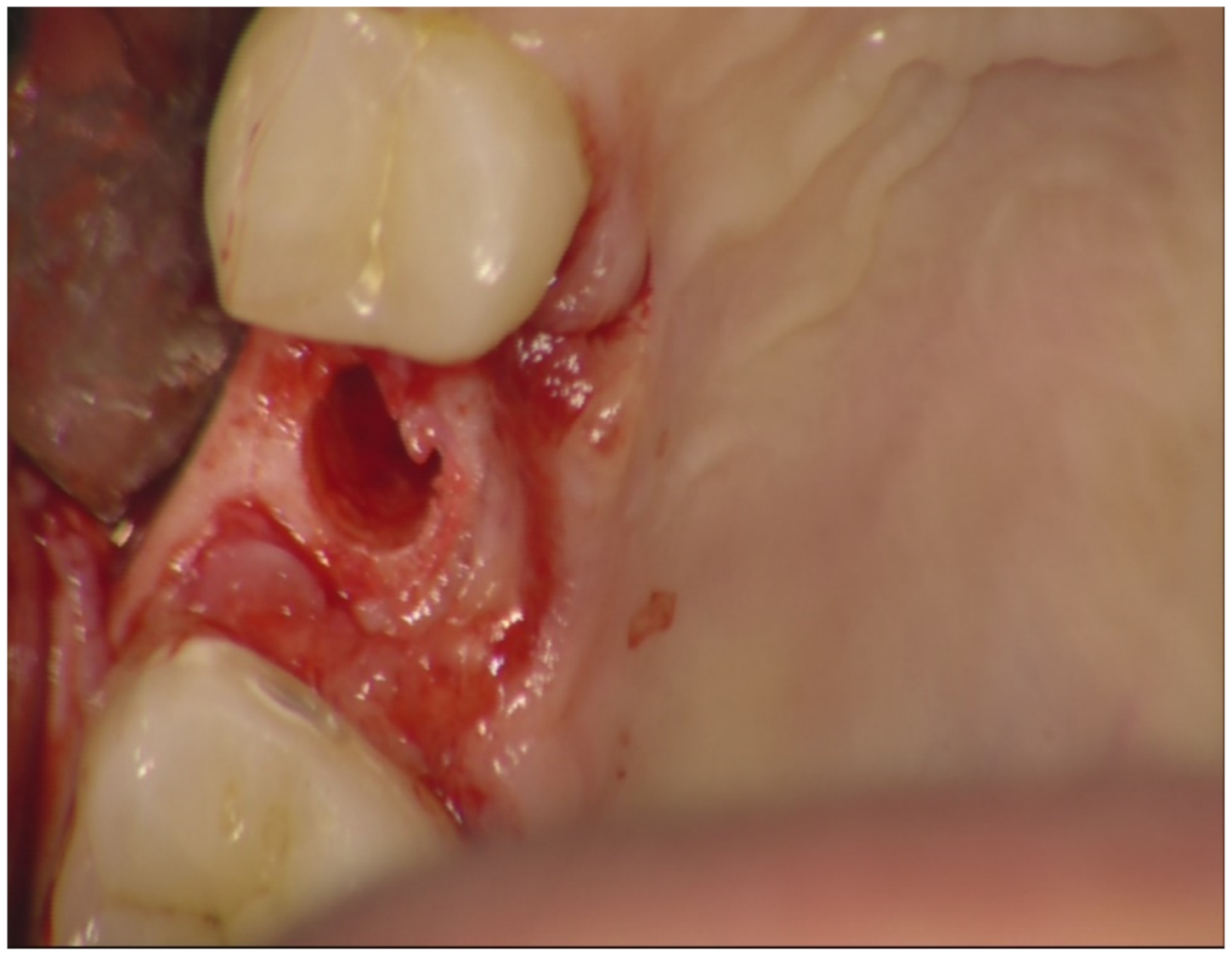
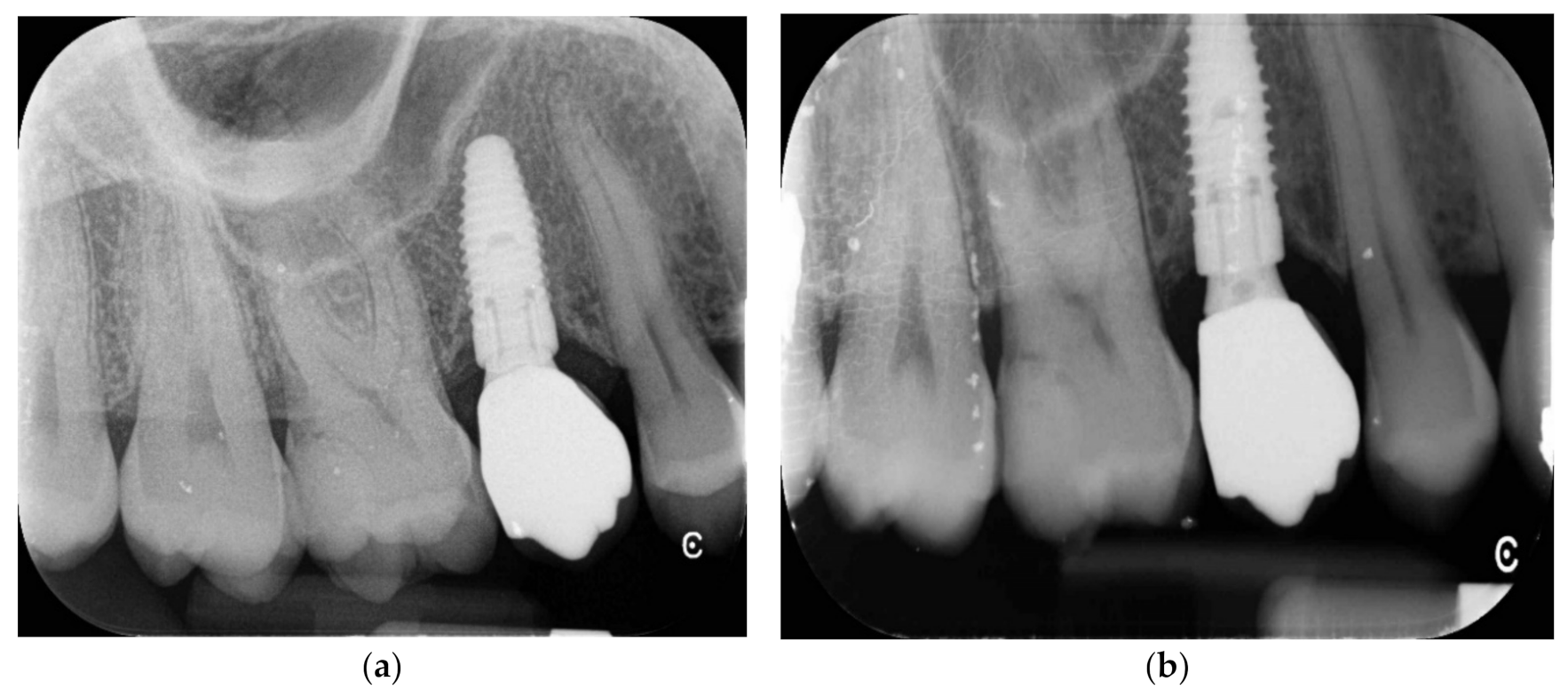
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reich, K.; Huber, C.; Lippnig, W.; Ulm, C.; Watzek, G.; Tangl, S. Atrophy of the residual alveolar ridge following tooth loss in an historical population. Oral Dis. 2010, 17, 33–44. [Google Scholar] [CrossRef] [Green Version]
- Urban, I.A.; Wessing, B.; Alández, N.; Meloni, S.; González-Martin, O.; Polizzi, G.; Sanz-Sanchez, I.; Montero, E.; Zechner, W. A multicenter randomized controlled trial using a novel collagen membrane for guided bone regeneration at dehisced single implant sites: Outcome at prosthetic delivery and at 1-year follow-up. Clin. Oral Implantol. Res. 2019, 30, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Spano, G.; Ceruso, F.M.; Gargari, M.; Lumbau, A.; Baldoni, E.; Massarelli, O.; Pisano, M.; Tallarico, M. Upper jaw implant restoration on six implants with flapless guided template surgery and immediate loadings: 5 years results of prospective case series. Oral Implantol. 2019, 12, 151–160. [Google Scholar] [CrossRef] [Green Version]
- Meloni, S.M.; Jovanovic, S.A.; Urban, I.; Baldoni, E.; Pisano, M.; Tallarico, M. Horizontal ridge augmentation using GBR with a native collagen membrane and 1:1 ratio of particulate xenograft and autologous bone: A 3-year after final loading prospective clinical study. Clin. Implantol. Dent. Relat. Res. 2019, 21, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Lumbau, A.; Spano, G.; Baldoni, E.; Pisano, M.; Tullio, A.; Tallarico, M. Sinus augmentation grafting with anorganic bovine bone versus 50% autologous bone mixed with 50% anorganic bovine bone: 5 years after loading results from a randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 483–492. [Google Scholar]
- Tallarico, M.; Ceruso, F.M.; Xhanari, E.; Gargari, M.; Canullo, L.; Meloni, S.M. Immediately loaded tilted implants combined with angulated screw channel zirconia abutments in atrophic maxillary patients: A three-year after loading prospective case series study. Oral Implantol. 2018, 11, 106–114. [Google Scholar]
- Wessing, B.; Urban, I.; Montero, E.; Zechner, W.; Hof, M.; Chamorro, J.A.; Martin, N.A.; Polizzi, G.; Meloni, S.; Sanz, M. A multicenter randomized controlled clinical trial using a new resorbable non-cross-linked collagen membrane for guided bone regeneration at dehisced single implant sites: Interim results of a bone augmentation procedure. Clin. Oral Implantol. Res. 2016, 28, e218–e226. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Tallarico, M.; Pisano, M.; Xhanari, E.; Canullo, L. Immediate Loading of Fixed Complete Denture Prosthesis Supported by 4–8 Implants Placed Using Guided Surgery: A 5-Year Prospective Study on 66 Patients with 356 Implants. Clin. Implantol. Dent. Relat. Res. 2016, 19, 195–206. [Google Scholar] [CrossRef]
- Tallarico, M.; Meloni, S.M. Retrospective Analysis on Survival Rate, Template-Related Complications, and Prevalence of Peri-implantitis of 694 Anodized Implants Placed Using Computer-Guided Surgery: Results Between 1 and 10 Years of Follow-Up. Int. J. Oral Maxillofac. Implantol. 2017, 32, 1162–1171. [Google Scholar] [CrossRef]
- Tallarico, M.; Canullo, L.; Pisano, M.; Peñarrocha-Oltra, D.; Penarrocha-Diago, M.; Meloni, S.M. An up to 7-Year Retrospective Analysis of Biologic and Technical Complication With the All-on-4 Concept. J. Oral Implantol. 2016, 42, 265–271. [Google Scholar] [CrossRef]
- Meloni, S.M.; Jovanovic, S.; Lolli, F.; Cassisa, C.; De Riu, G.; Pisano, M.; Lumbau, A.I.; Luglié, P.F.; Tullio, A. Grafting after sinus lift with anorganic bovine bone alone compared with 50:50 anorganic bovine bone and autologous bone: Results of a pilot randomised trial at one year. Br. J. Oral Maxillofac. Surg. 2015, 53, 436–441. [Google Scholar] [CrossRef]
- Ulm, C.; Solar, P.; Gsellmann, B.; Matejka, M.; Watzek, G. The edentulous maxillary alveolar process in the region of the maxillary sinus--a study of physical dimension. Int. J. Oral Maxillofac. Surg. 1995, 24, 279–282. [Google Scholar] [CrossRef]
- Tatum, H., Jr. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–209. [Google Scholar]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar]
- Juzikis, E.; Gaubys, A.; Rusilas, H. Uses of maxillary sinus lateral wall bony window in an open window sinus lift procedure: Literature review. Stomatologija 2018, 20, 14–21. [Google Scholar] [PubMed]
- Niño-Sandoval, T.C.; Vasconcelos, B.C.D.E.; Moraes, S.D.; Lemos, C.A.A.; Pellizzer, E. Efficacy of stem cells in maxillary sinus floor augmentation: Systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2019, 48, 1355–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawood, T.; Sadek, H. Maxillary Sinus Augmentation by Autogenous Block Graft A—Case Report. IOSR J. Dent. Med. Sci. 2016, 15, 81–87. [Google Scholar] [CrossRef]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152–154. [Google Scholar]
- Cosci, F.; Boni, M.; Baldazzi, C.; Bozzoli, P.; Norcia, A.; Russo, V. Rialzo del seno mascellare con approccio crestale: Studio multicentrico con 10 anni di follow-up. Quintessenza Internazionale 2004, 5, 73–79. [Google Scholar]
- Wallace, S.S.; Mazor, Z.; Froum, S.; Cho, S.-C.; Tarnow, D.P. Schneiderian membrane perforation rate during sinus elevation using piezosurgery: Clinical results of 100 consecutive cases. Int. J. Periodontics Restor. Dent. 2007, 27, 413–419. [Google Scholar]
- Nicholson, W.; Titanium, J. Alloys for Dental Implants: A Review. Prosthesis 2020, 2, 100–116. [Google Scholar] [CrossRef]
- Better, H.; Slavescu, D.; Barbu, H.; Cochran, D.L.; Chaushu, G. Minimally Invasive Sinus Lift Implant Device: A Multicenter Safety and Efficacy Trial Preliminary Results. Clin. Implantol. Dent. Relat. Res. 2012, 16, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Meloni, S.M.; Xhanari, E.; Pisano, M.; Cochran, D.L. Minimally Invasive Sinus Augmentation Procedure Using a Dedicated Hydraulic Sinus Lift Implant Device: A Prospective Case Series Study on Clinical, Radiologic, and Patient-Centered Outcomes. Int. J. Periodontics Restor. Dent. 2017, 37, 125–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tallarico, M.; Cochran, D.L.; Xhanari, E.; Dellavia, C.; Canciani, E.; Mijiritsky, E.; Meloni, S.M. Crestal sinus lift using an implant with an internal L-shaped channel: 1-year after loading results from a prospective cohort study. Eur. J. Oral Implantol. 2017, 10, 325–336. [Google Scholar]
- Chen, L.; Cha, J. An 8-Year Retrospective Study: 1100 Patients Receiving 1,557 Implants Using the Minimally Invasive Hydraulic Sinus Condensing Technique. J. Periodontol. 2005, 76, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Xhanari, E.; Tallarico, M.; Meloni, S.M.; Kalemaj, Z.; Ceruso, F.M.; Dedaj, E. Crestal versus lateral sinus lift: One year results from a within-patient randomized controlled trial. Clin. Trials Dent. 2019, 5, 67–78. [Google Scholar]
- Gatti, F.; Gatti, C.; Tallarico, M.; Tommasato, G.; Meloni, S.; Chiapasco, M. Maxillary Sinus Membrane Elevation Using a Special Drilling System and Hydraulic Pressure: A 2-Year Prospective Cohort Study. Int. J. Periodontics Restor. Dent. 2018, 38, 593–599. [Google Scholar] [CrossRef]
- Tallarico, M.; Vaccarella, A.; Marzi, G.C.; Alviani, A.; Campana, V. A prospective case-control clinical trial comparing 1- and 2-stage Nobel Biocare TiUnite implants: Resonance frequency analysis assessed by Osstell Mentor during integration. Quintessence Int. 2011, 42, 635–644. [Google Scholar]
- Tallarico, M.; Vaccarella, A.; Marzi, G.C. Clinical and radiological outcomes of 1- versus 2-stage implant placement: 1-year results of a randomised clinical trial. Eur. J. Oral Implantol. 2011, 4, 13–20. [Google Scholar]
- Buser, D.; Weber, H.-P.; Lang, N.P. Tissue integration of non-submerged implants. l-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin. Oral Implantol. Res. 1990, 1, 33–40. [Google Scholar] [CrossRef]
- California Dental Association, Task Force on Quality Evaluation. Quality Evaluation for Dental Care: Guidelines for the Assessment of Clinical Quality and Professional Performance and the Standards for the Program Design to Assure the Quality of Care; California Dental Association: Los Angeles, CA, USA, 1976. [Google Scholar]
- Pjetursson, B.E.; Rast, C.; Brägger, U.; Schmidlin, K.; Zwahlen, M.; Lang, N.P. Maxillary sinus floor elevation using the (transalveolar) osteotome technique with or without grafting material. Part I: Implant survival and patients’ perception. Clin. Oral Implantol. Res. 2009, 20, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Danesh-Sani, S.-A.; Loomer, P.M.; Wallace, S.S. A comprehensive clinical review of maxillary sinus floor elevation: Anatomy, techniques, biomaterials and complications. Br. J. Oral Maxillofac. Surg. 2016, 54, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Testori, T.; Weinstein, T.; Taschieri, S.; Wallace, S.S. Risk factors in lateral window sinus elevation surgery. Periodontology 2000 2019, 81, 91–123. [Google Scholar] [CrossRef] [PubMed]
- Toffler, M. Minimally invasive sinus floor elevation procedures for simultaneous and staged implant placement. N. Y. State Dent. J. 2004, 70, 38–44. [Google Scholar] [PubMed]
- Testori, T.; Weinstein, R.L.; Tascheri, S.; del Fabbro, M. Risk factor analysis following maxillary sinus augmentation: A retrospective multicenter studt. Int. J. Oral Maxillofac. Implant. 2012, 27, 1170–1176. [Google Scholar]
- Ortega-Mejia, H.; Estrugo-Devesa, A.; Saka-Herrán, C.; Ayuso-Montero, R.; López-López, J.; Velasco-Ortega, E. Platelet-Rich Plasma in Maxillary Sinus Augmentation: Systematic Review. Materials 2020, 13, 622. [Google Scholar] [CrossRef] [Green Version]




| 1 | General contraindications for implant surgery |
| 2 | Lack of occluding dentition in the area intended for implant placement |
| 3 | Untreated periodontitis |
| 4 | Poor oral hygiene (Bleeding on probing (BOP) and/or plaque index (PI) > 25%) |
| 5 | Severe or moderate bruxism |
| 6 | Irradiation of the head and neck area in the previous five years |
| 7 | Uncontrolled diabetes |
| 8 | Heavy smoker (>10 cigarettes/day) |
| 9 | Substance abuse and/or psychiatric disorder |
| 10 | Pregnancy or lactation |
| 11 | Lack of 5-year post-loading data |
| 1 Year | 5 Years | |
|---|---|---|
| Survival rate | 98.1% | 98.1% |
| Complications | BOP at 2 implants | None |
| Marginal Bone loss | 0.94 ± 0.18 mm | 1.24 ± 0.28 mm |
| Table 2 | Implant Survival Rate | MBL | Follow-Up |
|---|---|---|---|
| Chen e Cha et al., 2005 | 99.3% | Not reported | 8 years |
| Tallarico et al., 2017 | 100% | 0.19 ± 1.05 mm | 1 year |
| Xhanari et al., 2019 | 100% | 0.99 ± 0.55 mm | 1 year |
| Gatti et al., 2018 | 100% | 0.33 ± 0.24 mm | 2 years |
| Lumbau et al., 2020 | 98.1% | 1.24 ± 0.28 mm | 5 years |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lumbau, A.I.; Meloni, S.M.; Tallarico, M.; Melis, L.; Spano, G.; Baldoni, E.; Koshovari, A.; Pisano, M. Implant Placement Following Crestal Sinus Lift with Sequential Drills and Osteotomes: Five Years after Final Loading Results from a Retrospective Study. J. Funct. Biomater. 2021, 12, 10. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb12010010
Lumbau AI, Meloni SM, Tallarico M, Melis L, Spano G, Baldoni E, Koshovari A, Pisano M. Implant Placement Following Crestal Sinus Lift with Sequential Drills and Osteotomes: Five Years after Final Loading Results from a Retrospective Study. Journal of Functional Biomaterials. 2021; 12(1):10. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb12010010
Chicago/Turabian StyleLumbau, Aurea Immacolata, Silvio Mario Meloni, Marco Tallarico, Luca Melis, Giovanni Spano, Edoardo Baldoni, Alba Koshovari, and Milena Pisano. 2021. "Implant Placement Following Crestal Sinus Lift with Sequential Drills and Osteotomes: Five Years after Final Loading Results from a Retrospective Study" Journal of Functional Biomaterials 12, no. 1: 10. https://0-doi-org.brum.beds.ac.uk/10.3390/jfb12010010







