Antibiotic Use in Periodontal Therapy among French Dentists and Factors Which Influence Prescribing Practices
Abstract
:1. Introduction
2. Results
2.1. Characteristics of Respondents
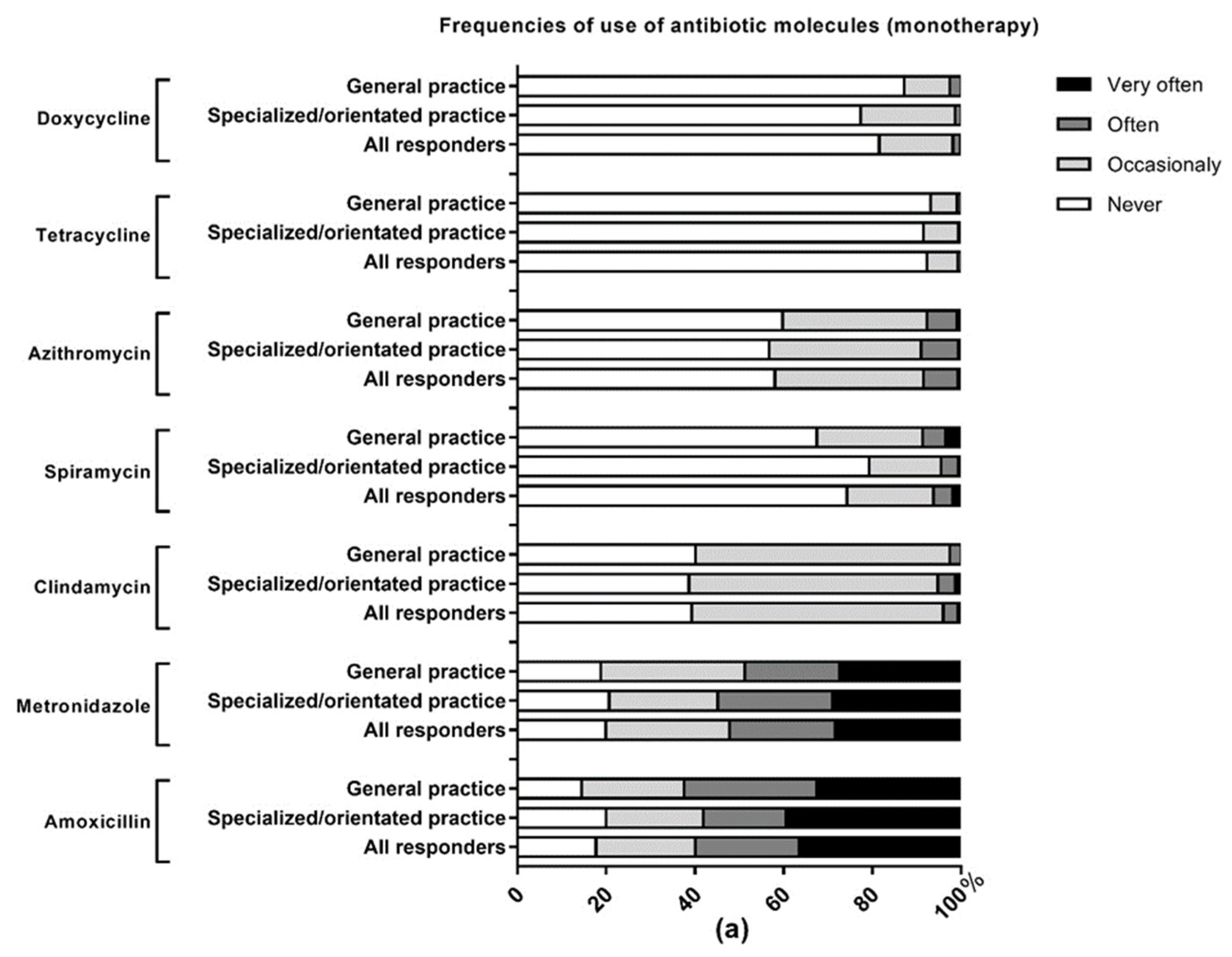
2.2. Knowledge and Use of Systemic Antibiotics
2.3. Knowledge and Use of Local Antibiotics
2.4. Factors Influencing Knowledge and Practice Scores
3. Discussion
3.1. Main Results and Comparison to Previous Studies
3.2. Limitations of the Present Study
3.3. Perspectives of the Present Study
- Education: It is clear that no antimicrobial stewardship program can be successful without education. The lack of education on the prescription of antibiotics and the issue of antimicrobial resistance during undergraduate or medical specialty training has been previously emphasized in France and other countries [63,64,65,66,67]. The results of this survey confirm post-graduate education as a determining factor in the prescribing habits of dentists and suggest that practitioners, particularly those who have been in practice for a long time, should be made more aware of the need to improve their practices in the prescription of antibiotics for periodontal therapy. The guidelines on implementing antimicrobial stewardship programs suggest that the culture of antimicrobial stewardship should be integrated early in the pre-clinical and clinical curriculum before certain attitudes and prescribing habits are formed [68]. According to the literature, only 40% of medical students are familiar even with the term “antimicrobial stewardship” [69]. It has also been observed that slightly less than one-third of dentists change their prescribing habits after they first graduated from dental school [31]. Importantly, “patient influence” has been identified as the most frequent factor influencing the prescription of antibiotics in primary care settings including dental care [70]. This suggests that not only healthcare professionals but also the general public need to be educated about the significance of antibiotic resistance and the importance of reducing the use of antibiotics in dental care.
- Development/update of guidelines: The effectiveness of implementing guidelines on the rate of appropriate use of antimicrobials is well documented in the literature [71]. They have the advantage of being accessible to a wide audience including non-specialists in the considered field and allow standardization and streamlining of practices. The most recent French national recommendations about the use of antibiotics in dentistry were published in 2011 [57]. A recent Cochrane review identified a total of 10 systematic reviews on adjunctive use of systemic antimicrobials in periodontal therapy published since 2014 and more than 20 randomized control trials since 2011 [72]. Key changes have also recently been made to how periodontal diseases are diagnosed and classified. The implementation of a new classification scheme for periodontal and peri-implant diseases has resulted in a S3 Level Clinical Practice Guideline (CPG) proposed by the European Federation of Periodontology to facilitate the use of the most appropriate interventions, according to the stage and grade of the disease [61]. Therefore, updated national recommendations about the use of antibiotics in dentistry, which represent the current state of science, would be desirable to better inform practitioners in making their decisions. Fortunately, French dentists are favorable to receiving up-to-date training on antibiotic use. 43.7% report feeling inadequately informed and trained on this subject and 93.7% are willing to receive regular updates on prescribing recommendations, particularly in the form of practical sheets [54].
- Complementary approaches: used alone, didactic passive educational materials are insufficient as antimicrobial stewardship activities. They should be used in conjunction with complementary approaches such as prospective audit and continuous feedback, which have been demonstrated to decrease the number of new prescriptions and to improve clinician satisfaction [68,73]. For example, Computer-Assisted Decision Support Programs can provide real-time feedback that has been shown to result in significant reductions in the use of antimicrobials and an increase in concordance with recommendations [74,75,76].
- Implementation of practical public health actions: An operational strategy has been proposed in 2016 by the French Ministry of Health which includes 13 measures to control antibiotic resistance [77]. We fully adhere to this roadmap and we believe that the focus should be placed on the participation of all health professionals including dentists for whom few visible actions have been implemented so far. In terms of education, we propose (i) the implementation of a mandatory course on antimicrobial resistance for all medical and dental undergraduates or residents as well as (ii) a mandatory course at regular intervals for dentists already in practice. Similar measures already exist with regard to in-office radiation protection skills and training in emergency procedures and care [78]. In clinical practice, (iii) the setting-up of a network of sentinel dentists, similar to the existing network of sentinel medical doctors set up in 1984 [79] to ensure continuous monitoring of indicators of antibiotic consumption and antimicrobial resistance. With regard to research (iv) a support for innovation in the field of alternative antimicrobial strategies to antibiotics in dental practice and the development of research on prescribing practices in dentistry. Hopefully, the results of these studies will enable stakeholders to better understand the prescribing patterns of dentists and to better involve them in the collective fight against antimicrobial resistance.
4. Materials and Methods
4.1. Study Design
4.2. Study Population
4.3. Development of the Questionnaire
4.4. Sample Size Calculation
4.5. Questionnaire Distribution
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic Resistance-the Need for Global Solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef] [Green Version]
- Laxminarayan, R.; Matsoso, P.; Pant, S.; Brower, C.; Røttingen, J.-A.; Klugman, K.; Davies, S. Access to Effective Antimicrobials: A Worldwide Challenge. Lancet Lond. Engl. 2016, 387, 168–175. [Google Scholar] [CrossRef]
- Gajdács, M.; Urbán, E.; Stájer, A.; Baráth, Z. Antimicrobial Resistance in the Context of the Sustainable Development Goals: A Brief Review. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 6. [Google Scholar] [CrossRef]
- Humphreys, G. Are Antibiotics Still “Automatic” in France? Bull. World Health Organ. 2011, 89, 8–9. [Google Scholar] [CrossRef] [PubMed]
- Évolution des Consommations D’antibiotiques en France Entre 2000 et 2015-Point d’Information-ANSM: Agence Nationale de Sécurité du Médicament et des Produits de Santé. Available online: https://ansm.sante.fr/S-informer/Points-d-information-Points-d-information/Evolution-des-consommations-d-antibiotiques-en-France-entre-2000-et-2015-Point-d-Information (accessed on 30 January 2021).
- Consommation D’antibiotiques et Antibiorésistance en France en 2018/les-Actualites/2019/Consommation-d-ANTIBIOTIQUES-et-Antibioresistance-en-France-en-2018. Available online: https://www.santepubliquefrance.fr/les-actualites/2020/consommation-d-antibiotiques-et-antibioresistance-en-france-en-2019 (accessed on 30 January 2021).
- Carlet, J.; Jarlier, V.; Acar, J.; Debaere, O.; Dehaumont, P.; Grandbastien, B.; Le Coz, P.; Lina, G.; Pean, Y.; Rambaud, C.; et al. Trends in Antibiotic Consumption and Resistance in France Over 20 Years: Large and Continuous Efforts but Contrasting Results. Open Forum Infect Dis. 2020, 7, 452. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). European Antimicrobial Resistance Surveillance Network (EARS-Net). Available online: https://www.google.fr/search?q=earss-net&oq=earssnet&aqs=chrome69i57j0l5.6322j0j4&sourceid=chrome&ie=UTF-8 (accessed on 10 September 2019).
- Carbonne, A.; Arnaud, I.; Maugat, S.; Marty, N.; Dumartin, C.; Bertrand, X.; Bajolet, O.; Savey, A.; Fosse, T.; Eveillard, M.; et al. MDRB Surveillance National Steering Group (BMR-Raisin). National multidrug resistant bacteria (MDRB) surveillance in France through the RAISIN network: A 9 year experience. J. Antimicrob. Chemother. 2013, 68, 954–959. [Google Scholar] [CrossRef] [Green Version]
- Santé, M. La Stratégie Nationale de Santé 2018–2022. Available online: https://solidarites-sante.gouv.fr/systeme-de-sante-et-medico-social/strategie-nationale-de-sante/article/la-strategie-nationale-de-sante-2018-2022 (accessed on 10 February 2021).
- Arrêté Du 22 Décembre 2020 Modifiant l’arrêté Du 12 Juin 2018 Modifié Relatif Au Service Sanitaire Pour Les Étudiants En Santé. Available online: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000042731332 (accessed on 30 January 2021).
- Gilchrist, M.; Wade, P.; Ashiru-Oredope, D.; Howard, P.; Sneddon, J.; Whitney, L.; Wickens, H. Antimicrobial Stewardship from Policy to Practice: Experiences from UK Antimicrobial Pharmacists. Infect. Dis. 2015, 4, 51–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norris, P.; Chamberlain, K.; Dew, K.; Gabe, J.; Hodgetts, D.; Madden, H. Public Beliefs about Antibiotics, Infection and Resistance: A Qualitative Study. Antibiotics 2013, 2, 465–476. [Google Scholar] [CrossRef]
- Gajdács, M.; Paulik, E.; Szabó, A. Knowledge, Attitude and Practice of Community Pharmacists Regarding Antibiotic Use and Infectious Diseases: A Cross-Sectional Survey in Hungary (KAPPhA-HU). Antibiotics 2020, 9, 41. [Google Scholar] [CrossRef] [Green Version]
- Marra, F.; George, D.; Chong, M.; Sutherland, S.; Patrick, D.M. Antibiotic Prescribing by Dentists Has Increased: Why? J. Am. Dent. Assoc. 2016, 147, 320–327. [Google Scholar] [CrossRef] [Green Version]
- Thornhill, M.H.; Dayer, M.J.; Durkin, M.J.; Lockhart, P.B.; Baddour, L.M. Oral Antibiotic Prescribing by NHS Dentists in England 2010–2017. Br. Dent. J. 2019, 227, 1044–1050. [Google Scholar] [CrossRef]
- Preus, H.R.; Fredriksen, K.W.; Vogsland, A.E.; Sandvik, L.; Grytten, J.I. Antibiotic-Prescribing Habits among Norwegian Dentists: A Survey over 25 Years (1990–2015). Eur. J. Oral Sci. 2017, 125, 280–287. [Google Scholar] [CrossRef]
- Cope, A.L.; Francis, N.A.; Wood, F.; Chestnutt, I.G. Antibiotic Prescribing in UK General Dental Practice: A Cross-Sectional Study. Community Dent. Oral Epidemiol. 2016, 44, 145–153. [Google Scholar] [CrossRef]
- Mainjot, A.; D’Hoore, W.; Vanheusden, A.; Van Nieuwenhuysen, J.-P. Antibiotic Prescribing in Dental Practice in Belgium. Int. Endod. J. 2009, 42, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Núñez, A.; Cisneros-Cabello, R.; Velasco-Ortega, E.; Llamas-Carreras, J.M.; Tórres-Lagares, D.; Segura-Egea, J.J. Antibiotic Use by Members of the Spanish Endodontic Society. J. Endod. 2009, 35, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Segura-Egea, J.J.; Velasco-Ortega, E.; Torres-Lagares, D.; Velasco-Ponferrada, M.C.; Monsalve-Guil, L.; Llamas-Carreras, J.M. Pattern of Antibiotic Prescription in the Management of Endodontic Infections amongst Spanish Oral Surgeons. Int. Endod. J. 2010, 43, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Tulip, D.E.; Palmer, N.O.A. A Retrospective Investigation of the Clinical Management of Patients Attending an out of Hours Dental Clinic in Merseyside under the New NHS Dental Contract. Br. Dent. J. 2008, 205, 659–664, discussion 648. [Google Scholar] [CrossRef] [Green Version]
- Palmer, N.A.; Pealing, R.; Ireland, R.S.; Martin, M.V. A Study of Prophylactic Antibiotic Prescribing in National Health Service General Dental Practice in England. Br. Dent. J. 2000, 189, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Germack, M.; Sedgley, C.M.; Sabbah, W.; Whitten, B. Antibiotic Use in 2016 by Members of the American Association of Endodontists: Report of a National Survey. J. Endod. 2017, 43, 1615–1622. [Google Scholar] [CrossRef]
- Salako, N.O.; Rotimi, V.O.; Adib, S.M.; Al-Mutawa, S. Pattern of Antibiotic Prescription in the Management of Oral Diseases among Dentists in Kuwait. J. Dent. 2004, 32, 503–509. [Google Scholar] [CrossRef]
- Al-Johani, K.; Reddy, S.G.; Al Mushayt, A.S.; El-Housseiny, A. Pattern of Prescription of Antibiotics among Dental Practitioners in Jeddah, KSA: A Cross-Sectional Survey. Niger. J. Clin. Pract. 2017, 20, 804–810. [Google Scholar] [CrossRef]
- Kaul, R.; Angrish, P.; Jain, P.; Saha, S.; Sengupta, A.V.; Mukherjee, S. A Survey on the Use of Antibiotics among the Dentists of Kolkata, West Bengal, India. Int. J. Clin. Pediatr. Dent. 2018, 11, 122–127. [Google Scholar] [CrossRef]
- Yingling, N.M.; Byrne, B.E.; Hartwell, G.R. Antibiotic Use by Members of the American Association of Endodontists in the Year 2000: Report of a National Survey. J. Endod. 2002, 28, 396–404. [Google Scholar] [CrossRef]
- Swift, J.Q.; Gulden, W.S. Antibiotic Therapy--Managing Odontogenic Infections. Dent. Clin. N. Am. 2002, 46, 623–633. [Google Scholar] [CrossRef]
- Suda, K.J.; Calip, G.S.; Zhou, J.; Rowan, S.; Gross, A.E.; Hershow, R.C.; Perez, R.I.; McGregor, J.C.; Evans, C.T. Assessment of the Appropriateness of Antibiotic Prescriptions for Infection Prophylaxis Before Dental Procedures, 2011 to 2015. JAMA Netw. Open 2019, 2, e193909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, K.; Farmer, J.; Singhal, S.; Marra, F.; Sutherland, S.; Quiñonez, C. The Use and Misuse of Antibiotics in Dentistry: A Scoping Review. J. Am. Dent. Assoc. 2018, 149, 869–884.e5. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Jepsen, S.; Jin, L.; Otomo-Corgel, J. Impact of the Global Burden of Periodontal Diseases on Health, Nutrition and Wellbeing of Mankind: A Call for Global Action. J. Clin. Periodontol. 2017, 44, 456–462. [Google Scholar] [CrossRef] [Green Version]
- Hescot, P. The New Definition of Oral Health and Relationship between Oral Health and Quality of Life. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. CSA 2017, 20, 189–192. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Severe Periodontitis in 1990-2010: A Systematic Review and Meta-Regression. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef]
- Feres, M.; Figueiredo, L.C.; Soares, G.M.S.; Faveri, M. Systemic Antibiotics in the Treatment of Periodontitis. Periodontol. 2015, 67, 131–186. [Google Scholar] [CrossRef]
- Canas, P.G.; Khouly, I.; Sanz, J.; Loomer, P.M. Effectiveness of Systemic Antimicrobial Therapy in Combination with Scaling and Root Planing in the Treatment of Periodontitis: A Systematic Review. J. Am. Dent. Assoc. 2015, 146, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Haffajee, A.D.; Socransky, S.S.; Gunsolley, J.C. Systemic Anti-Infective Periodontal Therapy. A Systematic Review. Ann. Periodontol. 2003, 8, 115–181. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Sanz, M.; Jepsen, S.; Needleman, I.; Roldán, S. A Systematic Review on the Effect of Systemic Antimicrobials as an Adjunct to Scaling and Root Planing in Periodontitis Patients. J. Clin. Periodontol. 2002, 29 (Suppl. 3), 136–159. [Google Scholar] [CrossRef]
- Herrera, D.; Alonso, B.; León, R.; Roldán, S.; Sanz, M. Antimicrobial Therapy in Periodontitis: The Use of Systemic Antimicrobials against the Subgingival Biofilm. J. Clin. Periodontol. 2008, 35 (Suppl. 8), 45–66. [Google Scholar] [CrossRef]
- Herrera, D.; Matesanz, P.; Bascones-Martínez, A.; Sanz, M. Local and Systemic Antimicrobial Therapy in Periodontics. J. Evid.-Based Dent. Pract. 2012, 12 (Suppl. 3), 50–60. [Google Scholar] [CrossRef]
- Keestra, J.A.J.; Grosjean, I.; Coucke, W.; Quirynen, M.; Teughels, W. Non-Surgical Periodontal Therapy with Systemic Antibiotics in Patients with Untreated Aggressive Periodontitis: A Systematic Review and Meta-Analysis. J. Periodontal. Res. 2015, 50, 689–706. [Google Scholar] [CrossRef] [PubMed]
- Rabelo, C.C.; Feres, M.; Gonçalves, C.; Figueiredo, L.C.; Faveri, M.; Tu, Y.-K.; Chambrone, L. Systemic Antibiotics in the Treatment of Aggressive Periodontitis. A Systematic Review and a Bayesian Network Meta-Analysis. J. Clin. Periodontol. 2015, 42, 647–657. [Google Scholar] [CrossRef]
- Bonito, A.J.; Lux, L.; Lohr, K.N. Impact of Local Adjuncts to Scaling and Root Planing in Periodontal Disease Therapy: A Systematic Review. J. Periodontol. 2005, 76, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Hung, H.-C.; Douglass, C.W. Meta-Analysis of the Effect of Scaling and Root Planing, Surgical Treatment and Antibiotic Therapies on Periodontal Probing Depth and Attachment Loss. J. Clin. Periodontol. 2002, 29, 975–986. [Google Scholar] [CrossRef]
- Matesanz-Pérez, P.; García-Gargallo, M.; Figuero, E.; Bascones-Martínez, A.; Sanz, M.; Herrera, D. A Systematic Review on the Effects of Local Antimicrobials as Adjuncts to Subgingival Debridement, Compared with Subgingival Debridement Alone, in the Treatment of Chronic Periodontitis. J. Clin. Periodontol. 2013, 40, 227–241. [Google Scholar] [CrossRef]
- Teughels, W.; Feres, M.; Oud, V.; Martín, C.; Matesanz, P.; Herrera, D. Adjunctive Effect of Systemic Antimicrobials in Periodontitis Therapy: A Systematic Review and Meta-Analysis. J. Clin. Periodontol. 2020, 47 (Suppl 22), 257–281. [Google Scholar] [CrossRef]
- Choudhury, M.; Needleman, I.; Gillam, D.; Moles, D.R. Systemic and Local Antimicrobial Use in Periodontal Therapy in England and Wales. J. Clin. Periodontol. 2001, 28, 833–839. [Google Scholar] [CrossRef]
- Falkenstein, S.; Stein, J.M.; Henne, K.; Conrads, G. Trends in Antibiotic Use and Microbial Diagnostics in Periodontal Treatment: Comparing Surveys of German Dentists in a Ten-Year Period. Clin. Oral Investig. 2016, 20, 2203–2210. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.; Kim, J.; Loo, S.; Quaranta, A.; Rincon, A.J.C. Prescribing Trends of Systemic Antibiotics by Periodontists in Australia. J. Periodontol. 2019, 90, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Kolltveit, K.M.; Tronstad, L.; Olsen, I. Systemic diseases caused by oral infection. Clin. Microbiol. Rev. 2000, 13, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Bui, F.Q.; Almeida-da-Silva, C.L.C.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Spengler, G.; Urbán, E. Identification and Antimicrobial Susceptibility Testing of Anaerobic Bacte-ria: Rubik’s Cube of Clinical Microbiology? Antibiotics 2017, 7, 25. [Google Scholar] [CrossRef] [Green Version]
- Espíndola, L.C.P.; do Nascimento, M.V.M.R.; do Souto, R.M.; Colombo, A.P.V. Antimicrobial susceptibility and virulence of Enterococcus spp. isolated from periodontitis-associated subgingival biofilm. J. Periodontol. 2021. [Google Scholar] [CrossRef]
- Baudet, A.; Kichenbrand, C.; Pulcini, C.; Descroix, V.; Lesclous, P.; Thilly, N.; Clément, C.; Guillet, J. Antibiotic Use and Resistance: A Nationwide Questionnaire Survey among French Dentists. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2020, 39, 1295–1303. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Marotta, C.; Amicone, M.; Bavaro, D.F.; Bernaudo, F.; Frisicale, E.M.; Kurotschka, P.K.; Mazzari, A.; Veronese, N.; Murri, R.; et al. Italian young doctors’ knowledge, attitudes and practices on antibiotic use and resistance: A national cross-sectional survey. J. Glob. Antimicrob. Resist. 2020, 23, 167–173. [Google Scholar] [CrossRef]
- Cummins, J.; McCarthy, M.; Esterman, A.; Karve, A.; Lee, A. Knowledge and Compliance of Dentists’ and Dental Students’ With Respect to Relevant Guidelines for Prescribing Antibiotic Prophylaxis for the Prevention of Infective Endocarditis: A Systematic Review. J. Evid. Based Dent. Pract. 2020, 20, 101311. [Google Scholar] [CrossRef] [PubMed]
- Lesclous, P. Prescription des antibiotiques en pratique bucco-dentaire-Recommandations Afssaps 2011. Méd. Buccale Chir. Buccale 2011, 17, 334–346. [Google Scholar] [CrossRef] [Green Version]
- Drisko, C.H. Non-Surgical Pocket Therapy: Pharmacotherapeutics. Ann. Periodontol. 1996, 1, 491–566. [Google Scholar] [CrossRef] [PubMed]
- Winkelhoff, A.J.V.; Rams, T.E.; Slots, J. Systemic Antibiotic Therapy in Periodontics. Periodontology 1996, 10, 45–78. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.A. Systemic Antibiotics in Periodontal Therapy. Aust. Dent. J. 2009, 54 (Suppl. 1), S96–S101. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S. EFP Workshop Participants and Methodological Consultants. Treatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice Guideline. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 4–60. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Polson, A. The Role of Local Drug Delivery in the Management of Periodontal Diseases: A Comprehensive Review. J. Periodontol. 1998, 69, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Butters, T.P.; Moore, L.S.P.; Castro-Sánchez, E.; Cooke, F.J.; Holmes, A.H. Exploring the coverage of antibiotic stewardship across UK clinical postgrad-uate training curricula. J. Antimicrob. Chemother. 2016, 71, 3284–3292. [Google Scholar] [CrossRef] [Green Version]
- Levin, C.; Thilly, N.; Dousak, M.; Beraud, G.; Klesnik, M.; Uhan, S.; Nathwani, D.; Beovic, B.; Pulcini, C. Perceptions, attitudes, and practices of French junior physicians regarding antibiotic use and resistance. Med. Mal. Infect. 2019, 49, 241–249. [Google Scholar] [CrossRef]
- Sánchez-Fabra, D.; Dyar, O.J.; Del Pozo, J.L.; Amiguet, J.A.; Colmenero, J.D.; Fariñas, M.D.C.; López-Medrano, F.; Portilla, J.; Praena, J.; Torre-Cisneros, J.; et al. En representación de ESGAP (ESCMID Study Group for Antimicrobial Stewardship). Perspective of Spanish medical students regarding undergraduate education in infectious diseases, bacterial resistance and antibiotic use in Spanish. Enferm. Infect. Microbiol. Clin. 2019, 37, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Mazzucco, W.; Marotta, C.; de Waure, C.; Gianluca, M.; Fasoletti, D.; Colicchio, A.; Luppi, D.; Pignatti, F.; Sessa, G.; Silenzi, A.; et al. Motivational aspects and level of satisfaction of Italian junior doctors with regard to knowledge and skills acquired attending specific general practice training courses. A national web survey. EuroMediterr. Biomed. J. 2017, 12, 77–86. [Google Scholar] [CrossRef]
- Mazzucco, W.; Lanza, G.; Gaglio, V.; Albanese, G.; Amata, O.; Casà, C.; Ferorelli, D.; Sessa, G.; Spina, E.; Silenzi, A.; et al. Medical workforce planning in a changing health context: Comparison between Italy and Europe. EuroMediterr. Biomed. J. 2019, 14, 49–55. [Google Scholar] [CrossRef]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016, 62, e51–e77. [Google Scholar] [CrossRef]
- Abbo, L.M.; Cosgrove, S.E.; Pottinger, P.S.; Pereyra, M.; Sinkowitz-Cochran, R.; Srinivasan, A.; Webb, D.J.; Hooton, T.M. Medical Students’ Perceptions and Knowledge about Antimicrobial Stewardship: How Are We Educating Our Future Prescribers? Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013, 57, 631–638. [Google Scholar] [CrossRef] [Green Version]
- Thompson, W.; Tonkin-Crine, S.; Pavitt, S.H.; McEachan, R.R.C.; Douglas, G.V.A.; Aggarwal, V.R.; Sandoe, J.A.T. Factors Associated with Antibiotic Prescribing for Adults with Acute Conditions: An Umbrella Review across Primary Care and a Systematic Review Focusing on Primary Dental Care. J. Antimicrob. Chemother. 2019, 74, 2139–2152. [Google Scholar] [CrossRef] [Green Version]
- Doron, S.; Davidson, L.E. Antimicrobial Stewardship. Mayo Clin. Proc. 2011, 86, 1113–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khattri, S.; Nagraj, S.K.; Arora, A.; Eachempati, P.; Kusum, C.K.; Bhat, K.G.; Johnson, T.M.; Lodi, G. Adjunctive Systemic Antimicrobials for the Non-Surgical Treatment of Periodontitis. Cochrane Database Syst. Rev. 2020, 11, CD012568. [Google Scholar] [CrossRef] [PubMed]
- Satterfield, J.; Miesner, A.R.; Percival, K.M. The Role of Education in Antimicrobial Stewardship. J. Hosp. Infect. 2020, 105, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.S.; Pestotnik, S.L.; Classen, D.C.; Clemmer, T.P.; Weaver, L.K.; Orme, J.F.; Lloyd, J.F.; Burke, J.P. A Computer-Assisted Management Program for Antibiotics and Other Antiinfective Agents. N. Engl. J. Med. 1998, 338, 232–238. [Google Scholar] [CrossRef] [Green Version]
- Richards, M.J.; Robertson, M.B.; Dartnell, J.G.A.; Duarte, M.M.; Jones, N.R.; Kerr, D.A.; Lim, L.-L.; Ritchie, P.D.; Stanton, G.J.; Taylor, S.E. Impact of a Web-Based Antimicrobial Approval System on Broad-Spectrum Cephalosporin Use at a Teaching Hospital. Med. J. Aust. 2003, 178, 386–390. [Google Scholar] [CrossRef]
- Agwu, A.L.; Lee, C.K.K.; Jain, S.K.; Murray, K.L.; Topolski, J.; Miller, R.E.; Townsend, T.; Lehmann, C.U. A World Wide Web-Based Antimicrobial Stewardship Program Improves Efficiency, Communication, and User Satisfaction and Reduces Cost in a Tertiary Care Pediatric Medical Center. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2008, 47, 747–753. [Google Scholar] [CrossRef] [Green Version]
- Ministère de la Santé: Comité Interministériel. Available online: https://www.hygienes.net/ministere-de-la-sante/comite-interministeriel (accessed on 6 March 2021).
- Légifrance: Le Service Public de la Diffusion du Droit. Available online: https://www.legifrance.gouv.fr/loda/id/JORFTEXT000039654152/2021-03-07/ (accessed on 6 March 2021).
- Réseau Sentinelles. Available online: https://websenti.u707.jussieu.fr/sentiweb/ (accessed on 6 March 2021).
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A New Classification Scheme for Periodontal and Peri-Implant Diseases and Conditions-Introduction and Key Changes from the 1999 Classification. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Armitage, G.C. Development of a Classification System for Periodontal Diseases and Conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.A.; Sa’at, N.; Sidik, T.M.I.T.A.B. Determination of Minimum Sample Size Requirement for Multiple Linear Regression and Analysis of Covariance Based on Experimental and Non-experimental Studies. Epidemiol. Biostat. Public Health 2017, 14, 117. [Google Scholar] [CrossRef]



| Characteristics | n | % | |
|---|---|---|---|
| Date of graduation (DDS) | <5 yrs | 77 | 28.3 |
| 5–10 yrs | 57 | 21 | |
| 10–20 yrs | 66 | 24.3 | |
| >20 yrs | 72 | 26.4 | |
| Location of graduation | France | 241 | 88.6 |
| Abroad | 31 | 11.4 | |
| Postgraduate background | Postgraduate certificate in periodontology | 109 | 40.1 |
| Other university degree in periodontology and oral implantology | 96 | 35.3 | |
| Current or former clinical lectureship | 75 | 25.6 | |
| Attendance at specialty congresses (SFPIO/EFP) | 183 | 67.3 | |
| Other training | 68 | 25 | |
| Type of professional practice | Academic position/ hospital activity | 81 | 29.8 |
| Self-employed | 224 | 82.3 | |
| Salaried | 75 | 25.6 | |
| Other | 10 | 3.7 | |
| “specialized/orientated” practice in Periodontology | Yes | 155 | 57 |
| No | 117 | 43 | |
| Type of periodontal care provided | Prophylaxis | 263 | 96.7 |
| Non-surgical periodontal treatment | 263 | 96.7 | |
| Surgical periodontal treatment | 177 | 65 | |
| Number of periodontitis patients treated per week | <5 patients per week | 95 | 34.9 |
| 5–10 patients per week | 78 | 28.7 | |
| >10 patients per week | 99 | 36.4 | |
| Items | All Respondents (n = 272) | “Specialized/ Orientated” Practice (n = 155) | General Practice (n = 117) | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-Value | ||
| Knowledge of national guidelines | 210 | 77.2 | 90 | 58.1 | 47 | 40.2 | <0.01 | |
| Recent exposure to training (<5 yrs) | 116 | 42.7 | 40 | 25.8 | 26 | 22.2 | n.s. | |
| Knowledge of the local antimicrobial products available on the market | Minocyclin (Parocline®) | 188 | 69.1 | 114 | 73.5 | 74 | 63.2 | n.s. |
| Chlorhexidine (Periochip®) | 83 | 30.5 | 63 | 40.6 | 20 | 17.1 | <0.001 | |
| Chlorhexidine + xantham (Chlo-Site®) | 26 | 9.6 | 17 | 11 | 9 | 7.7 | n.s. | |
| Neither | 70 | 25.8 | 32 | 20.6 | 38 | 32.5 | <0.05 | |
| Use of local antimicrobial systems | Minocyclin (Parocline®) | 60 | 22.1 | 42 | 27.1 | 18 | 15.4 | <0.05 |
| Chlorhexidine (Periochip®) | 12 | 4.4 | 5 | 3.2 | 7 | 6 | n.s. | |
| Chlorhexidine + xantham (Chlo-Site®) | 2 | 0.7 | 1 | 0.6 | 1 | 0.9 | n.s. | |
| Neither | 203 | 74.6 | 109 | 70.3 | 94 | 80.3 | n.s. | |
| As first-line treatment | never | 233 | 85.7 | 132 | 85.2 | 101 | 86.3 | n.s. |
| occasionally | 32 | 11.8 | 19 | 12.2 | 13 | 11.1 | ||
| often | 4 | 1.5 | 2 | 1.3 | 2 | 1.7 | ||
| very often | 3 | 1.1 | 2 | 1.3 | 1 | 0.9 | ||
| As second-line treatment | never | 204 | 75 | 108 | 69.7 | 96 | 82 | n.s. |
| occasionally | 61 | 22.4 | 42 | 27.1 | 19 | 16.2 | ||
| often | 5 | 1.8 | 4 | 2.6 | 1 | 0.9 | ||
| very often | 2 | 0.7 | 1 | 0.6 | 1 | 0.9 | ||
| Barriers to application of local antimicrobials | Lack of EBD | 133 | 49.4 | 77 | 49.7 | 56 | 47.9 | n.s. |
| Lack of experience | 110 | 40.9 | 47 | 30.3 | 63 | 53.8 | <0.001 | |
| High cost | 43 | 16 | 25 | 16.1 | 18 | 15.4 | n.s. | |
| impractical | 9 | 3.3 | 7 | 4.5 | 2 | 1.7 | n.s. | |
| Lack of outcomes | 52 | 19.3 | 37 | 23.9 | 15 | 12.8 | <0.05 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | n.a. | |
| Items | All Respondents | “Specialized/Orientated” Practice (n = 59) | General Practice (n = 38) | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-Value | ||
| Mild to moderate Periodontitis | never | 87 | 91.6 | 52 | 88.1 | 35 | 92.1 | n.s. |
| occasionally | 8 | 8.4 | 7 | 11.9 | 3 | 7.9 | ||
| often | 0 | 0 | 0 | 0 | 0 | 0 | ||
| very often | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Severe Periodontitis | never | 63 | 66.3 | 35 | 59.3 | 30 | 79 | n.s. |
| occasionally | 28 | 29.5 | 21 | 35.6 | 7 | 18.4 | ||
| often | 1 | 1 | 0 | 0 | 1 | 2.6 | ||
| very often | 3 | 3.2 | 3 | 5.1 | 0 | 0 | ||
| Localized aggressive periodontitis | never | 45 | 46.4 | 23 | 39 | 22 | 57.9 | n.s. |
| occasionally | 37 | 38.1 | 25 | 42.4 | 12 | 31.5 | ||
| often | 10 | 10.3 | 8 | 13.5 | 2 | 5.3 | ||
| very often | 5 | 5.1 | 3 | 5.1 | 2 | 5.3 | ||
| Generalized aggressive periodontitis | never | 59 | 62.8 | 32 | 54.2 | 30 | 78.9 | n.s. |
| occasionally | 24 | 25.5 | 19 | 32.2 | 5 | 13.2 | ||
| often | 7 | 7.4 | 4 | 6.8 | 3 | 7.9 | ||
| very often | 4 | 4.2 | 4 | 6.8 | 0 | 0 | ||
| Necrotizing periodontitis | never | 82 | 88.2 | 50 | 84.7 | 36 | 94.8 | n.s. |
| occasionally | 6 | 6.4 | 5 | 8.5 | 1 | 2.6 | ||
| often | 3 | 3.2 | 2 | 3.4 | 1 | 2.6 | ||
| very often | 2 | 2.1 | 2 | 3.4 | 0 | 0 | ||
| Periodontal abscess | never | 71 | 73.2 | 39 | 66.1 | 32 | 84.2 | n.s. |
| occasionally | 19 | 19.6 | 14 | 23.7 | 5 | 13.2 | ||
| often | 5 | 5.1 | 4 | 6.8 | 1 | 2.6 | ||
| very often | 2 | 2.1 | 2 | 3.4 | 0 | 0 | ||
| Unstandardized Coefficients | Standardized Coefficients | t | p-Value | ||
|---|---|---|---|---|---|
| B | Std. Error | beta | |||
| Number of periodontitis patients treated per week | 0.381 | 0.263 | 0.224 | 9.715 | <0.001 |
| Date of graduation (DDS) | −0.212 | 0.071 | −0.171 | 3.625 | 0.003 |
| Post graduate certificate in periodontology | 0.423 | 0.185 | 0.144 | 2.290 | 0.023 |
| Specialized/orientated practice | 0.287 | 0.180 | 0.099 | 1.592 | 0.112 |
| Unstandardized Coefficients | Standardized Coefficients | t | p-Value | ||
|---|---|---|---|---|---|
| B | Std. Error | beta | |||
| Date of graduation (DDS) | −0.408 | 0.108 | −0.208 | −3.775 | <0.001 |
| Post graduate certificate in periodontology | 0.695 | 0.286 | 0.149 | 2.428 | 0.016 |
| Academic position/ hospital activity | 1.298 | 0.290 | 0.277 | 4.477 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agossa, K.; Sy, K.; Mainville, T.; Gosset, M.; Jeanne, S.; Grosgogeat, B.; Siepmann, F.; Loingeville, F.; Dubar, M. Antibiotic Use in Periodontal Therapy among French Dentists and Factors Which Influence Prescribing Practices. Antibiotics 2021, 10, 303. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10030303
Agossa K, Sy K, Mainville T, Gosset M, Jeanne S, Grosgogeat B, Siepmann F, Loingeville F, Dubar M. Antibiotic Use in Periodontal Therapy among French Dentists and Factors Which Influence Prescribing Practices. Antibiotics. 2021; 10(3):303. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10030303
Chicago/Turabian StyleAgossa, Kevimy, Kadiatou Sy, Théo Mainville, Marjolaine Gosset, Sylvie Jeanne, Brigitte Grosgogeat, Florence Siepmann, Florence Loingeville, and Marie Dubar. 2021. "Antibiotic Use in Periodontal Therapy among French Dentists and Factors Which Influence Prescribing Practices" Antibiotics 10, no. 3: 303. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10030303






