Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Survey Method
2.3. Survey Data Analysis
2.4. Qualitative Research Method
3. Results
3.1. Survey Results
3.1.1. Knowledge and Awareness of Appropriate Use of Antibiotics
3.1.2. Awareness of Antibiotic Resistance and Knowledge of Outcomes of Antibiotic Resistance
3.1.3. Expectations Regarding Treatment for Cough or Common Cold
3.1.4. Preferences for Alternatives to Receiving an Antibiotic
3.2. Qualitative Results
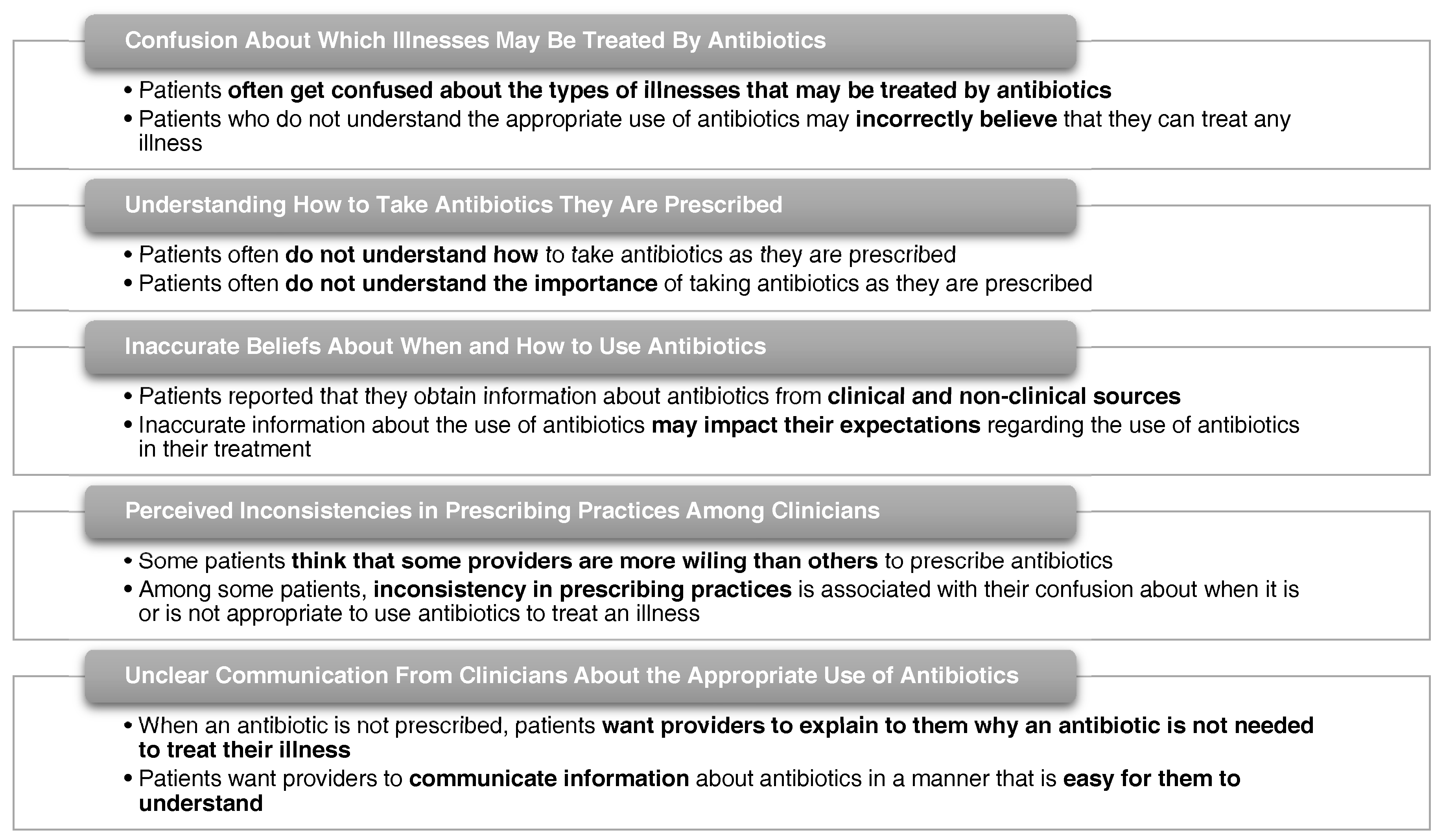
3.2.1. Confusion about Which Illnesses May Be Treated by Antibiotics
3.2.2. Understanding How to Take Antibiotics as They Are Prescribed
3.2.3. Inaccurate Beliefs about When and How to Use Antibiotics
3.2.4. Perceived Inconsistencies in Prescribing Practices Among Clinicians
3.2.5. Unclear Information from Clinicians about Appropriate Use of Antibiotics
4. Discussion
Strengths and Limitations of Study
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention Office of Infectious Disease. Antibiotic Resistance Threats in the United States. 2013. Available online: http://www.cdc.gov/drugresistance/threat-report-2013 (accessed on 2 February 2017).
- Ventola, C.L. The antibiotic resistance crisis: Part 2: Management strategies and new agents. P & T 2015, 40, 344–352. [Google Scholar]
- Center for Disease Dynamics, Economics & Policy. The State of the World’s Antibiotics. 2015. Available online: https://www.cddep.org/publications/state_worlds_antibiotics_2015/ (accessed on 2 February 2017).
- Institute of Medicine (US) Forum on Emerging Infections. The Resistance Phenomenon in Microbes and Infectious Disease Vectors: Implications for Human Health and Strategies for Containment: Workshop Summary. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/books/NBK97138/ (accessed on 5 June 2017).
- The Pew Charitable Trusts. Antibiotic Use in Outpatient Settings: Health Experts Create National Targets to Reduce Unnecessary Antibiotic Prescriptions. Available online: http://www.pewtrusts.org/en/research-and-analysis/reports/2016/05/antibiotic-use-in-outpatient-settings (accessed on 3 April 2017).
- Drekonja, D.M.; Filice, G.A.; Greer, N.; Olson, A.; MacDonald, R.; Rutks, I.; Wilt, T.J. Antimicrobial stewardship in outpatient settings: A systematic review. Infect. Control Hosp. Epidemiol. 2015, 36, 142–152. [Google Scholar] [CrossRef] [PubMed]
- MacDougall, C.; Polk, R.E. Antimicrobial stewardship programs in health care systems. Clin. Microbiol. Rev. 2005, 18, 638–656. [Google Scholar] [CrossRef] [PubMed]
- Gaarslev, C.; Yee, M.; Chan, G.; Fletcher-Lartey, S.; Khan, R. A mixed methods study to understand patient expectations for antibiotics for an upper respiratory tract infection. Antimicrob. Resist. Infect. Control. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Sirota, M.; Round, T.; Samaranayaka, S.; Kostopoulou, O. Expectations for antibiotics increase their prescribing: Causal evidence about localized impact. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2017, 36, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Cole, A. GPs feel pressurised to prescribe unnecessary antibiotics, survey finds. BMJ 2014. [Google Scholar] [CrossRef] [PubMed]
- Coenen, S.; Michiels, B.; Renard, D.; Denekens, J.; van Royen, P. Antibiotic prescribing for acute cough: The effect of perceived patient demand. Br. J. Gen. Pract. 2006, 56, 183–190. [Google Scholar] [PubMed]
- Coenen, S.; Francis, N.; Kelly, M.; Hood, K.; Nuttall, J.; Little, P.; Verheij, T.J.; Melbye, H.; Goossens, H.; Butler, C.C.; et al. Are patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute cough. PLoS ONE 2013, 8, e76691. [Google Scholar]
- Cals, J.W.L.; Boumans, D.; Lardinois, R.J.M.; Gonzales, R.; Hopstaken, R.M.; Butler, C.C.; Dinant, G.J. Public beliefs on antibiotics and respiratory tract infections: An internet-based questionnaire study. Br. J. Gen. Pract. 2007, 57, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Watkins, L.K.F.; Sanchez, G.V.; Albert, A.P.; Roberts, R.M.; Hicks, L.A. Knowledge and attitudes regarding antibiotic use among adult consumers, adult Hispanic consumers, and health care providers—United States, 2012–2013. Morb. Mortal. Wkly. Rep. 2015, 64, 767–770. [Google Scholar] [CrossRef]
- Macfarlane, J.; Holmes, W.; Macfarlane, R.; Britten, N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: Questionnaire study. BMJ 1997, 315, 1211–1214. [Google Scholar] [CrossRef] [PubMed]
- Brookes-Howell, L.; Hood, K.; Cooper, L.; Coenen, S.; Little, P.; Verheij, T.; Godycki-Cwirko, M.; Melbye, H.; Krawczyk, J.; Borras-Santos, A.; et al. Clinical influences on antibiotic prescribing decisions for lower respiratory tract infection: A nine country qualitative study of variation in care. BMJ Open 2012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, P.; Dorward, M.; Warner, G.; Stephens, K.; Senior, J.; Moore, M. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referral, and prescribing in primary care: Nested observational study. BMJ 2004. [Google Scholar] [CrossRef] [PubMed]
- Faber, M.S.; Heckenbach, K.; Velasco, E.; Eckmanns, T. Antibiotics for the common cold: Expectations of Germany’s general population. Euro Surveill. 2010. [Google Scholar] [CrossRef]
- Eng, J.V.; Marcus, R.; Hadler, J.L.; Imhoff, B.; Vugia, D.J.; Cieslak, P.R.; Zell, E.; Deneen, V.; McCombs, K.G.; Zansky, S.M.; et al. Consumer attitudes and use of antibiotics. Emerg. Infect. Dis. 2003, 9, 1128–1135. [Google Scholar]
- McNulty, C.A.M.; Lecky, D.M.; Hawking, M.K.D.; Roberts, C.; Quigley, A.; Butler, C.C. How much information about antibiotics do people recall after consulting in primary care? Fam. Pract. 2016, 33, 395–400. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey. 2015. Available online: http://apps.who.int/medicinedocs/documents/s22245en/s22245en.pdf (accessed on 28 September 2017).
- Fusch, P.K.; Ness, L.R. Are We There Yet? Data Saturation in Qualitative Research. Available online: http://tqr.nova.edu/wp-content/uploads/2015/09/fusch1.pdf (accessed on 25 September 2017).
- Vallin, M.; Polyzoi, M.; Marrone, G.; Rosales-Klintz, S.; Tegmark Wisell, K.; Stålsby Lundborg, C. Knowledge and attitudes towards antibiotic use and resistance—A latent class analysis of a Swedish population-based sample. PLoS ONE 2016, 11, e0152160. [Google Scholar] [CrossRef] [PubMed]
- You, J.H.; Yau, B.; Choi, K.C.; Huang, Q.R.; Lee, S.S. Public knowledge, attitudes, and behavior on antibiotic use: A telephone survey in Hong Kong. Infection 2008, 36, 153–157. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Special Eurobarometer 338. Antimicrobial Resistance. November—December 2009; TNS Opinion & Social; European Commission: Brussels, Belgium, 2010; Available online: https://ec.europa.eu/health//sites/health/files/antimicrobial_resistance/docs/ebs_338_en.pdf (accessed on 2 October 2017).
| Characteristics | n | % |
|---|---|---|
| All | 190 | |
| Age group | ||
| 24 or under | 16 | 8.4 |
| 25–34 | 43 | 22.6 |
| 35–44 | 44 | 23.2 |
| 45–54 | 31 | 16.3 |
| 55–64 | 25 | 13.2 |
| 65 or above | 31 | 16.3 |
| Gender | ||
| Male | 43 | 22.6 |
| Female | 147 | 77.4 |
| Parent of child taking antibiotic in past 2 years | ||
| Yes | 47 | 24.7 |
| No | 143 | 75.3 |
| Education | ||
| College Education | 134 | 70.5 |
| No College Education | 56 | 29.5 |
| Race | ||
| Non-Hispanic White | 135 | 71.1 |
| Non-Hispanic Black | 31 | 16.3 |
| Hispanic | 12 | 6.3 |
| Others | 12 | 6.3 |
| Characteristics | Antibiotics Work Extremely/Very/Somewhat Well For | When Someone Uses antibiotics When It Is Not Needed | ||||||
|---|---|---|---|---|---|---|---|---|
| Infections from Bacteria Such as Strep Throat Or Some Sinus Infections | Infections from a Virus Such as the Flu or the Common Cold | The Antibiotic Will Not Work Well in Treating that Person’s Illness the Next Time | It Can Weaken How Well the Antibiotic Will Work FOR Other People in the Future | |||||
| n (%) | p-Value * | n (%) | p-Value * | n (%) | p-Value * | n (%) | p-Value * | |
| All | 169 (88.9) | 101 (53.2) | 128 (67.4) | 101 (53.2) | ||||
| Gender | 0.580 | 0.491 | 0.466 | 0.224 | ||||
| Male | 37 (86.0) | 25 (58.1) | 27 (62.8) | 19 (44.2) | ||||
| Female | 132 (89.8) | 76 (51.7) | 101 (68.7) | 82 (55.8) | ||||
| Parent of child taking antibiotic in past 2 years | 0.604 | 0.740 | 1.000 | 0.866 | ||||
| Yes | 43 (91.5) | 26 (55.3) | 32 (68.1) | 24 (51.1) | ||||
| No | 126 (88.1) | 75 (52.4) | 96 (67.1) | 77 (53.8) | ||||
| Education | 0.021 | 0.526 | 0.028 | 0.038 | ||||
| College Education | 124 (92.5) | 69 (51.5) | 97 (72.4) | 78 (58.2) | ||||
| No College Education | 45 (80.4) | 32 (57.1) | 31 (55.4) | 23 (41.1) | ||||
| Characteristics | When You Have a Cough or a Common Cold, You Would Expect Your Provider to Give You Antibiotic | ||
|---|---|---|---|
| OR | 95% CI | p-Value | |
| Knowledge of appropriate use of antibiotics | |||
| Yes | - | - | - |
| No | 2.76 | (1.67–4.57) | <0.001 |
| Age (per 1 point increase) | 0.97 | (0.95–1.00) | 0.030 |
| Gender | |||
| Male | - | - | - |
| Female | 0.75 | (0.49–1.16) | 0.199 |
| Education | |||
| College Education | - | - | - |
| No College Education | 1.43 | (0.96–2.13) | 0.079 |
| Characteristics | If They Do Not Give You an Antibiotic, What Could Your Provider Do to Make You Feel Better? | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Suggest an Over-The-Counter Medicine That Could Help My Symptoms | Give Me an Order for a Medicine That Could Help My Symptoms | Tell Me Where I Could Learn more about My Illness (such as a Website or Handout) | Call me in 24 to 48 h to See If I Feel Better | Give Me Coupons for an Over-The-Counter Medicine That Could Help My Symptoms | ||||||
| n (%) | p * | n (%) | p * | n (%) | p * | n (%) | p * | n (%) | p * | |
| All | 149 (78.4) | 115 (60.5) | 69 (36.3) | 57 (30.0) | 69 (36.3) | |||||
| Gender | 0.140 | 1.000 | 0.107 | 0.185 | 0.212 | |||||
| Male | 30 (69.8) | 26 (60.5) | 11 (25.6) | 9 (20.9) | 12 (27.9) | |||||
| Female | 119 (81.0) | 89 (60.5) | 58 (39.5) | 48 (32.7) | 57 (38.8) | |||||
| Parent of child taking antibiotic in past 2 years | 0.689 | 0.126 | 1.000 | 1.000 | 0.301 | |||||
| Yes | 38 (80.9) | 33 (70.2) | 17 (36.2) | 14 (29.8) | 14 (29.8) | |||||
| No | 111 (77.6) | 82 (57.3) | 52 (36.4) | 43 (30.1) | 55 (38.5) | |||||
| Education | 0.004 | 1.000 | 0.186 | 0.023 | 0.020 | |||||
| College Education | 113 (84.3) | 81 (60.4) | 53 (39.6) | 47 (35.1) | 56 (41.8) | |||||
| No College Education | 36 (64.3) | 34 (60.7) | 16 (28.6) | 10 (17.9) | 13 (23.2) | |||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davis, M.E.; Liu, T.-L.; Taylor, Y.J.; Davidson, L.; Schmid, M.; Yates, T.; Scotton, J.; Spencer, M.D. Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study. Antibiotics 2017, 6, 23. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics6040023
Davis ME, Liu T-L, Taylor YJ, Davidson L, Schmid M, Yates T, Scotton J, Spencer MD. Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study. Antibiotics. 2017; 6(4):23. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics6040023
Chicago/Turabian StyleDavis, Marion E., Tsai-Ling Liu, Yhenneko J. Taylor, Lisa Davidson, Monica Schmid, Traci Yates, Janice Scotton, and Melanie D. Spencer. 2017. "Exploring Patient Awareness and Perceptions of the Appropriate Use of Antibiotics: A Mixed-Methods Study" Antibiotics 6, no. 4: 23. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics6040023






