Prevalence of OXA-Type β-Lactamase Genes among Carbapenem-Resistant Acinetobacter baumannii Clinical Isolates in Thailand
Abstract
:1. Introduction
2. Results
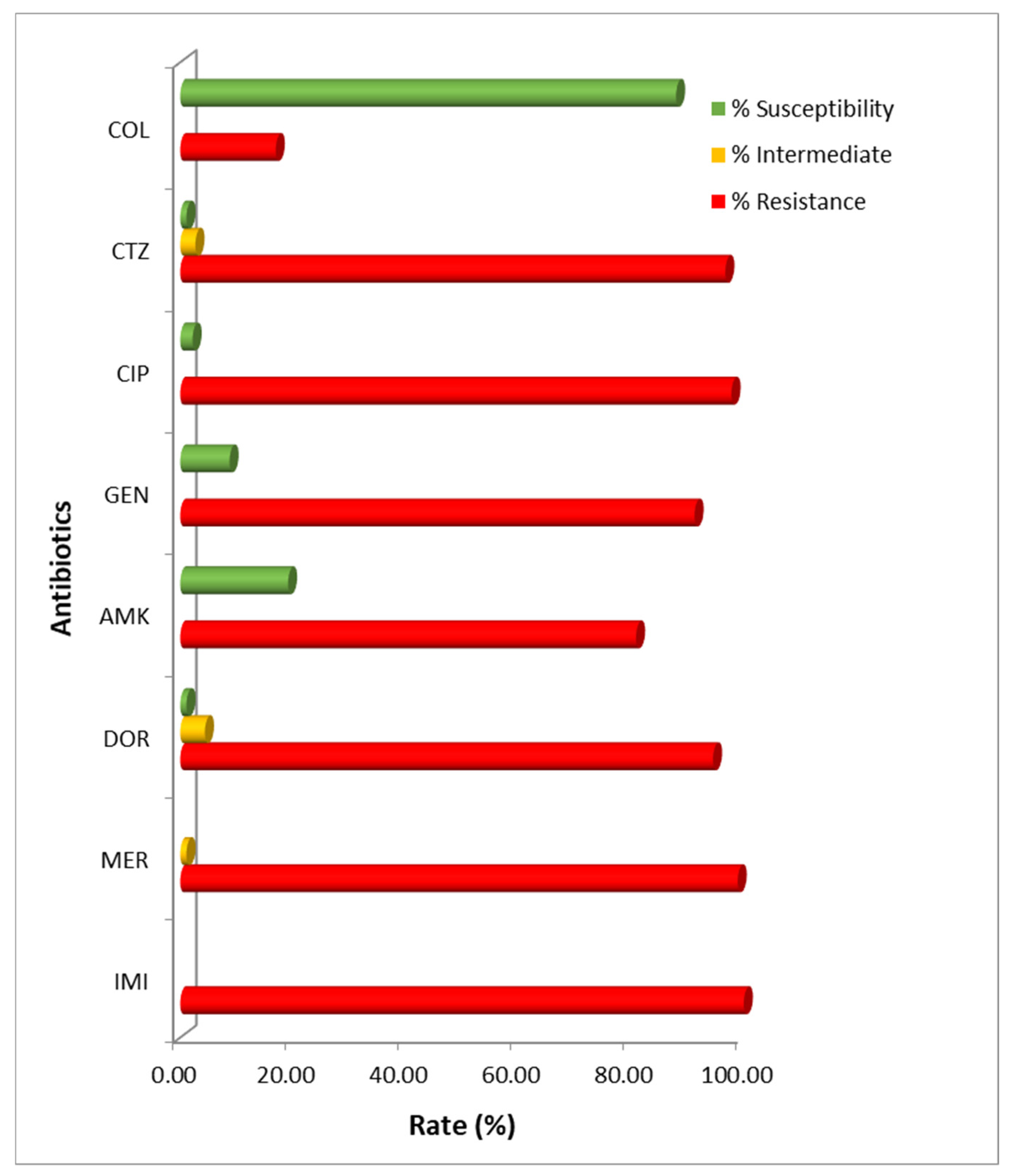
2.1. Antimicrobial Susceptibility Pattern
2.2. Distribution of OXA-Type Carbapenemases
2.3. Molecular Typing by Sequence Type (ST) Analysis
3. Discussion
4. Materials and Methods
4.1. Bacterial Collection and Identification
4.2. Antimicrobial Susceptibility Testing
4.3. Genotypic Determination of Carbapenemases
4.4. Multi-Locus Sequence Typing Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter baumannii: Emergence of a successful pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tosi, M.; Roa, E.; De Biasi, S.; Munari, E.; Venturelli, S.; Coloretti, I.; Biagioni, E.; Cossarizza, A.; Girardis, M. Multidrug resistant bacteria in critically ill patients: A step further antibiotic therapy. J. Emerg. Crit. Care Med. 2018, 2, 103. [Google Scholar] [CrossRef]
- Moubareck, C.A.; Halat, D.H. Insights into Acinetobacter baumannii: A review of microbiological, virulence, and resistance traits in a threatening nosocomial pathogen. Antibiotics 2020, 9, 119. [Google Scholar] [CrossRef] [Green Version]
- Rice, L.B. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J. Infect. Dis. 2008, 197, 1079–1081. [Google Scholar] [CrossRef]
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging strategies to combat ESKAPE Pathogens in the Era of Antimicrobial Resistance: A Review. Front. Microbiol. 2019, 10, 539. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.R.; Lee, J.H.; Park, M.; Park, K.S.; Bae, I.K.; Kim, Y.B.; Cha, C.J.; Jeong, B.C.; Lee, S.H. Biology of Acinetobacter baumannii: Pathogenesis, antibiotic resistance mechanisms, and prospective treatment option. Front. Cell Infect. Microbiol. 2017, 7, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seifert, H.; Stefanik, D.; Olesky, M.; Higgins, P.G. In vitro activity of the novel fluorocycline TP-6076 against carbapenem-resistant Acinetobacter baumannii. Int. J. Antimicrob. Agents. 2020, 55, 105829. [Google Scholar] [CrossRef]
- El-Badawy, M.F.; Abdelwahab, S.F.; Alghamdi, S.A.; Shohayeb, M.M. Characterization of phenotypic and genotypic traits of carbapenem-resistant Acinetobacter baumannii clinical isolates recovered from a tertiary care hospital in Taif, Saudi Arabia. Infect. Drug Resist. 2019, 12, 3113–3124. [Google Scholar] [CrossRef] [Green Version]
- Paiboonvong, T.; Rodjun, V.; Houngsaitong, J.; Chomnawang, M.; Montakantikul, P.; Chulavatnatol, S. Comparative in vitro activity of sitafloxacin against multidrug-resistant and carbapenem-resistant Acinetobacter baumannii clinical isolates in Thailand. Pharm. Sci. Asia. 2020, 47, 37–42. [Google Scholar] [CrossRef]
- Elshamy, A.A.; Aboshanab, K.M. A review on bacterial resistance to carbapenems: Epidemiology, detection and treatment options. Future Sci. OA 2020, 6, FSO438. [Google Scholar] [CrossRef] [Green Version]
- Gordon, N.C.; Wareham, D.W. Multidrug-resistant Acinetobacter baumannii: Mechanisms of virulence and resistance. Int. J. Antimicrob. Agents. 2010, 35, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, S.I.; Kim, Y.R.; Hong, K.W.; Wie, S.H.; Park, Y.J. Carbapenem-resistant Acinetobacter baumannii: Diversity of resistant mechanisms and risk factors for infection. Epidemiol. Infect. 2012, 140, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.F.; Lan, C.Y. Antimicrobial resistance in Acinetobacter baumannii: From bench to bedside. World J. Clin. Cases. 2014, 2, 787–814. [Google Scholar] [CrossRef] [PubMed]
- Codjoe, F.S.; Donkor, E.S. Carbapenem resistance: A review. Med. Sci. 2017, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Paton, R.; Miles, R.S.; Hood, J.; Amyes, S.G.; Miles, R.S. ARI 1: Beta-lactamase-mediated imipenem resistance in Acinetobacter baumannii. Int. J. Antimicrob. Agents. 1993, 2, 81–87. [Google Scholar] [CrossRef]
- Evans, B.A.; Amyes, G.B. OXA β-lactamases. Clin. Microbiol. Rev. 2014, 27, 241–263. [Google Scholar] [CrossRef] [Green Version]
- Al-Bayssari, C.; Dabboussi, F.; Hamze, M. Detection of expanded-spectrum β-lactamases in Gram-negative bacteria in the 21st century. Expert Rev. Anti-Infect. Ther. 2015, 13, 1139–1158. [Google Scholar] [CrossRef]
- D’Onofrio, V.; Conzemius, R.; Varda-Brkić, D.; Bogdan, M.; Grisold, A.; Gyssens, I.C.; Bedenić, B.; Barišić, I. Epidemiology of colistin-resistant, carbapenemase-producing Enterobacteriaceae and Acinetobacter baumannii in Croatia. Infect. Genet. Evol. 2020, 81, 104263. [Google Scholar] [CrossRef]
- AlAmri, A.M.; AlQurayan, A.M.; Sebastian, T.; AlNimr, A.M. Molecular surveillance of multidrug-resistant Acinetobacter baumannii. Curr. Microbiol. 2020, 77, 335–342. [Google Scholar] [CrossRef]
- Kuo, S.C.; Huang, W.C.; Huang, T.W.; Wang, H.Y.; Lai, J.F.; Chen, T.L.; Lauderdale, T.L. Molecular epidemiology of emerging blaOXA-23-Like- and blaOXA-24-Like-carrying Acinetobacter baumannii in Taiwan. Antimicrob. Agents Chemother. 2018, 62, e01215-17. [Google Scholar] [CrossRef] [Green Version]
- Poirel, L.; Nordmann, P. Genetic structures at the origin of acquisition and expression of the carbapenem-hydrolyzing oxacillinase gene blaOXA-58 in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2006, 50, 1442–1448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suárez, C.J.; Lolans, K.; Villegas, M.V.; Quinn, J.P. Mechanisms of resistance to beta-lactams in some common Gram-negative bacteria causing nosocomial infections. Expert. Rev. Anti Infect. Ther. 2005, 3, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Turton, J.F.; Woodford, N.; Glover, J.; Yarde, S.; Kaufmann, M.E.; Pitt, T.L. Identification of Acinetobacter baumannii by detection of the blaOXA-51-like carbapenemase gene intrinsic to this species. J. Clin. Microbiol. 2006, 44, 2974–2976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. 2017. Available online: https://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf (accessed on 1 October 2020).
- Oliveira, M.S.; Prado, G.V.; Costa, S.F.; Grinbaum, R.S.; Levin, A.S. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J. Antimicrob. Chemother. 2008, 61, 1369–1375. [Google Scholar] [CrossRef]
- Garnacho-Montero, J.; Amaya-Villar, R.; Ferrándiz-Millón, C.; Díaz-Martín, A.; López-Sánchez, J.M.; Gutiérrez-Pizarraya, A. Optimum treatment strategies for carbapenem-resistant Acinetobacter baumannii bacteremia. Expert Rev. Anti-Infect. Ther. 2015, 13, 769–777. [Google Scholar] [CrossRef]
- Kamolvit, W.; Sidjabat, H.E.; Paterson, D.L. Molecular epidemiology and mechanisms of carbapenem resistance of Acinetobacter spp. in Asia and Oceania. Microb. Drug Resist. 2015, 21, 424–434. [Google Scholar] [CrossRef]
- Yaowen, C.; Guangxin, L.; Ying, X.; Yanhong, W.; Min, S.; Chi, Z.; Wei, Z.; Jinwei, H.; Jingni, Y.; Xu, J.; et al. Characterization of carbapenem-resistant Acinetobacter baumannii isolates in a Chinese teaching hospital. Front. Microbiol. 2015, 6, 910. [Google Scholar] [CrossRef]
- Vijayakumar, S.; Mathur, P.; Kapil, A.; Das, B.K.; Ray, P.; Gautam, V.; Sistla, S.; Parija, S.C.; Walia, K.; Ohri, V.C.; et al. Molecular characterization & epidemiology of carbapenem-resistant Acinetobacter baumannii collected across India. Indian J. Med. Res. 2019, 149, 240–246. [Google Scholar] [CrossRef]
- Ibrahim, M.E. Prevalence of Acinetobacter baumannii in Saudi Arabia: Risk factors, antimicrobial resistance patterns and mechanisms of carbapenem resistance. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 1. [Google Scholar] [CrossRef]
- Rolain, J.M.; Loucif, L.; Al-Maslamani, M.; Elmagboul, E.; Al-Ansari, N.; Taj-Aldeen, S.; Shaukat, A.; Ahmedullah, H.; Hamed, M. Emergence of multidrug-resistant Acinetobacter baumannii producing OXA-23 carbapenemase in Qatar. New Microbes New Infect. 2016, 11, 47–51. [Google Scholar] [CrossRef] [Green Version]
- Leungtongkam, U.; Thummeepak, R.; Wongprachan, S.; Thongsuk, P.; Kitti, T.; Ketwong, K.; Runcharoen, C.; Chantratita, N.; Sitthisak, S. Dissemination of bla(OXA-23), bla(OXA-24), bla(OXA-58), and bla(NDM-1) genes of Acinetobacter baumannii isolates from four tertiary hospitals in Thailand. Microb. Drug Resist. 2018, 24, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Bartual, S.G.; Seifert, H.; Hippler, C.; Luzon, M.A.D.; Wisplinghoff, H.; Rodríguez-Valera, F. Development of a Multilocus Sequence Typing Scheme for Characterization of Clinical Isolates of Acinetobacter baumannii. J. Clin. Microbiol. 2005, 43, 4382–4390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saffari, F.; Monsen, T.; Karmostaji, A.; Azimabad, F.B.; Widerström, M. Significant spread of extensively drug-resistant Acinetobacter baumannii genotypes of clonal complex 92 among intensive care unit patients in a university hospital in southern Iran. J. Med. Microbiol. 2017, 66, 1656–1662. [Google Scholar] [CrossRef] [PubMed]
- Nawfal Dagher, T.; Al-Bayssari, C.; Chabou, S.; Antar, N.; Diene, S.M.; Azar, E.; Rolain, J.M. Investigation of multidrug-resistant ST2 Acinetobacter baumannii isolated from Saint George hospital in Lebanon. BMC Microbiol. 2019, 19, 29. [Google Scholar] [CrossRef]
- Dijkshoorn, L.; Aucken, H.; Gerner-Smidt, P.; Janssen, P.; Kaufmann, M.E.; Garaizar, J.; Ursing, J.; Pitt, T.L. Comparison of outbreak and nonoutbreak Acinetobacter baumannii strains by genotypic and phenotypic methods. J. Clin. Microbiol. 1996, 34, 1519–1525. [Google Scholar] [CrossRef] [Green Version]
- Kumar, S.; Patil, P.P.; Singhal, L.; Ray, P.; Patil, P.B. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii isolates reveals the emergence of blaOXA-23 and blaNDM-1 encoding international clones in India. Infect. Genet. Evol. 2019, 75, 103986. [Google Scholar] [CrossRef]
- Rao, M.; Rashid, F.; Shukor, S.; Hashim, R.; Ahmad, N. Detection of antimicrobial resistance genes associated with carbapenem resistance from the whole-genome sequence of Acinetobacter baumannii isolates from Malaysia. Can. J. Infect. Dis. Med. 2020, 2020, 5021064. [Google Scholar] [CrossRef] [Green Version]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI Document M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020; pp. 46–49. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [Green Version]
- Falah, F.; Shokoohizadeh, L.; Adabi, M. Molecular identification and genotyping of Acinetobacter baumannii isolated from burn patients by PCR and ERIC-PCR. Scars Burn Health 2019, 5, 2059513119831369. [Google Scholar] [CrossRef] [Green Version]
- Poirel, L.; Walsh, T.R.; Cuvillier, V.; Nordmann, P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn. Microbiol. Infect. Dis. 2011, 70, 119–123. [Google Scholar] [CrossRef]

| Isolation Site | No. of Isolates (%) |
|---|---|
| Sputum | 147 (80.33) |
| Pus | 17 (9.29) |
| Blood | 8 (4.37) |
| Urine | 9 (4.92) |
| Tissue | 2 (1.09) |
| Total | 183 (100) |
| Antibiotics | MIC Range a | MIC50 a | MIC90 a | Percentage (n) | ||
|---|---|---|---|---|---|---|
| Susceptible | Intermediate | Resistant | ||||
| Carbapenems | ||||||
| Imipenem | 8–1028 | 32 | 64 | 0.00 (0) | 0.00 (0) | 100.00 (183) |
| Meropenem | 4–256 | 16 | 64 | 0.00 (0) | 1.09 (2) | 98.91 (181) |
| Doripenem | 0.125–256 | 16 | 64 | 1.09 (2) | 4.37 (8) | 94.54 (173) |
| Ciprofloxacin | 0.125–>512 | 64 | 256 | 2.19 (4) | 0.00 (0) | 97.81 (179) |
| Ceftazidime | 4–>512 | 512 | >512 | 1.09 (2) | 2.69 (5) | 96.17 (176) |
| Gentamicin | 0.5–>512 | >512 | >512 | 8.74 (16) | 0.00 (0) | 91.26 (167) |
| Amikacin | 1–>2048 | >2048 | >2048 | 19.13 (35) | 0.00 (0) | 80.87 (148) |
| Colistin | 0.0625–512 | 0.25 | 4 | 87.98 (152) | 0.00 (0) | 16.94 (31) |
| Gene | Primer Sequences (5′ to 3′) | Product Size (bp) | |||
|---|---|---|---|---|---|
| Forward | Tm (°C) | Reverse | Tm (°C) | ||
| Class D | |||||
| oxacillinases | |||||
| blaoxa-23-like | GAT CGG ATT GGA | 60 | ATT TCT GAC CGC | 56 | 501 bp |
| GAA CCA GA | ATT TCC AT | ||||
| blaoxa-24/40-like | TAA TGC TTT GAT | 60 | AGT TGA GCG | 58 | 246 bp |
| CCC TTA AA | CAT CTT GG | ||||
| blaoxa-51-like | TAA TGC TTT GAT | 58 | TGG ATT GCA CTT | 58 | 353 bp |
| CGG CCT TG | CAT CTT GG | ||||
| blaoxa-58-like | AAG TAT TGG GGC | 60 | CCC CTC TGC GCT | 64 | 599 bp |
| TTG TGC TG | CTA CAT AC | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thirapanmethee, K.; Srisiri-a-nun, T.; Houngsaitong, J.; Montakantikul, P.; Khuntayaporn, P.; Chomnawang, M.T. Prevalence of OXA-Type β-Lactamase Genes among Carbapenem-Resistant Acinetobacter baumannii Clinical Isolates in Thailand. Antibiotics 2020, 9, 864. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9120864
Thirapanmethee K, Srisiri-a-nun T, Houngsaitong J, Montakantikul P, Khuntayaporn P, Chomnawang MT. Prevalence of OXA-Type β-Lactamase Genes among Carbapenem-Resistant Acinetobacter baumannii Clinical Isolates in Thailand. Antibiotics. 2020; 9(12):864. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9120864
Chicago/Turabian StyleThirapanmethee, Krit, Thayapa Srisiri-a-nun, Jantana Houngsaitong, Preecha Montakantikul, Piyatip Khuntayaporn, and Mullika Traidej Chomnawang. 2020. "Prevalence of OXA-Type β-Lactamase Genes among Carbapenem-Resistant Acinetobacter baumannii Clinical Isolates in Thailand" Antibiotics 9, no. 12: 864. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9120864




