Novel Approaches to Detect and Treat Biofilms within the Root Canals of Teeth: A Review
Abstract
:1. Introduction
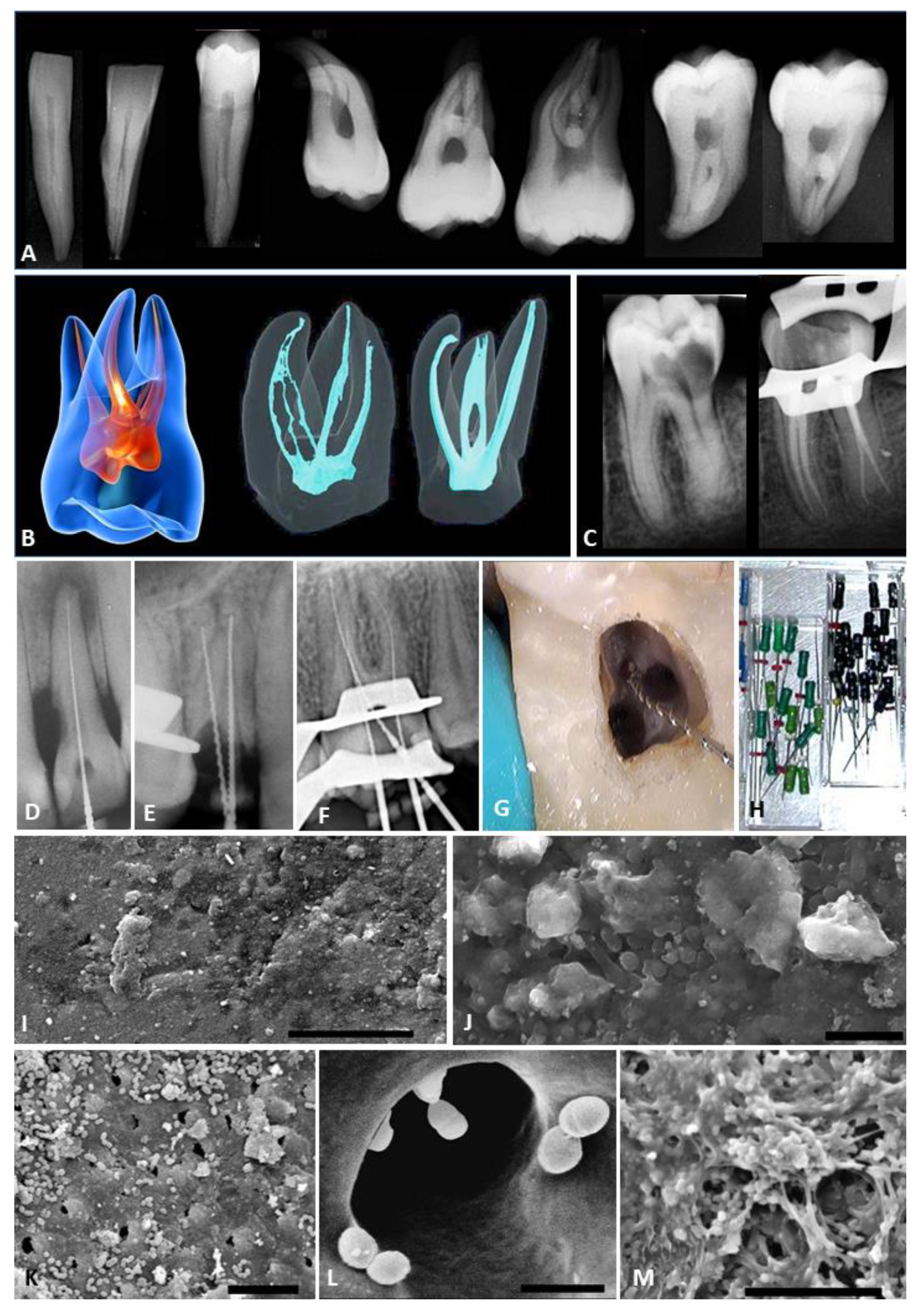
2. The Challenge of Biofilms in the Root Canal System
3. Real-Time Assessment of Endodontic Biofilms Using Fluorescence Methods
3.1. Fluorescence Using Ultraviolet Light or Visible Violet Light
3.2. Fluorescence Using Visible Red Light
4. Improved Antimicrobial Irrigant Solutions
5. Antimicrobial Medicaments
6. Conclusions
Funding
Conflicts of Interest
References
- Byström, A.; Sundqvist, G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand. J. Dent. Res. 1981, 89, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Hommez, G.M.G.; Verhelst, R.; Claeys, G.; Vaneechoutte, M.; De Moor, R.J.G. Investigation of the effect of the coronal restoration quality on the composition of the root canal microflora in teeth with apical periodontitis by means of T-RFLP analysis. Int. Endod. J. 2004, 37, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F.; Rôças, I.N. Polymerase chain reaction based analysis of microorganisms associated with failed endodontic treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 85–94. [Google Scholar] [CrossRef]
- Siqueira, J.F.; Rôças, I.N. Molecular methods to explore endodontic infections: Part 2- redefining the endodontic microbiota. J. Endod. 2005, 31, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Chu, F.C.; Leung, W.K.; Tsang, P.C.; Chow, T.W.; Samaranayake, L.P. Identification of cultivable microorganisms from root canals with apical periodontitis following two-visit endodontic treatment with antibiotics/steroid or calcium hydroxide dressings. J. Endod. 2006, 32, 17–23. [Google Scholar] [CrossRef]
- Tomson, P.L.; Simon, S.R. Contemporary cleaning and shaping of the root canal system. Prim. Dent. J. 2016, 5, 46–53. [Google Scholar] [CrossRef]
- Orstavik, D. Root canal disinfection: A review of concepts and recent developments. Aust. Endod. J. 2003, 29, 70–74. [Google Scholar] [CrossRef]
- Wu, M.K.; Wesselink, P.R. Efficacy of three techniques in cleaning the apical portion of curved root canals. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 79, 492–496. [Google Scholar] [CrossRef]
- Sundqvist, G.; Figdor, D.; Persson, S.; Sjögren, U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 86–93. [Google Scholar] [CrossRef]
- Molander, A.; Reit, C.; Dahlén, G.; Kvist, T. Microbial status of root filled teeth with apical periodontitis. Int. Endod. J. 1998, 31, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.F.A.; Pinheiro, C.R.; Gadê-Neto, E.L.; Sousa, E.L.R.; Ferraz, C.C.R.; Zaia, A.A.; Teixeira, F.B.; Souza-Filho, F.J. Microbiological examination of infected dental root canals. Oral Microbiol. Immunol. 2004, 19, 71–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundqvist, G. Taxonomy, ecology, and pathogenicity of the root canal flora. Oral Surg. Oral Med. Oral Pathol. 1994, 78, 522–530. [Google Scholar] [CrossRef]
- Creti, R.; Imperi, M.; Bertuccini, L.; Fabretti, F.; Orefici, G.; Di Rosa, R.; Baldassarri, L. Survey for virulence determinants among Enterococcus faecalis isolated from different sources. J. Med. Microbiol. 2004, 53, 13–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Athanassiadis, B.; Abbott, P.V.; Walsh, L.J. The use of calcium hydroxide, antibiotics and biocides as antimicrobial medicaments in endodontics. Aust. Dent. J. 2007, 52 (Suppl. S1), S64–S82. [Google Scholar] [CrossRef]
- Murray, B.E. The life and times of the Enterococcus. Clin. Microbiol. Rev. 1990, 3, 46–65. [Google Scholar] [CrossRef] [PubMed]
- Sedgley, C.; Lennan, D.B.; Clewell, D.B. Prevalence, phenotype, and genotype of oral enterococci. Oral Microbiol. Immunol. 2004, 19, 95–101. [Google Scholar] [CrossRef]
- Sedgley, C.M.; Molander, A.; Flannagan, S.E.; Nagel, A.C.; Appelbe, O.K.; Clewell, D.B.; Dahlén, G. Virulence, phenotype and genotype characteristics of endodontic Enterococcus spp. Oral Microbiol. Immunol. 2005, 20, 10–19. [Google Scholar] [CrossRef]
- Herzog, D.B.; Hosny, N.A.; Niazi, S.A.; Koller, G.; Cook, R.J.; Foschi, F.; Watson, T.F.; Mannocci, F.; Festy, F. Rapid bacterial detection during endodontic treatment. J. Dent. Res. 2017, 96, 626–632. [Google Scholar] [CrossRef]
- Conrads, G.; Gharbia, S.E.; Gulabivala, K.; Lampert, F.; Shah, H.N. The use of 16S r DNA directed PCR for the detection of endodontpathogenic bacteria. J. Endod. 1997, 23, 433–438. [Google Scholar] [CrossRef]
- Woo, P.C.; Lau, S.K.; Teng, J.L.; Tse, H.; Yuen, K.Y. Then and now: Use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin. Microbiol. Infect. 2008, 14, 908–934. [Google Scholar] [CrossRef] [Green Version]
- Pini, R.; Salimbeni, R.; Vannini, M.; Cavalieri, S.; Barone, R.; Clauser, C. Laser dentistry: Root canal diagnostic technique based on ultraviolet-induced fluorescence spectroscopy. Lasers Surg. Med. 1989, 9, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Shakibaie, F.; Walsh, L.J. Violet and blue light-induced green fluorescence emissions from dental caries. Aust. Dent. J. 2016, 61, 464–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, L.J. Caries diagnosis aided by fluorescence. In Dental Caries—Diagnosis and Management; Arkanslan, Z., Ed.; InTech Publishers: Rijeka, Croatia, 2018; pp. 97–115. [Google Scholar] [CrossRef] [Green Version]
- Shakibaie, F.; Walsh, L.J. Optical diagnostics to improve periodontal diagnosis and treatment. In Periodontology and Dental Implantology; Manakil, J., Ed.; InTech Publishers: Rijeka, Croatia, 2018; pp. 73–86. [Google Scholar] [CrossRef] [Green Version]
- Sarkissian, A.; Le, A.N. Fiber optic fluorescence microprobe for endodontic diagnosis. J. Dent. Educ. 2005, 69, 633–638. [Google Scholar] [PubMed]
- Shakibaie, F.; Lamard, L.; Rubinzstein-Dunlop, H.; Walsh, L.J. Application of fluorescence spectroscopy for microbial detection to enhance clinical investigations. In Photon Counting; Britun, N., Nikiforov, A., Eds.; InTech Publishers: Rijeka, Croatia, 2018; pp. 225–242. [Google Scholar] [CrossRef] [Green Version]
- Odor, T.M.; Chandler, N.P.; Watson, T.F.; Ford, T.R.; McDonald, F. Laser light transmission in teeth: A study of the patterns in different species. Int. Endod. J. 1999, 32, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Chandler, N.P.; Pitt Ford, T.R.; Watson, T.F. Pattern of transmission of laser light through carious molar teeth. Int. Endod. J. 2001, 34, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Chandler, N.P.; Pitt Ford, T.R.; Monteith, B.D. Laser light passage through restored and carious posterior teeth. J. Oral Rehabil. 2014, 41, 630–634. [Google Scholar] [CrossRef]
- Sainsbury, A.L.; Bird, P.S.; Walsh, L.J. DIAGNOdent laser fluorescence assessment of endodontic infection. J. Endod. 2009, 35, 1404–1407. [Google Scholar] [CrossRef]
- Shakibaie, F.; Walsh, L.J. Surface area and volume determination of subgingival calculus using laser fluorescence. Lasers Med. Sci. 2014, 29, 519–524. [Google Scholar] [CrossRef]
- Shakibaie, F.; Walsh, L.J. Performance differences in the detection of subgingival calculus by laser fluorescence devices. Lasers Med. Sci. 2015, 30, 2281–2286. [Google Scholar] [CrossRef]
- Ho, Q.V.; George, R.; Sainsbury, A.L.; Kahler, W.A.; Walsh, L.J. Laser fluorescence assessment of the root canal using plain and conical optical fibers. J. Endod. 2010, 36, 119–122. [Google Scholar] [CrossRef]
- George, R.; Walsh, L.J. Performance assessment of novel side firing flexible optical fibers for dental applications. Lasers Surg. Med. 2009, 41, 214–221. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Walsh, L.J. Performance assessment of novel side firing safe tips for endodontic applications. J. Biomed. Opt. 2011, 16, 048004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, O.A.; Boessler, C.; Paqué, F. Root canal preparation with a novel nickel-titanium instrument evaluated with micro-computed tomography: Canal surface preparation over time. J. Endod. 2010, 36, 1068–1072. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, E.A.; Carlon, D.; Meghil, M.M.; El-Awady, A.R.; Niu, L.; Bergeron, B.E.; Susin, L.; Cutler, C.W.; Pashley, D.H.; Tay, F.R. Efficacy of 3D conforming nickel titanium rotary instruments in eliminating canal wall bacteria from oval-shaped root canals. J. Dent. 2015, 43, 597–604. [Google Scholar] [CrossRef]
- Gavini, G.; Santos, M.D.; Caldeira, C.L.; Machado, M.E.L.; Freire, L.G.; Iglecias, E.F.; Peters, O.A.; Candeiro, G.T.M. Nickel-titanium instruments in endodontics: A concise review of the state of the art. Braz. Oral Res. 2018, 32 (Suppl. S1), e67. [Google Scholar] [CrossRef]
- Estrela, C.; Estrela, C.R.; Barbin, E.L.; Spanó, J.C.E.; Marchesan, M.A.; Pécora, J.D. Mechanism of action of sodium hypochlorite. Braz. Dent. J. 2002, 13, 113–117. [Google Scholar] [CrossRef]
- Clegg, M.S.; Vertucci, F.J.; Walker, C.; Belanger, M.; Britto, L.R. The effect of exposure to irrigant solutions on apical dentine biofilms in vitro. J. Endod. 2006, 32, 434–437. [Google Scholar] [CrossRef]
- Wright, P.P.; Walsh, L.J. Optimizing antimicrobial agents in endodontics. In Antibacterial Agents; Kumavath, R., Ed.; InTech Publishers: Rijeka, Croatia, 2017; pp. 87–108. [Google Scholar] [CrossRef] [Green Version]
- Baron, A.; Lindsey, K.; Sidow, S.J.; Dickinson, D.; Chuang, A.; McPherson, J.C. Effect of a benzalkonium chloride surfactant–sodium hypochlorite combination on elimination of Enterococcus faecalis. J. Endod. 2016, 42, 145–149. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Shen, Y.; Ma, J.; Haapasalo, M. The effect of detergents on the antibacterial activity of disinfecting solutions in dentin. J. Endod. 2012, 38, 948–953. [Google Scholar] [CrossRef]
- Xavier, A.C.; Martinho, F.C.; Chung, A.; Oliveira, L.D.; Jorge, A.O.; Valera, M.C.; Carvalho, C.A. One-visit versus two-visit root canal treatment: Effectiveness in the removal of endotoxins and cultivable bacteria. J. Endod. 2013, 39, 959–964. [Google Scholar] [CrossRef]
- Peters, O.A.; Bardsley, S.; Fong, J.; Pandher, G.; DiVito, E. Disinfection of root canals with photon-initiated photoacoustic streaming. J. Endod. 2011, 37, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- George, R.; Meyers, I.A.; Walsh, L.J. Laser activation of endodontic irrigants with improved conical laser fiber tips for removing smear layer in the apical third of the root canal. J. Endod. 2008, 34, 1524–1527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, L.J.; George, R. Activation of alkaline irrigation fluids in endodontics. Materials (Basel) 2017, 10, 1214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, P.P.; Kahler, B.; Walsh, L.J. The effect of heating to intracanal temperature on the stability of sodium hypochlorite admixed with etidronate or EDTA for continuous chelation. J. Endod. 2019, 45, 57–61. [Google Scholar] [CrossRef]
- Wright, P.P.; Scott, S.; Kahler, B.; Walsh, L.J. Organic tissue dissolution in clodronate and etidronate mixtures with sodium hypochlorite. J. Endod. 2019, 46, 289–294. [Google Scholar] [CrossRef]
- Wright, P.P.; Cooper, C.; Kahler, B.; Walsh, L.J. From an assessment of multiple chelators, clodronate has potential for use in continuous chelation. Int. Endod. J. 2020, 53, 122–134. [Google Scholar] [CrossRef]
- Fedorowicz, Z.; Nasser, M.; Sequeira-Byron, P.; de Souza, R.F.; Carter, B.; Heft, M. Irrigants for non-surgical root canal treatment in mature permanent teeth. Cochrane Database Syst. Rev. 2012, 9, CD008948. [Google Scholar] [CrossRef]
- George, R.; Walsh, L.J. Apical extrusion of root canal irrigants when using Er:YAG and Er,Cr:YSGG lasers with optical fibers: An in vitro dye study. J. Endod. 2008, 34, 706–708. [Google Scholar] [CrossRef] [Green Version]
- Saviola, G.; Abdi-Ali, L.; Comini, L.; Dalle-Carbonare, L.G. Use of clodronate in the management of osteoarthritis: An update. J. Biol. Regul. Homeost. Agents 2019, 33, 1315–1320. [Google Scholar] [CrossRef]
- Iranmanesh, F.; Parirokh, M.; Haghdoost, A.A.; Abbott, P.V. Effect of corticosteroids on pain relief following root canal treatment: A systematic review. Iran. Endod. J. 2017, 12, 123–130. [Google Scholar] [CrossRef]
- Mostafa, M.E.; El-Shrief, Y.A.; Anous, W.I.; Hassan, M.W.; Salamah, F.T.A.; El Boghdadi, R.M.; El-Bayoumi, M.A.A.; Seyam, R.M.; Abd-El-Kader, K.G.; Amin, S.A.W. Postoperative pain following endodontic irrigation using 1.3% versus 5.25% sodium hypochlorite in mandibular molars with necrotic pulps: A randomized double-blind clinical trial. Int. Endod. J. 2020, 53, 154–166. [Google Scholar] [CrossRef] [PubMed]
- Athanassiadis, B.; Abbott, P.V.; George, N.; Walsh, L.J. In vitro study of the inactivation by dentine of some antimicrobial endodontic medicaments and their bases. Aust. Dent. J. 2010, 55, 298–305. [Google Scholar] [CrossRef]
- Athanassiadis, B.; Abbott, P.V.; George, N.; Walsh, L.J. An in vitro study of the anti-microbial activity of some endodontic medicaments and their bases against Enterococcus faecalis biofilms. Aust. Dent. J. 2010, 55, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Athanassiadis, B.; Walsh, L.J. Aspects of solvent chemistry for calcium hydroxide medicaments. Materials (Basel) 2017, 10, 1219. [Google Scholar] [CrossRef] [Green Version]
- Shetty, S.; Kahler, S.L.; Kahler, B. Alkaline material effects on roots of teeth. Materials (Basel) 2017, 10, 1412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahler, S.L.; Shetty, S.; Andreasen, F.M.; Kahler, B. The effect of long-term dressing with calcium hydroxide on the fracture susceptibility of teeth. J. Endod. 2018, 44, 464–469. [Google Scholar] [CrossRef]
- Cao, Y.; Naseri, M.; He, Y.; Xu, C.; Walsh, L.J.; Ziora, Z.M. Non-antibiotic antimicrobial agents to combat biofilm-forming bacteria. J. Glob. Antimicrob. Resist. 2019. [Google Scholar] [CrossRef]
- Halkai, K.R.; Mudda, J.A.; Shivanna, V.; Rathod, V.; Halkai, R. Evaluation of antibacterial efficacy of fungal-derived silver nanoparticles against Enterococcus faecalis. Contemp. Clin. Dent. 2018, 9, 45–48. [Google Scholar] [CrossRef]
- Halkai, K.R.; Mudda, J.A.; Shivanna, V.; Rathod, V.; Halkai, R. Antibacterial efficacy of biosynthesized silver nanoparticles against Enterococcus faecalis biofilm: An in vitro study. Contemp. Clin. Dent. 2018, 9, 237–241. [Google Scholar] [CrossRef]
- Song, W.; Ge, S. Application of antimicrobial nanoparticles in dentistry. Molecules 2019, 24, 1033. [Google Scholar] [CrossRef] [Green Version]
- Bukhari, S.; Kim, D.; Liu, Y.; Karabucak, B.; Koo, H. Novel endodontic disinfection approach using catalytic nanoparticles. J. Endod. 2018, 44, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M.A.; Versiani, M.A.; De-Deus, G.; Dummer, P.M.H. A new system for classifying root and root canal morphology. Int. Endod. J. 2017, 50, 761–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Bacteria—summary
|
Gram-positive bacteria
|
Gram-negative bacteria
|
| Archaea, such as Methanobrevibacter oralis and M. filiformis. |
| Fungi, including Candida albicans |
| Method | Major Limitations |
|---|---|
| Physical debridement | |
| Hand endodontic files | Non-contact with walls of the root canal; instrument breakage |
| Rotary endodontic files | Limited contact with walls; excessive root structure removal |
| Ultrasonic endodontic files | Limited activation of irrigant fluid; apical fluid extrusion |
| Irrigant solutions | |
| Sodium hypochlorite | Chemical irritancy; chemical instability; instrument corrosion |
| Hydrogen peroxide | Chemical irritancy; interactions with other irrigant solutions |
| Chlorhexidine | Limited spectrum of activity; chemical degradation |
| EDTA | No antimicrobial actions; inactivates sodium hypochlorite |
| Medicament pastes | |
| Calcium hydroxide | Limited alkaline pH for aqueous preparations |
| Phenolic compounds | Limited spectrum of activity; chemical irritancy |
| Tetracyclines | Staining of roots from first generation tetracyclines |
| Clindamycin | Inherent resistance of E. faecalis; adverse reactions |
| Technology | Issues to Be Resolved |
|---|---|
| Fluorescence detection | Quenching of fluorescence emissions (e.g., by oxidants) Flexibility of optical fibers that penetrate the root canal system |
| Laser fluid agitation | Laser pulse patterns to optimize fluid agitation fluid extrusion |
| Sodium hypochlorite | Stabilizers and surfactants to optimize performance |
| Clodronate | Extent of anti-inflammatory actions |
| Phytochemicals | Spectrum of activity; irritancy and toxicity |
| Chitosan | Particle size; consistency of compositions |
| Metal nanoparticles | Penetration into biofilms; toxicity to the host |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walsh, L.J. Novel Approaches to Detect and Treat Biofilms within the Root Canals of Teeth: A Review. Antibiotics 2020, 9, 129. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9030129
Walsh LJ. Novel Approaches to Detect and Treat Biofilms within the Root Canals of Teeth: A Review. Antibiotics. 2020; 9(3):129. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9030129
Chicago/Turabian StyleWalsh, Laurence J. 2020. "Novel Approaches to Detect and Treat Biofilms within the Root Canals of Teeth: A Review" Antibiotics 9, no. 3: 129. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9030129





