Knowledge, Attitude, and Practices of Antibiotics and Antibiotic Resistance Among Chinese Pharmacy Customers: A Multicenter Survey Study
Abstract
:1. Introduction
2. Methodology
2.1. Survey Instrument
2.2. Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Ethics Approval and Consent to Participate
3. Results
3.1. Knowledge about Antibiotics
3.2. Attitude about Antibiotics
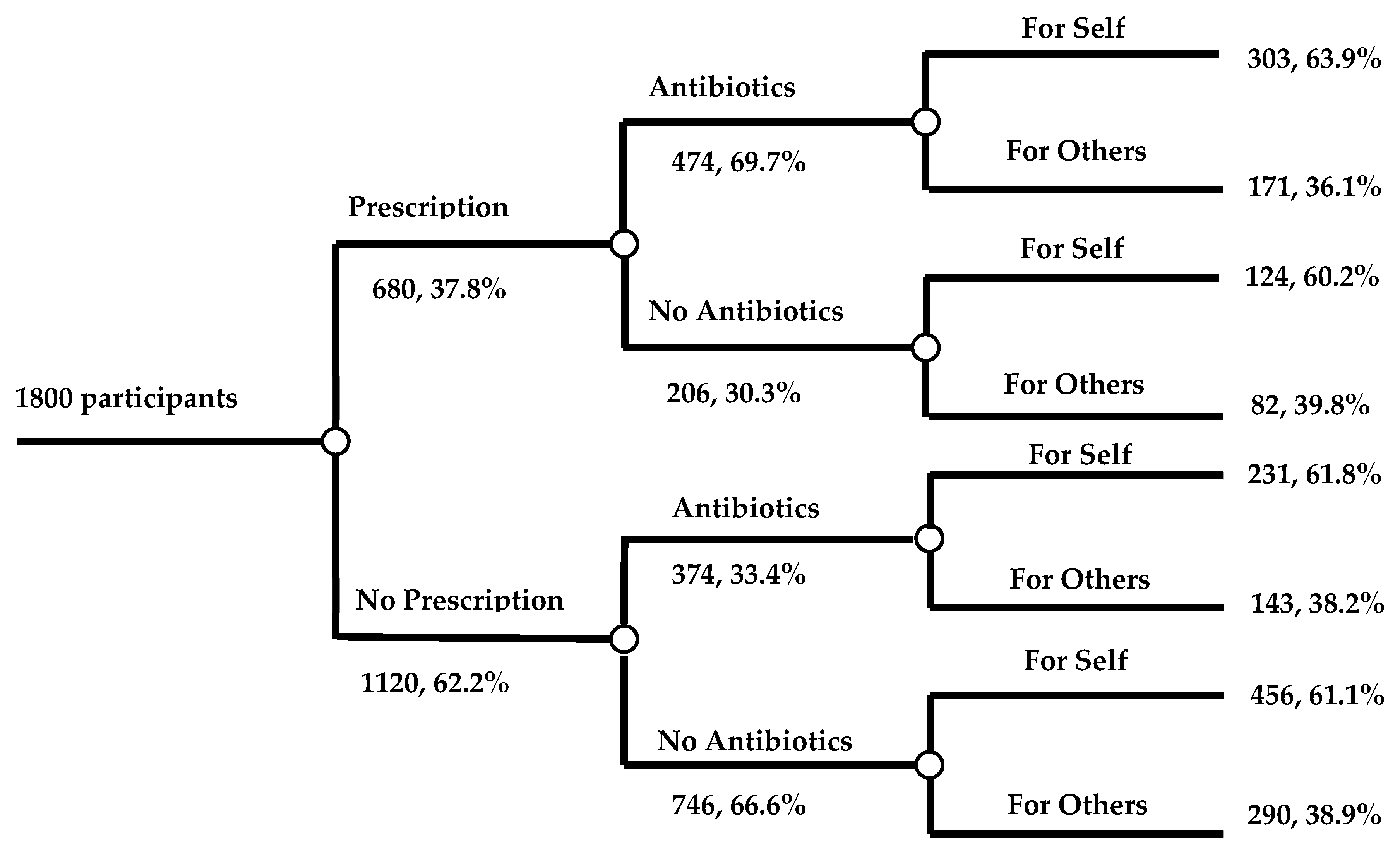
3.3. Practice about Antibiotics
3.4. Association of Median Scores of Participants with Demographic Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- O’NEILL, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. Available online: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (accessed on 25 December 2019).
- Septimus, E.J. Antimicrobial Resistance: An Antimicrobial/Diagnostic Stewardship and Infection Prevention Approach. Med. Clin. North Am. 2018, 102, 819–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayat, K.; Rosenthal, M.; Gillani, A.H.; Chang, J.; Ji, W.; Yang, C.; Jiang, M.; Zhao, M.; Fang, Y. Perspective of Key Healthcare Professionals on Antimicrobial Resistance and Stewardship Programs: A Multicenter Cross-Sectional Study From Pakistan. Front. Pharmacol. 2019, 10, 1520. [Google Scholar] [CrossRef]
- Hayat, K.; Rosenthal, M.; Zhu, S.; Gillani, A.H.; Chang, J.; Bogale, A.A.; Kabba, J.A.; Yang, C.; Jiang, M.; Zhao, M. Attitude of clinicians towards hospital-based antimicrobial stewardship programs: A multicenter cross-sectional study from Punjab, Pakistan. Expert Rev. Anti Infect. Ther. 2019, 17, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.; Wertheim, H.F.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance—the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef] [Green Version]
- Hayat, K.; Rosenthal, M.; Gillani, A.H.; Zhai, P.; Aziz, M.M.; Ji, W.; Fang, Y. Perspective of Pakistani Physicians towards Hospital Antimicrobial Stewardship Programs: A Multisite Exploratory Qualitative Study. Int. J. Environ. Res. Public Health. 2019, 16, 1565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antibiotic Resistance in Norway. 2017. Available online: https://www.fhi.no/en/op/hin/infectious-diseases/antibiotic-resistance-in-norway---p/#surveillance-of-antibiotic-resistance-in-norway (accessed on 15 December 2019).
- European Commission. EU Action on Antimicrobial Resistance. 2017. Available online: https://ec.europa.eu/health/amr/antimicrobial-resistance_en (accessed on 23 August 2019).
- Tangcharoensathien, V.; Chanvatik, S.; Sommanustweechai, A. Complex determinants of inappropriate use of antibiotics. Bull. World Health Organ. 2018, 96, 141–144. [Google Scholar] [CrossRef]
- The World Health Report 2007. A Safer Future: Global Public Health Security in the 21st Century. 2007. Available online: http://www.who.int/whr/2007/en/ (accessed on 27 August 2019).
- Goldstein, E.J. Beyond the target pathogen: Ecological effects of the hospital formulary. Curr. Opin. Infect. Dis. 2011, 24, S21–S31. [Google Scholar] [CrossRef]
- Qiao, M.; Ying, G.-G.; Singer, A.C.; Zhu, Y.G. Review of antibiotic resistance in China and its environment. Environ. Int. 2018, 11, 160–172. [Google Scholar] [CrossRef] [Green Version]
- Van Boeckel, T.P.; Gandra, S.; Ashok, A.; Caudron, Q.; Grenfell, B.T.; Levin, S.A.; Laxminarayan, R. Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data. Lancet Infect. Dis. 2014, 14, 742–750. [Google Scholar] [CrossRef]
- Li, J.; Song, X.; Yang, T.; Chen, Y.; Gong, Y.; Yin, X.; Lu, Z. Systematic Review of Antibiotic Prescription Associated With Upper Respiratory Tract Infections in China. Medicine 2016, 95, e3587. [Google Scholar] [CrossRef]
- Hu, F.; Zhu, D.; Wang, F.; Wang, M. Current Status and Trends of Antibacterial Resistance in China. Clin. Infect. Dis. 2018, 67, S128–S134. [Google Scholar] [CrossRef] [PubMed]
- He, Q.W.; Xu, X.H.; Lan, F.J.; Zhao, Z.C.; Wu, Z.Y.; Cao, Y.P.; Li, B. Molecular characteristic of mcr-1 producing Escherichia coli in a Chinese university hospital. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- State Food and Drug Administration. The five Prescription Sales Only Antibacterial Released by SFDA. 2004. Available online: http://eng.sfda.gov.cn/WS03/CL0757/61674.html (accessed on 23 August 2019).
- Saliba-Gustafsson, E.A.; Dunberger Hampton, A.; Zarb, P.; Orsini, N.; Borg, M.A.; Stålsby Lundborg, C. Factors associated with antibiotic prescribing in patients with acute respiratory tract complaints in Malta: A 1-year repeated cross-sectional surveillance study. BMJ Open 2019, 9, e032704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, J.; Ye, D.; Lv, B.; Jiang, M.; Zhu, S.; Yan, K.; Fang, Y. Sale of antibiotics without a prescription at community pharmacies in urban China: A multicentre cross-sectional survey. J. Antimicrob. Chemother. 2017, 72, 1235–1242. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. The Pursuit of Responsible Use of Medicines. 2012. Available online: https://www.who.int/medicines/publications/responsible_use/en/ (accessed on 23 December 2019).
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (accessed on 23 December 2019).
- Grigoryan, L.; Burgerhof, J.G.; Degener, J.E.; Deschepper, R.; Lundborg, C.S.; Monnet, D.L.; SAR Consortium. Attitudes, beliefs and knowledge concerning antibiotic use and self-medication: A comparative European study. Pharmacoepidemiol. Drug Saf. 2007, 16, 1234–1243. [Google Scholar] [CrossRef]
- Andre, M..; Vernby, A.; Berg, J.; Lundborg, C.S. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J. Antimicrob. Chemother. 2010, 65, 1292–1296. [Google Scholar] [CrossRef] [Green Version]
- Vallin, M.; Polyzoi, M.; Marrone, G.; Rosales-Klintz, S.; Wisell, K.T.; Lundborg, C.S. Knowledge and Attitudes towards Antibiotic Use and Resistance—A Latent Class Analysis of a Swedish Population-Based Sample. PLoS ONE 2016, 11, e0152160. [Google Scholar] [CrossRef] [Green Version]
- Jiangsu Provincial Bureau of Statistics. Jiangsu Statistical Yearbook 2015. 2016. Available online: http://www.jssb.gov.cn/2015nj/indexc.htm (accessed on 23 August 2019).
- Hunan Provincial Bureau of Statistics. Human Statistical Yearbook 2014. 2015. Available online: http://www.hntj.gov.cn/sjfb/tjnj/14tjnj/indexeh.htm (accessed on 23 August 2019).
- Shaanxi Provincial Bureau of Statistics. Shaanxi Statistical Yearbook 2015. 2016. Available online: http://www.shaanxitj.gov.cn/upload/2016/tongjinianj/2015/indexeh.htm (accessed on 23 August 2019).
- Waaseth, M.; Adan, A.; Røen, I.L.; Eriksen, K.; Stanojevic, T.; Halvorsen, K.H.; Ariansen, H. Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers—A cross-sectional study. BMC Public Health 2019, 19, 66–70. [Google Scholar] [CrossRef]
- Almohammed, R.A.; Bird, E.L. Public knowledge and behaviours relating to antibiotic use in Gulf Cooperation Council countries: A systematic review. J. Infect. Public Health 2019, 12, 159–166. [Google Scholar] [CrossRef]
- Al Omari, S.; Al Mir, H.; Wrayde, S.; Merhabi, S.; Dhaybi, I.; Jamal, S.; Al Atrouni, A. First Lebanese Antibiotic Awareness Week campaign: Knowledge, attitudes and practices towards antibiotics. J. Hosp. Infect. 2019, 101, 475–479. [Google Scholar] [CrossRef]
- Asghar, S.; Atif, M.; Mushtaq, I.; Malik, I.; Hayat, K. Factors associated with inappropriate dispensing of antibiotics among non-pharmacist pharmacy workers. Res. Soc. Adm. Pharm. 2019. [Google Scholar] [CrossRef] [PubMed]
- Zilinskas, G.; Tamasauskiene, L.; Tamasauskas, D. Analysis of citizens’ subjective perception of safe antibiotic use in European Union countries. J. Infect. Public Health 2019, 12, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Xi’an Municipal Human Resources and Social Security Bureau. List of Designated Retail Pharmacies in Xi’an. 2018. Available online: http://xahrss.xa.gov.cn/gk/bmcx/xafybddcl/17683.htm (accessed on 24 March 2019).
- Nanjing Administration for Market Regulation. Retail Pharmacy Enquiry System in Nanjing. 2018. Available online: http://49.65.0.143/njsjzx/businesshlw/zycx/index_view.jsp?sel=yplsxk&vh=medicalApparatus (accessed on 24 March 2019).
- Hunan Medical Products Administration Government. Retailed Pharmacies Enquiry System in Changsha. 2018. Available online: http://mpa.hunan.gov.cn/mpa/bsfw/sjcx/index.html (accessed on 24 March 2019).
- Gualano, M.R.; Gili, R.; Scaioli, G.; Bert, F.; Siliquini, R. General population’s knowledge and attitudes about antibiotics: A systematic review and meta-analysis. Pharmacoepidemiol. Drug Saf. 2015, 24, 2–10. [Google Scholar] [CrossRef]
- Awad, A.I.; Aboud, E.A. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS ONE 2015, 10, e0117910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Health and Health Commission. Notice of the General Office of the National Health and Health Commission on the Continuous Management of Clinical Application of Antibacterial Drugs. 2019. Available online: http://www.nhc.gov.cn/yzygj/s7659/201903/1d487eb7b7c74abc9fcb104f8b0905f2.shtml (accessed on 20 January 2020).
- National Health and Health Commission. Continuous Management of Antibacterial Agents in Clinical Application. 2018. Available online: http://www.nhc.gov.cn/xxgk/pages/viewdocument.jsp?dispatchDate=&staticUrl=/yzygj/s7659/201805/c79c998bdf8f4744858051cdfd1e6818.shtml (accessed on 20 January 2020).
- Hayat, K.; Li, P.; Rosenthal, M.; Xu, S.; Chang, J.; Gillani, A.H.; Cheng, A. Perspective of community pharmacists about community-based antimicrobial stewardship programs. A multicenter cross-sectional study from China. Expert Rev. Anti Infect. Ther. 2019, 12, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Finch, R.G.; Metlay, J.P.; Davey, P.G.; Baker, L.J. Educational interventions to improve antibiotic use in the community: Report from the International Forum on Antibiotic Resistance (IFAR) colloquium. Lancet Infect. Dis. 2002, 4, 44–53. [Google Scholar] [CrossRef]
- Gonzales, R.; Corbett, K.K.; Leeman-Castillo, B.A.; Glazner, J.; Erbacher, K.; Darr, C.A.; Kafadar, K. The “minimizing antibiotic resistance incolorado” project: Impact of patient education in improving antibiotic use in private office practices. Health Serv. Res. 2005, 40, 101–116. [Google Scholar] [CrossRef] [Green Version]
- Ranji, S.R.; Steinman, M.A.; Shojania, K.G.; Gonzales, R. Interventions to reduce unnecessary antibiotic prescribing—A systematic review and quantitative analysis. Med. Care 2008, 46, 847–862. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; Ferranti, R.; Mistretta, A. Pattern of antibiotic use in the community: νon-adherence and self-prescription rates in an Italian urban population. Mol. Med. Rep. 2012, 5, 1305–1310. [Google Scholar] [PubMed] [Green Version]
- Kennedy, J.; Tuleu, I.; Mackay, K. Unfilled prescriptions of medicare beneficiaries: Prevalence, reasons, and types of medicines prescribed. J. Manag. Care Pharm. 2008, 14, 553–560. [Google Scholar] [CrossRef] [Green Version]
- Ajzen, I. Attitudes, Personality, and Behavior; McGraw-Hill Education: New York, NY, USA, 2005. [Google Scholar]
- World Health Organization. Promoting Rational Use of Medicines: Core Components. 2016. Available online: http://apps.who.int/medicinedocs/collect/medicinedocs/pdf/h3011e/h3011e.pdf?ua=1 (accessed on 20 October 2019).
- Elong Ekambi, G.-A.; Okalla Ebongue, C.; Penda, I.C.; Nga, E.N.; Mpondo, E.M.; Moukoko, C.E.E. Knowledge, practices and attitudes on antibiotics use in Cameroon: Self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS ONE 2019, 14, e0212875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, D.; Chang, J.; Yang, C.; Yan, K.; Ji, W.; Aziz, M.M.; Fang, Y. How does the general public view antibiotic use in China? Result from a cross-sectional survey. Int. J. Clin. Pharm. 2017, 39, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Xu, S.; Zhu, S.; Li, Z.; Yu, J.; Zhang, Y.; Ross-Degnan, D. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: A mixed cross-sectional and longitudinal study. Lancet Infect. Dis. 2019, 19, 1345–1354. [Google Scholar] [CrossRef]
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 1059 | 58.8 |
| Female | 741 | 41.2 |
| Age (years) | ||
| 18–25 | 404 | 22.4 |
| 26–35 | 586 | 32.6 |
| 36–45 | 438 | 24.3 |
| 46–59 | 291 | 16.2 |
| >60 | 81 | 4.5 |
| Education | ||
| No formal education | 21 | 1.2 |
| Primary school | 47 | 2.6 |
| Junior high school | 168 | 9.3 |
| Senior high school | 363 | 20.2 |
| College and above | 1201 | 66.7 |
| Income (RMB) | ||
| <1000 | 218 | 12.1 |
| 1000–3000 | 326 | 18.1 |
| 3001–5000 | 587 | 32.6 |
| 5001–8000 | 411 | 22.9 |
| >8000 | 258 | 14.3 |
| Employment | ||
| Employed | 1091 | 60.7 |
| Self-employed | 258 | 14.3 |
| Unemployed | 112 | 6.2 |
| Student | 229 | 12.7 |
| Other | 110 | 6.1 |
| Question (Correct Answer) | Yes | No | Unclear | Median (IQR) |
|---|---|---|---|---|
| Antibiotics and anti-inflammatory medicines are the same (no) | 820 (45.6) | 642 (35.7) | 338 (18.7) | 2 (1) |
| Antibiotic can be used to treat bacterial diseases, i.e., pneumonia, typhoid, and wound infections (yes) | 1342 (74.6) | 161 (8.9) | 297 (16.5) | 1 (1) |
| Antibiotic can be used to treat common cold (no) | 949 (52.7) | 559 (31.1) | 292 (16.2) | 1 (1) |
| The antibiotics will not kill normal flora (no) | 403 (22.4) | 970 (53.9) | 427 (23.7) | 2 (0) |
| Unnecessary use of antibiotics is dangerous for health (yes) | 1396 (77.5) | 176 (9.8) | 228 (12.7) | 1 (0) |
| OTC use of antibiotics in pregnant women is safe (no) | 127 (7.1) | 1307 (72.6) | 366 (20.3) | 2 (0) |
| Antibiotics can be used along with tradition Chinese medicines (yes) | 319 (17.7) | 676 (37.6) | 805 (44.7) | 2 (1) |
| Question | 1-Strongly Agree; 5-Strongly Disagree. N (%) | Median (IQR) | ||||
|---|---|---|---|---|---|---|
| SA | A | N | D | SD | ||
| Costly antibiotics are more effective and have fewer side effects. | 95 (5.3) | 226 (12.6) | 582 (32.3) | 707 (39.3) | 190 (10.5) | 3 (1) |
| Costly antibiotics have fewer side effects. | 68 (3.8) | 247 (13.7) | 617 (34.3) | 695 (38.6) | 173 (9.6) | 3 (1) |
| Antibiotic use without a doctor’s prescription is safe. | 51 (2.8) | 248 (13.8) | 348 (19.3) | 824 (45.8) | 329 (18.3) | 4 (1) |
| Taking double dose of antibiotics can speed up the cure of diseases. | 48 (2.7) | 127 (7.0) | 324 (18.0) | 864 (48.0) | 437 (24.3) | 4 (1) |
| Taking many antibiotics produce the better result than one antibiotic. | 53 (2.9) | 164 (9.1) | 437 (24.3) | 784 (43.6) | 362 (20.1) | 4 (1) |
| The effectiveness of treatment would be reduced if a full course of antibiotics was not completed. | 185 (10.3) | 859 (47.7) | 441 (24.5) | 225 (12.5) | 90 (5.0) | 2 (1) |
| It is better to stop taking antibiotic when symptoms are improved. | 81 (4.5) | 386 (21.4) | 485 (27.0) | 693 (38.5) | 155 (8.6) | 3 (2) |
| The leftover antibiotics can be saved and used for the same symptoms again. | 83 (4.6) | 360 (20.0) | 553 (30.7) | 627 (34.9) | 177 (9.8) | 3 (1) |
| Question | Always N (%) | Often N (%) | Sometimes N (%) | Seldom N (%) | Never N (%) | Median (IQR) |
|---|---|---|---|---|---|---|
| I read the instructions in the package insert carefully before taking antibiotics. | 654 (36.3) | 563 (31.3) | 294 (16.3) | 214 (11.9) | 75 (4.2) | 2 (2) |
| I finish the full course of antibiotic treatment. | 401 (22.3) | 452 (25.1) | 572 (31.8) | 281 (15.6) | 94 (5.2) | 3 (1) |
| I change the dose during antibiotic treatment. | 68 (3.8) | 123 (6.8) | 501(27.8) | 516 (28.7) | 592 (32.9) | 4 (2) |
| I switch antibiotics during the course of treatment. | 66 (3.7) | 99 (5.5) | 415 (23.1) | 492 (27.3) | 728 (40.4) | 4 (2) |
| I keep leftover antibiotics at home in case of future need. | 294 (16.4) | 395 (21.9) | 436 (24.2) | 405 (22.5) | 270 (15.0) | 3 (2) |
| Variable | Median Knowledge Score (IQR) | p-Value | Median Attitude Score (IQR) | p-Value | Median Practice Score (IQR) | p-Value |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 2.00(1.00) | 0.28 | 3.50(1.00) | <0.001 | 3.00(2.00) | 0.58 |
| Female | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| Age (years) | ||||||
| 18–25 | 2.00(1.00) | 0.002 | 3.50(1.00) | <0.001 | 3.00(2.00) | 0.483 |
| 26–35 | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| 36–45 | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| 46–59 | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| >60 | 2.00(1.50) | 3.00(1.00) | 3.00(2.00) | |||
| Education | ||||||
| Out of School | 3.00(2.00) | <0.001 | 3.00(2.25) | <0.001 | 3.00(4.00) | 0.561 |
| Primary school | 2.00(2.00) | 3.00(1.00) | 3.00(1.00) | |||
| Junior high school | 2.00(2.00) | 3.00(1.00) | 3.00(1.75) | |||
| Senior high school | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| College and above | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| Income (RMB) | ||||||
| <1000 | 2.00(0.25) | 0.003 | 3.50(1.00) | 0.760 | 3.00(2.00) | 0.161 |
| 1000–3000 | 2.00(1.00) | 3.50(1.00) | 3.00(2.00) | |||
| 3001–5000 | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| 5001–8000 | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| >8000 | 2.00(1.00) | 3.50(1.00) | 3.00(2.00) | |||
| Employment | ||||||
| Employed | 2.00(1.00) | 0.018 | 3.50(1.00) | <0.001 | 3.00(1.00) | 0.413 |
| Self-employed | 2.00(1.00) | 3.50(1.00) | 3.00(1.00) | |||
| Unemployed | 2.00(1.00) | 3.00(1.00) | 3.00(1.00) | |||
| Student | 2.00(0.00) | 4.00(1.00) | 3.00(2.00) | |||
| Other | 2.00(1.00) | 4.00(1.00) | 3.00(1.00) | |||
| Score | Knowledge | Attitude | Practice | ||
|---|---|---|---|---|---|
| Coefficient | |||||
| Score | |||||
| Knowledge | 1 | 0.299** | 0.173** | ||
| Attitude | 0.299** | 1 | 0.252** | ||
| Practice | 0.173** | 0.252** | 1 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, P.; Hayat, K.; Shi, L.; Lambojon, K.; Saeed, A.; Majid Aziz, M.; Liu, T.; Ji, S.; Gong, Y.; Feng, Z.; et al. Knowledge, Attitude, and Practices of Antibiotics and Antibiotic Resistance Among Chinese Pharmacy Customers: A Multicenter Survey Study. Antibiotics 2020, 9, 184. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9040184
Li P, Hayat K, Shi L, Lambojon K, Saeed A, Majid Aziz M, Liu T, Ji S, Gong Y, Feng Z, et al. Knowledge, Attitude, and Practices of Antibiotics and Antibiotic Resistance Among Chinese Pharmacy Customers: A Multicenter Survey Study. Antibiotics. 2020; 9(4):184. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9040184
Chicago/Turabian StyleLi, Pengchao, Khezar Hayat, Li Shi, Krizzia Lambojon, Amna Saeed, Muhammad Majid Aziz, Tao Liu, Shiyu Ji, Yilin Gong, Zhitong Feng, and et al. 2020. "Knowledge, Attitude, and Practices of Antibiotics and Antibiotic Resistance Among Chinese Pharmacy Customers: A Multicenter Survey Study" Antibiotics 9, no. 4: 184. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics9040184






