Effects of Propolis on Infectious Diseases of Medical Relevance
Abstract
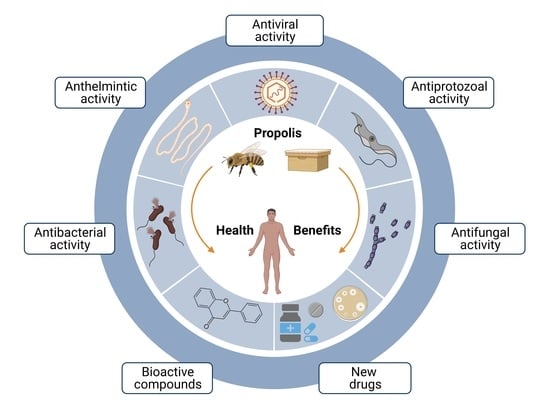
:Simple Summary
Abstract
1. Introduction
2. Antibacterial Activity of Propolis
2.1. Staphylococcus Infections
2.2. Streptococcus Infections
2.3. Gastrointestinal Infections
2.4. Nosocomial Infections
3. Antifungal Activity of Propolis
3.1. Candidiasis
3.2. Trichophyton Infections
3.3. Aspergillus and Penicillium Infections
4. Antiparasitic Activity
4.1. Malaria
4.2. Chagas Disease
4.3. Leishmaniasis
4.4. Giardiasis
4.5. Helminths
5. Antiviral Activity of Propolis
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloom, D.E.; Cadarette, D. Infectious disease threats in the twenty-first century: Strengthening the global response. Front. Immunol. 2019, 10, 549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morens, D.M.; Fauci, A.S. Emerging infectious diseases: Threats to human health and global stability. PLoS Pathog. 2013, 9, e1003467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordaliza, M. Natural products as leads to anticancer drugs. Clin. Transl. Oncol. 2007, 9, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-H. Current developments in the discovery and design of new drug candidates from plant natural product leads. J. Nat. Prod. 2004, 67, 273–283. [Google Scholar] [CrossRef]
- Toreti, V.C.; Sato, H.H.; Pastore, G.M.; Park, Y.K. Recent progress of propolis for its biological and chemical compositions and its botanical origin. Evid. -Based Complementary Altern. Med. 2013, 2013, 697390. [Google Scholar] [CrossRef]
- Bankova, V. Chemical diversity of propolis and the problem of standardization. J. Ethnopharmacol. 2005, 100, 114–117. [Google Scholar] [CrossRef]
- Huang, S.; Zhang, C.-P.; Wang, K.; Li, G.Q.; Hu, F.-L. Recent advances in the chemical composition of propolis. Molecules 2014, 19, 19610–19632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watanabe, M.A.E.; Amarante, M.K.; Conti, B.J.; Sforcin, J.M. Cytotoxic constituents of propolis inducing anticancer effects: A review. J. Pharm. Pharmacol. 2011, 63, 1378–1386. [Google Scholar] [CrossRef] [PubMed]
- Sforcin, J.M.; Bankova, V. Propolis: Is there a potential for the development of new drugs? J. Ethnopharmacol. 2011, 133, 253–260. [Google Scholar] [CrossRef]
- Bankova, V.S.; de Castro, S.L.; Marcucci, M.C. Propolis: Recent advances in chemistry and plant origin. Apidologie 2000, 31, 3–15. [Google Scholar] [CrossRef]
- Kujumgiev, A.; Tsvetkova, I.; Serkedjieva, Y.; Bankova, V.; Christov, R.; Popov, S. Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J. Ethnopharmacol. 1999, 64, 235–240. [Google Scholar] [CrossRef]
- Silva, J.C.; Rodrigues, S.; Feás, X.; Estevinho, L.M. Antimicrobial activity, phenolic profile and role in the inflammation of propolis. Food Chem. Toxicol. 2012, 50, 1790–1795. [Google Scholar] [CrossRef]
- Moreira, L.; Dias, L.G.; Pereira, J.A.; Estevinho, L. Antioxidant properties, total phenols and pollen analysis of propolis samples from Portugal. Food Chem. Toxicol. 2008, 46, 3482–3485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kocot, J.; Kiełczykowska, M.; Luchowska-Kocot, D.; Kurzepa, J.; Musik, I. Antioxidant potential of propolis, bee pollen, and royal jelly: Possible medical application. Oxidative Med. Cell. Longev. 2018, 2018, 1–29. [Google Scholar] [CrossRef]
- Hu, F.; Hepburn, H.; Li, Y.; Chen, M.; Radloff, S.; Daya, S. Effects of ethanol and water extracts of propolis (bee glue) on acute inflammatory animal models. J. Ethnopharmacol. 2005, 100, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Bueno-Silva, B.; Kawamoto, D.; Ando-Suguimoto, E.S.; Alencar, S.M.; Rosalen, P.L.; Mayer, M.P. Brazilian red propolis attenuates inflammatory signaling cascade in LPS-activated macrophages. PLoS ONE 2015, 10, e0144954. [Google Scholar] [CrossRef]
- Chan, G.C.-F.; Cheung, K.-W.; Sze, D.M.-Y. The immunomodulatory and anticancer properties of propolis. Clin. Rev. Allergy Immunol. 2013, 44, 262–273. [Google Scholar] [CrossRef]
- Rivera-Yañez, N.; Rodriguez-Canales, M.; Nieto-Yañez, O.; Jimenez-Estrada, M.; Ibarra-Barajas, M.; Canales-Martinez, M.; Rodriguez-Monroy, M. Hypoglycaemic and antioxidant effects of propolis of Chihuahua in a model of experimental diabetes. Evid. -Based Complementary Altern. Med. 2018, 2018. [Google Scholar] [CrossRef] [Green Version]
- Al-Hariri, M. Immune’s-boosting agent: Immunomodulation potentials of propolis. J. Fam. Community Med. 2019, 26, 57. [Google Scholar] [CrossRef]
- Andersson, D.I.; Hughes, D. Selection and Transmission of Antibiotic-Resistant Bacteria. Microb. Transm. 2019, 117–137. [Google Scholar] [CrossRef]
- Centres for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013; Centres for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2013. [Google Scholar]
- Munita, J.M.; Arias, C.A. Mechanisms of antibiotic resistance. Virulence Mech. Bact. Pathog. 2016, 4, 481–511. [Google Scholar]
- Assoni, L.; Milani, B.; Carvalho, M.R.; Nepomuceno, L.N.; Waz, N.T.; Guerra, M.E.S.; Converso, T.R.; Darrieux, M. Resistance Mechanisms to Antimicrobial Peptides in Gram-Positive Bacteria. Front. Microbiol. 2020, 11, 2362. [Google Scholar] [CrossRef] [PubMed]
- Algammal, A.M.; Hetta, H.F.; Elkelish, A.; Alkhalifah, D.H.H.; Hozzein, W.N.; Batiha, G.E.-S.; El Nahhas, N.; Mabrok, M.A. Methicillin-Resistant Staphylococcus aureus (MRSA): One Health Perspective Approach to the Bacterium Epidemiology, Virulence Factors, Antibiotic-Resistance, and Zoonotic Impact. Infect. Drug Resist. 2020, 13, 3255. [Google Scholar] [CrossRef] [PubMed]
- Raghukumar, R.; Vali, L.; Watson, D.; Fearnley, J.; Seidel, V. Antimethicillin-resistant Staphylococcus aureus (MRSA) activity of ‘pacific propolis’ and isolated prenylflavanones. Phytother. Res. 2010, 24, 1181–1187. [Google Scholar] [CrossRef] [PubMed]
- Wagh, V.D. Propolis: A wonder bees product and its pharmacological potentials. Adv. Pharmacol. Sci. 2013, 2013. [Google Scholar] [CrossRef] [Green Version]
- Grecka, K.; Kuś, P.M.; Okińczyc, P.; Worobo, R.W.; Walkusz, J.; Szweda, P. The anti-staphylococcal potential of ethanolic polish propolis extracts. Molecules 2019, 24, 1732. [Google Scholar] [CrossRef] [Green Version]
- AL-Ani, I.; Zimmermann, S.; Reichling, J.; Wink, M. Antimicrobial activities of European propolis collected from various geographic origins alone and in combination with antibiotics. Medicines 2018, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Rahman, M.M.; Richardson, A.; Sofian-Azirun, M. Antibacterial activity of propolis and honey against Staphylococcus aureus and Escherichia coli. Afr. J. Microbiol. Res. 2010, 4, 1872–1878. [Google Scholar]
- Dantas Silva, R.P.; Machado, B.A.S.; Barreto, G.d.A.; Costa, S.S.; Andrade, L.N.; Amaral, R.G.; Carvalho, A.A.; Padilha, F.F.; Barbosa, J.D.V.; Umsza-Guez, M.A. Antioxidant, antimicrobial, antiparasitic, and cytotoxic properties of various Brazilian propolis extracts. PLoS ONE 2017, 12, e0172585. [Google Scholar] [CrossRef] [PubMed]
- Boisard, S.; Le Ray, A.-M.; Landreau, A.; Kempf, M.; Cassisa, V.; Flurin, C.; Richomme, P. Antifungal and antibacterial metabolites from a French poplar type propolis. Evid. -Based Complementary Altern. Med. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Wojtyczka, R.D.; Dziedzic, A.; Idzik, D.; Kępa, M.; Kubina, R.; Kabała-Dzik, A.; Smoleń-Dzirba, J.; Stojko, J.; Sajewicz, M.; Wąsik, T.J. Susceptibility of Staphylococcus aureus clinical isolates to propolis extract alone or in combination with antimicrobial drugs. Molecules 2013, 18, 9623–9640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scazzocchio, F.; D’auria, F.; Alessandrini, D.; Pantanella, F. Multifactorial aspects of antimicrobial activity of propolis. Microbiol. Res. 2006, 161, 327–333. [Google Scholar] [CrossRef]
- Ristivojević, P.; Dimkić, I.; Trifković, J.; Berić, T.; Vovk, I.; Milojković-Opsenica, D.; Stanković, S. Antimicrobial activity of Serbian propolis evaluated by means of MIC, HPTLC, bioautography and chemometrics. PLoS ONE 2016, 11, e0157097. [Google Scholar] [CrossRef]
- Papachroni, D.; Graikou, K.; Kosalec, I.; Damianakos, H.; Ingram, V.; Chinou, I. Phytochemical analysis and biological evaluation of selected African propolis samples from Cameroon and Congo. Nat. Prod. Commun. 2015, 10, 1934578X1501000118. [Google Scholar] [CrossRef] [Green Version]
- Muli, E.; Maingi, J. Antibacterial activity of Apis mellifera L. propolis collected in three regions of Kenya. J. Venom. Anim. Toxins Incl. Trop. Dis. 2007, 13, 655–663. [Google Scholar] [CrossRef]
- Araujo, M.A.; Libério, S.A.; Guerra, R.N.; Ribeiro, M.N.S.; Nascimento, F.R. Mechanisms of action underlying the anti-inflammatory and immunomodulatory effects of propolis: A brief review. Rev. Bras. Farmacogn. 2012, 22, 208–219. [Google Scholar] [CrossRef] [Green Version]
- Cuevas, A.; Saavedra, N.; Salazar, L.A.; Abdalla, D.S. Modulation of immune function by polyphenols: Possible contribution of epigenetic factors. Nutrients 2013, 5, 2314–2332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fokt, H.; Pereira, A.; Ferreira, A.; Cunha, A.; Aguiar, C. How do bees prevent hive infections? The antimicrobial properties of propolis. Curr. Res. Technol. Educ. Top. Appl. Microbiol. Microb. Biotechnol. 2010, 1, 481–493. [Google Scholar]
- Devequi-Nunes, D.; Machado, B.A.S.; Barreto, G.d.A.; Rebouças Silva, J.; da Silva, D.F.; da Rocha, J.L.C.; Brandão, H.N.; Borges, V.M.; Umsza-Guez, M.A. Chemical characterization and biological activity of six different extracts of propolis through conventional methods and supercritical extraction. PLoS ONE 2018, 13, e0207676. [Google Scholar] [CrossRef]
- Seibert, J.B.; Bautista-Silva, J.P.; Amparo, T.R.; Petit, A.; Pervier, P.; dos Santos Almeida, J.C.; Azevedo, M.C.; Silveira, B.M.; Brandão, G.C.; de Souza, G.H.B. Development of propolis nanoemulsion with antioxidant and antimicrobial activity for use as a potential natural preservative. Food Chem. 2019, 287, 61–67. [Google Scholar] [CrossRef]
- Tiveron, A.P.; Rosalen, P.L.; Franchin, M.; Lacerda, R.C.C.; Bueno-Silva, B.; Benso, B.; Denny, C.; Ikegaki, M.; Alencar, S.M.d. Chemical characterization and antioxidant, antimicrobial, and anti-inflammatory activities of South Brazilian organic propolis. PLoS ONE 2016, 11, e0165588. [Google Scholar] [CrossRef] [Green Version]
- Pobiega, K.; Kraśniewska, K.; Przybył, J.L.; Bączek, K.; Żubernik, J.; Witrowa-Rajchert, D.; Gniewosz, M. Growth biocontrol of foodborne pathogens and spoilage microorganisms of food by polish propolis extracts. Molecules 2019, 24, 2965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kharsany, K.; Viljoen, A.; Leonard, C.; van Vuuren, S. The new buzz: Investigating the antimicrobial interactions between bioactive compounds found in South African propolis. J. Ethnopharmacol. 2019, 238, 111867. [Google Scholar] [CrossRef] [PubMed]
- Touzani, S.; Embaslat, W.; Imtara, H.; Kmail, A.; Kadan, S.; Zaid, H.; ElArabi, I.; Badiaa, L.; Saad, B. In Vitro Evaluation of the Potential Use of Propolis as a Multitarget Therapeutic Product: Physicochemical Properties, Chemical Composition, and Immunomodulatory, Antibacterial, and Anticancer Properties. Biomed Res. Int. 2019, 2019, 4836378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, T.H.; Chitra, E.; Ramamurthy, S.; Ling, C.C.S.; Ambu, S.P.; Davamani, F. Cationic chitosan-propolis nanoparticles alter the zeta potential of S. epidermidis, inhibit biofilm formation by modulating gene expression and exhibit synergism with antibiotics. PLoS ONE 2019, 14, e0213079. [Google Scholar] [CrossRef]
- Álvarez-Martínez, F.J.; Barrajón-Catalán, E.; Micol, V. Tackling antibiotic resistance with compounds of natural origin: A comprehensive review. Biomedicines 2020, 8, 405. [Google Scholar] [CrossRef]
- O’Loughlin, R.E.; Roberson, A.; Cieslak, P.R.; Lynfield, R.; Gershman, K.; Craig, A.; Albanese, B.A.; Farley, M.M.; Barrett, N.L.; Spina, N.L. The epidemiology of invasive group A streptococcal infection and potential vaccine implications: United States, 2000–2004. Clin. Infect. Dis. 2007, 45, 853–862. [Google Scholar] [CrossRef]
- Martin, J.M.; Green, M. Group A streptococcus. In Seminars in Pediatric Infectious Diseases; WB Saunders: Philadelphia, PA, USA, 2006; pp. 140–148. [Google Scholar]
- Rivero-Cruz, J.F.; Granados-Pineda, J.; Pedraza-Chaverri, J.; Pérez-Rojas, J.M.; Kumar-Passari, A.; Diaz-Ruiz, G.; Rivero-Cruz, B.E. Phytochemical constituents, antioxidant, cytotoxic, and antimicrobial activities of the ethanolic extract of Mexican brown propolis. Antioxidants 2020, 9, 70. [Google Scholar] [CrossRef] [Green Version]
- Asgharpour, F.; Moghadamnia, A.A.; Zabihi, E.; Kazemi, S.; Namvar, A.E.; Gholinia, H.; Motallebnejad, M.; Nouri, H.R. Iranian propolis efficiently inhibits growth of oral streptococci and cancer cell lines. BMC Complementary Altern. Med. 2019, 19, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeon, J.-G.; Rosalen, P.; Falsetta, M.; Koo, H. Natural products in caries research: Current (limited) knowledge, challenges and future perspective. Caries Res. 2011, 45, 243–263. [Google Scholar] [CrossRef]
- Sell, J.; Dolan, B. Common gastrointestinal infections. Prim. Care Clin. Off. Pract. 2018, 45, 519–532. [Google Scholar] [CrossRef]
- Almuhayawi, M.S. Propolis as a novel antibacterial agent. Saudi J. Biol. Sci. 2020, 27, 3079. [Google Scholar] [CrossRef]
- Berretta, A.A.; Arruda, C.; Miguel, F.G.; Baptista, N.; Nascimento, A.P.; Marquele-Oliveira, F.; Hori, J.I.; Barud, H.; Damaso, B.; Ramos, C. Functional properties of Brazilian propolis: From chemical composition until the market. Superfood Funct. Food Overv. Process. Util. 2017, 55–98. [Google Scholar] [CrossRef] [Green Version]
- Orsi, R.d.O.; Fernandes, A.; Bankova, V.; Sforcin, J. The effects of Brazilian and Bulgarian propolis in vitro against Salmonella Typhi and their synergism with antibiotics acting on the ribosome. Nat. Prod. Res. 2012, 26, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Monegro, A.F.; Muppidi, V.; Regunath, H. Hospital acquired infections. Statpearls [Internet] 2020, 2, 447. [Google Scholar]
- Magill, S.S.; Edwards, J.R.; Bamberg, W.; Beldavs, Z.G.; Dumyati, G.; Kainer, M.A.; Lynfield, R.; Maloney, M.; McAllister-Hollod, L.; Nadle, J. Multistate point-prevalence survey of health care–associated infections. N. Engl. J. Med. 2014, 370, 1198–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorlenko, C.L.; Kiselev, H.Y.; Budanova, E.V.; Zamyatnin, A.A.; Ikryannikova, L.N. Plant Secondary Metabolites in the Battle of Drugs and Drug-Resistant Bacteria: New Heroes or Worse Clones of Antibiotics? Antibiotics 2020, 9, 170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ling, H. Is it Possible to Treat Community-Acquired and Nosocomial Infections with the Same Method, without the Use of Antibiotics. J. Appl. Microb. Res. 2019, 2, 1–13. [Google Scholar]
- Meto, A.; Colombari, B.; Meto, A.; Boaretto, G.; Pinetti, D.; Marchetti, L.; Benvenuti, S.; Pellati, F.; Blasi, E. Propolis affects Pseudomonas aeruginosa growth, biofilm formation, eDNA release and phenazine production: Potential involvement of polyphenols. Microorganisms 2020, 8, 243. [Google Scholar] [CrossRef] [Green Version]
- Baptista, P.V.; McCusker, M.P.; Carvalho, A.; Ferreira, D.A.; Mohan, N.M.; Martins, M.; Fernandes, A.R. Nano-strategies to fight multidrug resistant bacteria—“A Battle of the Titans”. Front. Microbiol. 2018, 9, 1441. [Google Scholar] [CrossRef] [Green Version]
- Cortese, Y.J.; Wagner, V.E.; Tierney, M.; Devine, D.; Fogarty, A. Review of catheter-associated urinary tract infections and in vitro urinary tract models. J. Healthc. Eng. 2018, 2018, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Rai, M.; Kon, K. Fighting Multidrug Resistance with Herbal Extracts, Essential Oils and Their Components; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Robbins, N.; Wright, G.D.; Cowen, L.E. Antifungal drugs: The current armamentarium and development of new agents. Fungal Kingd. 2017, 4, 903–922. [Google Scholar]
- Gucwa, K.; Kusznierewicz, B.; Milewski, S.; Van Dijck, P.; Szweda, P. Antifungal activity and synergism with azoles of polish propolis. Pathogens 2018, 7, 56. [Google Scholar] [CrossRef] [Green Version]
- Huang, M.; Kao, K.C. Population dynamics and the evolution of antifungal drug resistance in Candida albicans. FEMS Microbiol. Lett. 2012, 333, 85–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popova, M.P.; Graikou, K.; Chinou, I.; Bankova, V.S. GC-MS profiling of diterpene compounds in Mediterranean propolis from Greece. J. Agric. Food Chem. 2010, 58, 3167–3176. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Wu, T.; Pan, S.; Xu, X. Antimicrobial mechanism of flavonoids against Escherichia coli ATCC 25922 by model membrane study. Appl. Surf. Sci. 2014, 305, 515–521. [Google Scholar] [CrossRef]
- Guevara-Lora, I.; Bras, G.; Karkowska-Kuleta, J.; González-González, M.; Ceballos, K.; Sidlo, W.; Rapala-Kozik, M. Plant-derived substances in the fight against infections caused by Candida species. Int. J. Mol. Sci. 2020, 21, 6131. [Google Scholar] [CrossRef]
- Kumamoto, C.A. Candida biofilms. Curr. Opin. Microbiol. 2002, 5, 608–611. [Google Scholar] [CrossRef]
- Bandara, H.; Matsubara, V.H.; Samaranayake, L.P. Future therapies targeted towards eliminating Candida biofilms and associated infections. Expert Rev. Anti-Infect. Ther. 2017, 15, 299–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arendrup, M.C. Epidemiology of invasive candidiasis. Curr. Opin. Crit. Care 2010, 16, 445–452. [Google Scholar] [CrossRef]
- Rodrigues, M.E.; Silva, S.; Azeredo, J.; Henriques, M. Novel strategies to fight Candida species infection. Crit. Rev. Microbiol. 2016, 42, 594–606. [Google Scholar] [CrossRef] [Green Version]
- Hidron, A.I.; Edwards, J.R.; Patel, J.; Horan, T.C.; Sievert, D.M.; Pollock, D.A.; Fridkin, S.K.; Team, N.H.S.N.; Facilities, P.N.H.S.N. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006–2007. Infect. Control Hosp. Epidemiol. 2008, 29, 996–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wisplinghoff, H.; Bischoff, T.; Tallent, S.M.; Seifert, H.; Wenzel, R.P.; Edmond, M.B. Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 2004, 39, 309–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cleveland, A.A.; Farley, M.M.; Harrison, L.H.; Stein, B.; Hollick, R.; Lockhart, S.R.; Magill, S.S.; Derado, G.; Park, B.J.; Chiller, T.M. Changes in incidence and antifungal drug resistance in candidemia: Results from population-based laboratory surveillance in Atlanta and Baltimore, 2008–2011. Clin. Infect. Dis. 2012, 55, 1352–1361. [Google Scholar] [CrossRef]
- Diekema, D.; Messer, S.; Brueggemann, A.; Coffman, S.; Doern, G.; Herwaldt, L.; Pfaller, M. Epidemiology of candidemia: 3-year results from the emerging infections and the epidemiology of Iowa organisms study. J. Clin. Microbiol. 2002, 40, 1298–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tortorano, A.M.; Kibbler, C.; Peman, J.; Bernhardt, H.; Klingspor, L.; Grillot, R. Candidaemia in Europe: Epidemiology and resistance. Int. J. Antimicrob. Agents 2006, 27, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Dota, K.F.D.; Consolaro, M.E.L.; Svidzinski, T.I.E.; Bruschi, M.L. Antifungal activity of Brazilian propolis microparticles against yeasts isolated from vulvovaginal candidiasis. Evid. -Based Complementary Altern. Med. 2011, 2011, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Capoci, I.R.G.; Bonfim-Mendonça, P.d.S.; Arita, G.S.; Pereira, R.R.d.A.; Consolaro, M.E.L.; Bruschi, M.L.; Negri, M.; Svidzinski, T.I.E. Propolis is an efficient fungicide and inhibitor of biofilm production by vaginal Candida albicans. Evid. -Based Complementary Altern. Med. 2015, 2015, 1–9. [Google Scholar] [CrossRef] [Green Version]
- De Castro, P.A.; Bom, V.L.P.; Brown, N.A.; de Almeida, R.S.C.; Ramalho, L.N.Z.; Savoldi, M.; Goldman, M.H.S.; Berretta, A.A.; Goldman, G.H. Identification of the cell targets important for propolis-induced cell death in Candida albicans. Fungal Genet. Biol. 2013, 60, 74–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szweda, P.; Gucwa, K.; Kurzyk, E.; Romanowska, E.; Dzierżanowska-Fangrat, K.; Jurek, A.Z.; Kuś, P.M.; Milewski, S. Essential oils, silver nanoparticles and propolis as alternative agents against fluconazole resistant Candida albicans, Candida glabrata and Candida krusei clinical isolates. Indian J. Microbiol. 2015, 55, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Falcão, S.I.; Vale, N.; Cos, P.; Gomes, P.; Freire, C.; Maes, L.; Vilas-Boas, M. In vitro evaluation of Portuguese propolis and floral sources for antiprotozoal, antibacterial and antifungal activity. Phytother. Res. 2014, 28, 437–443. [Google Scholar] [CrossRef]
- Alsayed, M.F.S.; Hashem, A.; Al-Hazzani, A.A.; Abd_Allah, E.F. Biological control of yeast contamination of industrial foods by propolis. Saudi J. Biol. Sci. 2020, 27, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Mutlu Sariguzel, F.; Berk, E.; Koc, A.N.; Sav, H.; Demir, G. Antifungal activity of propolis against yeasts isolated from blood culture: In Vitro evaluation. J. Clin. Lab. Anal. 2016, 30, 513–516. [Google Scholar] [CrossRef] [Green Version]
- Sayyadi, F.; Mahdavi, S.; Moghadamnia, A.A.; Moslemi, D.; Shirzad, A.; Motallebnejad, M. The effect of aqueous and ethanolic extract of Iranian propolis on Candida Albicans isolated from the mouth of patients with colorectal malignancy undergone chemotherapy: An in-vitro study. Casp. J. Intern. Med. 2020, 11, 62. [Google Scholar]
- Iadnut, A.; Mamoon, K.; Thammasit, P.; Pawichai, S.; Tima, S.; Preechasuth, K.; Kaewkod, T.; Tragoolpua, Y.; Tragoolpua, K. In Vitro antifungal and antivirulence activities of biologically synthesized ethanolic extract of Propolis-Loaded PLGA nanoparticles against candida albicans. Evid. -Based Complementary Altern. Med. 2019, 2019, 1–14. [Google Scholar] [CrossRef] [Green Version]
- de Carvalho, C.; Fernandes, W.H.C.; Mouttinho, T.B.F.; de Souza, D.M.; Marcucci, M.C.; D’Alpino, P.H.P. Evidence-based studies and perspectives of the use of Brazilian green and red Propolis in dentistry. Eur. J. Dent. 2019, 13, 459. [Google Scholar] [CrossRef]
- Negri, M.; Salci, T.P.; Shinobu-Mesquita, C.S.; Capoci, I.R.; Svidzinski, T.I.; Kioshima, E.S. Early state research on antifungal natural products. Molecules 2014, 19, 2925–2956. [Google Scholar] [CrossRef] [PubMed]
- Pippi, B.; Lana, A.; Moraes, R.; Güez, C.; Machado, M.; De Oliveira, L.; Lino von Poser, G.; Fuentefria, A. In vitro evaluation of the acquisition of resistance, antifungal activity and synergism of B razilian red propolis with antifungal drugs on C andida spp. J. Appl. Microbiol. 2015, 118, 839–850. [Google Scholar] [CrossRef] [PubMed]
- Berretta, A.A.; de Castro, P.A.; Cavalheiro, A.H.; Fortes, V.S.; Bom, V.P.; Nascimento, A.P.; Marquele-Oliveira, F.; Pedrazzi, V.; Ramalho, L.N.Z.; Goldman, G.H. Evaluation of mucoadhesive gels with propolis (EPP-AF) in preclinical treatment of candidiasis vulvovaginal infection. Evid.-Based Complementary Altern. Med. 2013, 2013, 641480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raheem, I.A.A.; Razek, A.A.; Elgendy, A.A.; Saleh, N.M.; Shaaban, M.I.; Abd El-Hady, F.K. Design, evaluation and antimicrobial activity Of Egyptian Propolis-Loaded Nanoparticles: Intrinsic role as a novel and naturally based root canal nanosealer. Int. J. Nanomed. 2019, 14, 8379. [Google Scholar] [CrossRef] [Green Version]
- Dezmirean, D.S.; Paşca, C.; Moise, A.R.; Bobiş, O. Plant Sources Responsible for the Chemical Composition and Main Bioactive Properties of Poplar-Type Propolis. Plants 2021, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Gnat, S.; Łagowski, D.; Nowakiewicz, A.; Zięba, P. The host range of dermatophytes, it is at all possible? Phenotypic evaluation of the keratinolytic activity of Trichophyton verrucosum clinical isolates. Mycoses 2019, 62, 274–283. [Google Scholar] [CrossRef]
- Khurana, A.; Sardana, K.; Chowdhary, A. Antifungal resistance in dermatophytes: Recent trends and therapeutic implications. Fungal Genet. Biol. 2019, 132, 103255. [Google Scholar] [CrossRef] [PubMed]
- Pires, C.A.A.; Cruz, N.F.S.D.; Lobato, A.M.; Sousa, P.O.D.; Carneiro, F.R.O.; Mendes, A.M.D. Clinical, epidemiological, and therapeutic profile of dermatophytosis. An. Bras. Dermatol. 2014, 89, 259–264. [Google Scholar] [CrossRef] [Green Version]
- Petrucelli, M.F.; Abreu, M.H.D.; Cantelli, B.A.M.; Segura, G.G.; Nishimura, F.G.; Bitencourt, T.A.; Marins, M.; Fachin, A.L. Epidemiology and Diagnostic Perspectives of Dermatophytoses. J. Fungi 2020, 6, 310. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Stec, N. Emerging drugs for the treatment of onychomycosis. Expert Opin. Emerg. Drugs 2019, 24, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, A.; Gomes, B.; Cambuim, I.; Maia, R.; Abreu, S.; Souza-Motta, C.; De Queiroz, L.; Porto, A. Trichophyton species susceptibility to green and red propolis from Brazil. Lett. Appl. Microbiol. 2009, 48, 90–96. [Google Scholar] [CrossRef]
- Veiga, F.F.; Gadelha, M.C.; da Silva, M.R.; Costa, M.I.; Kischkel, B.; de Castro-Hoshino, L.V.; Sato, F.; Baesso, M.L.; Voidaleski, M.F.; Vasconcellos-Pontello, V. Propolis extract for onychomycosis topical treatment: From bench to clinic. Front. Microbiol. 2018, 9, 779. [Google Scholar] [CrossRef] [Green Version]
- Gavanji, S.; Asgari, M.J.; Vaezi, R.; Larki, B. Antifungal effect of the extract of propolis on the growth of three species of Epidermophyton flucosum, Trichophyton violaseum and Trichophyton tonsorans in laboratory environment. Afr. J. Pharm. Pharmacol. 2011, 5, 2642–2646. [Google Scholar]
- Kosmidis, C.; Denning, D.W. The clinical spectrum of pulmonary aspergillosis. Thorax 2015, 70, 270–277. [Google Scholar] [CrossRef] [Green Version]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and multi-national prevalence of fungal diseases—Estimate precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Barac, A.; Kosmidis, C.; Alastruey-Izquierdo, A.; Salzer, H.J.; CPAnet. Chronic pulmonary aspergillosis update: A year in review. Med. Mycol. 2019, 57, S104–S109. [Google Scholar] [CrossRef] [PubMed]
- Frisvad, J.C.; Thrane, U.; Samson, R.A.; Pitt, J.I. Important mycotoxins and the fungi which produce them. Adv. Food Mycol. 2006, 571, 3–31. [Google Scholar]
- Milićević, D.R.; Škrinjar, M.; Baltić, T. Real and perceived risks for mycotoxin contamination in foods and feeds: Challenges for food safety control. Toxins 2010, 2, 572–592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zain, M.E. Impact of mycotoxins on humans and animals. J. Saudi Chem. Soc. 2011, 15, 129–144. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Pu, R.; Li, Y.; Wu, Z.; Li, C.; Miao, X.; Yang, W. Chemical Compositions of Propolis from China and the United States and their Antimicrobial Activities Against Penicillium notatum. Molecules 2019, 24, 3576. [Google Scholar] [CrossRef] [Green Version]
- Bankova, V. Recent trends and important developments in propolis research. Evid. -Based Complementary Altern. Med. 2005, 2, 29–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Özcan, M. Inhibition of Aspergillus parasiticus NRRL 2999 by pollen and propolis extracts. J. Med. Food 2004, 7, 114–116. [Google Scholar] [CrossRef]
- Simone-Finstrom, M.; Spivak, M. Propolis and bee health: The natural history and significance of resin use by honey bees. Apidologie 2010, 41, 295–311. [Google Scholar] [CrossRef] [Green Version]
- Nash, T.E. Parasitic Diseases that Cause Seizures: Parasitic Diseases that Cause Seizures. Epilepsy Curr. 2014, 14, 29–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pink, R.; Hudson, A.; Mouriès, M.-A.; Bendig, M. Opportunities and challenges in antiparasitic drug discovery. Nat. Rev. Drug Discov. 2005, 4, 727–740. [Google Scholar] [CrossRef] [PubMed]
- Watkins, B.M. Drugs for the control of parasitic diseases: Current status and development. Trends Parasitol. 2003, 19, 477–478. [Google Scholar] [CrossRef]
- Norman, F.F.; Comeche, B.; Chamorro, S.; Pérez-Molina, J.-A.; López-Vélez, R. Update on the major imported protozoan infections in travelers and migrants. Future Microbiol. 2020, 15, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Norman, F.F.; Monge-Maillo, B.; Martínez-Pérez, Á.; Perez-Molina, J.A.; López-Vélez, R. Parasitic infections in travelers and immigrants: Part I protozoa. Future Microbiol. 2015, 10, 69–86. [Google Scholar] [CrossRef] [PubMed]
- Woodhall, D.; Jones, J.L.; Cantey, P.T.; Wilkins, P.P.; Montgomery, S.P. Neglected parasitic infections: What every family physician needs to know. Am. Fam. Physician 2014, 89, 803–811. [Google Scholar]
- World Health Organization. World Malaria Report 2018; World Health Organ: Geneva, Switzerland, 2020. [Google Scholar]
- Monzote, L.; Cuesta-Rubio, O.; Campo Fernandez, M.; Márquez Hernandez, I.; Fraga, J.; Pérez, K.; Kerstens, M.; Maes, L.; Cos, P. In vitro antimicrobial assessment of Cuban propolis extracts. Memórias Do Inst. Oswaldo Cruz 2012, 107, 978–984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siheri, W.; Zhang, T.; Ebiloma, G.U.; Biddau, M.; Woods, N.; Hussain, M.Y.; Clements, C.J.; Fearnley, J.; Ebel, R.E.; Paget, T. Chemical and antimicrobial profiling of propolis from different regions within Libya. PLoS ONE 2016, 11, e0155355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afrouzan, H.; Zakeri, S.; Mehrizi, A.A.; Molasalehi, S.; Tahghighi, A.; Shokrgozar, M.A.; Es-Haghi, A.; Djadid, N.D. Anti-Plasmodial assessment of four different Iranian Propolis extracts. Arch. Iran. Med. 2017, 20, 270–281. [Google Scholar]
- AlGabbani, Q.; Mansour, L.; Elnakady, Y.A.; Al-Quraishy, S.; Alomar, S.; Al-Shaebi, E.M.; Abdel-Baki, A.-A.S. In vivo assessment of the antimalarial and spleen-protective activities of the Saudi propolis methanolic extract. Parasitol. Res. 2017, 116, 539–547. [Google Scholar] [CrossRef]
- Khaomek, P.; Ichino, C.; Ishiyama, A.; Sekiguchi, H.; Namatame, M.; Ruangrungsi, N.; Saifah, E.; Kiyohara, H.; Otoguro, K.; Omura, S. In vitro antimalarial activity of prenylated flavonoids from Erythrina fusca. J. Nat. Med. 2008, 62, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Mukhtar, H.M.; Kaur, H.; Kaur, L. Investigation of antiplasmodial efficacy of lupeol and ursolic acid isolated from Ficus benjamina leaves extract. Nat. Prod. Res. 2020, 34, 2514–2517. [Google Scholar] [CrossRef] [PubMed]
- Sosa-Estani, S.; Segura, E.L. Integrated control of Chagas disease for its elimination as public health problem—A Review. Memórias Do Inst. Oswaldo Cruz 2015, 110, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Mills, R.M. Chagas Disease. Epidemiology and Barriers to Treatment. Am. J. Med. 2020, 133, 1262–1265. [Google Scholar] [CrossRef] [PubMed]
- Higashi, K.; De Castro, S. Propolis extracts are effective against Trypanosoma cruzi and have an impact on its interaction with host cells. J. Ethnopharmacol. 1994, 43, 149–155. [Google Scholar] [CrossRef]
- da Silva Cunha, I.B.; Salomão, K.; Shimizu, M.; Bankova, V.S.; Custódio, A.R.; de CASTRO, S.L.; Marcucci, M.C. Antitrypanosomal activity of Brazilian propolis from Apis mellifera. Chem. Pharm. Bull. 2004, 52, 602–604. [Google Scholar] [CrossRef] [Green Version]
- Salomão, K.; Dantas, A.P.; Borba, C.M.; Campos, L.; Machado, D.; Aquino Neto, F.; De Castro, S. Chemical composition and microbicidal activity of extracts from Brazilian and Bulgarian propolis. Lett. Appl. Microbiol. 2004, 38, 87–92. [Google Scholar] [CrossRef]
- Marcucci, M.C.; Ferreres, F.; Garcıa-Viguera, C.; Bankova, V.; De Castro, S.; Dantas, A.; Valente, P.; Paulino, N. Phenolic compounds from Brazilian propolis with pharmacological activities. J. Ethnopharmacol. 2001, 74, 105–112. [Google Scholar] [CrossRef]
- Dantas, A.P.; Salomão, K.; Barbosa, H.S.; De Castro, S.L. The effect of Bulgarian propolis against Trypanosoma cruzi and during its interaction with host cells. Memórias Do Inst. Oswaldo Cruz 2006, 101, 207–211. [Google Scholar] [CrossRef] [Green Version]
- Prytzyk, E.; Dantas, A.P.; Salomão, K.; Pereira, A.S.; Bankova, V.S.; De Castro, S.L.; Neto, F.R.A. Flavonoids and trypanocidal activity of Bulgarian propolis. J. Ethnopharmacol. 2003, 88, 189–193. [Google Scholar] [CrossRef]
- Dantas, A.P.; Olivieri, B.P.; Gomes, F.H.; De Castro, S.L. Treatment of Trypanosoma cruzi-infected mice with propolis promotes changes in the immune response. J. Ethnopharmacol. 2006, 103, 187–193. [Google Scholar] [CrossRef]
- Salomao, K.; de Souza, E.M.; Henriques-Pons, A.; Barbosa, H.S.; de Castro, S.L. Brazilian green propolis: Effects in vitro and in vivo on Trypanosoma cruzi. Evid. -Based Complementary Altern. Med. 2011, 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Charlton, R.L.; Rossi-Bergmann, B.; Denny, P.W.; Steel, P.G. Repurposing as a strategy for the discovery of new anti-leishmanials: The-state-of-the-art. Parasitology 2018, 145, 219–236. [Google Scholar] [CrossRef] [Green Version]
- Chakravarty, J.; Sundar, S. Drug resistance in leishmaniasis. J. Glob. Infect. Dis. 2010, 2, 167. [Google Scholar] [CrossRef] [PubMed]
- Altamura, F.; Rajesh, R.; Catta-Preta, C.M.; Moretti, N.S.; Cestari, I. The current drug discovery landscape for trypanosomiasis and leishmaniasis: Challenges and strategies to identify drug targets. Drug Dev. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Santana, L.C.; Carneiro, S.M.P.; Caland-Neto, L.B.; Arcanjo, D.D.; Moita-Neto, J.M.; Citó, A.M.; Carvalho, F.A.A. Brazilian brown propolis elicits antileishmanial effect against promastigote and amastigote forms of Leishmania amazonensis. Nat. Prod. Res. 2014, 28, 340–343. [Google Scholar] [CrossRef]
- Ayres, D.C.; Marcucci, M.C.; Giorgio, S. Effects of Brazilian propolis on Leishmania amazonensis. Memórias Do Inst. Oswaldo Cruz 2007, 102, 215–220. [Google Scholar] [CrossRef]
- da Silveira Regueira-Neto, M.; Tintino, S.R.; Rolón, M.; Coronal, C.; Vega, M.C.; de Queiroz Balbino, V.; de Melo Coutinho, H.D. Antitrypanosomal, antileishmanial and cytotoxic activities of Brazilian red propolis and plant resin of Dalbergia ecastaphyllum (L) Taub. Food Chem. Toxicol. 2018, 119, 215–221. [Google Scholar] [CrossRef]
- Duran, N.; Muz, M.; Culha, G.; Duran, G.; Ozer, B. GC-MS analysis and antileishmanial activities of two Turkish propolis types. Parasitol. Res. 2011, 108, 95–105. [Google Scholar] [CrossRef]
- Duran, G.; Duran, N.; Culha, G.; Ozcan, B.; Oztas, H.; Ozer, B. In vitro antileishmanial activity of Adana propolis samples on Leishmania tropica: A preliminary study. Parasitol. Res. 2008, 102, 1217–1225. [Google Scholar] [CrossRef]
- Grecco, S.d.S.; Reimão, J.Q.; Tempone, A.G.; Sartorelli, P.; Cunha, R.L.; Romoff, P.; Ferreira, M.J.; Fávero, O.A.; Lago, J.H.G. In vitro antileishmanial and antitrypanosomal activities of flavanones from Baccharis retusa DC.(Asteraceae). Exp. Parasitol. 2012, 130, 141–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaur, G.; Chauhan, K.; Kaur, S. Lupeol induces immunity and protective efficacy in a murine model against visceral leishmaniasis. Parasitology 2019, 146, 1440–1450. [Google Scholar] [CrossRef]
- Lopes, S.P.; Yepes, L.M.; Pérez-Castillo, Y.; Robledo, S.M.; de Sousa, D.P. Alkyl and Aryl Derivatives Based on p-Coumaric Acid Modification and Inhibitory Action against Leishmania braziliensis and Plasmodium falciparum. Molecules 2020, 25, 3178. [Google Scholar] [CrossRef]
- Cuesta-Rubio, O.; Fernández, M.C.; Hernández, I.M.; Jaramillo, C.G.J.; González, V.H.; Porto, R.M.D.O.; Delange, D.M.; Fidalgo, L.M.; Piccinelli, A.L.; Campone, L. Chemical profile and anti-leishmanial activity of three Ecuadorian propolis samples from Quito, Guayaquil and Cotacachi regions. Fitoterapia 2017, 120, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Rebouças-Silva, J.; Celes, F.S.; Lima, J.B.; Barud, H.S.; de Oliveira, C.I.; Berretta, A.A.; Borges, V.M. Parasite killing of Leishmania (V) braziliensis by standardized propolis extracts. Evid. -Based Complementary Altern. Med. 2017, 2017, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machado, G.M.D.C.; Leon, L.L.; Castro, S.L.D. Activity of Brazilian and Bulgarian propolis against different species of Leishmania. Memórias Do Inst. Oswaldo Cruz 2007, 102, 73–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Silva, S.S.; Thomé, G.D.S.; Cataneo, A.H.D.; Miranda, M.M.; Felipe, I.; Andrade, C.G.T.D.J.; Watanabe, M.A.E.; Piana, G.M.; Sforcin, J.M.; Pavanelli, W.R. Brazilian propolis antileishmanial and immunomodulatory effects. Evid. -Based Complementary Altern. Med. 2013, 2013, 673058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pontin, K.; Da Silva Filho, A.A.; Santos, F.F.; e Silva, M.L.A.; Cunha, W.R.; Nanayakkara, N.D.; Bastos, J.K.; de Albuquerque, S. In vitro and in vivo antileishmanial activities of a Brazilian green propolis extract. Parasitol. Res. 2008, 103, 487–492. [Google Scholar] [CrossRef]
- Miranda, M.M.; Panis, C.; Cataneo, A.H.D.; Da Silva, S.S.; Kawakami, N.Y.; Lopes, L.G.d.F.; Morey, A.T.; Yamauchi, L.M.; Andrade, C.G.T.D.J.; Cecchini, R. Nitric oxide and Brazilian propolis combined accelerates tissue repair by modulating cell migration, cytokine production and collagen deposition in experimental leishmaniasis. PLoS ONE 2015, 10, e0125101. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, F.M.; Castro, R.A.; Batista, M.A.; Rossi, F.M.; Silveira-Lemos, D.; Frézard, F.; Moura, S.A.; Rezende, S.A. Association of water extract of green propolis and liposomal meglumine antimoniate in the treatment of experimental visceral leishmaniasis. Parasitol. Res. 2014, 113, 533–543. [Google Scholar] [CrossRef]
- Asfaram, S.; Fakhar, M.; Keighobadi, M.; Akhtari, J. Promising Anti-Protozoan Activities of Propolis (Bee Glue) as Natural Product: A Review. Acta Parasitol. 2020, 66, 1–12. [Google Scholar] [CrossRef]
- Simoben, C.V.; Ntie-Kang, F.; Akone, S.H.; Sippl, W. Compounds from African medicinal plants with activities against selected parasitic diseases: Schistosomiasis, trypanosomiasis and leishmaniasis. Nat. Prod. Bioprospecting 2018, 8, 151–169. [Google Scholar] [CrossRef] [Green Version]
- Leung, A.K.; Leung, A.A.; Wong, A.H.; Sergi, C.M.; Kam, J.K. Giardiasis: An overview. Recent Pat. Inflamm. Allergy Drug Discov. 2019, 13, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Vivancos, V.; González-Alvarez, I.; Bermejo, M.; Gonzalez-Alvarez, M. Giardiasis: Characteristics, pathogenesis and new insights about treatment. Curr. Top. Med. Chem. 2018, 18, 1287–1303. [Google Scholar] [CrossRef]
- Calzada, F.; Bautista, E. Plants used for the treatment of diarrhoea from Mexican flora with amoebicidal and giadicidal activity, and their phytochemical constituents. J. Ethnopharmacol. 2020, 253, 112676. [Google Scholar] [CrossRef] [PubMed]
- Alday-Provencio, S.; Diaz, G.; Rascon, L.; Quintero, J.; Alday, E.; Robles-Zepeda, R.; Garibay-Escobar, A.; Astiazaran, H.; Hernandez, J.; Velazquez, C. Sonoran propolis and some of its chemical constituents inhibit in vitro growth of Giardia lamblia trophozoites. Planta Med. 2015, 81, 742–747. [Google Scholar] [CrossRef] [Green Version]
- Freitas, S.; Shinohara, L.; Sforcin, J.; Guimarães, S. In vitro effects of propolis on Giardia duodenalis trophozoites. Phytomedicine 2006, 13, 170–175. [Google Scholar] [CrossRef]
- David, É.B.; de Carvalho, T.B.; Oliveira, C.M.; Coradi, S.T.; Sforcin, J.M.; Guimarães, S. Characterisation of protease activity in extracellular products secreted by Giardia duodenalis trophozoites treated with propolis. Nat. Prod. Res. 2012, 26, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Fattah, N.S.; Nada, O.H. Effect of propolis versus metronidazole and their combined use in treatment of acute experimental giardiasis. J. Egypt. Soc. Parasitol. 2007, 37, 691–710. [Google Scholar]
- Rossignol, J.-F. Cryptosporidium and Giardia: Treatment options and prospects for new drugs. Exp. Parasitol. 2010, 124, 45–53. [Google Scholar] [CrossRef]
- Ozioma, E.-O.J.; Chinwe, O.A.N. Herbal medicines in African traditional medicine. Herb. Med. 2019, 10, 191–214. [Google Scholar]
- Capela, R.; Moreira, R.; Lopes, F. An Overview of Drug Resistance in Protozoal Diseases. Int. J. Mol. Sci. 2019, 20, 5748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, F.E. History of human parasitology. Clin. Microbiol. Rev. 2002, 15, 595–612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hotez, P.J.; Brindley, P.J.; Bethony, J.M.; King, C.H.; Pearce, E.J.; Jacobson, J. Helminth infections: The great neglected tropical diseases. J. Clin. Investig. 2008, 118, 1311–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spiegler, V.; Liebau, E.; Hensel, A. Medicinal plant extracts and plant-derived polyphenols with anthelmintic activity against intestinal nematodes. Nat. Prod. Rep. 2017, 34, 627–643. [Google Scholar] [CrossRef]
- Garcia-Bustos, J.F.; Sleebs, B.E.; Gasser, R.B. An appraisal of natural products active against parasitic nematodes of animals. Parasites Vectors 2019, 12, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Hegazi, A.G.; Abd El Hady, F.K.; Shalaby, H.A. Inhibitory effect of Egyptian propolis on Fasciola gigantica eggs with reference to its effect on Clostridium oedematiens and correlation to chemical composition. Pak. J. Biol. Sci. Pjbs 2007, 10, 3295. [Google Scholar] [CrossRef]
- Hegazi, A.G.; Abd El Hady, F.K.; Shalaby, H.A. An in vitro effect of propolis on adult worms of Fasciola gigantica. Vet. Parasitol. 2007, 144, 279–286. [Google Scholar] [CrossRef]
- Mahmoud, T.Y.; Rizk, S.M.; Maghraby, A.S.; Shaheen, A.A. Propolis enhances the effectiveness of praziquantel in experimental schistosomiasis: Biochemical and histopathological study. Parasitol. Res. 2014, 113, 4513–4523. [Google Scholar] [CrossRef]
- Kismet, K.; Kilicoglu, B.; Koru, O.; Tanyuksel, M.; Oruc, M.T.; Sorkun, K.; Salih, B.; Akkus, M.A. Evaluation on scolicidal efficacy of propolis. Eur. Surg. Res. 2006, 38, 476–481. [Google Scholar] [CrossRef]
- Sinott, F.A.; Sena-Lopes, Â.; Leal, K.S.; de Oliveira Silva, M.T.; de Freitas, M.C.; de Moura, M.Q.; Berne, M.E.A.; Borsuk, S. Essential oil from Brazilian Red Propolis exhibits anthelmintic activity against larvae of Toxocara cati. Exp. Parasitol. 2019, 200, 37–41. [Google Scholar] [CrossRef]
- Siheri, W.; Ebiloma, G.U.; Igoli, J.O.; Gray, A.I.; Biddau, M.; Akrachalanont, P.; Alenezi, S.; Alwashih, M.A.; Edrada-Ebel, R.; Muller, S. Isolation of a novel flavanonol and an alkylresorcinol with highly potent anti-trypanosomal activity from Libyan propolis. Molecules 2019, 24, 1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caesar, L.K.; Cech, N.B. Synergy and antagonism in natural product extracts: When 1+ 1 does not equal 2. Nat. Prod. Rep. 2019, 36, 869–888. [Google Scholar] [CrossRef] [Green Version]
- Bdir, S.; Adwan, G. Prevalence of intestinal parasitic infections in Jenin Governorate, Palestine: A 10–year retrospective study. Asian Pac. J. Trop. Med. 2010, 3, 745–747. [Google Scholar] [CrossRef] [Green Version]
- Harizanov, R.; Rainova, I.; Tsvetkova, N.; Kaftandjiev, I.; Borisova, R.; Ivanova, A.; Videnova, M. Prevalence of intestinal parasitic infections among the Bulgarian population over a three year period (2015–2017). Helminthologia 2020, 57, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van den Enden, E. Pharmacotherapy of helminth infection. Expert Opin. Pharmacother. 2009, 10, 435–451. [Google Scholar] [CrossRef]
- Humphries, D.; Nguyen, S.; Boakye, D.; Wilson, M.; Cappello, M. The promise and pitfalls of mass drug administration to control intestinal helminth infections. Curr. Opin. Infect. Dis. 2012, 25, 584–589. [Google Scholar] [CrossRef]
- Waller, P. From discovery to development: Current industry perspectives for the development of novel methods of helminth control in livestock. Vet. Parasitol. 2006, 139, 1–14. [Google Scholar] [CrossRef]
- Cobo, F.; Talavera, P.; Concha, A. Diagnostic approaches for viruses and prions in stem cell banks. Virology 2006, 347, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Owen, J.A.; Punt, J.; Stranford, S.A. Kuby Immunology; WH Freeman: New York, NY, USA, 2013. [Google Scholar]
- Reta, D.H.; Tessema, T.S.; Ashenef, A.S.; Desta, A.F.; Labisso, W.L.; Gizaw, S.T.; Abay, S.M.; Melka, D.S.; Reta, F.A. Molecular and Immunological Diagnostic Techniques of Medical Viruses. Int. J. Microbiol. 2020, 2020, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, A.; Duran, G.G.; Duran, N.; Jenedi, K.; Bolgul, B.S.; Miraloglu, M.; Muz, M. Antiviral activity of hatay propolis against replication of herpes simplex virus type 1 and type 2. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 422. [Google Scholar] [CrossRef]
- Amoros, M.; Sauvager, F.; Girre, L.; Cormier, M. In vitro antiviral activity of propolis. Apidologie 1992, 23, 231–240. [Google Scholar] [CrossRef] [Green Version]
- Schnitzler, P.; Neuner, A.; Nolkemper, S.; Zundel, C.; Nowack, H.; Sensch, K.H.; Reichling, J. Antiviral activity and mode of action of propolis extracts and selected compounds. Phytother. Res. 2010, 24, S20–S28. [Google Scholar] [CrossRef] [PubMed]
- Nolkemper, S.; Reichling, J.; Sensch, K.H.; Schnitzler, P. Mechanism of herpes simplex virus type 2 suppression by propolis extracts. Phytomedicine 2010, 17, 132–138. [Google Scholar] [CrossRef]
- Gekker, G.; Hu, S.; Spivak, M.; Lokensgard, J.R.; Peterson, P.K. Anti-HIV-1 activity of propolis in CD4+ lymphocyte and microglial cell cultures. J. Ethnopharmacol. 2005, 102, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Hino, A.; Tsutsumi, A.; Park, Y.K.; Watanabe, W.; Kurokawa, M. Anti-influenza virus activity of propolis in vitro and its efficacy against influenza infection in mice. Antivir. Chem. Chemother. 2008, 19, 7–13. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, T.; Takeshita, Y.; Takamori, Y.; Kai, H.; Sawamura, R.; Yoshida, H.; Watanabe, W.; Tsutsumi, A.; Park, Y.K.; Yasukawa, K. Efficacy of Brazilian propolis against herpes simplex virus type 1 infection in mice and their modes of antiherpetic efficacies. Evid. -Based Complementary Altern. Med. 2011, 2011, 976196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madhav, N.; Oppenheim, B.; Gallivan, M.; Mulembakani, P.; Rubin, E.; Wolfe, N. Pandemics: Risks, impacts, and mitigation. In Disease Control Priorities: Improving Health and Reducing Poverty, 3rd ed; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2017; Chapter 17. [Google Scholar]
- Mohammadpour, M.; Zarifinezhad, E.; Ghanbarzadegan, A.; Naderimanesh, K.; Shaarbafchizadeh, N.; Bastani, P. Main Factors Affecting the Readiness and Responsiveness of Healthcare Systems during Epidemic Crises: A Scoping Review on Cases of SARS, MERS, and COVID-19. Iran. J. Med Sci. 2021, 46, 81–92. [Google Scholar] [PubMed]
- Bankova, V.; Galabov, A.; Antonova, D.; Vilhelmova, N.; Di Perri, B. Chemical composition of Propolis Extract ACF® and activity against herpes simplex virus. Phytomedicine 2014, 21, 1432–1438. [Google Scholar] [CrossRef]
- Maatouk, M.; Elgueder, D.; Mustapha, N.; Chaaban, H.; Bzéouich, I.M.; Loannou, I.; Kilani, S.; Ghoul, M.; Ghedira, K.; Chekir-Ghedira, L. Effect of heated naringenin on immunomodulatory properties and cellular antioxidant activity. Cell Stress Chaperones 2016, 21, 1101–1109. [Google Scholar] [CrossRef] [Green Version]
- Shen, H.; Yamashita, A.; Nakakoshi, M.; Yokoe, H.; Sudo, M.; Kasai, H.; Tanaka, T.; Fujimoto, Y.; Ikeda, M.; Kato, N. Inhibitory effects of caffeic acid phenethyl ester derivatives on replication of hepatitis C virus. PLoS ONE 2013, 8, e82299. [Google Scholar] [CrossRef]
- Wang, R.; Hu, H.; Chen, X.; Yin, Z.; Liang, X.; He, C.; Yin, L.; Ye, G.; Zou, Y.; Li, L. The Antiviral Activity of Kaempferol Against Pseudorabies Virus in Mice. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Xu, X.; Miao, J.; Shao, Q.; Gao, Y.; Hong, L. Apigenin suppresses influenza A virus-induced RIG-I activation and viral replication. J. Med Virol. 2020, 92, 3057–3066. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Gu, X.; Zhang, M.; Lv, X.; Zhang, C.; Li, J.; Hu, Z.; Wu, Q.; Zhang, R.; Wei, J. Epigallocatechin-3-gallate exhibits antiviral effects against the duck Tembusu virus via blocking virus entry and upregulating type I interferons. Poult. Sci. 2021, 100, 100989. [Google Scholar] [CrossRef] [PubMed]
- Jautová, J.; Zelenková, H.; Drotarová, K.; Nejdková, A.; Grünwaldová, B.; Hladiková, M. Lip creams with propolis special extract GH 2002 0.5% versus aciclovir 5.0% for herpes labialis (vesicular stage). Wien. Med. Wochenschr. 2019, 169, 193–201. [Google Scholar] [CrossRef] [Green Version]
- Tomanova, D.; Holcova, S.; Hladikova, M. Clinical study: Lotion containing propolis special extract GH 2002 0.5% vs. placebo as on-top treatment of herpes zoster. Health 2017, 9, 1337. [Google Scholar] [CrossRef] [Green Version]
- Berretta, A.A.; Silveira, M.A.D.; Capcha, J.M.C.; De Jong, D. Propolis and its potential against SARS-CoV-2 infection mechanisms and COVID-19 disease. Biomed. Pharmacother. 2020, 131, 110622. [Google Scholar] [CrossRef] [PubMed]
- Ripari, N.; Sartori, A.A.; da Silva Honorio, M.; Conte, F.L.; Tasca, K.I.; Santiago, K.B.; Sforcin, J.M. Propolis antiviral and immunomodulatory activity: A review and perspectives for COVID-19 treatment. J. Pharm. Pharmacol. 2021, 73, 281–299. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Kunugi, H. Propolis, bee honey, and their components protect against coronavirus disease 2019 (COVID-19): A review of in silico, in vitro, and clinical studies. Molecules 2021, 26, 1232. [Google Scholar] [CrossRef] [PubMed]
- Gismondi, A.; Di Marco, G.; Canini, A. Detection of plant microRNAs in honey. PLoS ONE 2017, 12, e0172981. [Google Scholar]
- Zhu, K.; Liu, M.; Fu, Z.; Zhou, Z.; Kong, Y.; Liang, H.; Lin, Z.; Luo, J.; Zheng, H.; Wan, P. Plant microRNAs in larval food regulate honeybee caste development. Plos Genet. 2017, 13, e1006946. [Google Scholar] [CrossRef]
| Propolis Origin | Bacterial Species | Activity | Ref. |
|---|---|---|---|
| Brazil (red, green, and brown propolis from different regions) | S. aureus | Red extracts showed highest activity compared with green and brown extracts (MIC: 25–200 μg/mL both propolis) | [30] |
| Poland | Twelve MSSA and MRSA clinical isolates | Displayed variable effectiveness against twelve clinical isolates (MBC: 0.78–3.13 mg/mL) | [32] |
| Germany, Ireland, and Czech Republic | S. aureus, MRSA, and S. epidermidis | The three propolis showed moderate antibacterial activity (MIC: 0.08–2.5 mg/mL) | [28] |
| Italy | Staphylococcus spp. and S. aureus | Propolis (MIC: 0.31–2.5 mg/mL) showed inhibitory action on the lipase activity of 18 Staphylococcus spp. and an inhibition on coagulase of 11 S. aureus strains; showed inhibition of adhesion and consequent biofilm growth of S. aureus | [33] |
| Serbia (53 samples from different regions; blue and orange propolis) | S. aureus | All propolis samples showed antibacterial activity, with orange-type (0.1–14.7 mg/mL) showing higher activity than blue-type propolis samples (1.8–12.9 mg/mL) | [34] |
| Propolis/ Compound | Bacterial Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Brazil (red, green, and brown propolis from diverse regions) | S. aureus | Ferulic acid, gallic acid, caffeic acid, coumaric acid, p-coumaric acid, catechin, drupanin, kaempferide, artepillin C, luteolin, and pinocembrin | All propolis showed distinct antibacterial activities (200–1600 µg/mL) | [40,41,42] |
| Poland (25 different samples) | S. aureus and S. epidermidis; 16 MSSA and four MRSA clinical isolates | Flavonols, flavones, flavanones, pinocembrin, chrysin, pinobanksin, apigenin, kaempferol, p-coumaric acid, ferulic acid, and caffeic acid | All propolis (1–8 mg/mL) showed distinct antibacterial effect on S. aureus and S. epidermidis; in the clinical isolates, all the samples of propolis presented different activities and two of them showed higher antistaphylococcal activity; propolis effectively eradicated staphylococcal biofilm | [27,43] |
| Pinocembrin, galangin, and chrysin (South African propolis) | S. aureus | Pinocembrin, galangin, and chrysin | The combinations of these three flavonoids presented higher inhibition than alone flavonoids (0.04–0.26 mg/mL) | [44] |
| Propolis Origin | Antibiotics | Bacterial Species | Activity | Ref. |
|---|---|---|---|---|
| Ireland | Two-drug combinations: vancomycin, oxacillin, and levofloxacin | MRSA | Propolis (MIC: 0.4–5 mg/mL) synergistically enhanced the efficacy of antibiotics, especially those acting on cell wall synthesis (vancomycin (0.2 mg/mL) and oxacillin (12.5 mg/mL)) on drug-resistant bacteria | [28] |
| Poland | Amikacin, kanamycin, gentamycin, tetracycline, and fusidic acid | S. aureus | Propolis (16–32 µg/mL) showed a synergistic effect in combination with various antibiotics (1–0.0312 µg/mL) that inhibit protein synthesis | [27] |
| Cefoxitin, clindamycin, tetracycline, tobramycin, linezolid, trimethoprim + sulfamethoxazole, penicillin, and erythromycin | S. aureus clinical isolates | The combination of propolis (MIC: 0.39–0.78 mg/mL) with different drugs potentiated the antibacterial effect of eight antistaphylococcals (1–30 µg/mL) against all strains | [32] | |
| Italy | Ampicillin, gentamycin, streptomycin, chloramphenicol, ceftriaxone, and vancomycin | S. aureus and S. epidermidis. | Propolis increased the antibacterial effect of ampicillin (0.05–3.12 µg/mL), gentamycin (0.05–1.56 µg/mL), and streptomycin (0.05–50 µg/mL); moderately for chloramphenicol (0.05–25 µg/mL), ceftriaxone, and vancomycin (0.39–3.15 µg/mL) | [33] |
| Nanoparticles prepared with Malaysian propolis | Rifampicin, ciprofloxacin, vancomycin, and doxycycline | S. epidermidis | Propolis nanoparticles (15.63–125 µg/mL disrupted bacterial biofilms by causing membrane damage and significantly reducing biofilm formation, and showed synergism with antibiotics (0.2–25 µg/mL) | [46] |
| Propolis/ Compound | Bacterial Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Germany, Ireland, and Czech Republic | S. pyogenes and S. pneumoniae | N. I. | Moderate antibacterial activity (MIC: 0.6–5 mg/mL) | [28] |
| Mexico | S. mutans | Pinocembrin, chrysin, galangin, alpinetin, dillenetin, isorhamnetin, ferulic acid, syringic acid, and caffeic acid | Propolis (MIC: 125–1024 µg/mL) presented antibacterial activity; galangin, ferulic acid, syringic acid, and caffeic acid showed activity against this oral pathogen | [50] |
| South of Brazil (different samples) | S. mutans | Gallic acid, caffeic acid, coumaric acid, artepillin C, and pinocembrin | All samples of propolis (25–800 µg/mL) have an inhibitory action biofilm growth | [42] |
| Iran/ quercetin | S. mutans and S. pneumoniae | Quercetin | Both propolis (MIC: 3.12–100 µg/mL) were efficient against the bacteria studied and showed an inhibitory activity S. mutans biofilm adherence | [51] |
| Propolis/ Compound | Bacterial Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Germany, Ireland, and Czech Republic | E. coli, S. choleraesuis, and S. flexneri | N.I. | All showed moderate antibacterial activity (MIC: 0.6–5 mg/mL) | [28] |
| Brazil (red, green, and brown propolis) and Southern Poland | E. coli and L. monocytogenes | Ferulic acid, p-coumaric acid, caffeic acid, catechin, luteolin, drupanin, kaempferide, artepillin C, pinocembrin, chrysin, pinobanksin, apigenin, and kaempferol | All samples showed distinct antibacterial activities (25–800 µg/mL) | [40,41,43] |
| Pinocembrin, galangin, and chrysin (South African propolis) | L. monocytogenes and E. coli | Pinocembrin, galangin, and chrysin | The combinations of these three flavonoids (0.04–0.26 mg/mL) presented higher inhibition activity than alone components | [44] |
| Propolis Origin | Bacterial Species | Activity | Ref. |
|---|---|---|---|
| Brazil (red, green, and brown propolis from different regions) | Klebsiella sp. | Red extracts showed higher activity than green and brown extracts (MIC: 31.1–1000 µg/mL both propolis) | [30] |
| Germany, Ireland, and Czech Republic | P. aeruginosa, H. influenzae, K. pneumoniae, and two clinical isolates of K. pneumoniae | All propolis showed moderate antibacterial activity (0.06–2.5 µg/mL) | [28] |
| Cameroon, Congo, and Kenya | K. pneumoniae and P. aeruginosa | All propolis showed differences in antibacterial activity (50 mg/mL) | [35,36] |
| Propolis/ Compound | Bacterial Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Albania | P. aeruginosa | Caffeic acid, p-coumaric acid, ferulic acid, isoferulic acid, quercetin, apigenin, pinobanksin, chrysin, pinocembrin, galangin, and CAPE | Propolis (15.6–62.5 mg/mL) inhibited the microbial development and biofilm growth, also decreased extracellular DNA release and phenazine production | [61] |
| Pinocembrin, galangin, and chrysin (South African propolis) | P. aeruginosa and K. pneumoniae | Pinocembrin, galangin, and chrysin | Combinations of the three flavonoids (0.6–25 µg/mL) present better antibacterial effect than single components | [44] |
| Propolis Origin | Fungal Species | Activity | Ref. |
|---|---|---|---|
| Brazil (green propolis) | Vaginal isolates of C. albicans | Suppress growth and biofilm formation | [81] |
| Brazil | C. albicans, C. glabrata, C. tropicalis, C. guilliermondii, and C. parapsilosis | All strains were suppressed, with minimal variation independent of the yeast species (273.43 μg/mL) | [80] |
| C. albicans | Showed fungicidal activity against the three morphogenetic types; the induced cell death was mediated by metacaspase and Ras signaling | [82] | |
| Brazil (topical pharmaceutical preparation based upon propolis) | Vulvovaginal candidiasis infection in a mouse model (C. albicans) | Can partially control C. albicans infections (0.05%, 0.1%, and 0.2%) | |
| Poland (different samples) | Azole-resistant C. albicans, C. glabrata, and C. krusei clinical isolates | Only one of the four propolis samples revealed high activity (MFC: 0.0006–1.25% v/v) | [83] |
| Portugal and France | C. albicans and C. glabrata | Presented distinct antifungal activities (15.63–250 μg/mL) | [31,84] |
| Germany, Ireland, and Czech Republic | C. albicans, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei | Propolis from Ireland and Czech demonstrated excellent fungicidal (0.1–5 mg/mL) effects; propolis from Germany showed mostly fungistatic (0.1–2.5 mg/mL) activity. C. glabrata, C. parapsilosis, and C. tropicalis were the most sensitive. | [28] |
| Saudi Arabia | C. zeylanoides, C. famata, C. sphaerica, C. guilliermondii, C. magnoliae, C. colliculosa, C. krusei, C. pelliculosa, and C. parapsilosis | Showed fungicidal (2.5% v/v) and fungistatic (5%) effects against different strains | [85] |
| Iran | 22 samples of C. albicans and one sample of C. glabrata isolates from oral cavities of patients with clinical oral candidiasis | Both extracts showed inhibitory effects on Candida, but the extract that presented greater effectiveness even above the aqueous (0.2–130 mg/mL) one was the ethanolic (0.4–210 mg/mL) | [87] |
| Propolis-loaded nanoparticles from Thailand | C. albicans | Inhibited the virulence factors of C. albicans, such as adhesion, hyphal germination, biofilm formation, and invasion (1 and 2 mg/mL) | [88] |
| Propolis Origin | Fungal Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Brazil | C. albicans and C. parapsilosis | Caffeic acid, p-coumaric acid, cinnamic acid, aromadendrin, artepillin C | Showed fungicide (0.5%) action on different strains; C. albicans being the most sensitive, and C. parapsilosis being the most resistant | [92] |
| Brazil (propolis-based gels) | Vaginal candidiasis mouse model | Presented antifungal effect (1%) similar to clotrimazole cream | ||
| Poland (50 different samples) | 69 C. albicans, 10 C. glabrata, and 10 C. krusei clinical isolates | Caffeic acid, p-coumaric acid, ferulic acid, quercetin, pinobanksin, luteolin, kaempferol, apigenin, pinocembrin, acacetin, galangin, kaempferide, and naringenin | All samples showed high activity in the inhibition of biofilm formation by C. glabrata and C. krusei (0.04–1.25% v/v); inhibited yeast-to-mycelia morphological change and mycelial growth of C. albicans (0.16–0.31% v/v); propolis combined with fluconazole and voriconazole on C. albicans (0.5–512 μg/mL) was shown to have a clear synergism | [66] |
| Poland (from agricultural areas and Southern Poland) | C. albicans and C. krusei | Pinocembrin, chrysin, pinobanksin, apigenin, kaempferol, p-coumaric acid, ferulic acid, and caffeic acid | Samples from Southern Poland showed greater antifungal activity (2–16 mg/mL) | [43] |
| Propolis Origin | Fungal Species | Activity | Ref. |
|---|---|---|---|
| Brazil (red and green propolis) | T. rubrum, T. tonsurans, and T. mentagrophytes | Both propolis were active on the strains, but the red propolis was more efficient than the green (256–1024 µg/mL) | [100] |
| Brazil (green propolis) | Clinical isolates of T. rubrum and T. interdigitale from onychomycosis cases | Propolis had the ability to decrease the cells in the preformed Trichophyton biofilm (0.044–0.088 mg/mL) | [101] |
| Brazil (topical green propolis treatment) | Sixteen patients with onychomycosis | Treatment showed a complete mycological and clinical cure of onychomycosis (10%) |
| Propolis Origin | Parasitic Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Cuba (20 different samples) | P. falciparum. | Liquiritigenin and lupeol | Three samples of propolis (0.2 μg/mL) shows activity against P. falciparum | [120] |
| Libya (12 different samples) | N.I. | All samples of propolis (1.65–53.6 μg/mL) showed antiprotozoal activity | [121] | |
| Iran (four different samples) | Palmitic acid, stearic acid, pinocembrin, tectochrysin, and 4′,5-dihidroxy-7-methoxyflavanone | All samples of propolis presented antimalarial in vitro and in vivo activity at different concentrations (16.2–80 μg/mL) | [122] | |
| Saudi Arabia | P. chabaudi-infected mice | N.I. | Considerably suppressed the parasitemia and demosntraed important effect in decresing anemic in infected mice (25–100 mg/Kg), reduced oxidative damage by enhancing the catalase function and the glutathione concentrations, and enhanced the quantity of TNF-α, IFN-γ, G-CSF, and GM-CSF. | [123] |
| Propolis Origin | Parasitic Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Brazil | T. cruzi | N.I. | Activity on T. cruzi trypomastigotes. | [30] |
| N.I. | Effective on the three forms of the parasite strongly inhibits infection levels promoting lysis of bloodstream trypomastigotes, diminishing the number of parasites in peritoneal macrophages and infected heart muscle cells (0.1–0.75 mg/mL) | [128] | ||
| Caffeic acid, cinnamic acid, pantenoic acid, ferulic acid, linoleic acid, amyrin, pinostobin | In vitro effect against T. cruzi (0.4–1.4 mg/mL) | [129,130] | ||
| 3-prenyl-4-hydroxycinnamic acid and 2,2-dimethyl-6-carboxyethenyl-8-prenyl-2H-1-benzopyran. | Propolis (2.64 mg/mL) and its compounds (0.73–1.2 mg/mL) identified showed anti-trypanosome effects | [131] | ||
| Brazil and Bulgaria | N.I. | Both propolis (0.015–1.5 mg/mL) showed activity against T. cruzi, diminishing the infection and the intracellular replication of amastigotes; in epimastigotes, the main targets are the mitochondrion and reservosomes | [132] | |
| Bulgaria (two different samples) | Caffeic acid, stearic acid, oleic acid, ferulic acid, coumaric acid, pinocembrin, chrysin, pinostrobin | Both samples of propolis had great inhibition effect mainly on T. cruzi epimastigotes (48.6–84.8 mg/mL); effect on trypomastigotes (160.5–1065.8 mg/mL) was similar to that of the reference drug | [133] | |
| Bulgaria | T. cruzi-infected mice. | N.I. | Reduced parasitemia and showed no toxic hepatic or renal effect, decreased spleen mass, modulated the initial inflammatory reaction, favored a greater number of CD8+, and partially inhibited the increase in CD4 (50mg/Kg) | [134] |
| Brazil | N.I. | Reduced parasitemia enhanced the survival of the animals, and did not induce any hepatic, muscular lesion, or renal toxicity (25–300 mg/Kg) | [135] |
| Propolis Origin | Parasitic Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Brazil (brown, green, and red propolis) and Portugal | L. braziliensis, L. infantum, and L. amazonensis | N.I. | All inhibited the growth of promastigotes of distinct parasitic strains and effectively reduced number of internalized amastigotes in infected murine macrophages (36–250 mg/mL) | [84,139,140,141] |
| Turkey (Three regions: Adana, Hatay, and Bursa) | L. tropica and L. infantum | Adana: cembrene; Hatay: chrysin; Bursa: cinnamyl cinnamate | All propolis (50–1000 μg/mL) showed good antileishmanial activity, but that of Bursa was the most effective | [142,143] |
| Cuba (20 different samples) | L. infantum | Amyrin, lupeol, and cycloartenol | All samples of propolis (3.2–22.2 μg/mL) presented antiprotozoal properties | [120] |
| Ecuador (three different samples) | L. amazonensis | Naringenin, sakuranetin, eupatolitin, and rhamnazin | All inhibited L. amazonensis growth, but the sample rich in flavonoids was the most effective (12.5–200 mg/mL) | [147] |
| Brazil (two different samples) | L. amazonensis, L. braziliensis, L. chagasi, and L. major | Minas Gerais: diethyl 2-methylsuccinate, cinnamic acid, pentanedioc acid, and hydrocinnamic acid; Ribeirao Petro: artepillin C, 4,5-dicaffeoylquinic acid, p-coumaric acid, and drupanin | Both showed great antileishmanial activity. Ribeirao Petro propolis exhibited a dose-dependent effect against promastigotes of L. amazonensis and controlled the parasite burden inside infected macrophages (2.8–229.3 μg/mL) | [148,149] |
| Brazil | L. braziliensis-infected mice | N.I. | Reduced growth by promoting morphologic alterations in promastigotes; in supernatants from liver cells and peritoneal exudate of mice pretreated with propolis and infected, increased TNF-α production was seen (5–100 μg/mL) | [150] |
| Brazil (green propolis) | N.I. | Decreases lesion development caused by L. braziliensis more than 75%, while the glucantime treatment showed a 57.7% decrease (10–250 μg/mL) | [151] |
| Propolis Origin | Substances | Infection Model | Activity | Ref. |
|---|---|---|---|---|
| Brazil | Nitric oxide | L. braziliensis-infected mice | The combination of propolis (5 mg/kg) with NO favored the healing, collagen synthesis, the function of macrophages and fibroblasts, reduced expression of proinflammatory and tissue damage markers | [152] |
| Brazil (green propolis) | Liposomal meglumine antimoniate | L. infantum-infected mice | Reduced the parasitic burden in the liver, without damaging kidney, liver, spleen, and heart (500 mg/kg) | [153] |
| Propolis Origin | Parasitic Species | Activity | Ref. |
|---|---|---|---|
| Mexico (Sonoran Desert, region Ures) | G. lamblia | Inhibitory activity against G. lamblia in a dose-dependent manner (63.8 μg/mL) | [159] |
| Brazil | Effectively eliminated trophozoites of G. lamblia (125 μg/mL) | [160,161] | |
| Egypt | G. lamblia-infected immunodeficient mice | Reduces infection, enhanced IFN-γ serum level and CD4+:CD8+ T cell ratio. Co-administration of propolis and metronidazole had remarkable activity in controlling the parasite number. Favors intestinal homeostasis and the histological integrity (NS) | [162] |
| Propolis Origin | Parasitic Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Egypt | F. gigantica | Diprenyl-dihydrocoumaric acids, coumarate esters, ferulate esters, hydroxy acetophenones, furanon derivative, furofuran lignans, benzofuran lignans, and valeric acids derivatives | Alteration in the architecture, inhibitory activity on the viability and hatchability of immature helminths (10–800 μg/mL) | [170,171] |
| S. mansoni-infected mice | N.I. | Propolis administration (500 mg/kg) not eliminated the worms of infected mice, but significantly reduced the hepatic granuloma number, hepatic, splenic and plasma MPO activity, as well the liver and thymus NO levels; also, regulation of plasma antioxidant proteins evidenced by decrease in MDA and normalization of GSH | [172] | |
| Turkey | E. granulosus | N.I. | Propolis (1 µg/mL) killed all the protoscoleces | [173] |
| Brazil (essential oil of red propolis) | T. cati | N.I. | Have 100% larvicidal effect after treatment (1 µg/mL) of 48 h and can suppress the ability of the treated T. cati larvae to infect the mice | [174] |
| Libya (five different samples) | T. spiralis | Cycloartanol, mangiferolic acid, agathadiol, isocupressic acid, isoagatholal | All propolis samples (4.7–59.3 μg/mL) showed moderate activity | [175] |
| Propolis Origin | Viral Species | Activity | Ref. |
|---|---|---|---|
| Czech Republic (aqueous and ethanolic extract) | HSV-2 | Both propolis (0.0005–0.005%) decreased the infection and exhibited a concentration- and time-dependent antiviral effect; high antiviral effect when viruses were pretreated prior to infection | [188] |
| United States, Brazil, and China | HIV-1. | Three propolis inhibited viral expression in CD4+ lymphocytes and microglial cell in a concentration-dependent manner; propolis from United States suppressed cell fusion in cultures of CD4+ lymphocytes (0.8–66.6 μg/mL) | [189] |
| Brazil (13 different samples) | Influenza virus. | Four samples had anti-influenza virus effect in vitro (10–149.2 μg/mL) | [190] |
| Influenza virus-infected mice. | Only one propolis sample (10 mg/mL) effectively prolonged the lifetimes of infected mice; anti-influenza effectiveness of propolis in mice was dose-dependent | ||
| Brazil (13 different samples) | HSV-1-infected mice | The three propolis had direct anti-HSV-1 effects, stimulated immunological effect on intradermal HSV-1 infection in mice (0.4, 2, and 10 mg/mL) | [191] |
| Propolis Origin | Parasitic Species | Identified Compounds | Activity | Ref. |
|---|---|---|---|---|
| Canada | HSV-1 and HSV-2 | Benzoic acid, cinnamic acid, vanillic acid, p-coumaric acid, ferulic acid, caffeic acid, palmitic acid, oleic acid, pinocembrin, pinobanksin, chrysin, galangin, isosakuranetin, alpinone, kaempferol, pinostrobin chalcone, and pinocembrin chalcone | Presents a pronounced viricidal effect and interfered with virus adsorption (0.1 mg/mL) | [194] |
| Turkey (south) | Gallic acid, (±)-catechin, caffeic acid, syringic acid, epigallocatechin, p-coumaric acid, trans-ferulic acid, trans-isoferulic acid, myricetin, trans-cinnamic acid, benzoic acid, daidzein, luteolin, pinobanksin, (±)-naringenin, apigenin, kaempferol, chrysin, pinocembrin, galangin, and CAPE | Suppressed the replication of HSV-1 and HSV-2; inhibited HSV-1 replication following 24 h of incubation and effect on HSV-2 at 48 h following incubation; decreased the number of viral copies; activity similar to that of acyclovir; a synergism of the propolis and acyclovir combined on HSV-1 and HSV-2 replication compared with acyclovir alone (25–3200 μg/mL) | [185] | |
| Czech Republic (aqueous and ethanolic propolis) | HSV-1 | Caffeic acid, p-coumaric acid, benzoic acid, galangin, pinocembrin, and chrysin | Both samples presented high anti-HSV-1 effect in cells pretreated prior to viral infection; galangin and chrysin were the most bioactive compounds; however, the propolis had higher antiherpetic effects than single isolated constituents (1%) | [187] |
| Propolis Origin | Model | Activity | Ref. |
|---|---|---|---|
| Central Europe (lip cream with propolis) | Patients with herpes labialis | Lip cream with propolis (0.5%) produced a better effect than acyclovir in the treatment of patients with herpes labialis in the vesicular phase | [200] |
| Central Europe (constituent of a lotion) | Herpes zoster in patients | Improvement in pain and healing of lesions were better and quicker with treatment of the propolis lotion (0.5%); approximately 50% of propolis-treated patients had no injuries on day 14 and the formation of new vesicles was suppressed | [201] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rivera-Yañez, N.; Rivera-Yañez, C.R.; Pozo-Molina, G.; Méndez-Catalá, C.F.; Reyes-Reali, J.; Mendoza-Ramos, M.I.; Méndez-Cruz, A.R.; Nieto-Yañez, O. Effects of Propolis on Infectious Diseases of Medical Relevance. Biology 2021, 10, 428. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10050428
Rivera-Yañez N, Rivera-Yañez CR, Pozo-Molina G, Méndez-Catalá CF, Reyes-Reali J, Mendoza-Ramos MI, Méndez-Cruz AR, Nieto-Yañez O. Effects of Propolis on Infectious Diseases of Medical Relevance. Biology. 2021; 10(5):428. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10050428
Chicago/Turabian StyleRivera-Yañez, Nelly, C. Rebeca Rivera-Yañez, Glustein Pozo-Molina, Claudia F. Méndez-Catalá, Julia Reyes-Reali, María I. Mendoza-Ramos, Adolfo R. Méndez-Cruz, and Oscar Nieto-Yañez. 2021. "Effects of Propolis on Infectious Diseases of Medical Relevance" Biology 10, no. 5: 428. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10050428