Clinical Significance of the Head-Up Tilt Test in Improving Prognosis in Patients with Possible Neurally Mediated Syncope
Abstract
:Simple Summary
Abstract
1. Introduction
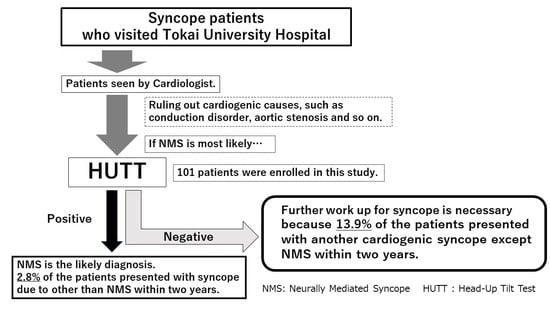
2. Materials and Methods
2.1. Ethics Statement
2.2. Patient Information and Data Collection
2.3. Head-Up Tilt Test (HUTT)
2.4. Evaluation of the HUTT Results
2.5. Follow-Up in the Patients after the HUTT
2.6. Statistical Analyses
3. Results
3.1. Patients’ Characteristics
3.2. HUTT Result
3.3. Details of 12 Lead ECG Analysis
3.4. Recurrence of Syncope after the HUTT and ICM Placement
3.5. Unexpected Cardiac Events after the HUTT
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moya, A.; Sutton, R.; Ammirati, F.; Blanc, J.J.; Brignole, M.; Dahm, J.B.; Deharo, J.-C.; Gajek, J.; Gjesdal, K. Guidelines for the diagnosis and management of syncope, 2009 version. Eur. Heart J. 2009, 30, 2631–2671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brignole, M.; Moya, A.; de Lange, F.J.; Deharo, J.C.; Elliott, P.M.; Fanciulli, A.; van Dijk, J.G. Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of Syncope. Eur. Heart J. 2018, 38, e43–e80. [Google Scholar] [CrossRef]
- Saklani, P.; Krahn, A.; Klein, G. Syncope. Circulation 2013, 127, 1330–1339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soteriades, E.S.; Evans, J.C.; Larson, M.G.; Chen, M.H.; Chen, L.; Benjamin, E.J.; Levy, D. Incidence and prognosis of syncope. N. Engl. J. Med. 2002, 347, 878–885. [Google Scholar] [CrossRef]
- Walsh, C.A. Syncope and sudden death in the adolescent. Adolesc Med. 2001, 12, 105–132. [Google Scholar]
- Komiyama, T.; Nagata, E.; Hashida, T.; Sakama, S.; Ayabe, K.; Kamiguchi, H.; Sasaki, A.; Yoshioka, K.; Kobayashi, H. Neurally mediated syncope diagnosis based on adenylate cyclase activity in Japanese patients. PLoS ONE 2019, 14, e0214733. [Google Scholar] [CrossRef]
- Hasegawa, M.; Komiyama, T.; Ayabe, K.; Sakama, S.; Sakai, T.; Lee, K.H.; Morise, M.; Yagishita, A.; Amino, M.; Sasaki, A.; et al. Diagnosis and prevention of the vasodepressor type of neurally mediated syncope in Japanese patients. PLoS ONE 2021, 16, e0251450. [Google Scholar] [CrossRef] [PubMed]
- Komiyama, T.; Hirokawa, T.; Sato, K.; Oka, A.; Kamiguchi, H.; Nagata, E.; Sakura, H.; Otsuka, K.; Kobayashi, H. Relationship between human evolution and neurally mediated syncope disclosed by the polymorphic sites of the adrenergic receptor gene α2B-AR. PLoS ONE 2015, 10, e0120788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaufmann, H.; Bhattacharya, K. Diagnosis and treatment of neurally mediated syncope. Neurologist 2002, 8, 175–185. [Google Scholar] [CrossRef]
- Brignole, M.; Menozzi, C.; Del Rosso, A.; Costa, S.; Gaggioli, G.; Bottoni, N.; Bartoli, P.; Sutton, R. New classification of haemodynamics of vasovagal syncope: Beyond the VASIS classification: Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Europace 2000, 2, 66–76. [Google Scholar] [CrossRef]
- Shen, W.K.; Sheldon, R.S.; Benditt, D.G.; Cohen, M.I.; Forman, D.E.; Goldberger, Z.D.; Grubb, B.P.; Hamdan, M.H.; Krahn, A.D.; Link, M.S. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J. Am. Coll. Cardiol. 2017, 70, e39–e110. [Google Scholar] [CrossRef]
- Grubb, B.P.; Kosinski, D. Current trends in etiology, diagnosis, and management of neurocardiogenic syncope. Curr. Opin. Cardiol. 1996, 11, 32–41. [Google Scholar] [CrossRef]
- Christou, G.A.; Kouidi, E.J.; Anifanti, M.A.; Sotiriou, P.G.; Deligiannis, A.P. A novel strategy for evaluating tilt test in athletes with syncope. Eur. J. Prev. Cardiol. 2016, 23, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Racco, F.; Sconocchini, C.; Alesi, C.; Zappelli, L.; Pratillo, G. Long-term follow-up after syncope: A group of 183 patients observed for 5 years. Minerva Cardioangiol. 2000, 48, 69–78. [Google Scholar]
- Krahn, A.D.; Klein, G.J.; Yee, R.; Hoch, J.S.; Skanes, A.C. Cost implications of testing strategy in patients with syncope: Randomized assessment of syncope trial. J. Am. Coll. Cardiol. 2003, 42, 495–501. [Google Scholar] [CrossRef] [Green Version]
- Sakhi, R.; Theuns, D.A.M.J.; Szili-Torok, T.; Yap, S.C. Insertable cardiac monitors: Current indications and devices. Expert Rev. Med. Devices 2019, 16, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Pokushalov, E.; Urban, L.; Taborsky, M.; Kuck, K.H.; Lebedev, D.; Rieger, G.; Pürerfellner, H. Performance of a new leadless implantable cardiac monitor in detecting and quantifying atrial fibrillation results of the XPECT Trial. Circ. Arrhythm Electrophysiol. 2010, 3, 141–147. [Google Scholar] [CrossRef] [Green Version]
- Di Girolamo, E.; Di Iorio, C.; Leonzio, L.; Sabatini, P.; Barsotti, A. Usefulness of a tilt training program for the prevention of refractory neurocardiogenic syncope in adolescents: A controlled study. Circulation 1999, 100, 1798–1801. [Google Scholar] [CrossRef] [Green Version]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raviele, A.; Gasparini, G.; Di Pede, F.; Delise, P.; Bonso, A.; Piccolo, E. Usefulness of head-up tilt test in evaluating patients with syncope of unknown origin and negative electrophysiologic study. Am. J. Cardiol. 1990, 65, 1322–1327. [Google Scholar] [CrossRef]
- Alboni, P.; Furlan, R. Vasovagal Syncop; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar] [CrossRef]
- Foglia-Manzillo, G.; Giada, F.; Gaggioli, G.; Bartoletti, A.; Lolli, G.; Dinelli, M.; Del Rosso, A.; Santarone, M.; Raviele, A.; Brignole, M. Efficacy of tilt training in the treatment of neurally mediated syncope. A randomized study. Europace 2004, 6, 199–204. [Google Scholar] [CrossRef]
- Rowe, P.C.; Calkins, H.; DeDusk, K.; McKenzie, R.; Anand, R.; Sharma, G.; Cuccherini, B.A.; Soto, N.; Hohman, P.; Snader, S. Fludrocortisone acetate to treat neurally mediated hypotension in chronic fatigue syndrome: A randomized controlled trial. J. Am. Med. Assoc. 2001, 285, 52–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ungar, A.; Galizia, G.; Morrione, A.; Mussi, C.; Noro, G.; Ghirelli, L.; Masotti, G.; Rengo, F.; Marchionni, N.; Abete, P. Two-year morbidity and mortality in elderly patients with syncope. Age Ageing 2011, 40, 696–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salim, M.A.; Di Sessa, T.G. Effectiveness of fludrocortisone and salt in preventing syncope recurrence in children: A double-blind, placebo-controlled, randomized trial. J. Am. Coll. Cardiol. 2005, 45, 484–488. [Google Scholar] [CrossRef] [Green Version]
- Ninni, S.; Kouakam, C.; Szurhaj, W.; Baille, G.; Klug, D.; Lacroix, D.; Derambure, P. Usefulness of head-up tilt test combined with video electroencephalogram to investigate recurrent unexplained atypical transient loss of consciousness. Arch. Cardiovasc. Dis. 2019, 112, 82–94. [Google Scholar] [CrossRef]
- Henderson, S.S.; Reed, M.J.; Newby, D.E.; Gray, A.J. 018 One-year prognosis after syncope and the failure of the ROSE decision instrument to predict 1-year adverse events. Emerg. Med. J. 2011, 28, A8–A9. [Google Scholar] [CrossRef]
- Giancaterino, S.; Lupercio, F.; Nishimura, M.; Hsu, J.C. Current and future use of insertable cardiac monitors. JACC Clin. Electrophysiol. 2018, 4, 1383–1396. [Google Scholar] [CrossRef]
- Li, Y.; Nantsupawat, T.; Olson, M.; Tholakanahalli, V.; Adabag, S.; Wang, Z.; Benditt, D.G.; Li, J.-M. A single center experience on the clinical utility evaluation of an insertable cardiac monitor. J. Electrocardiol. 2018, 51, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Burkowitz, J.; Merzenich, C.; Grassme, K.; Brüggenjürgen, B. Insertable cardiac monitors in the diagnosis of syncope and the detection of atrial fibrillation: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016, 23, 1261–1272. [Google Scholar] [CrossRef]
- Dalgaard, F.; Pallisgaard, J.L.; Numé, A.K.; Lindhardt, T.B.; Gislason, G.H.; Torp-Pedersen, C.; Ruwald, M.H. Rate or rhythm control in older atrial fibrillation patients: Risk of fall-related injuries and syncope. J. Am. Geriatr. Soc. 2019, 67, 2023–2030. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Jang, S.Y.; Yim, H.R.; On, Y.K.; Huh, J.; Shin, D.H.; Kim, J.H.; Kim, J.S. Gender difference in patients with recurrent neurally mediated syncope. Yonsei Med. J. 2010, 51, 499–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Negative (n = 29) | Positive (n = 72) | p Value | |
|---|---|---|---|
| Age | 51.8 ± 19.7 years old | 48.8 ± 21.6 years old | 0.51 |
| Male | 72.4% (21) | 63.9% (46) | 0.49 |
| Hypertension | 41.4% (12) | 25% (18) | 0.15 |
| RAS inhibitor | 27.6% (8) | 18.1% (13) | 0.49 |
| α blocker | 3.4% (1) | 4.2% (3) | 1 |
| β blocker | 13.8% (4) | 6.9% (5) | 0.27 |
| Diuretics | 13.8% (4) | 7.8% (2) | 0.06 |
| Calcium channel blocker | 20.7% (6) | 15.3% (11) | 0.56 |
| CVA | 3.4% (1) | 0% (0) | 0.29 |
| Diabetes mellitus | 13.8% (4) | 11.1% (8) | 0.74 |
| Atrial fibrillation | 6.8% (2) | 5.5% (4) | 1 |
| Ischemic heart disease | 13.8% (4) | 6.9% (5) | 0.27 |
| Non-ischemic heart disease | 6.8% (2) | 1.4% (1) | 0.2 |
| Ejection fraction of Left ventricle | 64.9 ± 10.7% | 68.8 ± 8.1% | 0.05 |
| History of Smoking | 51.7% (15) | 43.1% (31) | 0.31 |
| Epilepsy | 0% (0) | 1.4% (1) | 1 |
| HUTT | p Value | ||
|---|---|---|---|
| Negative (n = 29) | Positive (n = 71) | ||
| HR | 68 ± 14 | 62 ± 14 | 0.06 |
| PR | 163 ± 30.6 | 162 ± 23.8 | 0.88 |
| Axis | 65.2 ± 79.2 | 46.3 ± 39.0 | 0.1 |
| QRS | 113 ± 61.9 | 94.4 ± 19.3 | 0.03 |
| QTc | 430 ± 33.9 | 413 ± 26.9 | 0.01 |
| RBBB | 3 (10.3%) | 10 (14.1%) | 0.75 |
| LBBB | 2 (6.9%) | 0 (0%) | 0.08 |
| Brugada | 1 (3.4%) | 2 (2.8%) | - |
| DP | 0 (0%) | 1 (1.4%) | - |
| ERP | 3 (10.3%) | 13 (18.3%) | 0.547 |
| Positive HUTT | |||||
|---|---|---|---|---|---|
| Patient | Sex | Age | The Type of NMS | Days after HUT Test | The Details of Cardiac Event |
| 1 | Female | 70 | Vasopressor | 549 | Although no AF was detected prior to HUTT, the patient presented with syncope due to AF with rapid ventricular response. She underwent catheter ablation because her AF was refractory to antiarrhythmic medications. |
| 2 | Female | 73 | Vasopressor | 1111 | Although no AF was detected prior to HUTT, the patient presented with syncope due to AF with rapid ventricular response. She was told to undergo catheter ablation, however, she refused the procedure. |
| Negative HUT test | |||||
| 3 | Female | 75 | N/A | 23 | The patient presented with syncope and found to have 5 sec of long pause with faintness at the emergency room. The patient required pacemaker implantation due to sick sinus syndrome. |
| 4 | Male | 82 | N/A | 516 | The patient presented with bradycardia and syncope and was brought to the emergency room. He was found out to have advanced atrioventricular conduction block and required pacemaker implantation. |
| 5 | Male | 55 | N/A | 417 | The patient had history of old myocardial infarction (ejection fraction of 44%) of left anterior descending artery. He was found to be dead at home due to unknown etiology. After the investigation, we decided that the most likely cause of death was cardiogenic disease. |
| 6 | Female | 61 | N/A | 1 | The patient presented with syncope and the monitor electrocardiogram demonstrated unstable ventricular tachycardia with heart rate was 180 beats per minute. The syncope occurred on the day when we performed HUTT. She was diagnosed as cardiac sarcoidosis and required ICD placement. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayabe, K.; Komiyama, T.; Hasegawa, M.; Sakai, T.; Morise, M.; Sakama, S.; Yagishita, A.; Amino, M.; Ikari, Y.; Yoshioka, K. Clinical Significance of the Head-Up Tilt Test in Improving Prognosis in Patients with Possible Neurally Mediated Syncope. Biology 2021, 10, 919. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10090919
Ayabe K, Komiyama T, Hasegawa M, Sakai T, Morise M, Sakama S, Yagishita A, Amino M, Ikari Y, Yoshioka K. Clinical Significance of the Head-Up Tilt Test in Improving Prognosis in Patients with Possible Neurally Mediated Syncope. Biology. 2021; 10(9):919. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10090919
Chicago/Turabian StyleAyabe, Kengo, Tomoyoshi Komiyama, Misaki Hasegawa, Tetsuri Sakai, Masahiro Morise, Susumu Sakama, Atsuhiko Yagishita, Mari Amino, Yuji Ikari, and Koichiro Yoshioka. 2021. "Clinical Significance of the Head-Up Tilt Test in Improving Prognosis in Patients with Possible Neurally Mediated Syncope" Biology 10, no. 9: 919. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10090919