1. Introduction
Breast cancer is the most common cancer in women worldwide. In Greece, it is estimated that one in twelve women will be affected by breast cancer during her lifespan. Almost 4500 women are diagnosed with breast cancer every year [
1]. It is the leading cancer type in women in all European countries [
2].
Quality of life (QOL) is defined as “an individual’s perception of his/her position in life in the context of the culture and value systems in which he/she lives and in relation to his/her goals, expectations, standards, and concerns” by the World Health Organization Quality of Life Group. This definition considers that quality of life is a subjective concept and depends on an individual’s judgment [
3].
Breast cancer and its treatment impacts patients’ quality of life [
4]. Quality of life in breast cancer patients has received increasing attention due to a rising number of new cases, an improved survival rate, and the vital role of the woman in the family [
5].
Several studies have examined the determinants of quality of life in breast cancer survivors and in patients after completion of therapy [
6,
7]. One study reported that five years after breast cancer diagnosis, the major determinants for quality of life are body mass index, relapse, socioeconomic deprivation, and comorbidities [
6]. Specifically, it was found that body mass index, relapse, and socioeconomic deprivation were determinants of quality of life in younger women; in older women, comorbidities and socioeconomic deprivation were predictors of quality of life [
6].
One study examined the impact of socioeconomic and clinical characteristics on quality of life in 188 breast cancer survivors five years after diagnosis. Quality of life was assessed with the Short Form Health Survey (SF-12), EORTCQLQ-C30, and EORTCQLQ-BR23 questionnaires. It was found that only age at diagnosis and comorbidities were determinants of quality of life [
8]. In a more recent study it was reported that sociodemographic factors (level of education, marital status), age, comorbidities (e.g., diabetes, high cholesterol), stage of cancer, surgery, radiotherapy or hormone therapy do not have a significant effect on quality of life. The study investigated 77 patients and used the SF-36 scale [
9]. Furthermore, a study of 544 female breast cancer patients revealed that demographic and clinical factors such as age, education, employment, marital status, income, chemotherapy, duration since treatment, and recurrence status had no impact on quality of life. EORTC QLQ-C30 and EORTC QLQ-BR23 was used for evaluating QOL [
10]. The results of the above studies are conflicting, so there is a need for further research in order to investigate if demographic characteristics such as age, marital status, educational status, and occupational status influence quality of life in Greek breast cancer patients six months after the end of chemotherapy.
In addition, there are some studies that examine the impact of type of treatment on quality of life of breast cancer survivors [
7,
10,
11]. It was reported that the type of breast cancer surgery did not influence any aspect of quality of life, only body image [
10]. Chemotherapy has profound effects on quality of life (Yeo et al., 2018) regardless of whether it is administered in low or high doses [
12]. Menopausal symptoms, whether they are due to natural menopause or due to cancer treatment, also affect quality of life [
11]. Premenopausal breast cancer survivors have endocrine changes that affect quality of life. Women who become menopausal due to treatment have more severe menopausal symptoms compared to those who have a natural transition [
7]. It was found that hormone therapy had no significant impacts on quality of life [
9], but on the other hand causes some physical symptoms in breast cancer patients [
13].
Anemia is a common adverse effect in cancer patients undergoing chemotherapy [
14]. According to Schrijvers et al. (2010), anemia is defined as “a reduction of the hemoglobin (Hb) concentration, red blood cell count or packed cell volume below normal levels. Mild anemia is defined as an Hb ≤ 11 g/dL and Hb ≥ 10 g/dL, moderate anemia as Hb of ≤9.9 and ≥8 g/dL and severe anemia as an Hb of <8 g/dL” [
15]. It is well documented that anemia induced by chemotherapy is associated with impaired quality of life in cancer patients [
16]. Moreover, chemotherapy-induced neutropenia is a frequent complication in cancer patients because of myelosuppression [
17]. This is associated with important effects on quality of life, because of hospitalization for febrile neutropenia and fear of hospitalization [
18] Nowadays, myelotoxic regimes remain the current standard in care of breast cancer patients [
17]. There is evidence that anemia and neutropenia are toxicities in breast cancer patients undergoing chemotherapy and most commonly appear 7–14 days after the completion of chemotherapy [
19]. There is no evidence for a relationship between hemoglobin and neutrophil levels and quality of life in breast cancer survivors after the completion of chemotherapy.
The aforementioned studies primarily investigated factors or determinants influencing quality of life and used several questionnaires for assessing quality of life, such as SF-36, EORTC-QLQ-C30, EORTC-QLQ-BR23, and FACT-B.
Undoubtedly, there is a growing interest in quality of life of breast cancer survivors after the acute phase of treatment [
7,
20]. In Greece, to the best of our knowledge, there are a limited number of studies assessing quality of life beyond chemotherapy in breast cancer patients (e.g., [
21]), which is what stimulated this researcher’s interest in further investigation of this phenomenon.
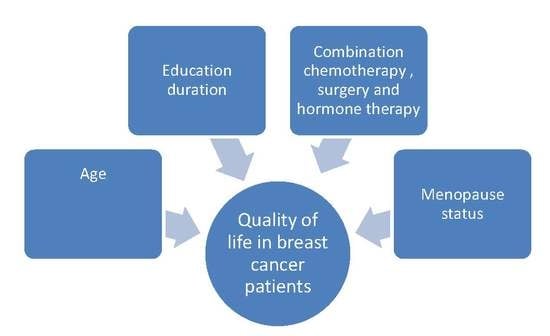
The purpose of the present study was to assess breast cancer patients’ quality of life six months after the completion of adjuvant chemotherapy, and to investigate factors affecting this. Specifically, we aimed to assess the following research questions:
Does age affect the domains of quality of life in breast cancer patients?
Do different sociodemographic factors (educational status, occupational status, marital status) affect quality of life in breast cancer patients?
Do treatment type, white blood cell count, hematocrit, hemoglobin, or menopausal status influence the domains of quality of life in breast cancer patients?
4. Discussion
This study assessed the quality of life in Greek breast cancer patients and the factors (clinical, demographics) influencing this, six months after they completed their chemotherapy. It contributes to the growing body of evidence regarding quality of life in breast cancer survivors and provides important information for Greek oncology nurses, because describing this phenomenon is a significant step toward appropriate interventions. In this study we found that age, menopausal status, and hormone therapy influenced certain domains of quality of life in breast cancer patients.
Breast cancer patients in this study sample experienced low levels of physical functioning, mental health, emotional role, and vitality. This is consistent with the results of other studies [
21,
26].
We examined the associations between demographic and clinical characteristics and we found that there is statistically significant difference between age and menopausal status, as well as between age and work status; the older women were post-menopausal and retired. This is an expected outcome because older women tended to be retired. Also, we found that there was an association between type of surgery and menopausal status. To the best of our knowledge, the type of hormonal therapy after the surgery was associated with menopausal status but there is not clear evidence that the type of breast surgery affected menopausal status [
27]. This is influenced by the kind of therapy after the surgery (chemotherapy, radiation therapy, hormone therapy). Hence, there is a need for further research in order to draw a safe conclusion.
The influence of various demographic characteristics in breast cancer survivors’ quality of life was studied previously and was also investigated in the present study. We found that age affected one subscale of quality of life, physical role. This is inconsistent with the findings of other studies [
9,
10], and is partially consistent with one study which reported that only age at diagnosis was a determinant of the quality of life [
8]. This discrepancy across the literature might be explained by the differences in the sample size or different questionnaires that were used across the studies. We also find a marginal effect of age on physical role; which younger participants might have had a better quality of life in physical role than the older women (>60 years old). Although this is an expected outcome, in previous studies it was considered that early age (<50 years) was a predictive factor of a worse quality of life [
9,
28]. There is a need for further research in order to clarify the influence of age in quality of life of breast cancer survivors, especially in Greek patients.
We found that educational status has no effect on quality of life. This finding is consistent with previous studies [
9,
10]. A marginal effect of educational status on the physical role and general health subscales was found. A possible explanation for these results is the small sample size in educational status groups. Also, we found that work did not influence any domain of quality of life. This is in line with a previous study which reported that employment had no impact on quality of life [
10].
It is worthwhile to note that we did not find any influence of demographic on the mental health domain of quality of life. This is in accordance with the findings of other studies [
9,
20]. There is a need for further research in Greece to clarify if the aforementioned factors influence mental health; more specific questionnaires should be used.
The present study also examined whether clinical characteristics influence quality of life and its domains. Menopausal status has a significant effect on physical role. This association has also been reported in China and in Australia in breast cancer survivors [
11,
29]. Also, we found women experiencing menopausal symptoms due to treatment had a higher quality of life than post-menopausal women. A possible explanation for this finding is the fact that women in this sample were younger and they experienced menopausal symptoms after initial treatment [
30] so, the menopausal status per se may not affect their quality of life in a great manner. As is reported above, we found an association between age and menopausal status and this finding strengthens our explanation. Moreover, we found another marginal but not significant effect of menopausal status on emotional role, in which women who were menopausal due to treatment had better emotional role scores than the others. This might be explained their young age. In a previous systematic review, it was considered that younger age was associated with depression [
28]. Future studies could test whether symptoms of depression mediate the association between age and quality of life in Greek breast cancer patients. Furthermore, we found an effect of treatment type on the quality of life subscales. Specifically, we found that hormone therapy on top of surgery and chemotherapy seemed to be associated with better quality of life regarding bodily pain and vitality. This finding is inconsistent with the findings of another study [
9]. Seventy breast cancer survivors were examined, but they did not refer many details of duration of survival after their initial treatment. Also, they used the same scale as the present study but they did not refer specifically to influences of hormone therapy and other types of therapy on quality of life subscales. Also, this finding is partially consistent with the findings of Mortada et al. [
13] who reported that the hormonal therapy group had higher scores in all domains of quality of life (they used EORTC-QLQ30 and QLQ-BC23). This conflicting finding might be explained by the fact that the studies used different scales and had different sample sizes. Moreover, in our study there was a shorter period between the initial type of treatment (surgery, chemotherapy, and hormonal therapy) and the interview, so the participants would not have noticed as many disruptions in all domains of their quality of life. It is noteworthy that the marginal effect of hormone therapy on social function is explained by the previous finding. We can hypothesize that these patients had no bodily pain and had better vitality so it was easier for them to have a better social life.
No significant association was found between surgery type and quality of life subscales. Similarly, Dadjoul et al. [
9] did not find any influence of type of surgery on overall quality of life. Another study in long-term breast cancer survivors (5 years) reported that surgical modality has no significant impact on any quality of life domains except body image [
10]. Once again, it is worth mentioning the marginally higher general health scores in patients with lumpectomy and the non-significant higher scores in some subscales (physical role, bodily pain, social functioning, and mental health). This result might be explained by the small sample size (in the present study a few patients were undergoing mastectomy). Further study is needed to make clear the effect of type surgery in breast cancer patients in Greece.
Regarding the influence of hematocrit and hemoglobin in quality of life, we showed that there is not a statistically significant difference. This is an expected outcome, because our patients did not experience severe anemia so it did not affect their quality of life. On the other hand, they had finished their chemotherapy less than six months before the study, and as we know anemia is a serious adverse effect during chemotherapy [
16]. To the best of our knowledge this is the first study that examines the association between anemia and quality of life in breast cancer survivors. Therefore, it is not possible for us to compare these results. Further study is needed with larger sample sizes in order to ascertain if there is association between hematocrit and hemoglobin levels on quality of life in breast cancer survivors in Greece and elsewhere.
We also found a marginally higher effect of hematocrit in emotional role and social functioning where participants with low hematocrit levels had lower scores than those with normal levels. This is explained by the fact that low levels of hematocrit influence patients’ daily activities and impact their quality of life [
16]. Future studies could test this hypothesis by examining the influence of low levels of hematocrit on different domains of quality of life.
Our study showed that there was no impact of white cell count levels on domains of quality of life. This was also an expected outcome because our sample had no cases of severe neutropenia. There is a need for further research to clarify if white cell count levels influence quality of life.
Analysis yielded an interesting result. Breast cancer survivors who received hormone therapy in addition to surgery and chemotherapy had higher scores in the bodily pain domain of quality of life than others who did not receive this type of therapy. This is not consistent with the finding of one study that examined 186 women who took hormonal therapy after surgery and found that women taking hormonal therapy had more severe joint or bone pain than women not taking hormonal therapy [
31]. This discrepancy might be attributable to the different sample size, different culture, and different methodologies used by the two studies. Undoubtedly, there is a need for further research in order to discriminate the influences of hormonal therapy and previous therapy on breast cancer survivors’ quality of life.
Another interesting result is the interaction of hormone therapy and other treatment types. Women who had received hormone therapy in addition to surgery and chemotherapy had better quality of life regarding bodily pain. Although hormone therapy causes joint pain, this result is inconsistent with the known results [
31]. This discrepancy might be explained by the small size of the present study.
Finally, we found that the effect of type of treatment on vitality was significant. It should be pointed out that vitality is linked to fatigue. Fatigue is a common and disabling symptom in cancer patients and in patients’ survivorship. It can be measured by the vitality subscale of SF-36 questionnaire [
32]. Therefore the above result is an expected outcome because fatigue is a symptom associated with chemotherapy, radiation therapy, surgery, and hormonal therapy and often persists after the completion of therapy [
31,
33].
Limitations of the Study
This study has some limitations. It was conducted in one hospital located in a major Greek city and the sample was relatively small, so the results cannot be generalized with respect to the entire Greek population. Another limitation was the cross-sectional nature of the present study; we could not assess the trajectory of quality of life at the end the chemotherapy, six months on, one year on, or five years on. A future study in Greece employing a longitudinal design could provide more clear conclusions. Although we studied the influence of demographic and clinical characteristics, the present study did not investigate some other important clinical characteristics such as type of chemotherapy regimen, its duration, etc. However, the results provide valuable information for the issue at hand, and illustrate the great need for further longitudinal studies in order to draw reliable conclusions. Despite these limitations our study has one significant strength: To our knowledge, this is the first population-based study to investigate factors influencing quality of life in breast cancer survivors in Greece, where culture and lifestyle are significantly different from those in western populations.