Herpes Simplex Virus Proctitis Masquerading as Rectal Cancer
Abstract
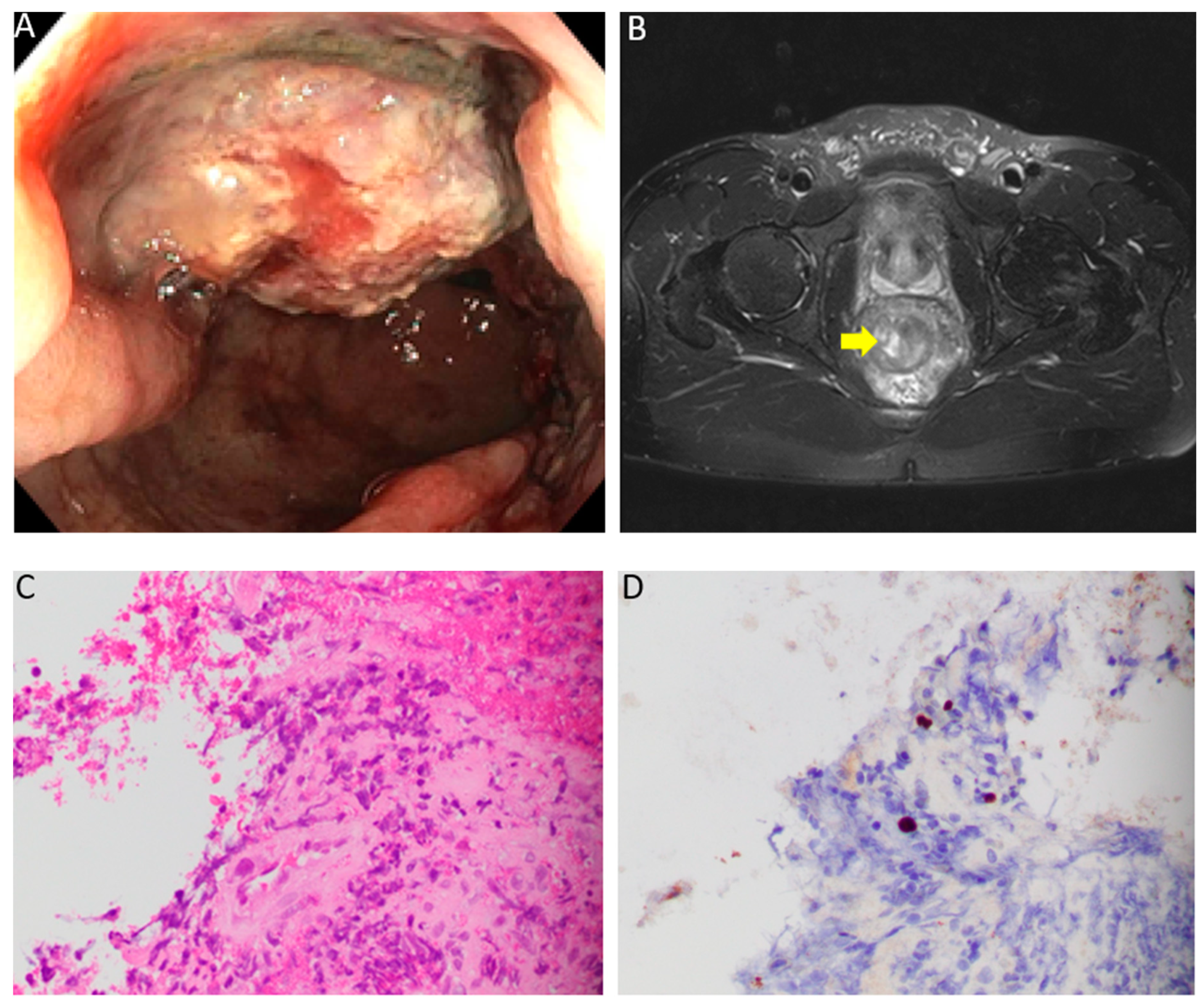
:1. Case Description
2. Discussion
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alfa-Wali, M.; Muktar, S.; Pissas, D.; Slater, C. Unusual case of a rectal tumour. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Serigado, J.; Lewis, E.; Kim, G. Rectal bleeding caused by a syphilitic inflammatory mass. BMJ Case Rep. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Vaidya, G.; Kalakonda, A.; Manocha, D.; Rawlins, S. Cytomegalovirus Colitis Mimicking Rectal Carcinoma in a Young Immunocompetent Patient. ACG Case Rep. J. 2015, 2, 165–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burkes, R.L.; Meyer, P.R.; Gill, P.S.; Parker, J.W.; Rasheed, S.; Levine, A.M. Rectal lymphoma in homosexual men. Arch. Intern. Med. 1986, 146, 913–915. [Google Scholar] [CrossRef] [PubMed]
- Coghill, A.E.; Shiels, M.S.; Rycroft, R.K.; Copeland, G.; Finch, J.L.; Hakenewerth, A.M.; Pawlish, K.S.; Engels, E.A. Rectal squamous cell carcinoma in immunosuppressed populations: Is this a distinct entity from anal cancer? AIDS 2016, 30, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Lamb, C.A.; Lamb, E.I.; Mansfield, J.C.; Sankar, K.N. Sexually transmitted infections manifesting as proctitis. Frontline Gastroenterol. 2013, 4, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Bissessor, M.; Fairley, C.K.; Read, T.; Denham, I.; Bradshaw, C.; Chen, M. The etiology of infectious proctitis in men who have sex with men differs according to HIV status. Sex Transm. Dis. 2013, 40, 768–770. [Google Scholar] [CrossRef] [PubMed]
- Corey, L.; Spear, P.G. Infections with herpes simplex viruses (1). N. Engl. J. Med. 1986, 314, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.D.; Smith, I.W.; Elton, R.A. The epidemiology of herpes simplex types 1 and 2 infection of the genital tract in Edinburgh 1978-1991. Genitourin Med. 1993, 69, 381–383. [Google Scholar] [CrossRef] [PubMed]
- Jin, F.; Prestage, G.P.; Mao, L.; Kippax, S.C.; Pell, C.M.; Donovan, B.; Templeton, D.J.; Taylor, J.; Mindel, A.; Kaldor, J.M.; et al. Transmission of herpes simplex virus types 1 and 2 in a prospective cohort of HIV-negative gay men: the health in men study. J. Infect. Dis. 2006, 194, 561–570. [Google Scholar] [CrossRef]
- Goodell, S.E.; Quinn, T.C.; Mkrtichian, E.; Schuffler, M.D.; Holmes, K.K.; Corey, L. Herpes simplex virus proctitis in homosexual men. Clinical, sigmoidoscopic, and histopathological features. N. Engl. J. Med. 1983, 308, 868–871. [Google Scholar] [CrossRef] [PubMed]
- Eyzaguirre, E.; Haque, A.K. Application of immunohistochemistry to infections. Arch. Pathol. Lab. Med. 2008, 132, 424–431. [Google Scholar] [PubMed]
- Gonzales Zamora, J.A.; Espinoza, L.A. Verrucous herpes of the finger in a patient with HIV-1 infection. Infection 2018, 46, 285–286. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayoade, F.; Gonzales Zamora, J.A.; Tjendra, Y. Herpes Simplex Virus Proctitis Masquerading as Rectal Cancer. Diseases 2019, 7, 36. https://0-doi-org.brum.beds.ac.uk/10.3390/diseases7020036
Ayoade F, Gonzales Zamora JA, Tjendra Y. Herpes Simplex Virus Proctitis Masquerading as Rectal Cancer. Diseases. 2019; 7(2):36. https://0-doi-org.brum.beds.ac.uk/10.3390/diseases7020036
Chicago/Turabian StyleAyoade, Folusakin, Jose Armando Gonzales Zamora, and Youley Tjendra. 2019. "Herpes Simplex Virus Proctitis Masquerading as Rectal Cancer" Diseases 7, no. 2: 36. https://0-doi-org.brum.beds.ac.uk/10.3390/diseases7020036





