Cut-Off Points of Visceral Adipose Tissue Associated with Metabolic Syndrome in Military Men
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collect
2.3. Blood Collection and Biochemical Analyzes
2.4. Blood Pressure Assessment
2.5. Anthropometric Evaluation
2.6. DXA Body Composition
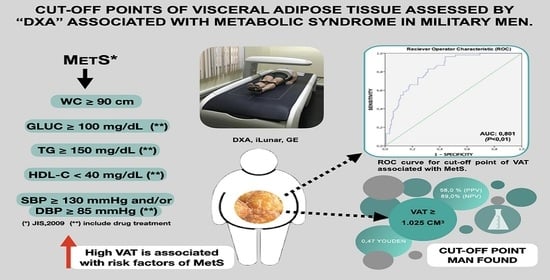
2.7. MetS Diagnosis
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blüher, M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [Green Version]
- McCracken, E.; Monaghan, M.; Sreenivasan, S. Pathophysiology of the Metabolic Syndrome. Clin. Dermatol. 2018, 36, 14–20. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [Green Version]
- de Sá Rego Fortes, M.; da Rosa, S.E.; Coutinho, W.; Neves, E.B. Epidemiological Study of Metabolic Syndrome in Brazilian Soldiers. Arch. Endocrinol. Metab. 2019, 63, 345–350. [Google Scholar] [CrossRef]
- Jemtel, T.H.L.; Samson, R.; Milligan, G.; Jaiswal, A.; Oparil, S. Visceral Adipose Tissue Accumulation and Residual Cardiovascular Risk. Curr. Hypertens. Rep. 2018, 20, 77. [Google Scholar] [CrossRef] [PubMed]
- Sam, S. Differential Effect of Subcutaneous Abdominal and Visceral Adipose Tissue on Cardiometabolic Risk. Horm. Mol. Biol. Clin. Investig. 2018, 33, 438–448. [Google Scholar] [CrossRef] [PubMed]
- Sasai, H.; Brychta, R.J.; Wood, R.P.; Rothney, M.P.; Zhao, X.; Skarulis, M.C.; Chen, K.Y. Does Visceral Fat Estimated by Dual-Energy X-ray Absorptiometry Independently Predict Cardiometabolic Risks in Adults? J. Diabetes Sci. Technol. 2015, 9, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Madden, A.M.; Smith, S. Body Composition and Morphological Assessment of Nutritional Status in Adults: A Review of Anthropometric Variables. J. Hum. Nutr. Diet. 2016, 29, 7–25. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Berg, E.; Cheng, X.; Shen, W. How to Best Assess Abdominal Obesity. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 360. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.L.; Wilson, K.E.; Heymsfield, S.B. Dual Energy X-ray Absorptiometry Body Composition Reference Values from NHANES. PLoS ONE 2009, 4, e7038. [Google Scholar] [CrossRef] [Green Version]
- Ofenheimer, A.; Breyer-Kohansal, R.; Hartl, S.; Burghuber, O.C.; Krach, F.; Schrott, A.; Wouters, E.F.M.; Franssen, F.M.E.; Breyer, M.-K. Reference Values of Body Composition Parameters and Visceral Adipose Tissue (VAT) by DXA in Adults Aged 18–81 Years—Results from the LEAD Cohort. Eur. J. Clin. Nutr. 2020, 74, 1181–1191. [Google Scholar] [CrossRef]
- Lang, P.-O.; Trivalle, C.; Vogel, T.; Proust, J.; Papazyan, J.-P.; Dramé, M. Determination of Cutoff Values for DEXA-Based Body Composition Measurements for Determining Metabolic and Cardiovascular Health. BioResearch Open Access 2015, 4, 16–25. [Google Scholar] [CrossRef]
- Kaul, S.; Rothney, M.P.; Peters, D.M.; Wacker, W.K.; Davis, C.E.; Shapiro, M.D.; Ergun, D.L. Dual-Energy X-ray Absorptiometry for Quantification of Visceral Fat. Obesity 2012, 20, 1313–1318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rothney, M.P.; Catapano, A.L.; Xia, J.; Wacker, W.K.; Tidone, C.; Grigore, L.; Xia, Y.; Ergun, D.L. Abdominal Visceral Fat Measurement Using Dual-Energy X-ray: Association with Cardiometabolic Risk Factors. Obesity 2013, 21, 1798–1802. [Google Scholar] [CrossRef] [PubMed]
- Ergun, D.L.; Rothney, M.P.; Oates, M.K.; Xia, Y.; Wacker, W.K.; Binkley, N.C. Visceral Adipose Tissue Quantification Using Lunar Prodigy. J. Clin. Densitom. 2013, 16, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, B.J.; Penninx, B.W.J.H.; Ryan, A.S.; Berman, D.M.; Lynch, N.A.; Dennis, K.E. Visceral Adipose Tissue Cutoffs Associated With Metabolic Risk Factors for Coronary Heart Disease in Women. Diabetes Care 2003, 26, 1413–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bi, X.; Seabolt, L.; Shibao, C.; Buchowski, M.; Kang, H.; Keil, C.D.; Tyree, R.; Silver, H.J. DXA-Measured Visceral Adipose Tissue Predicts Impaired Glucose Tolerance and Metabolic Syndrome in Obese Caucasian and African-American Women. Eur. J. Clin. Nutr. 2015, 69, 329–336. [Google Scholar] [CrossRef] [Green Version]
- Miazgowski, T.; Kucharski, R.; Sołtysiak, M.; Taszarek, A.; Miazgowski, B.; Widecka, K. Visceral Fat Reference Values Derived from Healthy European Men and Women Aged 20–30 Years Using GE Healthcare Dual-Energy X-ray Absorptiometry. PLoS ONE 2017, 12, e0180614. [Google Scholar] [CrossRef] [Green Version]
- Andriolo, A.; Faulhaber, A.C.L.; Junior, A.P.; Martins, A.R.; de Oliveira Machado, A.M.; Ballarati, C.A.F.; Soares, C.A.S.; dos Ssantos Ferreira, C.E.; Granato, C.F.H.; de Oliveira Galoro, C.A.; et al. Recomendações Da Sociedade Brasileira de Patologia Clínica/Medicina Laboratorial (SBPC/ML): Colet e Preparo Da Amostra Biológica, 1st ed.; Manole Ltda: Rio de Janeiro, Brazil, 2014; Volume 1. [Google Scholar]
- de Vigilância Sanitária, A.N. Resolução RDC no 306, de 07 de Dezembro de Dispõe Sobre o Regulamento Técnico para o Gerenciamento de Resíduos de Serviços de Saúde 2004. Available online: https://www.saude.mg.gov.br/images/documentos/res_306.pdf (accessed on 8 July 2021).
- Malachias, M.; Souza, W.; Plavnik, F.; Rodrigues, C.; Brandão, A.; Neves, M.; Bortolotto, L.; Franco, R.; Figueiredo, C.; Jardim, P.; et al. Capítulo 3—Avaliação Clínica e Complementar. Arq. Bras. Cardiol. 2016, 107, 1–83. [Google Scholar] [CrossRef]
- Filho, J.F. A Prática Da Avaliação Física: Testes, Medidas, Avaliação Física Em Escolares, Atletas e Academias de Ginástica, 3rd ed.; SHAPE: Rio de Janeiro, Brazil, 2003; Volume 1. [Google Scholar]
- dos Santos Ribeiro, G.; Fragoso, E.B.; Nunes, R.D.; Lopes, A.L. Erro Técnico de Medida Em Antropometria: Análise de Precisão e Exatidão Em Diferentes Plicômetros. Rev. Educ. Física J. Phys. Educ. 2019, 88. [Google Scholar] [CrossRef]
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. Appl. Stat. Methods 2009, 8, 597–599. [Google Scholar] [CrossRef]
- Li, C.; Chen, J.; Qin, G. Partial Youden Index and Its Inferences. J. Biopharm. Stat. 2019, 29, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Obuchowski, N.A.; Bullen, J.A. Receiver Operating Characteristic (ROC) Curves: Review of Methods with Applications in Diagnostic Medicine. Phys. Med. Biol. 2018, 63, 07TR01. [Google Scholar] [CrossRef]
- da Rosa, S.E.; Lippert, M.A.; Marson, R.A.; de Sá Rego Fortes, M.; Rodrigues, L.C.; Filho, J.F. Physical Performance, Body Composition And Metabolic Syndrome In Military Personnel From The Brazilian Army. Rev. Bras. Med. Esporte 2018, 24, 422–425. [Google Scholar] [CrossRef]
- da Costa, F.F.; Montenegro, V.B.; Lopes, T.J.A.; Costa, E.C. Combinação de Fatores de Risco Relacionados à Síndrome Metabólica Em Militares Da Marinha Do Brasil. Arq. Bras. Cardiol. 2011, 97, 485–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rostami, H.; Tavakoli, H.R.; Rahimi, M.H.; Mohammadi, M. Metabolic Syndrome Prevalence among Armed Forces Personnel (Military Personnel and Police Officers): A Systematic Review and Meta-Analysis. Mil. Med. 2019, 184, e417–e425. [Google Scholar] [CrossRef] [Green Version]
- Gámez, A.A.; Sotolongo, O.G.; Cuza, E.R.; Helps, A.B.; Vaillant, R.A. El Síndrome Metabólico Como Factor de Riesgo Para La Disfunción Endotelial. Rev. Cuba. Med. Mil. 2007, 36. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0138-65572007000100002 (accessed on 8 July 2021).
- Saboya, P.P.; Bodanese, L.C.; Zimmermann, P.R.; da Silva Gustavo, A.; Assumpção, C.M.; Londero, F. Metabolic Syndrome and Quality of Life: A Systematic Review. Rev. Lat. Am. Enfermagem 2016, 24. [Google Scholar] [CrossRef] [Green Version]
- da Rosa, S.E.; Filho, J.F.; de Sá Rego Fortes, M.; Chain, A.C.; Martinez, E.C. Serum Biochemical Markers and Anthropometric Measurements in the Brazilian Army Militaries Selected for the United Nations’ Peacekeeping Mission in Haiti. Glob. J. Res. Anal. 2015, 4, 38–40. [Google Scholar]
- Bosch, T.A.; Dengel, D.R.; Kelly, A.S.; Sinaiko, A.R.; Moran, A.; Steinberger, J. Visceral Adipose Tissue Measured by DXA Correlates with Measurement by CT and Is Associated with Cardiometabolic Risk Factors in Children. Pediatr. Obes. 2015, 10, 172–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, T.L. Practical and technical advantages of DXA visceral fat assessment compared with computed tomography. Age 2010, 36, 50. [Google Scholar]


| Parameters (n) | WMetSFR (196) | MetSFR (74) | p Value * | Effect Size (d) | 95%CI | ICC | CV | α |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||||||
| Age | 36.0 ± 6.3 | 38.0 ± 7.3 | 0.026 | 0.30 | 0.04–0.57 | 0.421 | 1.71 | 0.448 |
| Height (cm) | 177.5 ± 6.0 | 177.5 ± 6.2 | 0.829 | 0.02 | 0.23–0.29 | −0.061 | 1.61 | −0.060 |
| BM (kg) | 80.9 ± 12.3 | 94.5 ± 12.3 | 0.000 | 0.98 | 0.70–1.26 | 0.084 | 2.18 | 0.108 |
| BMI | 25.7 ± 3.6 | 29.8 ± 6.2 | 0.000 | 1.03 | 0.76–1.32 | 0.150 | 6.61 | 0.197 |
| LM (kg) | 58.8 ± 5.9 | 62.5 ± 6.5 | 0.000 | 0.60 | 0.33–0.88 | −0.038 | 0.36 | −0.041 |
| FM (kg) | 20.8 ± 8.4 | 28.9 ± 8.7 | 0.000 | 0.95 | 0.67–1.23 | 0.024 | 10.28 | 0.030 |
| FMI (kg/m2) | 6.6 ± 2.6 | 9.2 ± 2.7 | 0.000 | 0.97 | 0.69–1.25 | 0.044 | 13.30 | 0.057 |
| %BF-DXA | 24.5 ± 6.7 | 30.1 ± 5.7 | 0.000 | 0.87 | 0.59–1.15 | 0.029 | 8.41 | 0.037 |
| VAT (cm3) | 806.4 ± 597.6 | 1550.6 ± 716.8 | 0.000 | 1.18 | 0.89–1.46 | −0.189 | 27.87 | −0.296 |
| VAT (g) | 761.2 ± 563.9 | 1462.8 ± 676.2 | 0.000 | 1.18 | 0.89–1.46 | −0.189 | 27.85 | −0.296 |
| WC (cm) | 87.1 ± 8.6 | 96.3 ± 7.6 | 0.000 | 1.14 | 0.85–1.42 | −0.087 | 1.98 | 0.121 |
| Triglycerides (mmol/L) | 83.4 ± 38.0 | 117.8 ± 55.7 | 0.000 | 0.78 | 0.51–1.06 | 0.011 | 1.71 | 0.014 |
| Glucose (mmol/L) | 94.5 ± 8.6 | 100.7 ± 10.0 | 0.000 | 0.58 | 0.41–0.96 | −0.361 | 0.82 | −0.367 |
| HDL-c (mmol/L) | 54.4 ± 16.0 | 46.9 ± 10.8 | 0.000 | 0.52 | 0.24–0.79 | 0.087 | 8.08 | 0.101 |
| SBP (mmHg) | 117.1 ± 9.7 | 130.0 ± 12.8 | 0.000 | 1.21 | 0.92–1.49 | −0.319 | 1.56 | −0.628 |
| DBP (mmHg) | 80.0 ± 6.2 | 90.0 ± 11.3 | 0.000 | 1.28 | 0.98–1.56 | −0.007 | 4.80 | −0.010 |
| Variables | VAT-DXA | |||
|---|---|---|---|---|
| WMetSRF | MetSRF | |||
| Independent Variables | r * | p * | r * | p * |
| Age | 0.280 | 0.000 | 0.363 | 0.000 |
| Height (cm) | 0.071 | 0.323 | 0.124 | 0.291 |
| BM (kg) | 0.775 | 0.000 | 0.548 | 0.000 |
| BMI | 0.800 | 0.000 | 0.644 | 0.000 |
| FMI (kg/m2) | 0.872 | 0.000 | 0.747 | 0.000 |
| LM (kg) | 0.331 | 0.000 | 0.056 | 0.637 |
| FM (kg) | 0.880 | 0.000 | 0.722 | 0.000 |
| %BF-DXA | 0.825 | 0.000 | 0.722 | 0.000 |
| WC (cm) | 0.885 | 0.000 | 0.836 | 0.000 |
| Triglycerides (mmol/L) | 0.260 | 0.000 | 0.164 | 0.163 |
| Glucose (mmol/L) | 0.216 | 0.002 | 0.343 | 0.003 |
| HDL-c (mmol/L) | −0.175 | 0.014 | −0.138 | 0.241 |
| SBP (mmHg) | 0.033 | 0.643 | 0.019 | 0.874 |
| DBP (mmHg) | 0.119 | 0.098 | 0.127 | 0.282 |
| VAT Cutoff (cm3) | Sensitivity (%) | Specificity (%) | Youden Index ** | PPV (%) | NPV (%) |
|---|---|---|---|---|---|
| 48.0 | 100.0 | 0.0 | 0.00 | 27.4 | 0.0 |
| 568.5 | 95.9 | 44.9 | 0.41 | 39.7 | 3.3 |
| 811.5 | 85.1 | 57.7 | 0.43 | 43.3 | 91.1 |
| 1025.0 * | 77.0 | 69.9 | 0.47 | 49.1 | 89.0 |
| 1417.0 | 56.8 | 83.2 | 0.40 | 56.0 | 83.6 |
| 2062.5 | 23.0 | 95.9 | 0.35 | 69.2 | 77.0 |
| 4201.0 | 0.0 | 100.0 | 0.00 | 27.2 | 100.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Rosa, S.E.; Costa, A.C.; Fortes, M.S.R.; Marson, R.A.; Neves, E.B.; Rodrigues, L.C.; Ferreira, P.F.; Filho, J.F. Cut-Off Points of Visceral Adipose Tissue Associated with Metabolic Syndrome in Military Men. Healthcare 2021, 9, 886. https://0-doi-org.brum.beds.ac.uk/10.3390/healthcare9070886
da Rosa SE, Costa AC, Fortes MSR, Marson RA, Neves EB, Rodrigues LC, Ferreira PF, Filho JF. Cut-Off Points of Visceral Adipose Tissue Associated with Metabolic Syndrome in Military Men. Healthcare. 2021; 9(7):886. https://0-doi-org.brum.beds.ac.uk/10.3390/healthcare9070886
Chicago/Turabian Styleda Rosa, Samir Ezequiel, Amina Chain Costa, Marcos S. R. Fortes, Runer Augusto Marson, Eduardo Borba Neves, Laercio Camilo Rodrigues, Paula Fernandez Ferreira, and Jose Fernandes Filho. 2021. "Cut-Off Points of Visceral Adipose Tissue Associated with Metabolic Syndrome in Military Men" Healthcare 9, no. 7: 886. https://0-doi-org.brum.beds.ac.uk/10.3390/healthcare9070886