Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview
Abstract
:1. Introduction
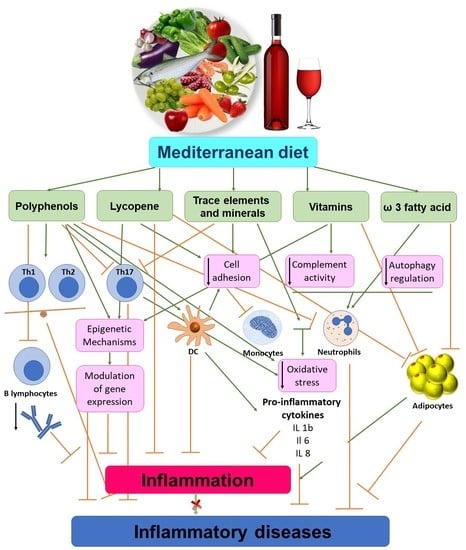
2. Mediterranean Diet and Inflammation
3. Role of Mediterranean Diet Components on Inflammatory Response
3.1. Trace Elements and Minerals Contribution
3.2. Salt Intake
3.3. The Olive Oil Treasure
3.4. Polyphenols and Neutrophil Activity
3.5. Lycopene’s Value
4. Mediterranean Diet’s Impact on Epigenetic Mechanisms
5. Chronic Diseases and Mediterranean Diet Interventions
5.1. Autoimmune Diseases
5.2. Hyperuricaemia
5.3. Cardiovascular Disease
5.4. Allergic Diseases and Asthma
5.5. Inflammatory Bowel Diseases
6. Acute Inflammation-Sepsis
7. Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| MD | Mediterranean diet |
| WD | Western diet |
| CVD | Cardiovascular Diseases |
| T2DM | Type 2 Diabetes Mellitus |
References
- Grammaticos, P.C.; Diamantis, A. Useful known and unknown views of the father of modern medicine, Hippocrates and his teacher Democritus. Hell. J. Nucl. Med. 2008, 11, 2–4. [Google Scholar] [PubMed]
- Roberts, C.K.; Barnard, R.J. Effects of exercise and diet on chronic disease. J. Appl. Physiol. 2005, 98, 3–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galbete, C.; Kröger, J.; Jannasch, F.; Iqbal, K.; Schwingshackl, L.; Schwedhelm, C.; Weikert, C.; Boeing, H.; Schulze, M.B. Nordic diet, Mediterranean diet, and the risk of chronic diseases: The EPIC-Potsdam study. BMC Med. 2018, 16, 99. [Google Scholar] [CrossRef]
- Al-Dayyat, H.M.; Rayyan, Y.M.; Reema Fayez Tayyem, R.F. Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors. Diabetes Metab. Syndr. 2018, 12, 569–575. [Google Scholar] [CrossRef]
- Agudo, A.; Cayssials, V.; Bonet, C.; Tjønneland, A.; Overvad, K.; Boutron-Ruault, M.C.; Affret, A.; Fagherazzi, G.; Katzke, V.; Schübel, R.; et al. Inflammatory potential of the diet and risk of gastric cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am. J. Clin. Nutr. 2018, 107, 607–616. [Google Scholar] [CrossRef]
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients 2017, 9, 1227. [Google Scholar] [CrossRef] [Green Version]
- Lăcătușu, C.M.; Grigorescu, E.D.; Floria, M.; Alina Onofriescu, A.; Mihai, B.M. The Mediterranean Diet: From an Environment-Driven Food Culture to an Emerging Medical Prescription. Int. J. Environ. Res. Public Health 2019, 16, 942. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Ding, N.; Katherine, L.; Tucker, K.L.; Weisskopf, M.G.; Sparrow, D.; Hu, H.; Park, S.K. A Western Diet Pattern Is Associated with Higher Concentrations of Blood and Bone Lead among Middle-Aged and Elderly Men. J. Nutr. 2017, 147, 1374–1383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet: A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef] [PubMed]
- Winkvist, A.; Bärebring, L.; Gjertsson, I.; Ellegård, L.; Lindqvist, H.M. A randomized controlled cross-over trial investigating the effect of anti-inflammatory diet on disease activity and quality of life in rheumatoid arthritis: The Anti-inflammatory Diet in Rheumatoid Arthritis (ADIRA) study protocol. Nutr. J. 2018, 17, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dobrosielski, D.A.; Papandreou, C.; Patil, S.P.; Salas-Salvadó, J. Diet and exercise in the management of obstructive sleep apnoea and cardiovascular disease risk. Eur. Respir. Rev. 2017, 26, 160110. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.h.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menotti, A.; Puddu, P.E. How the seven countries study contributed to the definition and development of the Mediterranean diet concept: A 50-year journey. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Mora, J.J.; García-Vigara, A.; Sánchez-Sánchez, M.L.; Miguel-Ángel García-Pérez, M.A.; Tarín, J.; Cano, A. The Mediterranean diet: Ahistorical perspective on food for health. Maturitas 2020, 132, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Cani, P.D.; Van Hul, M. Mediterranean diet, gut microbiota, and health: When age and calories do not add up! Gut 2020, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meslier, V.; Laiola, M.; Roager, H.M.; De Filippis, F.; Roume, H.; Quinquis, B.; Giacco, R.; Mennella, I.; Ferracane, R.; Pons, N.; et al. Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independentlyof energy intake. Gut 2020. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, T.S.; Rampelli, S.; Jeffery, I.B.; Santoro, A.; Neto, M.; Capri, M.; Giampieri, E.; Jennings, A.; Candela, M.; Turroni, S.; et al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: The NU-AGE 1-year dietary intervention across five European countries. Gut 2020. [Google Scholar] [CrossRef] [Green Version]
- Bonaccio, M.; Di Castelnuovo, A.; De Curtis, A.; Costanzo, S.; Persichillo, M.; Donati, M.B.; Cerletti, C.H.; Iacoviello, L.; de Gaetano, G.; Moli-sani Project Investigators. Adherence to the Mediterranean diet is associated with lower platelet and leukocyte counts: Results from the Moli-sani study. Blood 2014, 123, 3037–3044. [Google Scholar] [CrossRef] [Green Version]
- Mena, M.P.; Sacanella, E.; Vazquez-Agell, M.; Morales, M.; Fitó, M.; Escoda, R.; Serrano-Martínez, M.; Salas-Salvadó, J.; Benages, B.; Casas, R.; et al. Inhibition of circulating immune cell activation: A molecular antiinflammatory effect of the Mediterranean diet. Am. J. Clin. Nutr. 2009, 89, 248–256. [Google Scholar] [CrossRef] [Green Version]
- Ibarra, O.; Gili, M.; Roca, M.; Vives, M.; Serrano, M.J.; Pareja, A.; Garcia-Campayo, J.; Gomez-Juanes, R.; Garcia-Toro, M. The Mediterranean Diet and micronutrient levels in depressive patients. Nutr. Hosp. 2015, 31, 1171–1175. [Google Scholar] [CrossRef]
- Guner, S.; Guner, S.I.; Gokalp, M.A.; Ceylan, M.F.; Unsal, S.S.; Demir, H. Do the Trace Elements Play a Role in the Etiopathogenesis of Developmental Dysplasia of Hip? Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 910–913. [Google Scholar]
- Castiglione, D.; Platania, A.; Conti, A.; Falla, M.; D’Urso, M.; Marranzano, M. Dietary Micronutrient and Mineral Intake in the Mediterranean Healthy Eating, Ageing, and Lifestyle (MEAL) Study. Antioxidants 2018, 7, 79. [Google Scholar] [CrossRef] [Green Version]
- Mesías, M.; Seiquer, I.; Navarro, P.M. Is the Mediterranean diet adequate to satisfy zinc requirements during adolescence? Public Health Nutr. 2012, 15, 1429–1436. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Yosef, N.; Thalhamer, T.; Zhu, C.H.; Xiao, S.H.; Kishi, Y.; Aviv Regev, A.; Kuchroo, K.V. Induction of Pathogenic TH17 Cells by Inducible Salt-Sensing Kinase SGK1. Nature 2013, 496, 513–517. [Google Scholar] [CrossRef] [Green Version]
- Kleinewietfeld, M.; Manzel, A.; Titze, J.; Kvakan, H.; Yosef, N.; Linker, R.A.; Muller, D.N.; Hafler, D.A. Sodium Chloride Drives Autoimmune Disease by the Induction of Pathogenic TH17 Cells. Nature 2013, 496, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Min, B.; Fairchild, R.L. Over-salting ruins the balance of the immune menu. Clin. Investig. 2015, 125, 4002–4004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- La Verde, M.; Mulè, S.; Zappalà, G.; Privitera, G.; Maugeri, G.; Pecora, F.; Marina Marranzano, M. Higher Adherence to the Mediterranean Diet Is Inversely Associated With Having Hypertension: Is Low Salt Intake a Mediating Factor? Int. J. Food Sci Nutr. 2018, 69, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.L.; Chin, K.Y. The Biological Activities of Oleocanthal from a Molecular Perspective. Nutrients 2018, 10, 570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogliano, V.; Sacchi, R. Oleocanthal in olive oil: Between myth and reality. Mol. Nutr. Food Res. 2006, 50, 5–6. [Google Scholar] [CrossRef] [PubMed]
- De Roos, B.; Zhang, X.; Gutierrez, G.R.; Wood, S.H.; Rucklidge, G.J.; Reid, M.D.; Duncan, G.J.; Cantlay, L.L.; Duthie, G.G.; O’Kennedy, N. Anti-platelet effects of olive oil extract: In vitro functional and proteomic studies. Eur. J. Nutr. 2011, 50, 553–562. [Google Scholar] [CrossRef]
- Luque-Sierra, A.; Alvarez-Amor, L.; Robert Kleemann, R.; Martín, F.; Varela, L.M. Extra-Virgin Olive Oil with Natural Phenolic Content Exerts an Anti-Inflammatory Effect in Adipose Tissue and Attenuates the Severity of Atherosclerotic Lesions in Ldlr-/-.Leiden Mice. Mol. Nutr. Food Res. 2018, 62, e1800295. [Google Scholar] [CrossRef]
- Debbabi, M.; Zarrouk, A.; Bezine, M.; Meddeb, W.; Nury, T.H.; AsmaaBadreddine, A.; Karym, E.M.; Sghaier, R.; Bretillon, L.; Guyot, S.; et al. Comparison of the effects of major fatty acids present in the Mediterranean diet (oleic acid, docosahexaenoic acid) and in hydrogenated oils (elaidic acid) on 7-ketocholesterol-induced oxiapoptophagy in microglial BV-2 cells. Chem. Phys. Lipids 2017, 207, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Yarla, N.S.; Polito, A.; Peluso, I. Effects of Olive Oil on TNF-α and IL-6 in Humans: Implication in Obesity and Frailty. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Naruszewicz, M.; Czerwińska, M.E.; Kiss, A.K. Oleacein. Translation from Mediterranean Diet to Potential Antiatherosclerotic Drug. Curr. Pharm. Des. 2014, 21. [Google Scholar] [CrossRef]
- Martorell, M.; Capó, X.; Sureda, A.; Tur, J.A.; Pons, P. Effects of docosahexaenoic acid diet supplementation, training, and acute exercise on oxidative balance in neutrophils. Appl. Physiol. Nutr. Metab. 2014, 39, 446–457. [Google Scholar] [CrossRef]
- Martínez-Soto, J.C.; Domingo, J.C.; BegoñaCordobilla, B.; Nicolás, M.; Fernández, L.; Albero, P.; Gadea, J.; Landeras, J. Dietary supplementation with docosahexaenoic acid (DHA) improves seminal antioxidant status and decreases sperm DNA fragmentation. Syst. Biol. Reprod. Med. 2016, 62, 387–395. [Google Scholar] [CrossRef] [Green Version]
- Kumar, V.N.; Elango, P.; Asmathulla, S.; Kavimani, S. A Systematic Review on Lycopene and its Beneficial Effects. Biomed. Pharmacol. J. 2017, 10. [Google Scholar] [CrossRef]
- Cicerale, S.; Lucas, L.J.; Keast, R.S.J. Oleocanthal: A Naturally Occurring Anti-Inflammatory Agent in Virgin Olive Oil. Olive Oil-Const. Qual. Health Prop. Bioconversions 2012. [Google Scholar] [CrossRef] [Green Version]
- Han, G.M.; Han, X.F. Lycopene reduces mortality in people with systemic lupus erythematosus: A pilot study based on the third national health and nutrition examination survey. J. Dermatol. Treat. 2016, 27, 430–435. [Google Scholar] [CrossRef]
- Buyuklu, M.; Kandemir, F.M.; Ozkaraca, M.; Set, T.; Bakirci, E.M.; Topal, E.M.; Ileriturk, M.; Turkmen, K. Benefical effects of lycopene against contrast medium-induced oxidative stress, inflammation, autophagy, and apoptosis in rat kidney. Hum. Exp. Toxicol. 2015, 34, 487–496. [Google Scholar] [CrossRef]
- Liu, X.; Allen, J.D.; Arnold, J.T.; Blackman, M.R. Lycopene inhibits IGF-I signal transduction and growth in normal prostate epithelial cells by decreasing DHT-modulated IGF-I production in co-cultured reactive stromal cells. Carcinogenesis 2008, 29, 816–823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, P.M.; Wu, Z.Z.; Zhang, Y.Q.; Wung, B.S. Lycopene inhibits ICAM-1 expression and NF-κB activation by Nrf2-regulated cell redox state in human retinal pigment epithelial cells. Life Sci. 2016, 155, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, V.; Rodríguez-Rodríguez, R.; Martínez-Garza, U.; Rosell-Cardona, C.; Lamuela-Raventós, R.M.; Marrero, P.F.; Haro, D.; Relat, J. Mediterranean Tomato-Based Sofrito Sauce Improves Fibroblast Growth Factor 21 (FGF21) Signaling in White Adipose Tissue of Obese ZUCKER Rats. Mol. Nutr. Food Res. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.H.; Kim, W.K.; Ha, A.W.; Kim, M.H.; Chang, M.J. Anti-inflammatory effect of lycopene in SW480 human colorectal cancer cells. Nutr. Res. Pract. 2017, 11, 90–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varriale, A. DNA methylation, epigenetics, and evolution in vertebrates: Facts and challenges. Int. J. Evol. Biol. 2014, 2014, 475981. [Google Scholar] [CrossRef]
- Jones, P.A.; Takai, D. The role of DNA methylation in mammalian epigenetics. Science 2001, 293, 1068–1070. [Google Scholar] [CrossRef] [PubMed]
- Roncero-Ramos, I.; Rangel-Zuñiga, O.A.; Lopez-Moreno, J.; Alcala-Diaz, J.F.; Perez-Martinez, P.; Jimenez-Lucena, R.; Castaño, J.P.; Roche, H.M.; Javier Delgado-Lista, J.; Ordovas, J.M.; et al. Mediterranean Diet, Glucose Homeostasis, and Inflammasome Genetic Variants: The CORDIOPREV Study. Mol. Nutr. Food Res. 2018, 62, e1700960. [Google Scholar] [CrossRef]
- Carruba, G.; Cocciadiferro, L.; Di Cristina, A.; Granata, O.M.; Dolcemascolo, C.; Campisi, I.; Zarcone, M.; Cinquegrani, M.; Traina, A. Nutrition, aging and cancer: Lessons from dietary intervention studies. Immun. Ageing 2016, 13, 13. [Google Scholar] [CrossRef]
- Malireddy, S.; Kotha, S.R.; Secor, J.D.; Gurney, T.O.; Abbott, J.A.; Maulik, G.; Maddipati, K.R.; Parinandi, N.L. Phytochemical antioxidants modulate mammalian cellular epigenome: Implications in health and disease. Antioxid. Redox Signal. 2012, 17, 327–339. [Google Scholar] [CrossRef] [Green Version]
- Victorelli, S.; Passos, J.F. Telomeres and Cell Senescence. Size Matters Not. 2017, 21, 14–20. [Google Scholar]
- Leung, C.W.; Fung, T.T.; McEvoy, C.T.; Lin, J.; Epel, E.S. Diet Quality Indices and Leukocyte Telomere Length Among Healthy US Adults: Data from the National Health and Nutrition Examination Survey, 1999–2002. Am. J. Epidemiol. 2018, 187, 2192–2201. [Google Scholar] [CrossRef] [Green Version]
- Nonino, C.B.; Pinhanelli, V.C.; Noronha, N.Y.; Quinhoneiro, D.C.G.; Pinhel, M.S.; De Oliveira, B.A.P.; Marchini, J.S.; Nicoletti, C.F. Green tea supplementation promotes leukocyte telomere length elongation in obese women. La suplementación con té verde promueve la elongación de los telómeros de leucocitos en mujeresobesas. Nutr. Hosp. 2018, 35, 570–575. [Google Scholar]
- Gomez-Delgado, F.; Delgado-Lista, J.; Lopez-Moreno, J.; Rangel-Zuñiga, O.A.; Alcala-Diaz, J.F.; Leon-Acuña, A.; Corina, A.; Yubero-Serrano, E.; Torres-Peña, J.D.; Camargo, A.; et al. Telomerase RNA Component Genetic Variants Interact with the Mediterranean Diet Modifying the Inflammatory Status and its Relationship with Aging: CORDIOPREV Study. J. Gerontol. Biol. Sci. Med. Sci. 2018, 73, 327–332. [Google Scholar] [CrossRef] [Green Version]
- Chaudhry, H.; Zhou, J.; Zhong, Y.; Ali, M.M.; McGuire, F.; Nagarkatti, P.S.; Nagarkatti, M. Role of Cytokines as a Double-edged Sword in Sepsis. In Vivo 2013, 27, 669–684. [Google Scholar] [PubMed]
- Sakhaei, R.; Shahvazi, S.; Mozaffari-Khosravi, H.; Samadi, M.; Khatibi, N.; Nadjarzadeh, A.; Zare, F.; Salehi-Abargouei, A. The dietary approaches to stop hypertension (DASH)-style diet and an alternative Mediterranean diet are differently associated with serum inflammatory markers in female adults. Food Nutr. Bull. 2018, 39, 361–376. [Google Scholar] [CrossRef]
- Clements, S.J.; Maijo, M.; Ivory, K.; Nicoletti, C.; Carding, S.R. Age-Associated Decline in Dendritic Cell Function, and the Impact of Mediterranean Diet Intervention in Elderly Subjects. Front. Nutr. 2017, 4, 65. [Google Scholar] [CrossRef] [Green Version]
- Bédard, A.; Tchernof, A.; Lamarche, B.; Corneau, L.; Dodin, S.; Lemieux, S. Effects of the traditional Mediterranean diet on adiponectin and leptin concentrations in men and premenopausal women: Do sex differences exist? Eur. J. Clin. Nutr. 2014, 68, 561–566. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.A.; González Sagrado, M.; Aller, R.; Conde, R.; Izaola, O.; de la Fuente, B.; Primo, D. Roles of G1359A polymorphism of the cannabinoid receptor gene (CNR1) on weight loss and adipocytokines after a hypocaloric diet. Nutr. Hosp. 2011, 26, 317–322. [Google Scholar]
- Arpón, A.; Milagro, F.I.; Razquin, C.; Corella, D.; Estruch, R.; Fitó, M.; Marti, A.; Martínez-González, M.A.; Ros, E.; Salas-Salvadó, J.; et al. Impact of Consuming Extra-Virgin Olive Oil or Nuts within a Mediterranean Diet on DNA Methylation in Peripheral White Blood Cells within the PREDIMED-Navarra Randomized Controlled Trial: A Role for Dietary Lipids. Nutrients 2017, 10, 15. [Google Scholar] [CrossRef] [Green Version]
- Miljković, D.; Dekanski, D.; Miljković, Z.; Momčilović, M.; Mostarica-Stojkovic, M. Dry olive leaf extract ameliorates experimental autoimmune encephalomyelitis. Clin. Nutr. J. 2009, 28, 346–350. [Google Scholar] [CrossRef]
- Borges-Costa, J.; Silva, R.; Gonçalves, L.; Filipe, P.; de Almeida, L.S.; Gomes, M.M. Clinical and laboratory features in acute generalized pustular psoriasis: A retrospective study of 34 patients. Am. J. Clin. Dermatol. 2011, 12, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Augustin, M.; Kirsten, N.; Körber, A.; Wilsmann-Theis, D.; Itschert, G.; Staubach-Renz, P.; Maul, J.T.; Zander, N. Prevalence, Predictors and Comorbidity of Dry Skin in the General Population. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 147–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shalom, G.; Zisman, D.; Babaev, M.; Horev, A.; Tiosano, S.; Schonmann, Y.; Comaneshter, D.; Cohen, A.D. Psoriasis in Israel: Demographic, epidemiology, and healthcare services utilization. Int. J. Dermatol. 2018, 57, 1068–1074. [Google Scholar] [CrossRef]
- Lee, E.J.; Han, K.D.; Han, J.H.; Lee, J.H. Smoking and risk of psoriasis: A nationwide cohort study. J. Am. Acad. Dermatol. 2017, 77, 573–575. [Google Scholar] [CrossRef] [Green Version]
- Parisi, R.; Webb, R.T.; Carr, M.J.; Moriarty, K.J.; Kleyn, K.E.; Griffiths, C.E.M.; Ashcrof, D.M. Alcohol-Related Mortality in Patients with Psoriasis: A Population-Based Cohort Study. JAMA Dermatol. 2017, 153, 1256–1262. [Google Scholar] [CrossRef] [PubMed]
- Barrea, L.; Nappi, F.; Di Somma, C.; Savanelli, M.C.; Falco, A.; Balato, A.; Balato, N.; Savastano, S. Environmental Risk Factors in Psoriasis: The Point of View of the Nutritionist. Int. J. Environ. Res. Public Health 2016, 13, 743. [Google Scholar] [CrossRef] [Green Version]
- Huerta, C.; Rivero, E.; García Rodríguez, L.A. Incidence and risk factors for psoriasis in the general population. Arch. Dermatol. 2007, 143, 1559–1565. [Google Scholar] [CrossRef] [Green Version]
- Barrea, L.; Balato, N.; Di Somma, C.; Macchia, P.E.; Napolitano, M.; Savanelli, M.C.; Esposito, K.; Annamaria Colao, A.; Savastano, S.; Savanelli, M.; et al. Nutrition and psoriasis: Is there any association between the severity of the disease and adherence to the Mediterranean diet? J. Transl. Med. 2015, 13, 18. [Google Scholar] [CrossRef] [Green Version]
- Lin, X.; Meng, X.; Zhiqi, S. Homocysteine and psoriasis. Biosci. Rep. 2019, 39. [Google Scholar] [CrossRef] [PubMed]
- Balić, A.; Vlašić, D.; Zužul, K.; Marinović, B.; BukvićMokos, Z. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Int. J. Mol. Sci. 2020, 21, 741. [Google Scholar] [CrossRef] [Green Version]
- Damiani, G.; Bragazzi, N.L.; McCormick, T.S.; Daniele, P.; Pigatto, M.; Pacifico, A.; Tiodorovic, D.; Di Franco, S.; Alfieri, A.; Fiore, M.; et al. Gut microbiota and nutrient interactions with skin in psoriasis: A comprehensive review of animal and human studies. World J. Clin. Cases 2020, 8, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.R.; Lee, J.H. An observational study on the obesity and metabolic status of psoriasis patients. Ann. Dermatol. 2013, 25, 440–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, P.B. Is dietary supplementation more common among adults with psoriasis? Results from the National Health and Nutrition Examination Survey. Complement. Ther. Med. 2014, 22, 159–165. [Google Scholar] [CrossRef]
- Murray, M.L.; Bergstresser, P.R.; Adams-Huet, B.; Cohen, J.B. Relationship of psoriasis severity to obesity using same-gender siblings as controls for obesity. Clin. Exp. Dermatol. 2009, 34, 140–144. [Google Scholar] [CrossRef]
- Wolk, K.; Mallbris, L.; Larsson, P.; Rosenblad, A.; Vingård, E.; Ståhle, M. Excessive body weight and smoking associates with a high risk of onset of plaque psoriasis. Acta Derm. Venereol. 2009, 89, 492–497. [Google Scholar] [CrossRef]
- Paller, A.S.; Mercy, K.; Kwasny, M.J.; Choon, S.E.; Cordoro, K.M.; Girolomoni, G.; Menter, A.; Tom, W.L.; Mahoney, A.M.; Annet, M.; et al. Association of pediatric psoriasis severity with excess and central adiposity: An international cross-sectional study. JAMA Dermatol. 2013, 149, 166–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schön, M.P.; Erpenbeck, L. The Interleukin-23/Interleukin-17 Axis Links Adaptive and Innate Immunity in Psoriasis. Front. Immunol. 2018, 9, 1323. [Google Scholar] [CrossRef] [Green Version]
- Carrascosa, J.M.; Rocamora, V.; Fernandez-Torres, R.M.; Jimenez-Puya, R.; Moreno, J.C.; Coll-Puigserver, N.; Fonseca, E. Obesity and psoriasis: Inflammatory nature of obesity, relationship between psoriasis and obesity, and therapeutic implications. Actas Dermosifiliogr. 2014, 105, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, C.; Kouvari, M.; D’Cunha, N.M.; Georgousopoulou, E.N.; Panagiotakos, D.B.; Duane, D.; Mellor, D.D.; Kellett, J.; Naumovski, N. The effects of the Mediterranean diet on rheumatoid arthritis prevention and treatment: A systematic review of human prospective studies. Rheumatol. Int. 2018, 38, 737–747. [Google Scholar] [CrossRef]
- Constantin, M.M.; Nita, I.E.; Olteanu, R.; Constantin, T.; Bucur, S.; Matei, C.; Raducan, A. Significance and impact of dietary factors on systemic lupus erythematosus pathogenesis. Exp. Ther. Med. 2019, 17, 1085–1090. [Google Scholar] [CrossRef] [Green Version]
- Stamostergiou, J.; Theodoridis, X.; Ganochoriti, V.; Bogdanos, D.P.; Sakkas, L.I. The Role of the Mediterranean Diet in Hyperuricemia and Gout. Mediterr. J. Rheumatol. 2018, 29, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Kontogianni, M.D.; Chrysohoou, C.; Panagiotakos, D.B.; Tsetsekou, E.; Zeimbekis, A.; Pitsavos, C.; Stefanadis, C. Adherence to the Mediterranean diet and serum uric acid: The ATTICA study. Scand. J. Rheumatol. 2012, 41, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Prasad, P.; Krishnan, E. Filipino gout: A review. Arthritis Care Res. 2014, 66, 337–343. [Google Scholar] [CrossRef]
- Choi, J.W.; Ford, E.S.; Gao, X.; Choi, H.K. Sugar-sweetened soft drinks, dietsoft drinks, and serum uric acid level: The Third National Health andNutrition Examination Survey. Arthritis Rheum. 2008, 59, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.Y.; Appel, L.J.; Choi, M.J.; Gelber, A.C.; Charleston, J.; Norkus, E.P.; Miller, E.R., III. The effects of vitamin C supplementation on serum concentrations of uric acid: Results of a randomized controlled trial. Arthritis Rheum. 2005, 52, 1843–1847. [Google Scholar] [CrossRef]
- Li, X.; Meng, X.; Timofeeva, M.; Tzoulaki, I.; Tsilidis, K.K.; Ioannidis, J.P.; Campbell, H.; Theodoratou, E. Serum uric acid levels and multiple health outcomes: Umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ 2017, 357, j2376. [Google Scholar] [CrossRef] [Green Version]
- Andrés, M.; Sivera, F.; Falzon, L.; Buchbinder, R.; Carmona, L. Dietarysupplements for chronic gout. Cochrane Database Syst. Rev. 2014, 10, CD010156. [Google Scholar]
- Hernáez, Á.; Castañer, O.; Elosua, R.; Pintó, X.; Estruch, R.; Salas-Salvadó, J.; Corella, D.; Arós, F.; Serra-Majem, L.; Fiol, M.; et al. Mediterranean Diet Improves High-Density Lipoprotein Function in High-Cardiovascular-Risk Individuals: A Randomized Controlled Trial. Circulation 2017, 135, 633–643. [Google Scholar] [CrossRef] [Green Version]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and Vascular Effect of the Mediterranean Diet. Int. J. Mol. Sci. 2019, 20, 4716. [Google Scholar] [CrossRef] [Green Version]
- Sureda, A.; Bibiloni, M.D.M.; Julibert, A.; Bouzas, C.; Argelich, E.; Llompart, I.; Pons, A.; Tur, J.A. Adherence to the Mediterranean Diet and Inflammatory Markers. Nutrients 2018, 10, 62. [Google Scholar] [CrossRef] [Green Version]
- Paterson, K.E.; Myint, P.K.; Jennings, A.; Bain, L.K.M.; Lentjes, M.; Khaw, K.T.; Welch, A.A. Mediterranean Diet Reduces Risk of Incident Stroke in a Population with Varying Cardiovascular Disease Risk Profiles. Stroke 2018, 49, 2415–2420. [Google Scholar]
- Iliadi, V.; Shirobokova, S.; Soloviev, A.; Konstantinidis, T. Study of Cells Blebbing in Patients with Allergy Disorders. J. Allerg. Res. 2019, 1, 43–47. [Google Scholar]
- Garcia-Marcos, L. Mediterranean Diet as a Protection Against Asthma: Still Another Brick in Building a Causative Association. Allergol. Immunopathol. 2016, 44, 97–98. [Google Scholar] [CrossRef] [PubMed]
- Arvaniti, F.; Priftis, K.N.; Panagiotakos, D.B. Dietary habits and asthma: A review. Allergy Asthma Proc. 2010, 31, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.G.; Garg, M.L.; Powell, H.; Gibson, P.G. Lycopene-rich treatments modify noneosinophilic airway inflammation in asthma: Proof of concept. Free Radic. Res. 2008, 42, 94–102. [Google Scholar] [CrossRef]
- Okada, H.; Kuhn, C.; Feillet, H.; Bach, J.F. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: An update. Clin. Exp. Immunol. 2010, 160, 1–9. [Google Scholar] [CrossRef]
- Tsigalou, C.; Konstantinidis, T.G.; Cassimos, D.; Karvelas, A.; Grapsa, A.; Tsalkidis, A.; Panopoulou, M.; Tsakris, A. Inverse association between Helicobacter pylori infection and childhood asthma in Greece: A case-control study. GERMS 2019, 9, 182–187. [Google Scholar] [CrossRef]
- Tilles, S.A. Microbes, Infections, and Their Relationship to Asthma. Immunol. Allergy Clin. N. Am. 2019, 39, xiii–xiv. [Google Scholar] [CrossRef]
- Fischer, A.; Johansson, I.; Anders Blomberg, A.; Sundström, B.; Anders Blomberg, A.; Sundström, B. Adherence to a Mediterranean-like Diet as a Protective Factor Against COPD: A Nested Case-Control Study. COPD J. Chronic Obstr. Pulm. Dis. 2019, 16, 272–277. [Google Scholar] [CrossRef] [Green Version]
- Shivashankar, R.; Lewis, J.D. The Role of Diet in Inflammatory Bowel Disease. Curr. Gastroenterol. Rep. 2017, 19, 22. [Google Scholar] [CrossRef] [Green Version]
- Aleksandrova, K.; Romero-Mosquera, B.; Hernandez, V. Diet, Gut Microbiome and Epigenetics: Emerging Links with Inflammatory Bowel Diseases and Prospects for Management and Prevention. Nutrients 2017, 9, 962. [Google Scholar] [CrossRef]
- Molendijk, I.; van der Marel, S.; Maljaars, P.W.J. Towards a Food Pharmacy: Immunologic Modulation through Diet. Nutrients 2019, 11, 1239. [Google Scholar] [CrossRef] [Green Version]
- Gray, M.S.; Wang, H.E.; Martin, K.D.; Donnelly, J.P.; Gutiérrez, O.M.; Shikany, J.M.; Judd, S.E.; Shikany, J.M.; Judd, S.E. Adherence to Mediterranean-style Diet and Risk of Sepsis in the REasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort. Br. J. Nutr. 2018, 120, 1415–1421. [Google Scholar] [CrossRef] [Green Version]
- Nettleton, J.A.; Steffen, L.M.; Mayer-Davis, E.J.; Jenny, N.S.; Jiang, R.; Herrington, D.M.; Jacobs, D.R., Jr.; Jenny, N.S.; Jiang, R.; Herrington, D.M.; et al. Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Clin. Nutr. 2006, 83, 1369–1379. [Google Scholar] [CrossRef]
- Gutiérrez, O.M.; Judd, S.E.; Voeks, J.H.; Carson, A.P.; Safford, M.M.; Shikany, J.M.; Wang, H.E.; Carson, A.P.; Safford, M.M.; Shikany, J.M.; et al. Diet patterns and risk of sepsis in communitydwelling adults: A cohort study. BMC Infect. Dis. 2015, 15, 231–239. [Google Scholar] [CrossRef] [Green Version]
- Rivera, C.A.; Gaskin, L.; Singer, G.; Houghton, J.; Allman, M. Western diet enhances hepatic inflammation in mice exposed to cecal ligation and puncture. BMC Physiol. 2010, 10, 20. [Google Scholar] [CrossRef] [Green Version]
- Strandberg, L.; Verdrengh, M.; Enge, M.; Andersson, N.; Amu, S.; Onnheim, K.; Benrick, A.; Brisslert, M.; Bylund, J.; Bokarewa, M.; et al. Mice chronically fed high-fat diet have increased mortality and disturbed immune response in sepsis. PLoS ONE 2009, 4, e7605. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsigalou, C.; Konstantinidis, T.; Paraschaki, A.; Stavropoulou, E.; Voidarou, C.; Bezirtzoglou, E. Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicines 2020, 8, 201. https://0-doi-org.brum.beds.ac.uk/10.3390/biomedicines8070201
Tsigalou C, Konstantinidis T, Paraschaki A, Stavropoulou E, Voidarou C, Bezirtzoglou E. Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicines. 2020; 8(7):201. https://0-doi-org.brum.beds.ac.uk/10.3390/biomedicines8070201
Chicago/Turabian StyleTsigalou, Christina, Theocharis Konstantinidis, Afroditi Paraschaki, Elisavet Stavropoulou, Chrissoula Voidarou, and Eugenia Bezirtzoglou. 2020. "Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview" Biomedicines 8, no. 7: 201. https://0-doi-org.brum.beds.ac.uk/10.3390/biomedicines8070201