Neonatal Resuscitation with an Intact Cord: Current and Ongoing Trials
Abstract
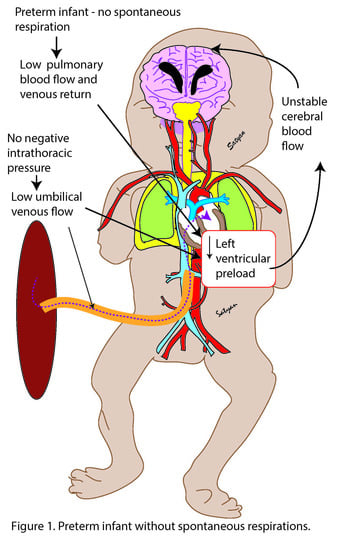
:1. Introduction
2. Feasibility Studies in Preterm Infants
3. Completed Randomized Controlled Trials
4. Ongoing Randomized Controlled Trials
5. Challenges with Resuscitation with an Intact Cord
6. Conclusions
Funding
Conflicts of Interest
References
- Andersson, O.; Lindquist, B.; Lindgren, M.; Stjernqvist, K.; Domellof, M.; Hellstrom-Westas, L. Effect of delayed cord clamping on neurodevelopment at 4 years of age: A randomized clinical trial. JAMA Pediatr. 2015, 169, 631–638. [Google Scholar] [CrossRef]
- Tarnow-Mordi, W.; Morris, J.; Kirby, A.; Robledo, K.; Askie, L.; Brown, R.; Evans, N.; Finlayson, S.; Fogarty, M.; Gebski, V.; et al. Delayed versus immediate cord clamping in preterm infants. N. Engl. J. Med. 2017. [Google Scholar] [CrossRef]
- Fogarty, M.; Osborn, D.A.; Askie, L.; Seidler, A.L.; Hunter, K.; Lui, K.; Simes, J.; Tarnow-Mordi, W. Delayed vs early umbilical cord clamping for preterm infants: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2018, 218, 1–18. [Google Scholar] [CrossRef]
- Redmond, A.; Isana, S.; Ingall, D. Relation of onset of respiration to placental transfusion. Lancet 1965, 1, 283–285. [Google Scholar] [CrossRef]
- Philip, A.G.; Yee, A.B.; Rosy, M.; Surti, N.; Tsamtsouris, A.; Ingall, D. Placental transfusion as an intrauterine phenomenon in deliveries complicated by foetal distress. Br. Med. J. 1969, 2, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Vyas, H.; Milner, A.D.; Hopkins, I.E. Intrathoracic pressure and volume changes during the spontaneous onset of respiration in babies born by cesarean section and by vaginal delivery. J. Pediatr. 1981, 99, 787–791. [Google Scholar] [CrossRef]
- Katheria, A.C.; Lakshminrusimha, S.; Rabe, H.; McAdams, R.; Mercer, J.S. Placental transfusion: A review. J. Perinatol. 2017, 37, 105–111. [Google Scholar] [CrossRef]
- Ersdal, H.L.; Linde, J.; Mduma, E.; Auestad, B.; Perlman, J. Neonatal outcome following cord clamping after onset of spontaneous respiration. Pediatrics 2014, 134, 265–272. [Google Scholar] [CrossRef]
- Nevill, E.; Meyer, M.P. Effect of delayed cord clamping (dcc) on breathing and transition at birth in very preterm infants. Early Hum. Dev. 2015, 91, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Alison, B.J.; Wallace, E.M.; Crossley, K.J.; Gill, A.W.; Kluckow, M.; te Pas, A.B.; Morley, C.J.; Polglase, G.R.; Hooper, S.B. Delaying cord clamping until ventilation onset improves cardiovascular function at birth in preterm lambs. J. Physiol. 2013, 591, 2113–2126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatt, S.; Polglase, G.R.; Wallace, E.M.; Te Pas, A.B.; Hooper, S.B. Ventilation before umbilical cord clamping improves the physiological transition at birth. Front. Pediatr. 2014, 2, 113. [Google Scholar] [CrossRef]
- Richardson, D.K.; Phibbs, C.S.; Gray, J.E.; McCormick, M.C.; Workman-Daniels, K.; Goldmann, D.A. Birth weight and illness severity: Independent predictors of neonatal mortality. Pediatrics 1993, 91, 969–975. [Google Scholar] [CrossRef]
- Winter, J.; Kattwinkel, J.; Chisholm, C.; Blackman, A.; Wilson, S.; Fairchild, K. Ventilation of preterm infants during delayed cord clamping (ventfirst): A pilot study of feasibility and safety. Am. J. Perinatol. 2017, 34, 111–116. [Google Scholar] [CrossRef]
- Blank, D.A.; Badurdeen, S.; Omar, F.K.C.; Jacobs, S.E.; Thio, M.; Dawson, J.A.; Kane, S.C.; Dennis, A.T.; Polglase, G.R.; Hooper, S.B.; et al. Baby-directed umbilical cord clamping: A feasibility study. Resuscitation 2018, 131, 1–7. [Google Scholar] [CrossRef]
- Knol, R.; Brouwer, E.; Vernooij, A.S.N.; Klumper, F.J.C.M.; DeKoninck, P.; Hooper, S.B.; te Pas, A.B. Clinical aspects of incorporating cord clamping into stabilisation of preterm infants. Arch. Dis. Child Fetal. Neonatal. Ed. 2018, 103, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Pratesi, S.; Montano, S.; Ghirardello, S.; Mosca, F.; Boni, L.; Tofani, L.; Dani, C. Placental circulation intact trial (PCI-T)—resuscitation with the placental circulation intact vs. Cord milking for very preterm infants: A feasibility study. Front. Pediatr. 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Duley, L.; Dorling, J.; Pushpa-Rajah, A.; Oddie, S.J.; Yoxall, C.W.; Schoonakker, B.; Bradshaw, L.; Mitchell, E.J.; Fawke, J.A. Randomised trial of cord clamping and initial stabilisation at very preterm birth. Arch. Dis. Child Fetal. Neonatal. Ed. 2017. [Google Scholar] [CrossRef]
- Katheria, A.; Poeltler, D.; Durham, J.; Steen, J.; Rich, W.; Arnell, K.; Maldonado, M.; Cousins, L.; Finer, N. Neonatal resuscitation with an intact cord: A randomized clinical trial. J. Pediatr. 2016, 178, 75–80. [Google Scholar] [CrossRef]
- Katheria, A.C.; Brown, M.K.; Faksh, A.; Hassen, K.O.; Rich, W.; Lazarus, D.; Steen, J.; Daneshmand, S.S.; Finer, N.N. Delayed cord clamping in newborns born at term at risk for resuscitation: A feasibility randomized clinical trial. J. Pediatr. 2017, 187, 313–317. [Google Scholar] [CrossRef]
- Thomas, M.R.; Yoxall, C.W.; Weeks, A.D.; Duley, L. Providing newborn resuscitation at the mother’s bedside: Assessing the safety, usability and acceptability of a mobile trolley. BMC Pediatr. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Katheria, A.C.; Sorkhi, S.R.; Hassen, K.; Faksh, A.; Ghorishi, Z.; Poeltler, D. Acceptability of bedside resuscitation with intact umbilical cord to clinicians and patients’ families in the united states. Front. Pediatr. 2018, 6, 100. [Google Scholar] [CrossRef]

| Study | n | GA (weeks) | Intervention | Time of Cord Clamping, Control Arm | Time of Cord Clamping Intervention Arm | Clinical Outcome |
|---|---|---|---|---|---|---|
| Duley et al., 2017 [17] | 137 | 23–31 | Resuscitation if needed | 20 s | 120 s | No difference |
| Katheria et al., 2016 [18] | 154 | 23–31 | CPAP and PPV if apneic | 60 s | 60 s | No difference |
| Katheria et al., 2018 [19] | 60 | 37–42 | Resuscitation if needed | 60 s | 3–5 min | No Difference |
| Study | Proposed N | GA (weeks) | Intervention | Time of Cord Clamping, Control Arm | Time of Cord Clamping Intervention Arm | Primary Outcome |
|---|---|---|---|---|---|---|
| VentFirst | 940 | 23–28 | CPAP 30–120 s | 30–60 s | 120 s | IVH |
| Nep-Cord 3 | 231 | 37–41 | Resuscitation if needed | <60 s | 180 s | SpO2, HR, and Apgar scores in first 10 min |
| Baby DUCC | 120 | 32–41 | Resuscitation if needed | Immediate cord clamping (duration not specified) | Until 1 minute after CO2 detector change or 5 min | Heart Rate at 60 and 120 s |
| ABC2 | 660 | 24–31 | Resuscitation if needed | 30–60 s | Until stable (approx. 4 min) | Intact Survival (survival without grade 2 ivh or nec) |
| Nevill and Meyers | 120 | 23–31 | Start CPAP and or PPV at 15 s until 60 s | 60 s | 60 s | Need for blood transfusion |
| PCI-Trial | 202 | 23–29 | Resuscitation if needed | Intact cord milking × 4 | 3 min | composite outcome of severe IVH, chronic lung disease or death |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katheria, A.C. Neonatal Resuscitation with an Intact Cord: Current and Ongoing Trials. Children 2019, 6, 60. https://0-doi-org.brum.beds.ac.uk/10.3390/children6040060
Katheria AC. Neonatal Resuscitation with an Intact Cord: Current and Ongoing Trials. Children. 2019; 6(4):60. https://0-doi-org.brum.beds.ac.uk/10.3390/children6040060
Chicago/Turabian StyleKatheria, Anup C. 2019. "Neonatal Resuscitation with an Intact Cord: Current and Ongoing Trials" Children 6, no. 4: 60. https://0-doi-org.brum.beds.ac.uk/10.3390/children6040060