1. Introduction
When the author was named as Interim Director of Pediatric Echocardiography Laboratory at Children’s Memorial Hermann Hospital/University of Texas-Houston Medical School, Houston, Texas in 2006, some of the staff critiqued this appointment, as the author was considered to be an interventionist pediatric cardiologist. The author responded to this critique by sending them a list of the his echo publications [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33]. It may be worthwhile reviewing the author’s professional echocardiography experience.
At the time of the author’s fellowship training in 1969/1970 at Stanford University Medical Center, Palo Alto, California, there were only two echocardiography recording machines in the United States: one was at University of Indiana, Indianapolis, Indiana and the other at Stanford University. The author was exposed to echocardiography to evaluate mitral valve motion and pericardial effusion on M-mode tracings. During subsequent fellowship training at Case-Western Reserve University and the University of California at Los Angeles, the echo machines had not yet arrived at the respective institutions. By 1972, when the author joined the Faculty at the Medical College of Georgia, Augusta, Georgia, there were indeed echocardiography facilities at that institution. Shortly thereafter, Dr. Wesley Covitz (who was trained with Richard Meyer, one of the premier pediatric echocardiographers of that time) joined our faculty at Georgia and provided the author with additional understanding of the principles and practice of M-mode echocardiography, thereby adding to the author’s knowledge base. This resulted in the author’s active participation in echocardiography research at that time [
1,
2,
3,
4,
5]. Two-dimensional (2D) echocardiography was coming in to vogue as the author was leaving Medical College of Georgia to take a position at the King Faisal Specialist Hospital & Research Center in Riyadh, Saudi Arabia. There were portable echocardiography machines (Apagee) at that institution which the author could use in a clinic setting and perform 2D studies of children following their formal evaluations by history, physical examination, electrocardiogram (ECG) and chest x-ray (norms at that time). This provided the author with experience and expertise to teach sonographers and other trainees. As the author gained expertise in 2D, suddenly, Doppler echocardiography surfaced. The author had to learn this modality as well. Then, as the author was leaving Riyadh to join the Faculty at University of Wisconsin, Madison, Wisconsin, the color Doppler technique was introduced, which again, the author had to learn. In this review, the author’s contributions to the echocardiography literature will be discussed.
2. Estimation of Left-to-Right Shunt in Isolated Ventricular Septal Defects by Echocardiography
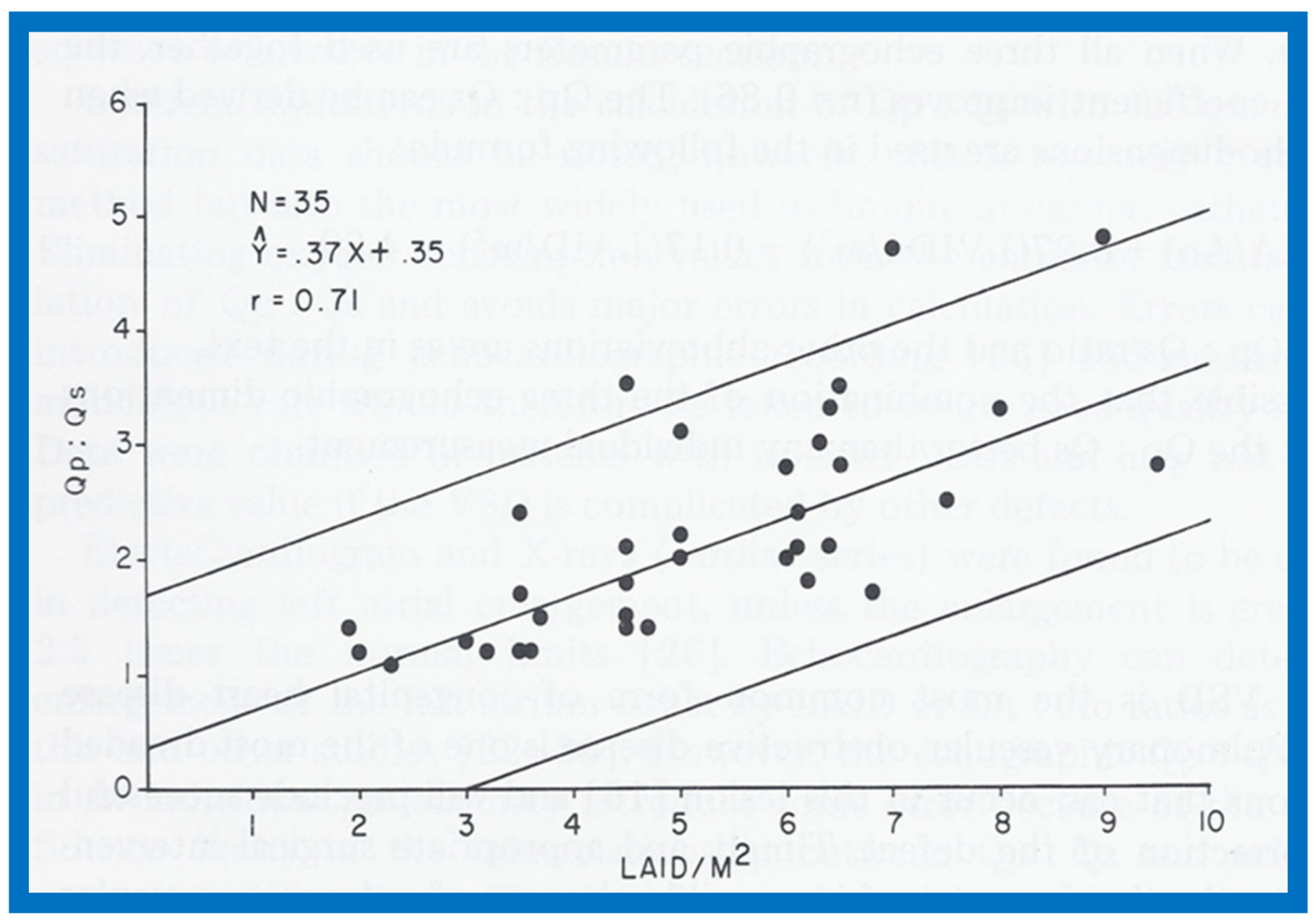
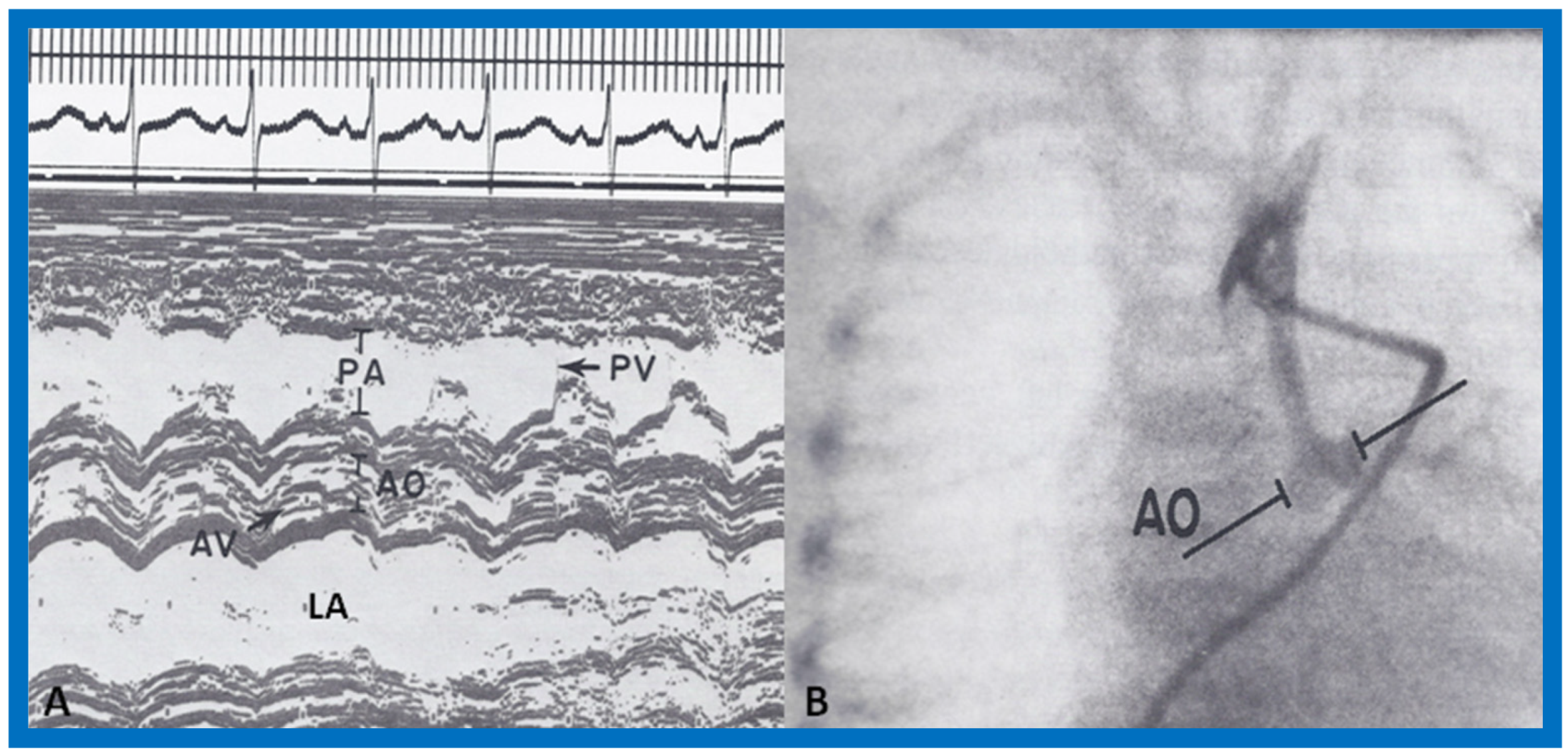
In the mid-1970s, in an attempt to noninvasively quantify the degree of left-to-right shunt in infants and children with isolated ventricular septal defects (VSDs), we compared the cardiac catheterization data with echocardiographic values (echo performed within 24 h of cardiac catheterization) in 35 babies; 35 children with normal hearts by physical examination and ECG were used as controls [
1]. The size of the left atrium (LA), the LA to aortic root (Ao) ratio and the size of the left ventricle (LV) in the VSD group were larger (
p < 0.01) than those of control subjects (for actual values, see Table I of [
1]). In the VSD group, the echo values were increased in proportion to the catheterization-measured pulmonary to systemic flow ratio (Qp:Qs), with r values ranging from 0.71 to 0.73 (
Figure 1,
Figure 2 and
Figure 3). In addition, Qp:Qs greater than 2:1 was always present with a LA:Ao ratio larger than 1.4:1. It was found that the combination of these echo parameters resulted in better predictions of Qp:Qs than any of the echo parameters used alone.
We concluded that the echocardiographic technique is useful in estimating Qp:Qs and in the clinical assessment of patients with isolated VSD [
1]. The author is pleased that these observations remain valid, even more than 40 years after the publication of our study, and the addition of 2D and Doppler studies have increased the value of echocardiography in the assessment of VSD patients so that cardiac catheterization and angiography is rarely required prior to surgery at the present time.
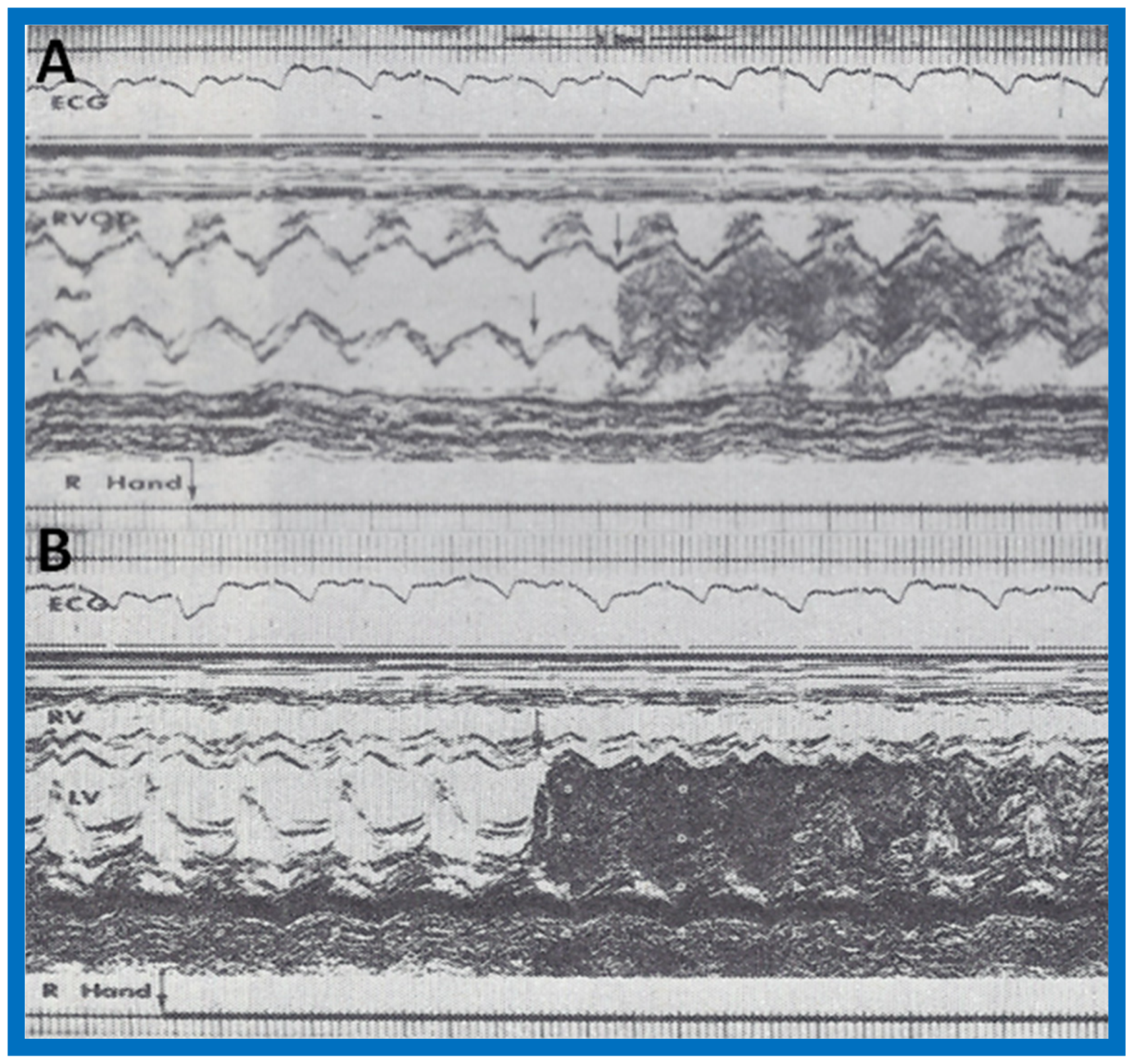
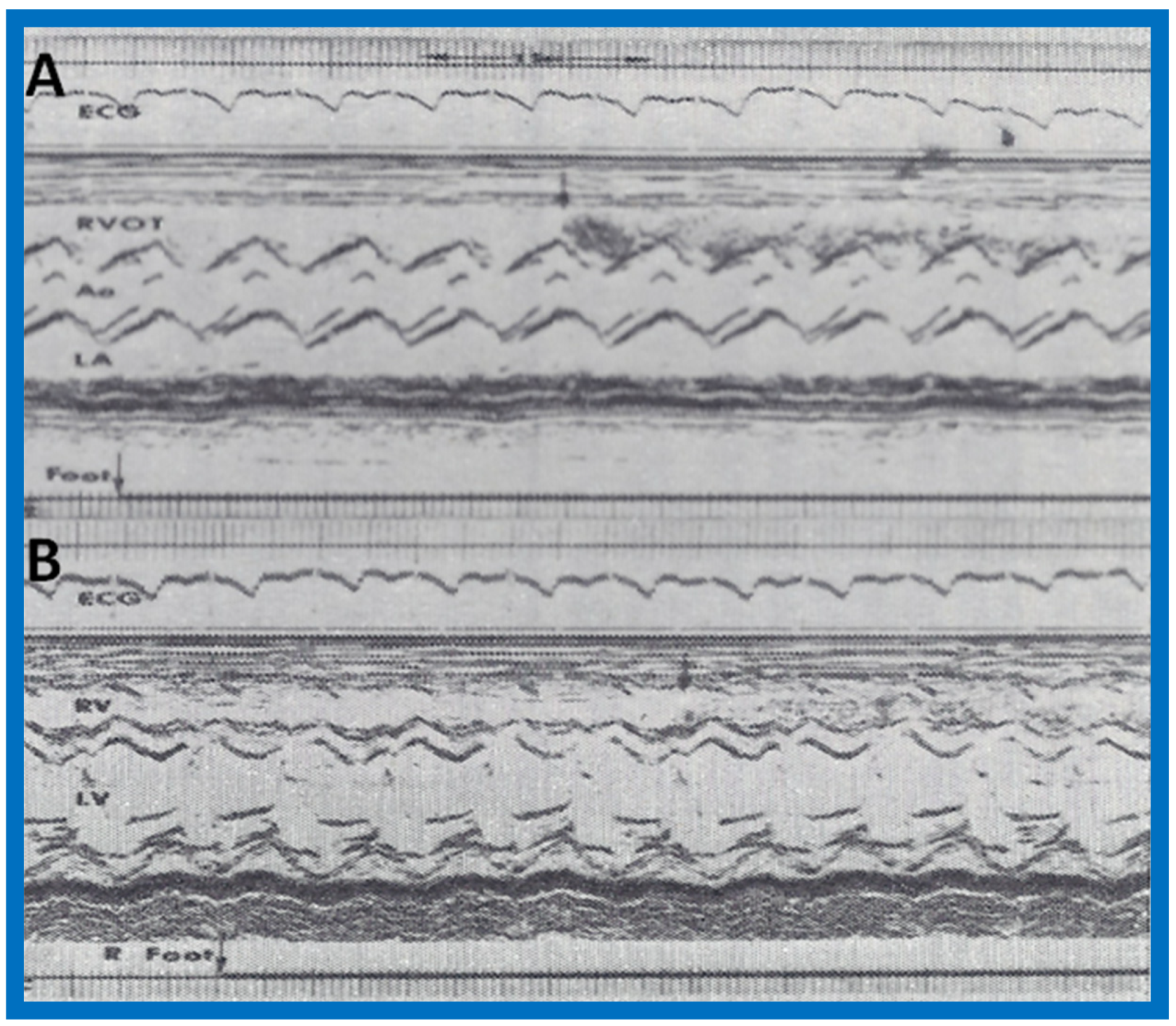
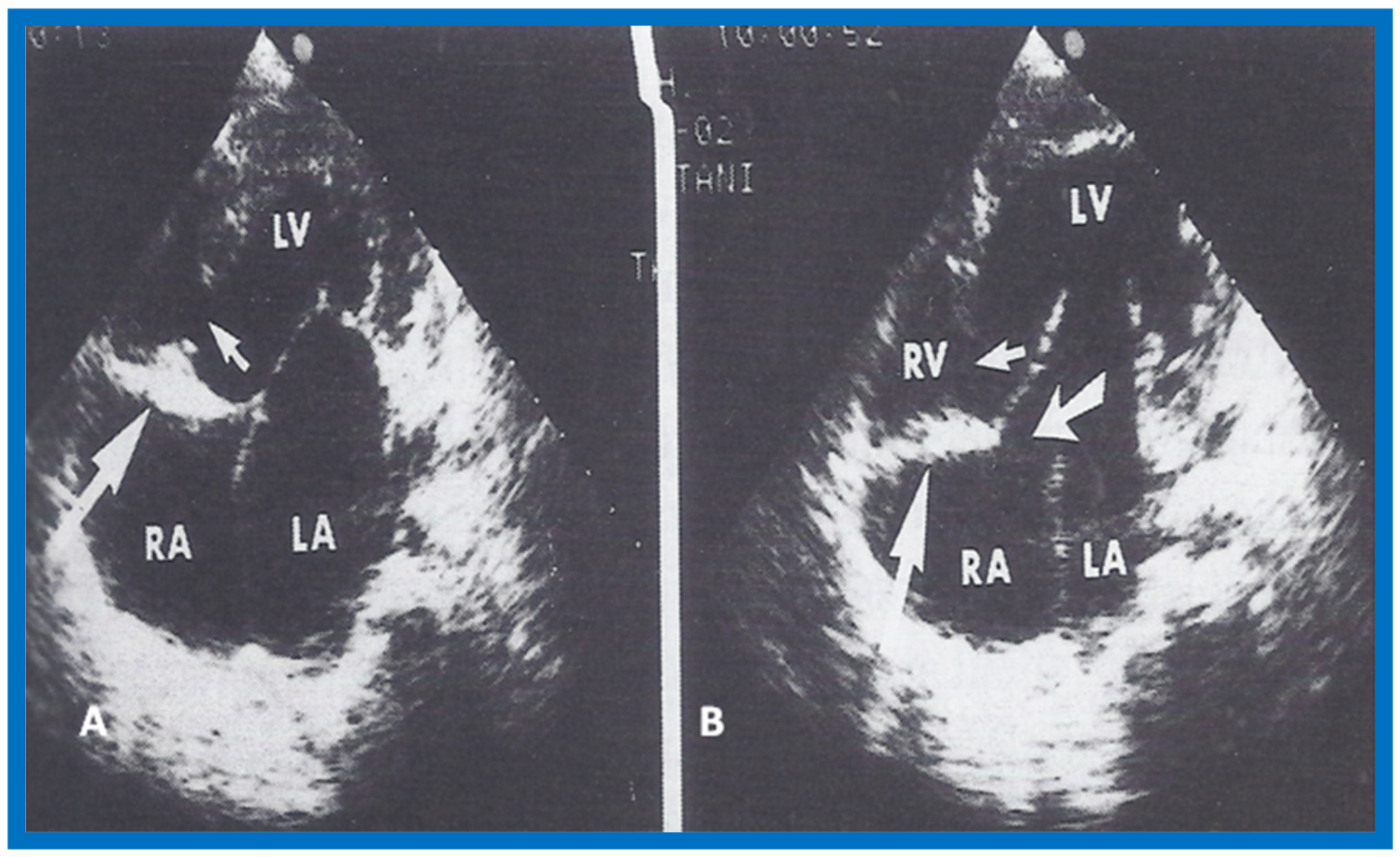
3. Contrast Echocardiography in the Diagnosis of Anomalous Connection of the Right Superior Vena Cava to the Left Atrium
An infant without abnormal cardiac findings other than cyanosis was studied by contrast echocardiography (by injection of agitated saline) and an anomalous systemic venous connection to the left atrium was suspected [
2]. A moderate degree of cyanosis was noted by the pediatrician at 4 months of age and the baby was referred to the author for cardiac evaluation. Arterial blood gas analysis revealed a PO
2 of 31 torr in room air, confirming the clinical finding of cyanosis. The PO
2 did not increase following the administration of 100% oxygen for 15 min. Physical examination did not reveal any other abnormalities. The electrocardiogram (ECG) was normal, as was her M-mode echocardiogram. Agitated saline injection into a vein on the dorsum of each hand resulted in opacification of the left atrium, left ventricle and aorta (
Figure 4A,B) without visualization of the right heart structures, suggesting anomalous drainage of the superior vena cava into the left atrium. Injection into a vein in the right foot resulted in opacification of the right heart without visualization of the left heart (
Figure 5A,B), suggesting normal drainage of the inferior vena cava into the right atrium.
At the age of 8 months, cardiac catheterization with selective cineangiography was performed. The left atrium (LA) was catheterized via a tight patent foramen ovale, and the catheter was advanced from the LA into the superior vena cava (SVC) and into both right and left innominate veins. The right heart saturations were low (60–62%) without any evidence for a step up. The pulmonary venous saturations were normal (98%) with a step down in the left atrium and left ventricle (79%). The pressures in all cardiac chambers were normal (See Table 1 of [
2]). Selective cineangiography into the right (
Figure 6A,B) and left (
Figure 6C) innominate veins confirmed the diagnosis of anomalous connection of the right SVC to the LA. No persistent left SVC was identified. Because of a lack of other symptoms and only mild polycythemia (hemoglobin of 15 gm%), surgical correction was deferred at that time with a plan for surgery at a later date.
An extensive review of the literature revealed only four published cases of anomalous connection of the right SVC to the LA as of the time of our review [
2]. Ages at diagnosis were 2 to 34 years, with our subject being 8 months-old. All of them presented with cyanosis and diagnosis was made by angiography, except for our case, which was initially diagnosed by contrast echocardiography and later confirmed by angiography. The differential diagnosis of cyanosis (and arterial desaturation) without any other abnormal cardiac findings includes pulmonary arteriovenous fistula, connection of pulmonary artery to the LA and of course anomalous systemic venous connection to the left atrium. In pulmonary arteriovenous fistula and connection of pulmonary artery to the LA, the contrast would first appear in the right ventricle before the LA, LV and Ao. In addition, differential contrast patterns at the site of injection into the veins of the upper and lower extremities should not be present with pulmonary artriovenous fistula and connection of pulmonary artery to the LA. The associated discussion also included a review of the possible embryological origin of anomalous systemic venous connection to the left atrium [
2].
At the age of twenty-six months, surgical repair was performed under cardiopulmonary bypass, as described in
Figure 7 [
3]. Repeat contrast study following surgical correction showed opacification of right heart structures without contrast detected in the left heart after injection of agitated saline into the arm veins (
Figure 8), indicating the positive outcome of the surgery [
3]. The discussion focused on methods of surgical repair performed in the other three cases reported prior to our report and the usefulness of contrast echocardiography in diagnosing several types of congenital heart defects [
3].
In an editorial communication published later [
34], apart from a discussion of the lack of gender predilection for the prevalence of this rare anomaly, the differential diagnosis of cyanosis without any other abnormal cardiac findings with the use of noninvasive contrast echo studies, surgery to treat this anomaly and postoperative evaluation, we presented another noninvasive method to diagnose this condition, namely first pass radionuclide angiographic study (
Figure 9).
5. Reviews: Echocardiographic Evaluation of Left Ventricular Function
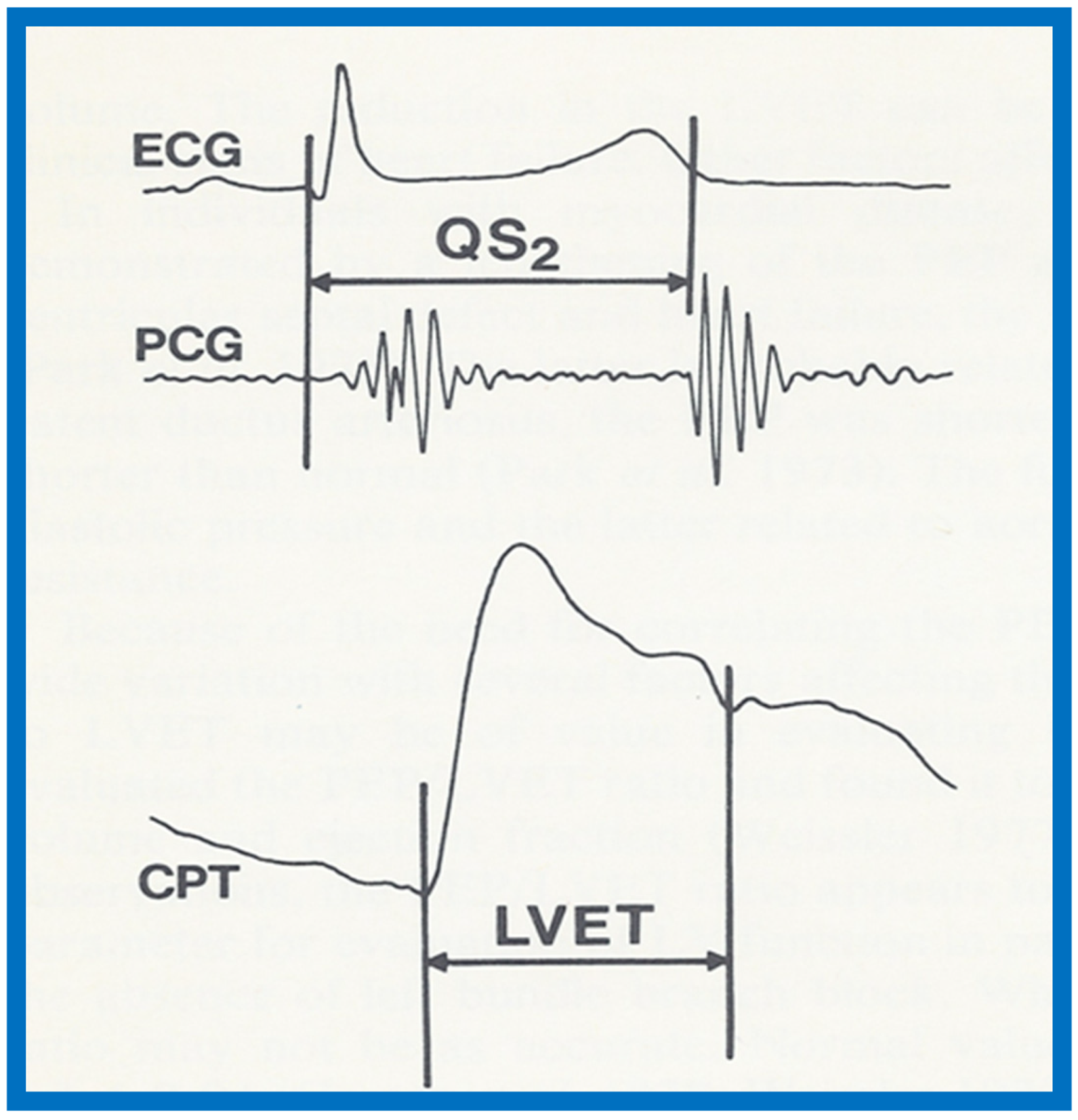
We reviewed echocardiographic evaluations of the left ventricular function in two papers in early 1980s [
5,
6]. We began with a review of determinants of ventricular function, namely, preload or ventricular end-diastolic volume, contractile state of the myocardium, which is the innate force of the myocardial contraction and is independent of the load on the ventricle and afterload, or intraventricular systolic tension during ventricular ejection. Then, it was proposed that ventricular functional abnormalities in children could be grouped into four major pathophysiologic categories: 1. Volume overloading of the ventricle, as seen in ventricular septal defect, patent ductus arteriosus and mitral and aortic insufficiency; 2. Pressure overloading, as seen in aortic stenosis and systemic hypertension; 3. Ventricular under loading, as seen in mitral stenosis and pericardial tamponade; and 4. Primary disturbance of the contractile state of the myocardium, as seen in cardiomyopathy.
We presented the methods of measurements/calculations of systolic time intervals (
Figure 11 and
Figure 12), left ventricular volumes, LV shortening fraction (
Figure 13), LV velocity of circumferential fiber shortening (Vcf), percent thickening of the LV posterior wall (
Table 1) and their utility in the evaluation of LV function. This was followed by a discussion of diastolic function of the LV, other indices of LV function, LV function in aortic stenosis, LV function in LV volume overloading conditions and congestive cardiomyopathy. Then, newer methods (as of early 1980s) of assessing LV function by two-dimensional echocardiography, Doppler ultrasound-measured aortic blood flow velocity and radio-nuclide ejection fraction were briefed. The papers were concluded by outlining the value and limitations of noninvasive technology, as they were at that time [
5,
6].
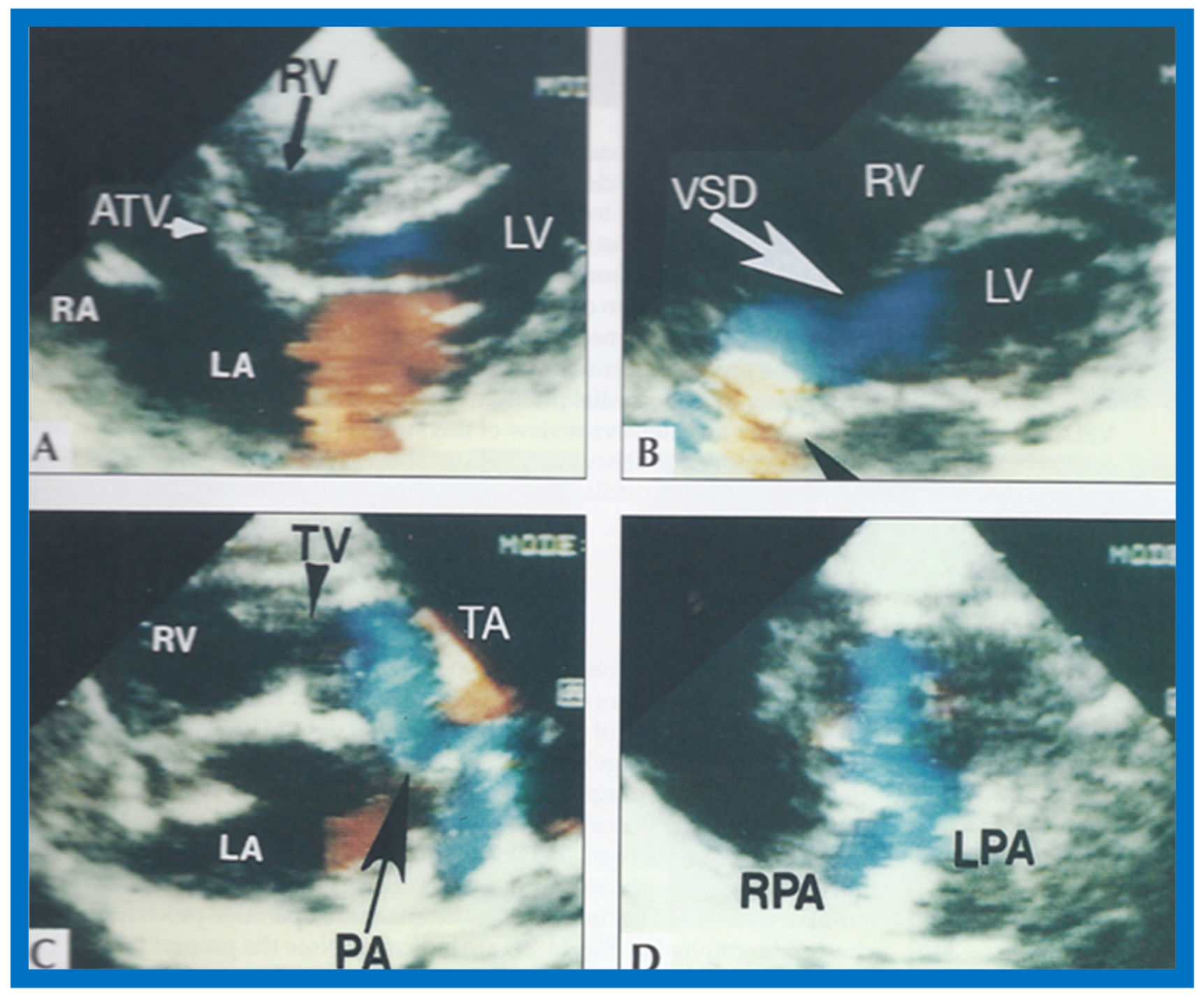
6. Echocardiographic Features of Tricuspid Atresia
The M-mode and two-dimensional echocardiographic features of tricuspid atresia were discussed in the author’s first book on tricuspid atresia, written in collaboration with his colleague, Dr Wesley Covitz at the Medical College of Georgia [
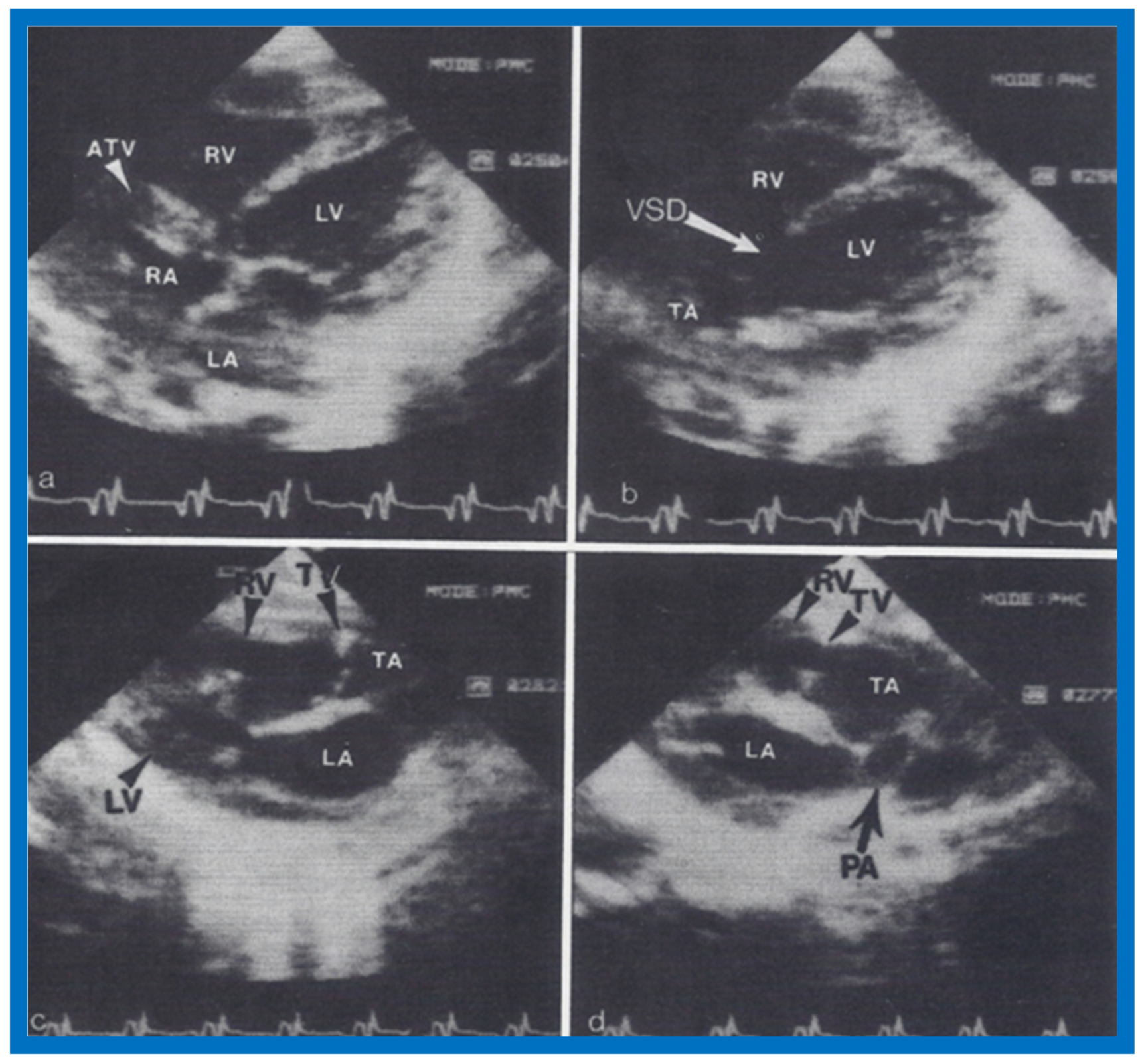
7]. The two-dimensional (2D) echocardiographic pictures in 1982 were crude (
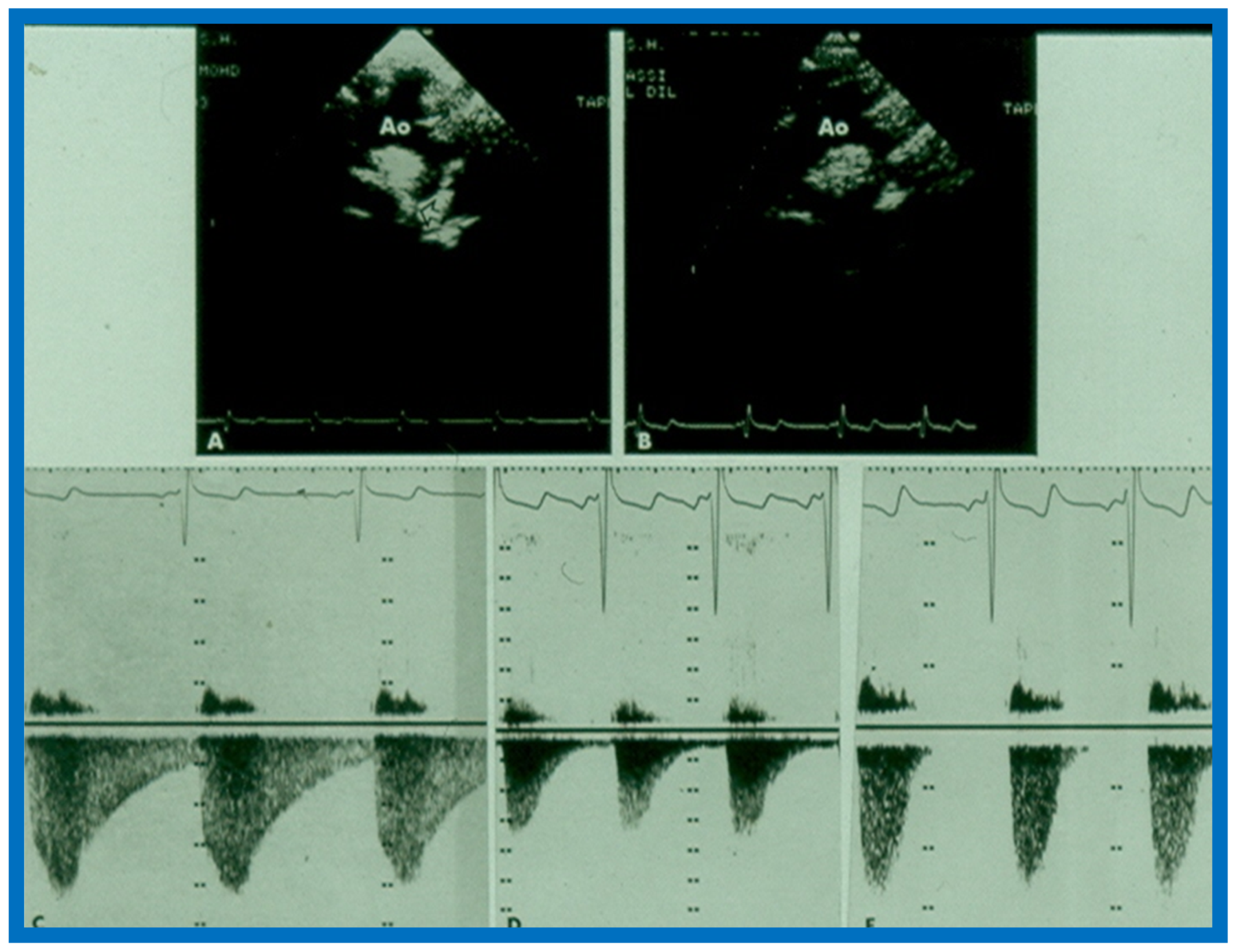
Figure 14) [
7]; however, they represented the state of the art echocardiography machines of that time.
More recently, the author reviewed the echo-Doppler evaluation of tricuspid atresia [
37,
38,
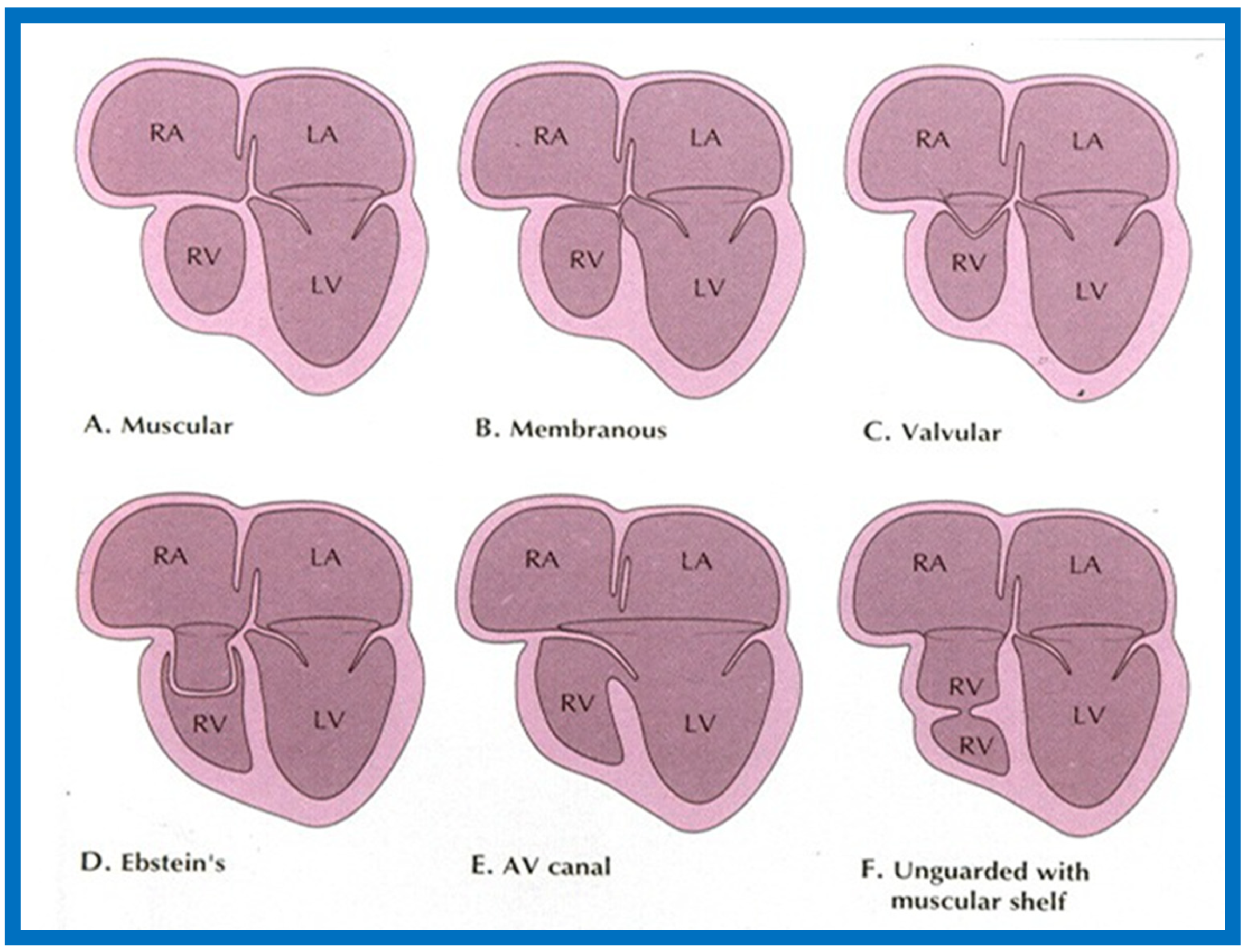
39]; these findings will be presented. M-mode echocardiography, while not diagnostic, is useful for evaluating the size of the left atrium (LA) and left ventricle (LV) and LV function. On 2D echocardiography, the atretic tricuspid valve is visualized directly as a dense band of echoes at the site where the tricuspid valve should be in the most frequent muscular type, as shown in
Figure 14,
Figure 15,
Figure 16 and
Figure 17. This anatomy is better demonstrated in apical and subcostal four-chamber views than in other views. The other types, namely membranous, valvular, Ebstein’s, atrioventricular septal and unguarded valve with muscular shelf (
Figure 18) [
40], are rare and may also be recognized on 2D echocardiography.
Following the demonstration of the atretic tricuspid valve, the sizes of the cardiac chambers were evaluated both by M-mode (Z scores) and 2D echocardiography; enlarged RA, LA and LV, and a small RV, were seen (
Figure 14,
Figure 15,
Figure 16 and
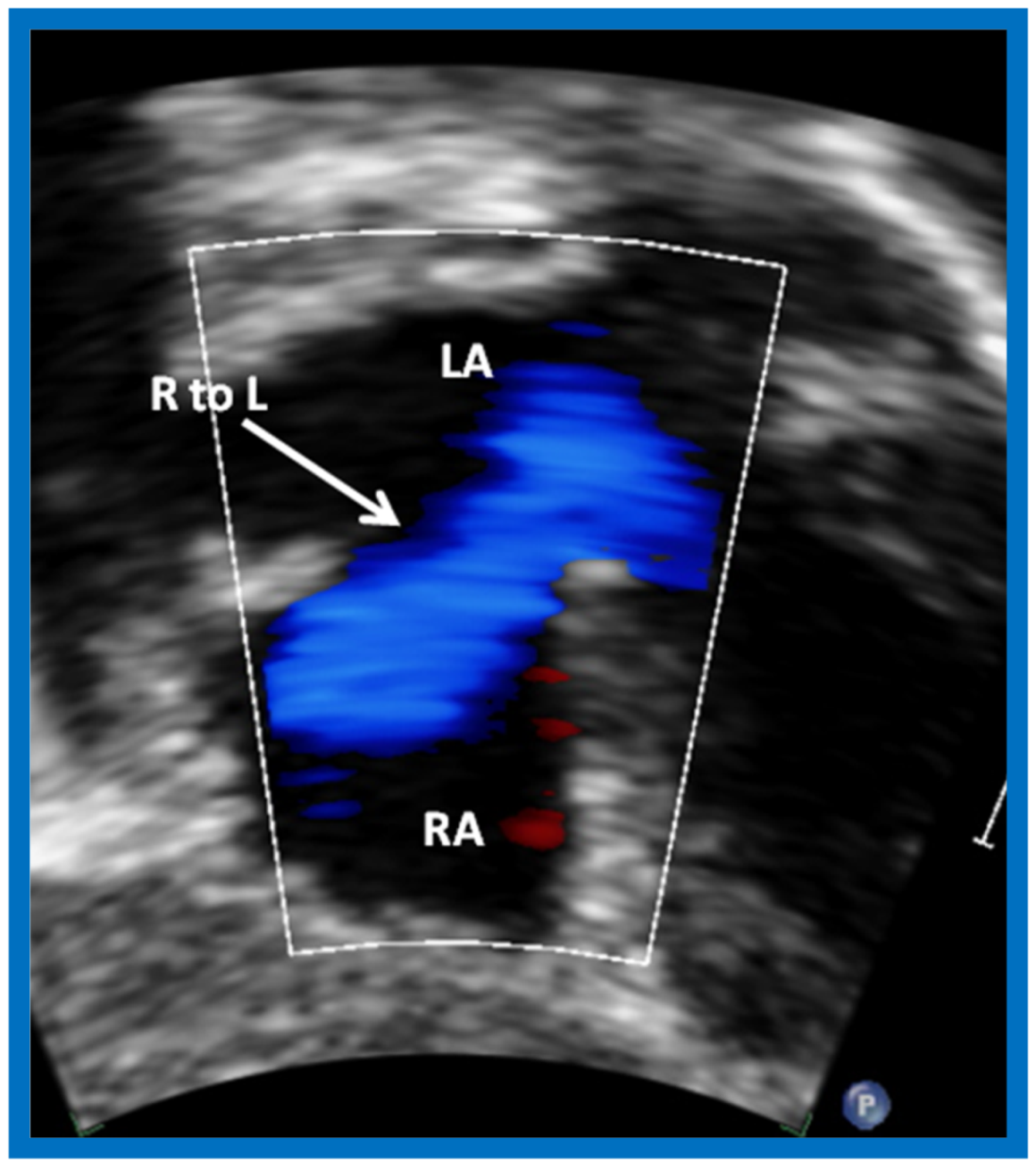
Figure 17). Pulsed (not shown) and color Doppler (
Figure 19) studies were helpful in illustrating the right-to-left shunt across the patent foramen ovale or atrial septal defect. Contrast study using agitated saline with 2D imaging clearly demonstrated successive opacification of the RA, LA, LV and then the RV in that order, but such a study is not necessary for diagnosis.
The relationship of the great arteries is examined next in order to classify them into various types [
41]. The relationship of the great arteries is established by following the vessels arising from the ventricles until pulmonary bifurcation or aortic arch. In Type I patients with normally related great arteries, the aorta arises from the LV (
Figure 20), while in Type II patients with transposition of the great arteries, the PA arises from the LV (
Figure 21 and
Figure 22). In Type III patients, it may be little more difficult to assign the great artery relationship, and sometimes angiography is needed. In type IV with truncus arteriosus, the limited data [
22] suggest that this can be done by echocardiography (
Figure 23 and
Figure 24).
Further subdividing into subtypes a (pulmonary atresia), b (pulmonary stenosis or hypoplasia), and c (normal pulmonary arteries) is done by examining the pulmonary arteries irrespective of type.
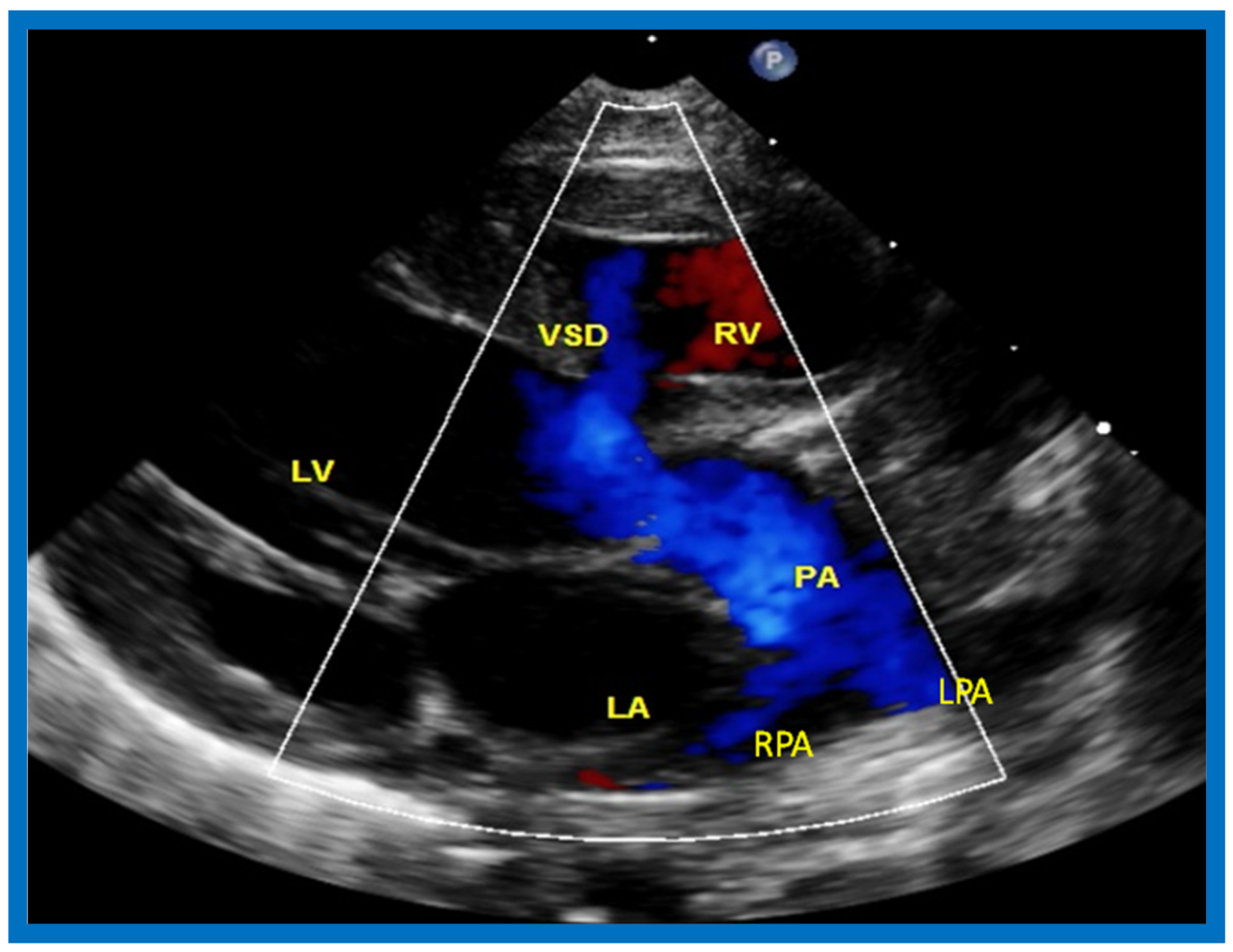
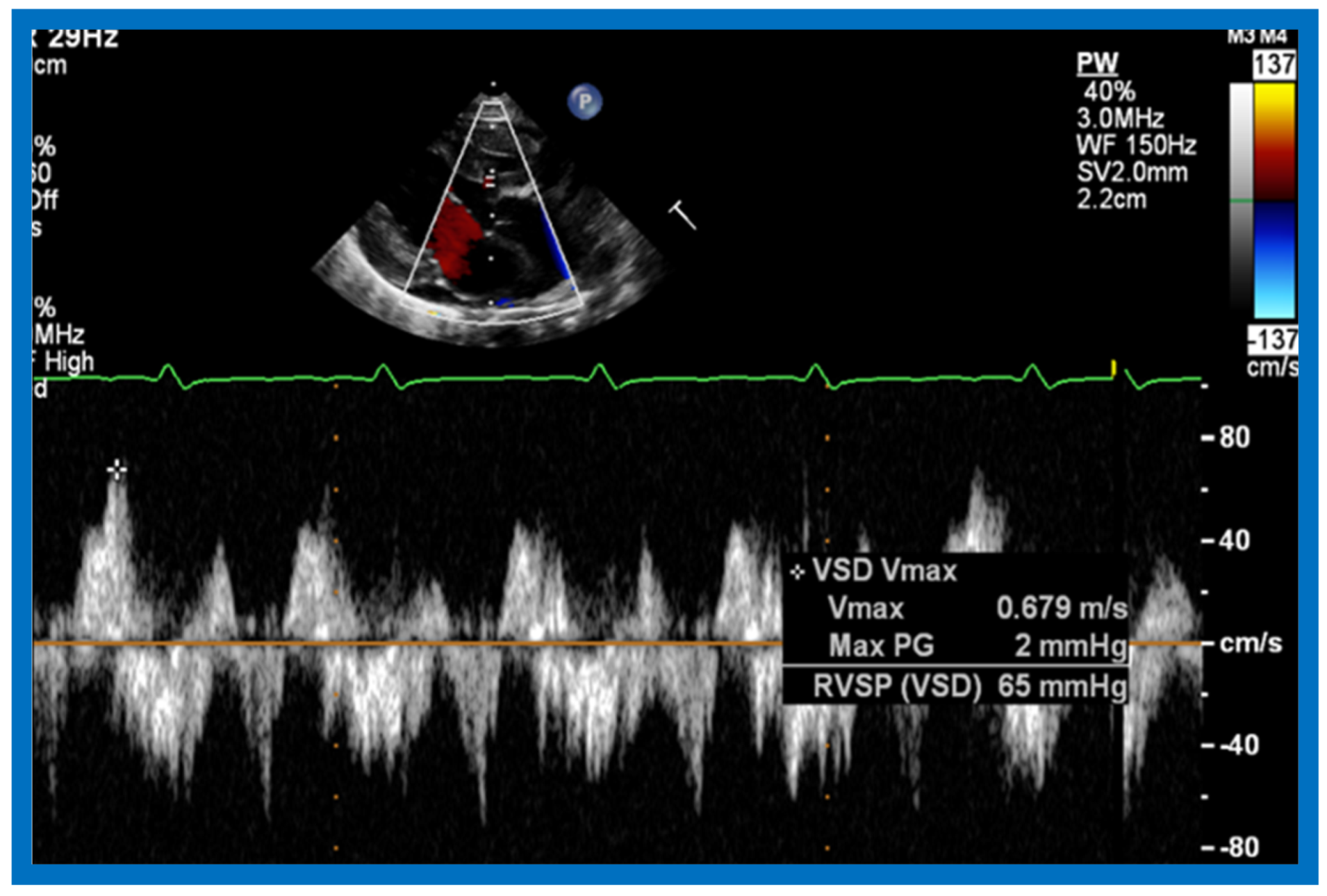
Then, the ventricular septum is evaluated; the ventricular septum is intact in most Type Ia cases. In children with Type I (normally related great arteries), the VSD supplies pulmonary blood flow (
Figure 20) while in patients with Type II (transposition the great arteries), the VSD allows blood to flow into the systemic circuit (
Figure 21 and
Figure 22). In Type I patients, the VSD is demonstrated by 2D (
Figure 20A) and the left to-right shunt across it by color (
Figure 20B), pulsed and CW (
Figure 20C) Doppler signals. Interrogation of the right ventricular outflow tract and pulmonary artery region is performed; peak Doppler flow velocity across the right ventricular outflow tract and pulmonary valve is helpful in identifying obstruction across these sites. The Doppler data from the VSD and RVOT are also helpful in estimating of pulmonary artery pressures. In these Type I babies, the 2D size of the VSD and the peak Doppler flow velocity across it are useful in quantifying the size of the VSD (
Figure 20); the higher the VSD Doppler velocity, the smaller the defect. However, in patients with pulmonary hypertension, severe infundibular or valvar pulmonary stenosis, the VSD Doppler velocities do not reflect the size of the VSD. Barring these exceptions, right ventricular and pulmonary arterial pressure may be estimated using modified Bernoulli equation (RV/PA systolic pressure = systolic BP − 4V
2).
In Type II patients, the VSD may be small, causing obstruction to blood flow to the systemic circuit; therefore, the size of the VSD should be ascertained by 2D (
Figure 21 and
Figure 22), color Doppler (
Figure 22), pulsed (
Figure 25) and CW Doppler, as necessary. In these Type II patients, the high VSD velocity is indicative of subaortic obstruction. Interrogation of left ventricular outflow and PA region may reveal pulmonary or subpulmonary stenosis; the higher the velocity, the more severe the obstruction. Study from suprasternal notch may show aortic coarctation (
Figure 26), which is not uncommon in patients with the Type II anatomy.
A large number of other cardiac defects are known to be associated with tricuspid atresia [
37,
38]. Consequently, echo-Doppler studies should scrutinize for these defects during such studies.
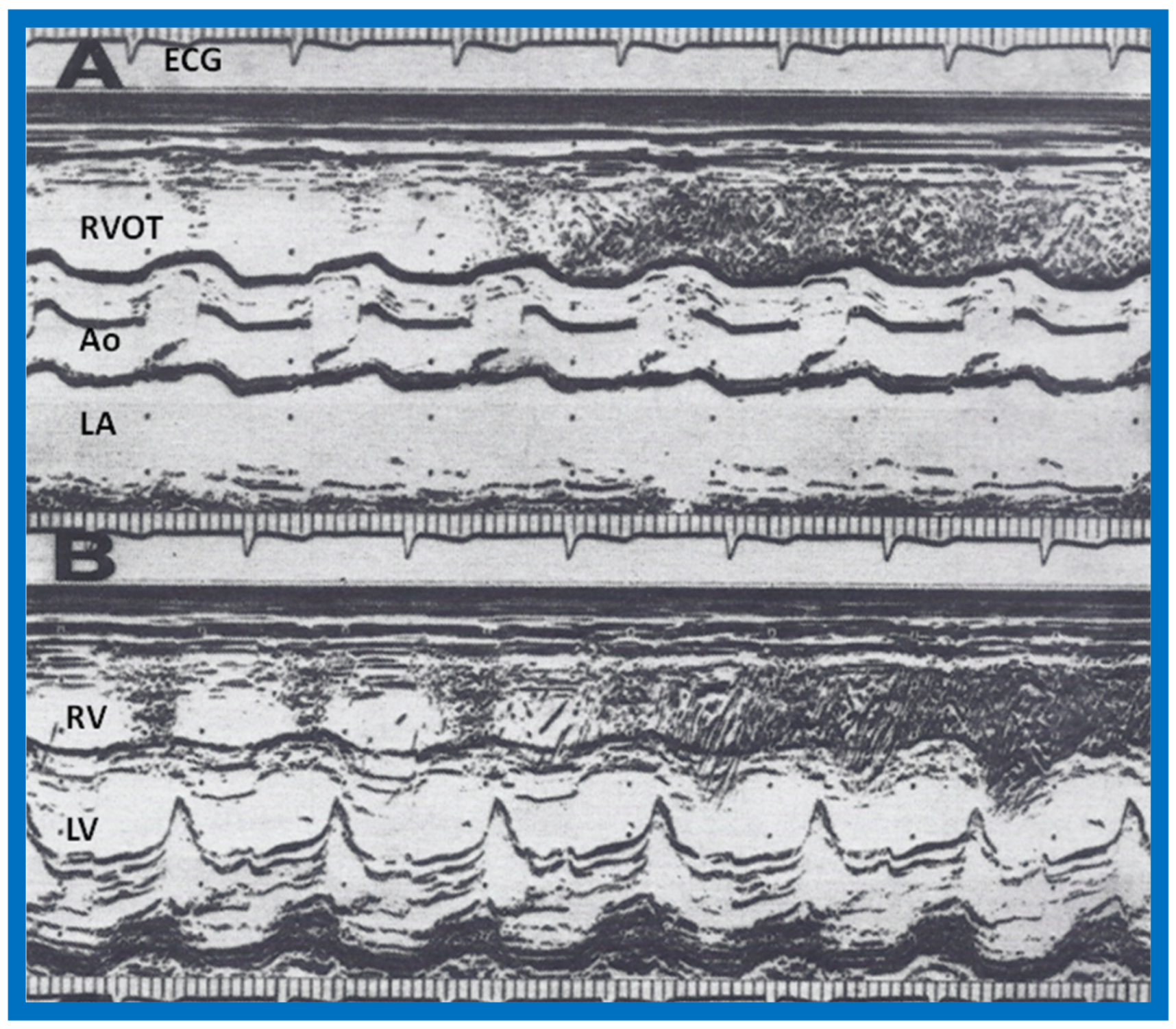
7. Contrast Echocardiography in the Evaluation of Hypoxemia Following Open Heart Surgery
We have used contrast echocardiography in other situations as well [
8]. A three-year-old child had surgical correction of tetralogy of Fallot by patch closure of the VSD, resection of infundibular muscle and relief of valvar obstruction by a transannular pericardial patch. Following surgery, the child maintained good perfusion and normal vital signs, but had marked hypoxemia. Arterial PO
2 was around 30 torr with O
2 saturations in the mid 50s without any change in 100% O
2. No cardiac murmurs were heard, and on the chest X-ray, no pulmonary pathology was identified. Since the foramen ovale was not closed during surgery, it was thought that patent foramen ovale (PFO) may be the reason for the hypoxemia. Contrast echocardiography was performed to confirm PFO as the site of right-to-left shunt. M-mode recordings from the parasternal short axis view of the LA, Ao, and right ventricular outflow tract (RVO) were made while injecting agitated saline into the right atrial line. This revealed the almost simultaneous appearance of contrast echoes in the Ao and RVO without opacification of the LA (
Figure 27), suggesting that there was no interatrial shunt, and that the shunt was distal to the atria. A similar contrast study while recording the LV and right ventricle (RV) demonstrated the almost simultaneous appearance of contrast echoes in both the LV and the RV (
Figure 28), indicating that that the right-to-left shunt was at the ventricular level.
The patient was returned to the operating room and, upon inspection of the ventricular septum via right atriotomy, a second VSD was noted adjacent to previously closed VSD, separated by a muscle bundle. The defect was closed with another Dacron patch. The PFO was also closed with sutures. The PO2 and O2 saturation improved. Repeat contrast echo study did not reveal any evidence of right-to-left shunt.
Other investigators used contrast echocardiography to demonstrate residual postoperative shunts, as reviewed in our paper [
8], and our report further demonstrates the usefulness of this technique in evaluating postoperative residual shunts. We concluded that this technique is useful in identifying and localizing shunts in postoperative patients [
8].
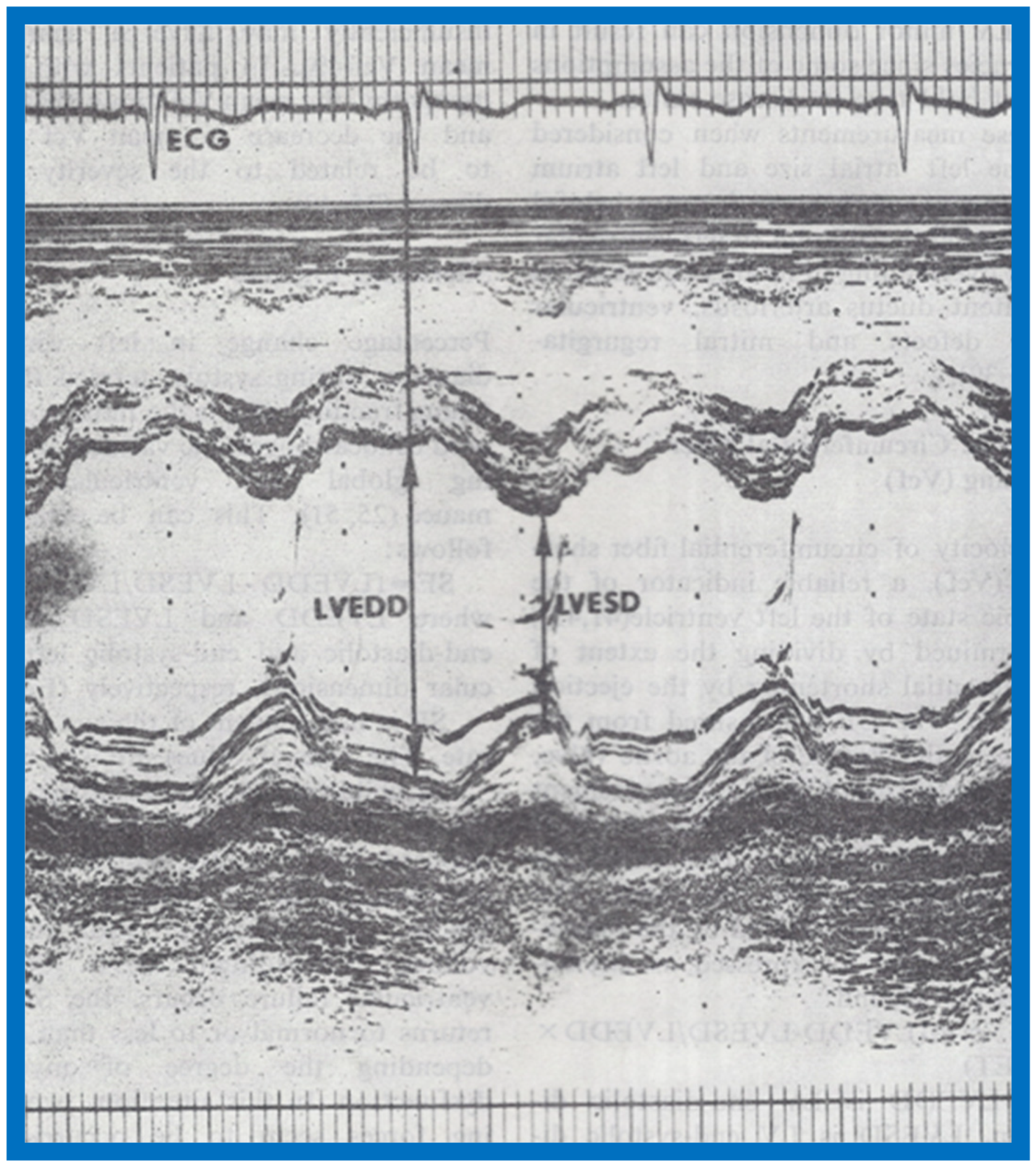
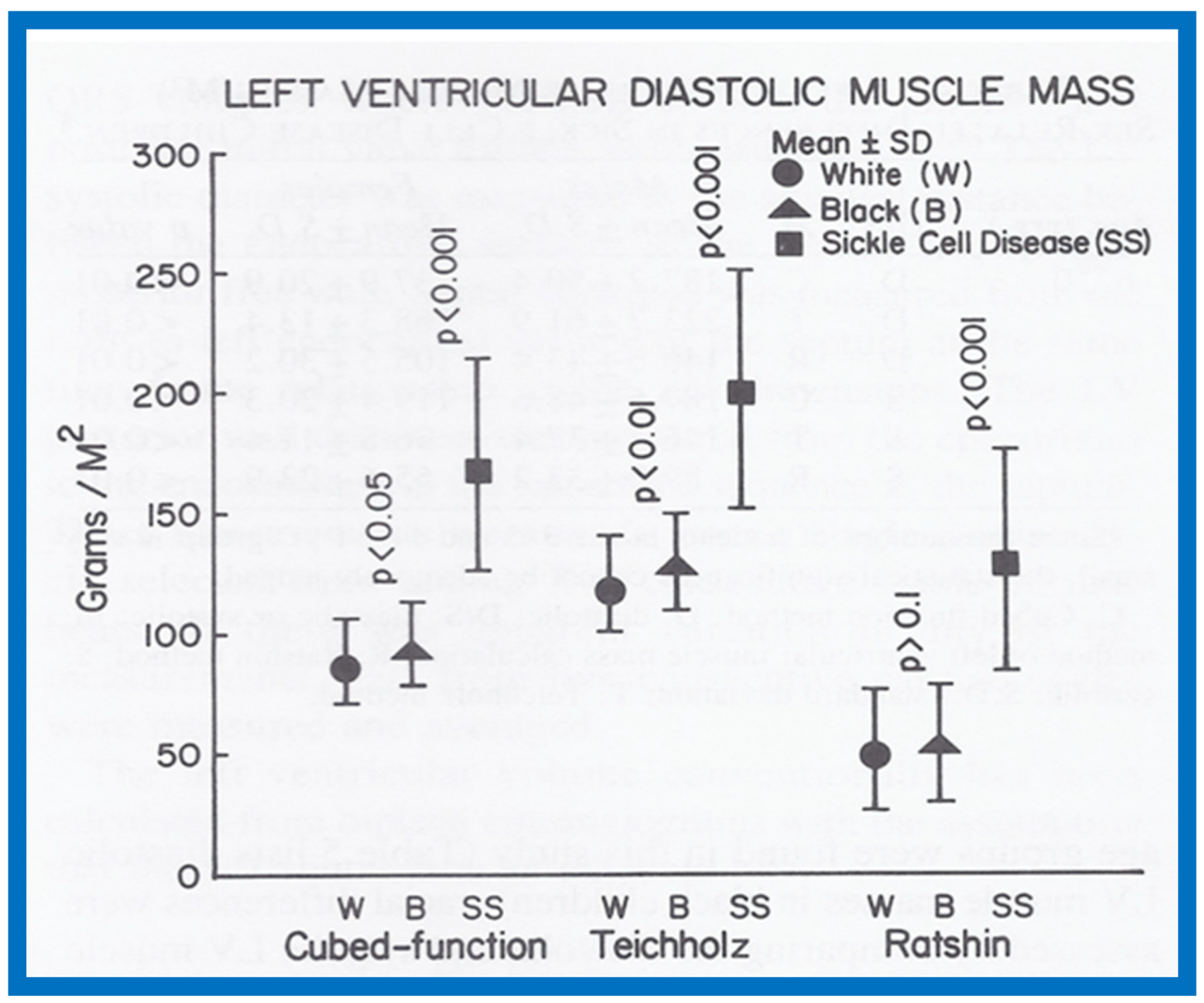
8. Quantitation of Left Ventricular Muscle Mass by M-Mode Echocardiography in Children
While there have been several studies on LV muscle mass (LVMM) by echocardiography in adult subjects, there had only been a limited number on echocardiographic measurements of the LVMM in children as of the early 1980s. The purpose of our investigation [
9] was to establish normal echocardiographic LVMM in children, to identify sex- and race-related variation in LVMM, to establish if this measurement is sensitive to detect increased LVMM in children with sickle cell disease and to find the most appropriate method (from among the 3 available methods at that time) for calculating the LVMM in children. These data were presented in part at the VIII World Congress of Cardiology, Tokyo, Japan, in September 1978 [
42].
We studied 204 normal children, aged 3-17 years; 107 were white and 97 black. The children were divided into 3 to 5, 6 to 10, 11 to 14 and 15 to 17 year age groups. The study subjects also included 47 children with sickle cell disease; 28 were boys and 19 were girls. All normal children were examined by one of the investigators; their normalcy was confirmed by physical examination and by ECG. Children with sickle cell disease had SS hemoglobin on hemoglobin electrophoresis, confirming their diagnoses. Weight, height, blood pressure, chest circumference and the antero-posterior diameter of the chest were measured in all children, as was their hemoglobin. Standard M-mode recordings from the parasternal short axis view of the left ventricle at the tips of the mitral valve were obtained, and measurements of LV end-diastolic (LVEDD) and end-systolic (LVESD) dimensions, as well as LV posterior wall and ventricular septal thickness in diastole and systole, were made in a standard fashion. The LVMM was calculated by three different methods, namely the cubed-function method and the methods described by Teichholtz and by Ratshin [
9].
The results were presented in nine tables and three figures [
9]. There were no gender-related differences in LVMM. There was also no significant difference in LVMM normalized to body surface area (g/M
2) between the various age groups. Consequently, the LVMM data of all ages were combined, but were separated for the normal black and white children. The diastolic LVMM was higher (
p < 0.05 to < 0.01) in black (96 ± 17 g/M
2) than in white (89 ± 18 g/M
2) children (
Figure 29). Racial differences in systolic LVMM were less marked (
Figure 30). The age distribution, weight, height, systolic and diastolic blood pressures, chest circumference and antero-posterior diameter of the chest were similar (
p > 0.05 to
p > 0.1) between black and white children, and were unlikely to have been responsible for LVMM differences. However, the hemoglobin was lower (
p < 0.05 to < 0.01) in black than in white children, which may have explained their higher LVMM.
Both the diastolic (170 ± 44 g/M
2) and systolic (163 ± 44 g/M
2) LVMMs were higher (
p < 0.001) in sickle cell disease children than those without (
Figure 29 and
Figure 30). The weight, height, body surface area, chest circumference and antero-posterior diameter of the chest and blood pressures were similar (
p > 0.05 to > 0.1) in sickle cell disease vs. non sickle cell disease children. The causes for this increase may be related to chronic anemia producing augmented stroke volume and cardiac output with consequent LV hypertrophy similar to that seen thalassemia. The occlusion of coronary microcirculation by sickled red blood cells may be an additional factor. Among sickle cell disease children, the LVMM was larger (
p < 0.05 to < 0.01) in boys than in girls. The reason for this is not clear, but may be related to differences in inappropriate response to anemia or incidence of sickling in the coronary circulation.
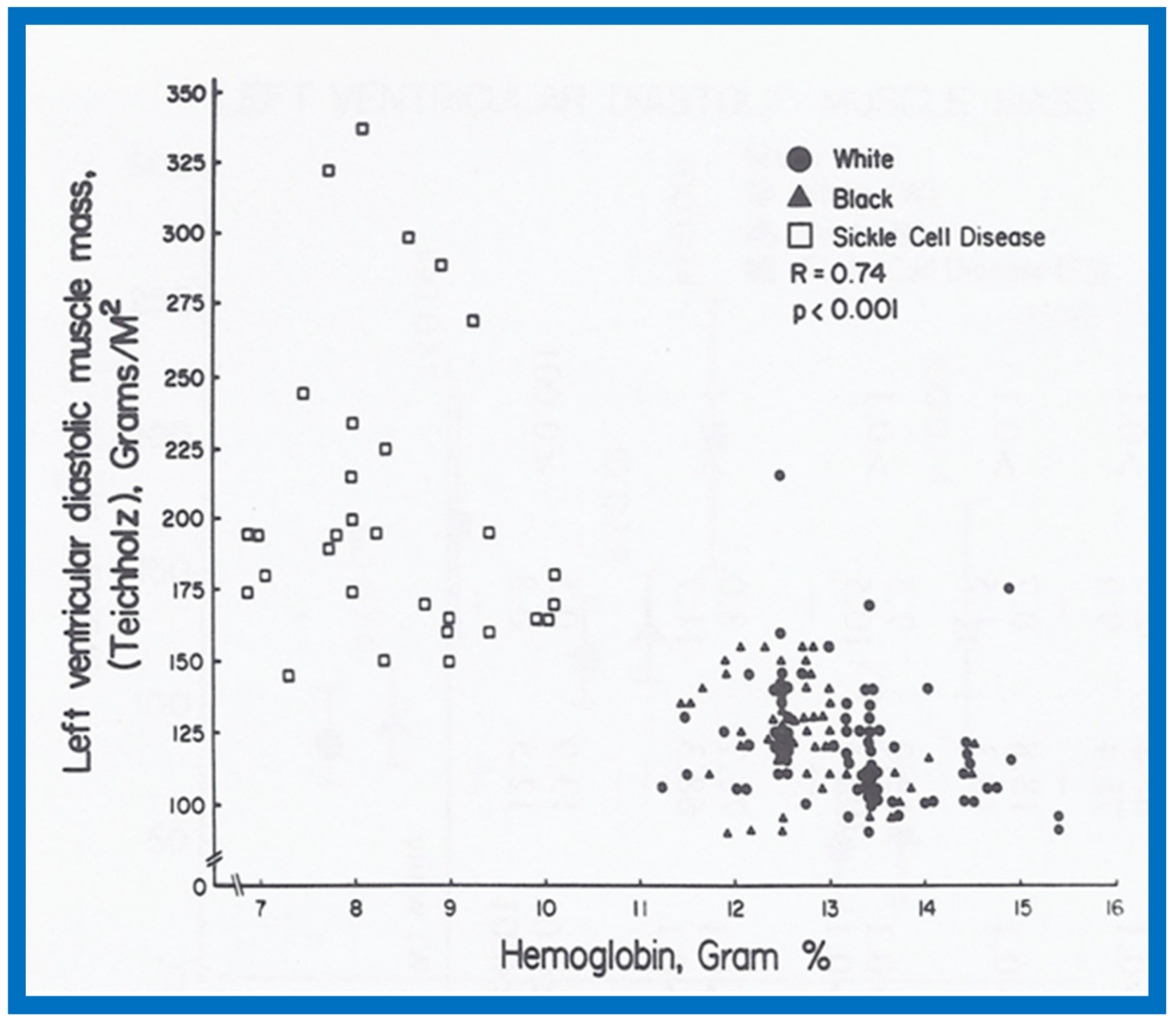
A significant correlation (
R = 0.72,
p < 0.001) was found between the level of hemoglobin and LVMM (
Figure 31) for the entire group.
Since multiple methods of measuring LVMM were available, we attempted to compare these methods to decide which was best for the evaluation of LVMM. All three methods were able to detect the increased LVMM in sickle cell patients. However, in the Ratshin’s method, the mean values were low with a wide scatter (white, 55 ± 25; black, 54 ± 24). In the method of Teichholz, there was a significant difference between the diastolic (white, 121 ± 20; black, 130 ± 20) and systolic (white, 75 ± 11; black, 77 ± 13) LVMM, while there was no such a difference in the cubed-function method (diastolic—white, 89 ± 18, black, 96 ± 17; systolic—white, 88 ± 15, black, 90 ± 19). In theory, there is no reason to have markedly different values for diastolic and systolic LVMM. For these reasons, we concluded that the cubed-function method may be better than the other two in the evaluation of LVMM in children [
9]. The means and standard deviations for LVMM are listed in
Table 2 [
9].
On the basis of this study, it may be concluded that (i) there are no major gender-related differences in echocardiographic LVMM in children, (ii) the LVMM is larger in black than in white children, (iii) the LVMM in children with sickle cell disease is increased when compared with normal children, (iv) the cube-function method of LVMM calculation is better than the other two methods studied, and (v) normal LVMM in children is reasonably well established by this study (
Table 2).
9. Race and Sex Related Differences in Echocardiographic Measurements in Children
Although echocardiography was commonly used for the evaluation of infants and children with suspected heart disease in early 1980s, most of the normal standards did not take race or sex into consideration at that time. This was despite the fact that a substantial influence of gender and race on the ECGs had been shown. The purpose of our study was to scrutinize if sex and race had an important influence on conventional echocardiographic measures [
10]. These data were presented in part at the first World Congress of Pediatric Cardiology, London, England, in June 1980 [
43].
The study included a total of 273 black and white children of both sexes between the ages of 3 and 19; there were 136 black children and 137 white children and 143 were boys and 130 were girls. The subjects were divided into age groups of 3–5, 6–10, 11–14, and 15–19 years. As in our prior studies, all normal children were examined by one of the investigators, and their normalcy was confirmed by physical examination and by normal ECG. Echocardiographic data were also secured as previously detailed [
5,
6,
9] (
Figure 12 and
Figure 13), and calculations were made as listed in
Table 1. Weight, height, blood pressure (systolic and diastolic), chest circumference, antero-posterior diameter of the chest and hemoglobin were measured in all children.
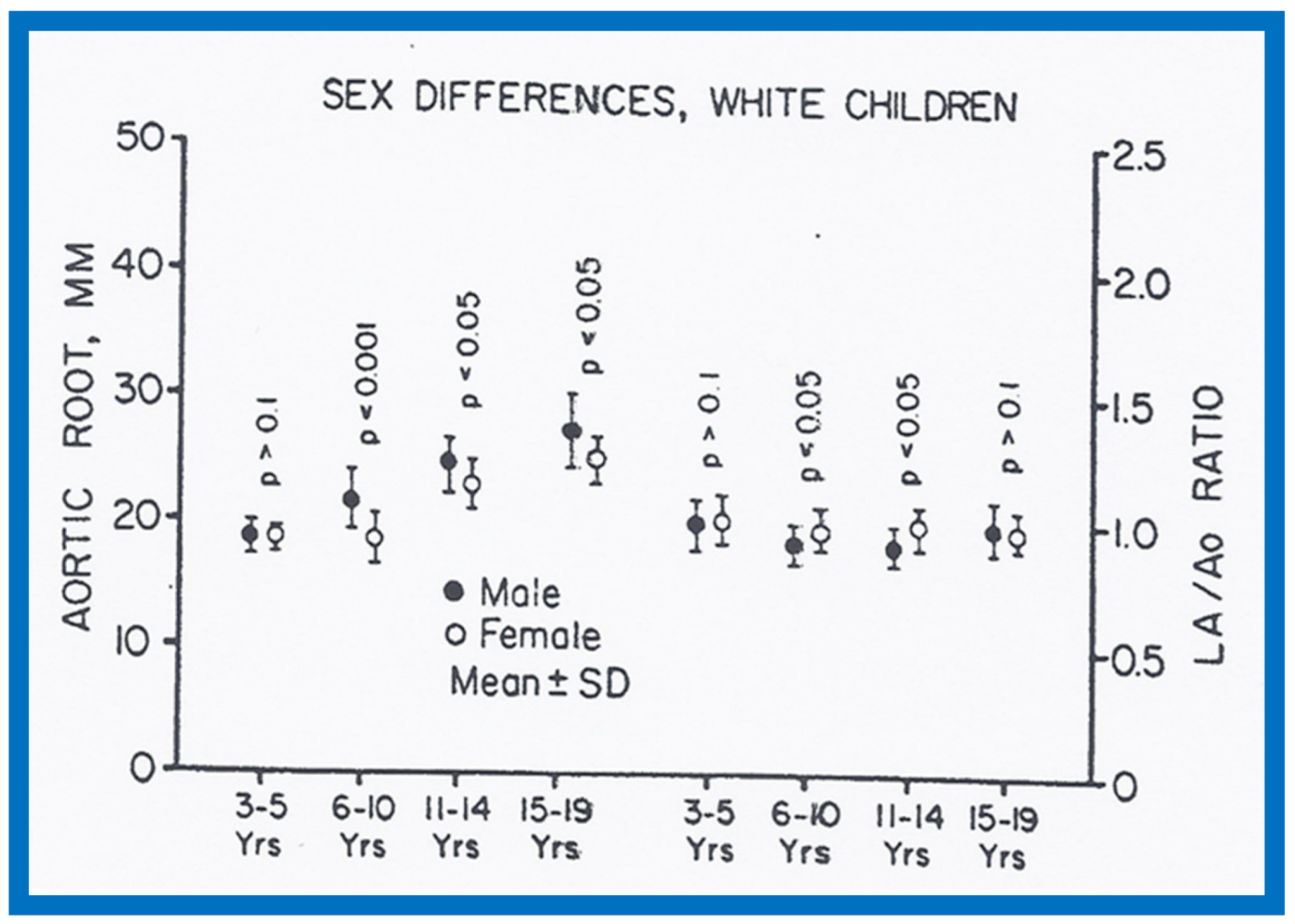
There were no major gender-related differences (
p > 0.05 to
p > 0.1) in echocardiographic measurements with the exception of larger (
p < 0.05 to
p <0.01) Ao and LA in boys than in girls (
Figure 32 and
Figure 33). Larger Ao and LA is seen more consistently in black children than in white children. In addition, the LV posterior wall and interventricular septal thickness diastole were greater (
p < 0.01) in teenage boys than girls. There were no differences (
p > 0.05 to
p > 0.1) in weight, height, blood pressure (systolic and diastolic), chest circumference, antero-posterior diameter of the chest and heart rate between boys and girls, but the hemoglobin was lower (
p < 0.05 to
p <0.01) in 15–19-year-old girls than boys. The reason for larger Ao in boys than girls remains unexplained.
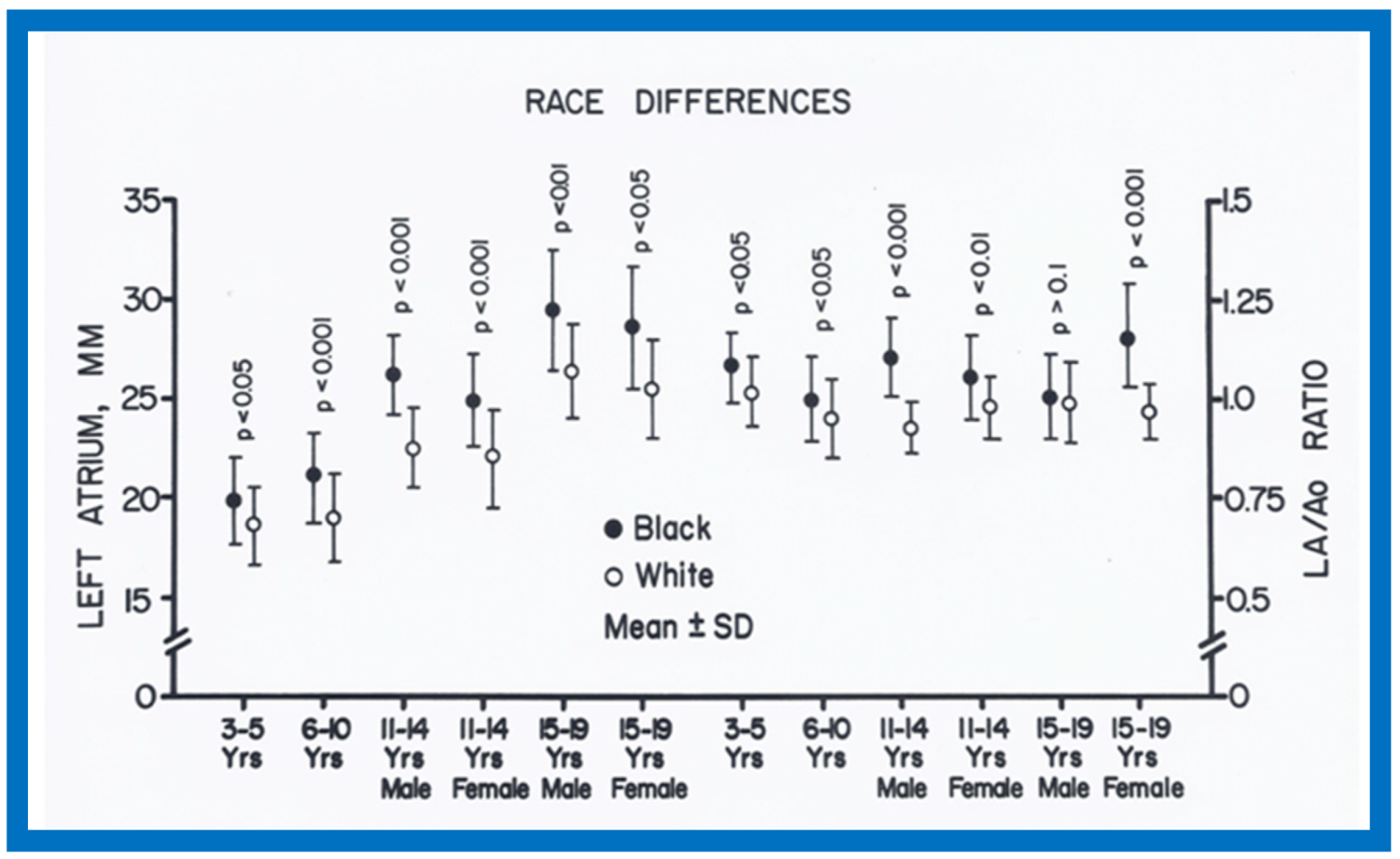
When racial differences were examined, larger (
p < 0.05 to 0.0001) LA and/or LA/Ao ratio in black than white children of all age-sex subgroups were found (
Figure 34). Also, a thicker LV posterior wall and/or LV muscle mass (in black than in white) was found in most age–gender subgroups (
Figure 35). The weight, height, body surface area, chest circumference, antero-posterior diameter of the chest and blood pressure were similar (
p > 0.05), but lower (
p < 0.05 to 0.01) hemoglobin levels in black than white children were seen (
Figure 36) and may, in part, be responsible for the echo differences.
In contrast to significant gender- and race-related ECG differences, the echo differences are few. Normal echocardiographic tables incorporating the detected differences along with percentile distributions are listed in multiple tables in the appendix of our publication [
10].
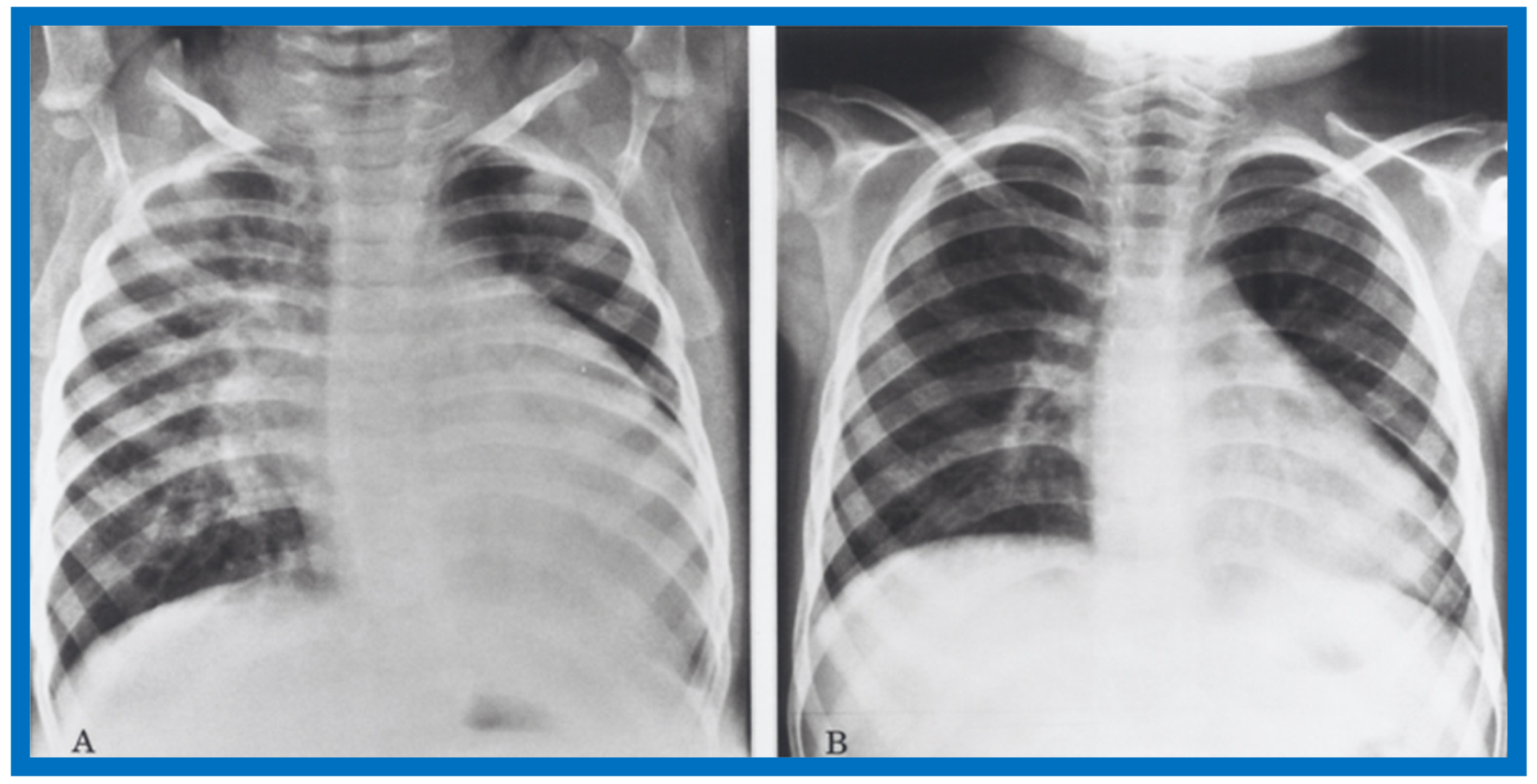
11. Afterload Reduction in the Management of Primary Myocardial Disease
While the use of inotropic agents and diuretics in the management of heart failure in children is widely accepted, the use of afterload reduction had not been well recognized in the management of children with heart failure as of early and mid-1980s. Therefore, we sought to explore the afterload reduction principle in the management of infants and children with primary myocardial disease (PMD) [
12]. The results of this study were presented in part at the 2nd World Congress of Pediatric Cardiology in June 1985 [
44] and at the at the 54th Annual Scientific Meeting of the American Academy of Pediatrics in October 1986 [
45].
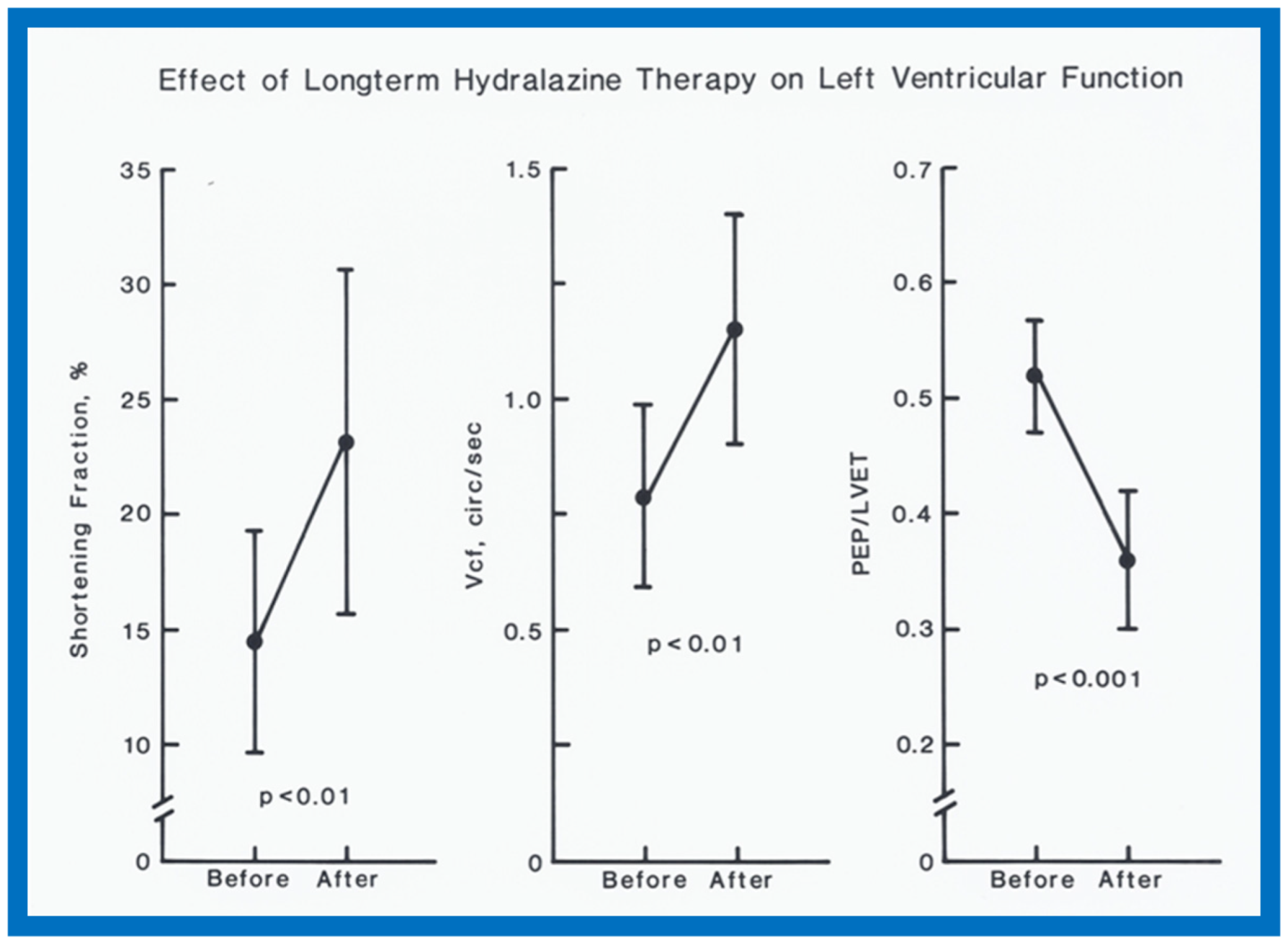
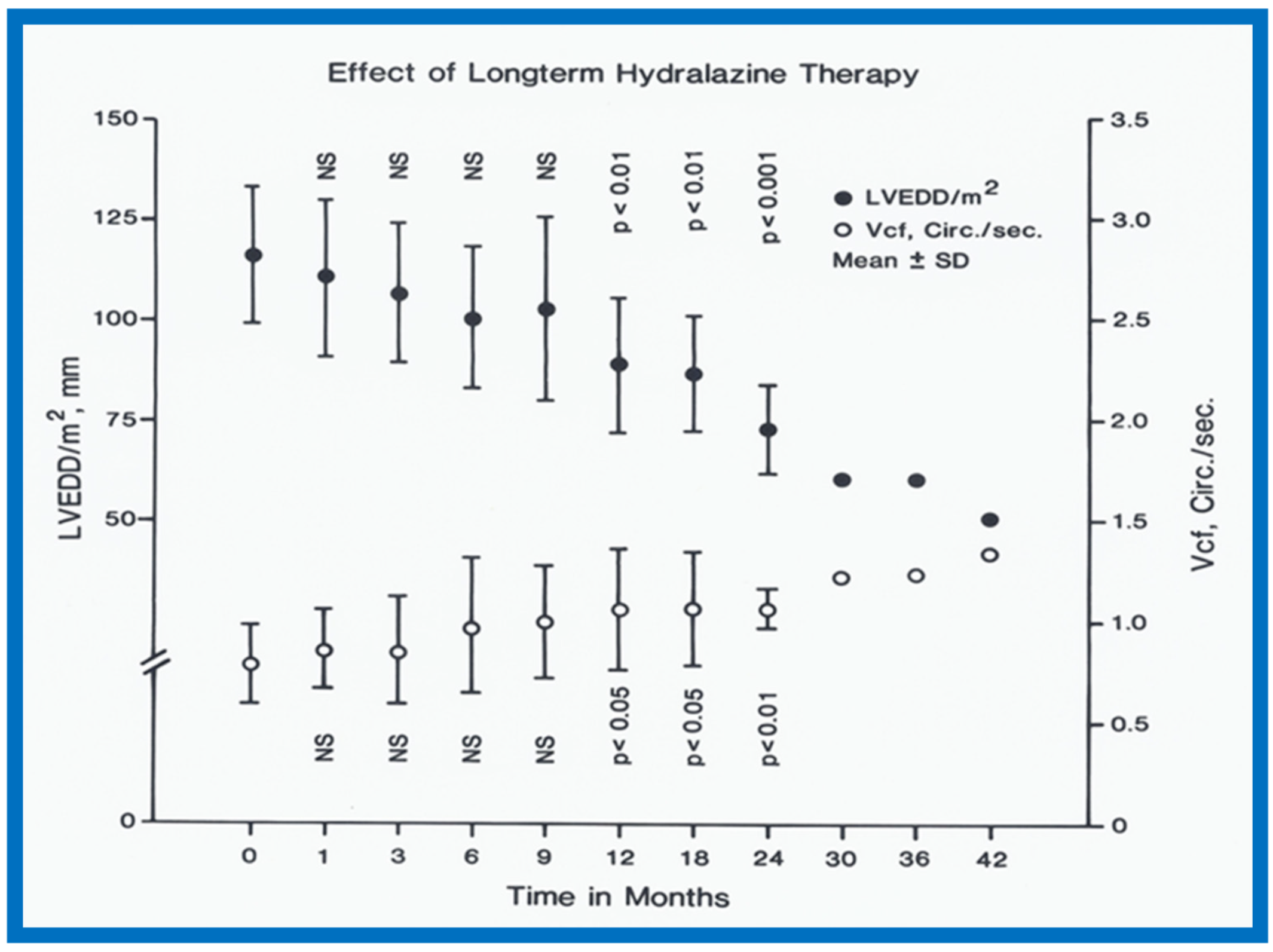
Cardiac catheterization and selective cine-angiography confirmed the clinical diagnosis of PMD in all but one patient. This lone exception child had anomalous origin of the left coronary artery from the pulmonary artery and was excluded from the study. Twenty-six infants and children, aged 3 to 48 months with PMD, were divided into two groups: the first group received conventional anticongestive therapy including digitalis and diuretics while the second group, in addition to conventional therapy, also received hydralazine (4.0 mg/kg/day in four divided doses). In the hydralazine group, the administration of intravenous hydralazine (0.2–0.25 mg/kg) during cardiac catheterization resulted in increased cardiac index (3.18 ± 0.29 vs. 3.75 ± 0.39 L/min/M2; p < 0.01) and decreased systemic vascular resistance (18.68 ± 2.47 vs. 15.4 ± 2.28 units; p < 0.05) without any change in mean arterial pressure (63.6 ± 9.93 vs. 63.7 ± 8.27 mmHg; p > 0.1). Echocardiographic studies were initially performed at 1- to 3-month intervals, and later, at 6-month intervals.
In the hydralazine group, at a median follow-up of 21 months, the LV dimension decreased; (116 ± 7 vs. 87 ± 21 mm/M
2;
p < 0.01), shortening fraction increased (14.5 ± 4.9 vs. 23.2 ± 7.5;
p < 0.01) and Vcf (0.79 ± 0.2 vs. 1.15 ± 0.55 circ/sec;
p < 0.01) (
Figure 37), and the ratio of pre-ejection period to LV ejection time normalized (0.52 ± 0.05 vs. 0.35 ± 0.06;
p < 0.001) (
Figure 37). These improvements occurred gradually but became statistically significant (
p < 0.05 to < 0,001) at 12 months following the initiation of hydralazine therapy (
Figure 38 and
Figure 39). Other indices of LV function also improved, as detailed in the Table from our paper [
12] for the interested reader.
Examples of improvement in LV dimension on echo studies are shown in
Figure 40 and
Figure 41. The cardiac size and pulmonary venous congestion on chest roentgenograms improved in the hydralazine group (
Figure 42 and
Figure 43). No significant changes in any of these parameters occurred in the control group.
While this was a prospective study, we did not use concurrent controls, nor was this a double-blind randomized study with placebo administration in the control group. Consequently, we suggested a double-blind randomized study to confirm our findings. We stated that hydralazine does not alter the basic cardiac disease, but by improving the cardiac output, prolongs the patients’ life, giving an opportunity for recovery of cardiac function and spontaneous improvement, should that be the natural history of disease. We concluded that hydralazine therapy is a valuable addition in the management of PMD in infants and children [
12]. Subsequent to the initiation of our study, afterload reducing, angiotensin-converting enzyme (ACE) inhibitors came into vogue and may be considered superior to hydralazine.
In a chapter in Current Therapy [
46] and in an editorial [
47] published during the early part of the above study, the author reviewed the concept of afterload reduction. The use of intravenous vasodilators (sodium nitroprusside and nitroglycerin) to treat postoperative patients with low cardiac output and oral vasodilators (prazosin and hydralazine) to treat chronic congestive heart failure were also reviewed [
46,
47]. Indeed, these reviews, in part, enticed the author to initiate the afterload reduction study [
12] just reviewed.
In an editorial communication in 1995 [
48], we commented on the use of ACE inhibitors instead of vasodilators such as hydralazine as afterload reducing agents to treat dilated cardiomyopathy.
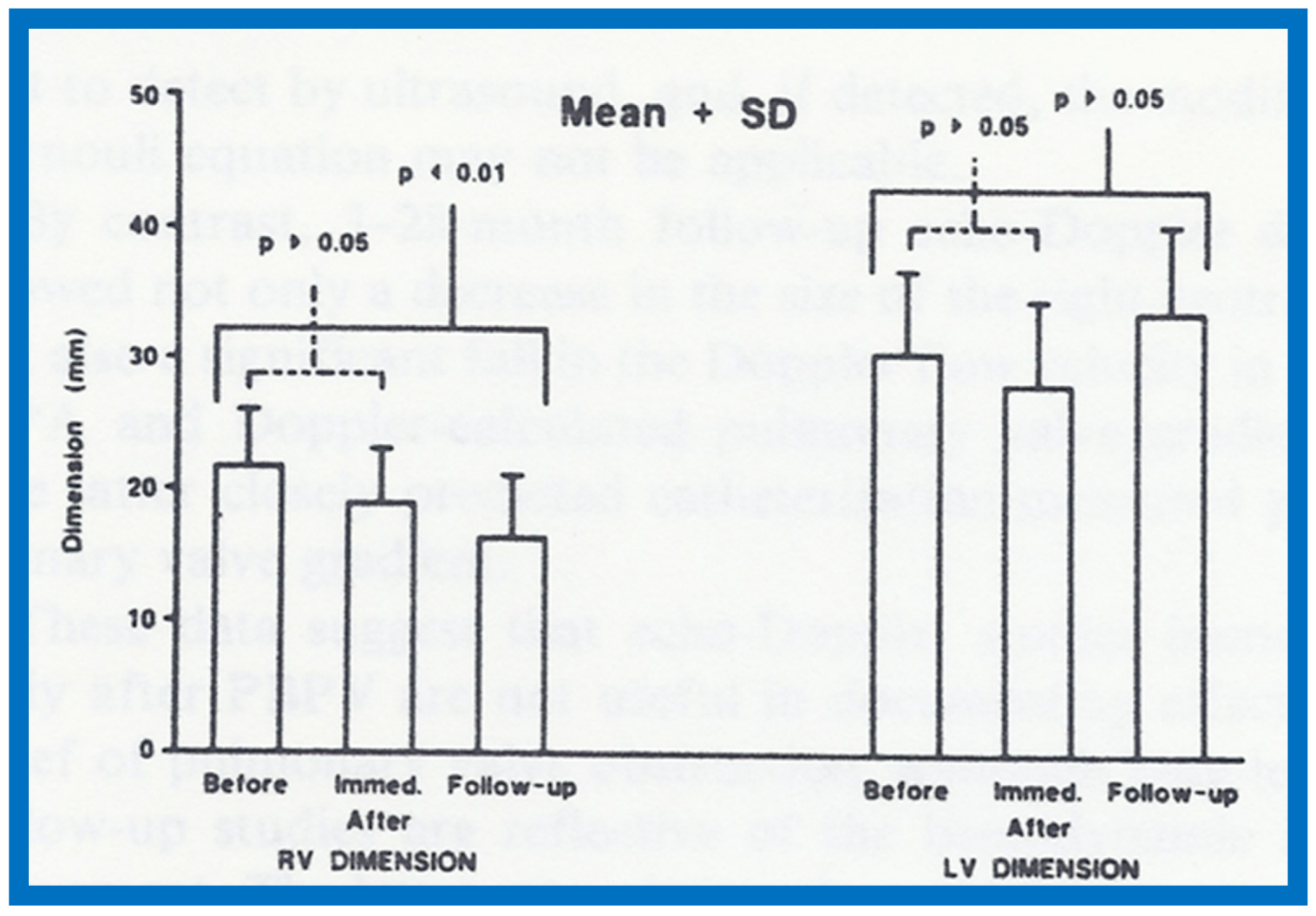
12. Echo-Doppler Studies in the Evaluation of the Results of Balloon Pulmonary Valvuloplasty
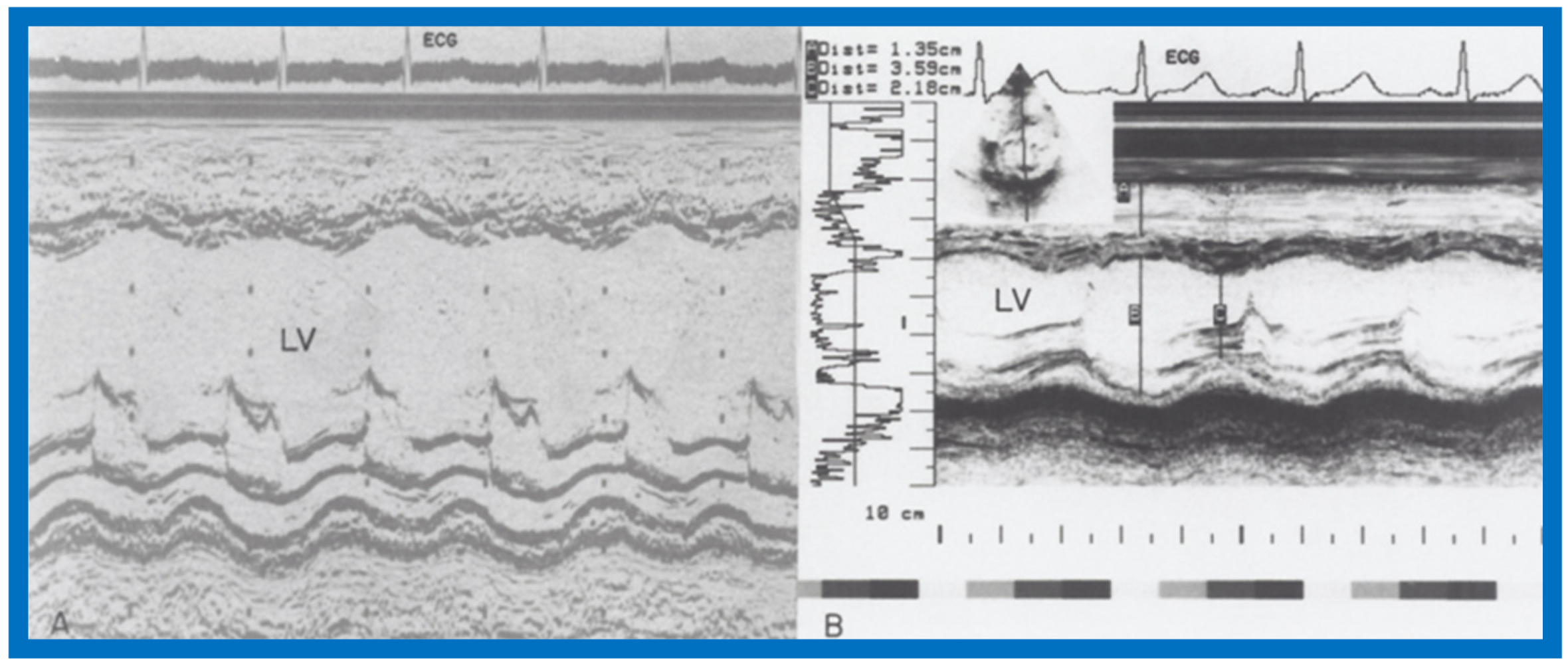
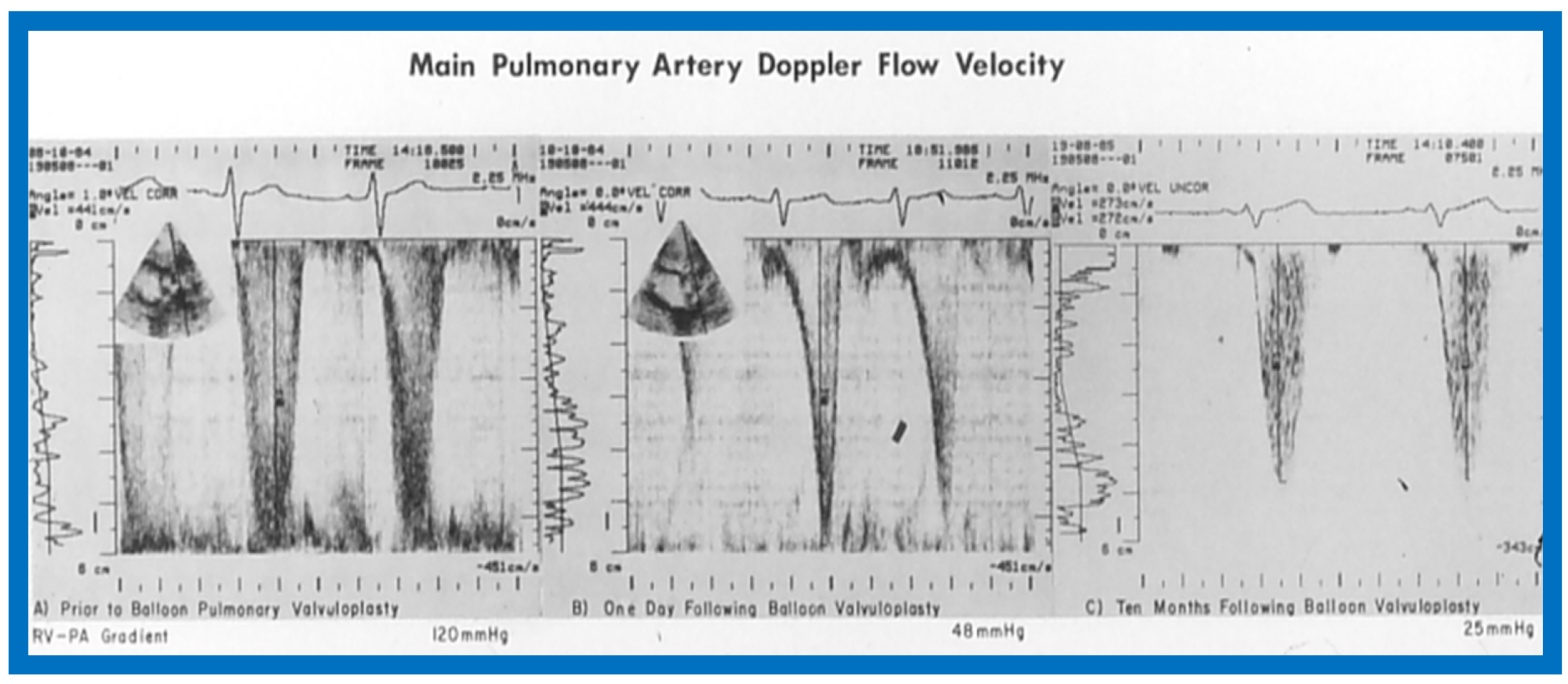
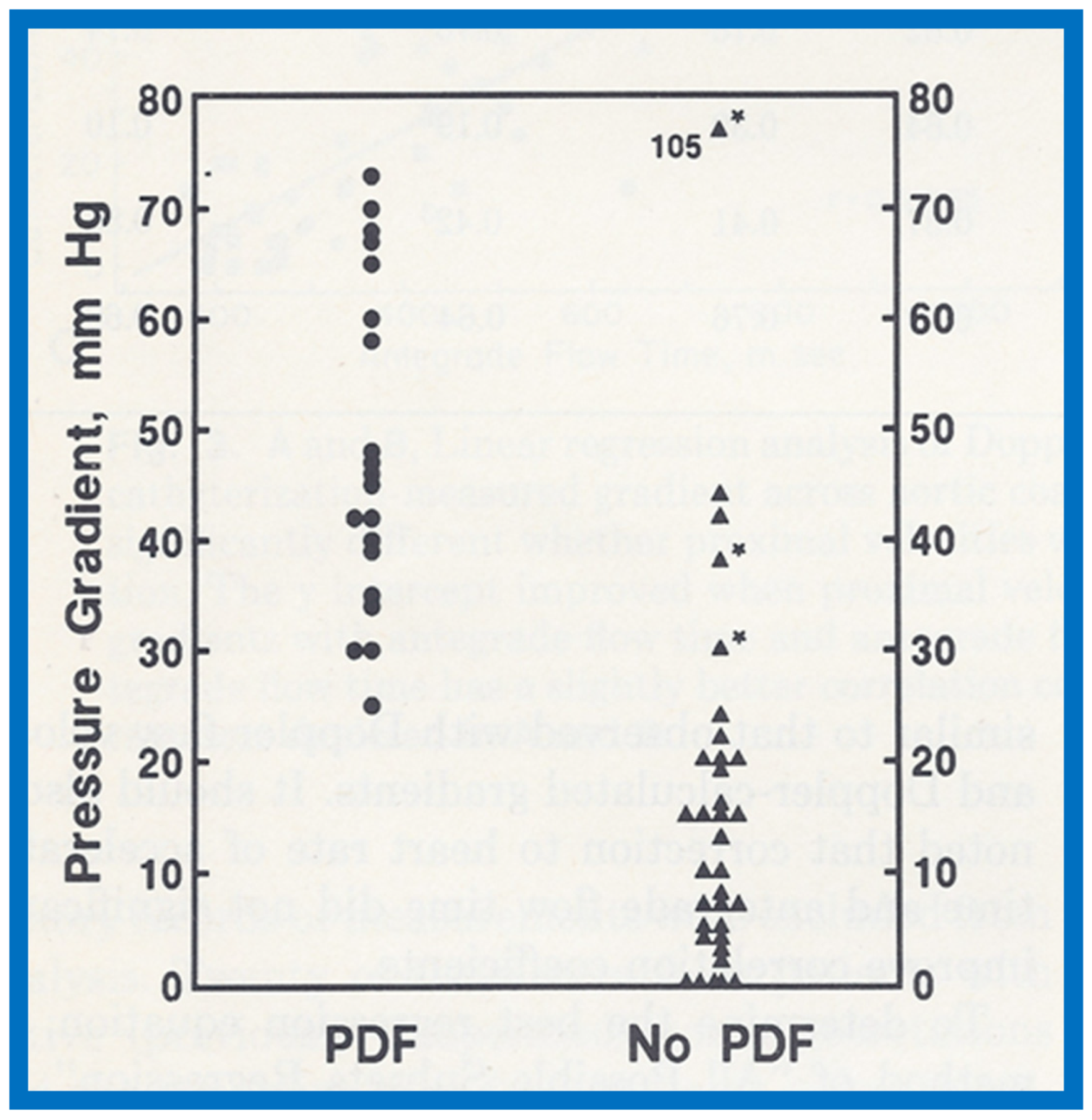
The utility of echo-Doppler studies in the assessment of the results of balloon dilatation of the pulmonary valve was examined [
13]. While the right ventricular end-diastolic dimension (RVED) did not significantly change (
p > 0.05) immediately following balloon pulmonary valvuloplasty (
Figure 44), the Doppler flow velocity and calculated pressure gradient across the pulmonary valve (
Figure 45) decreased significantly (
p < 0.01).
However, there was some discrepancy between the Doppler-derived and catheterization-measured transpulmonary valve gradients in four patients. These patients had either severe stenosis (catheterization gradients between 94 to 190 mmHg) or severe residual infundibular stenosis immediately following balloon valvuloplasty. In one patient, despite a fall in pulmonary valvar gradient by catheterization, the Doppler flow velocity did not decrease. We explored potential causes for this discrepancy and excluded technical aspects of Doppler recording, but surmised that small vertex shed distance in small orifices or cone-shaped spray formation instead of in a focused jet, making it difficult to detect by ultrasound, as postulated by Vasko and associates [
49], which may explain the discrepancy. Or, as our later experience suggested, this may in part be related to RV infundibular constriction which occurred immediately after balloon pulmonary valvuloplasty.
At follow-up (3 to 28 months after valvuloplasty), the RVED (
Figure 46) decreased significantly (
p < 0.01), as did the Doppler flow velocity and calculated pressure gradient across the pulmonary valve (
Figure 47) (
p < 0.01). The Doppler gradient reduction is similar to that obtained by cardiac catheterization concurrently. In addition, there was a good correlation (
r = 0.8) between Doppler-derived and catheterization-measured transpulmonary valve gradients at follow-up.
It was concluded that echo-Doppler studies may not be truly indicative of the immediate results, but are reflective of the results at follow-up; the latter may obviate the need for repeat cardiac catheterization for evaluations of follow-up results of balloon pulmonary valvuloplasty [
13].
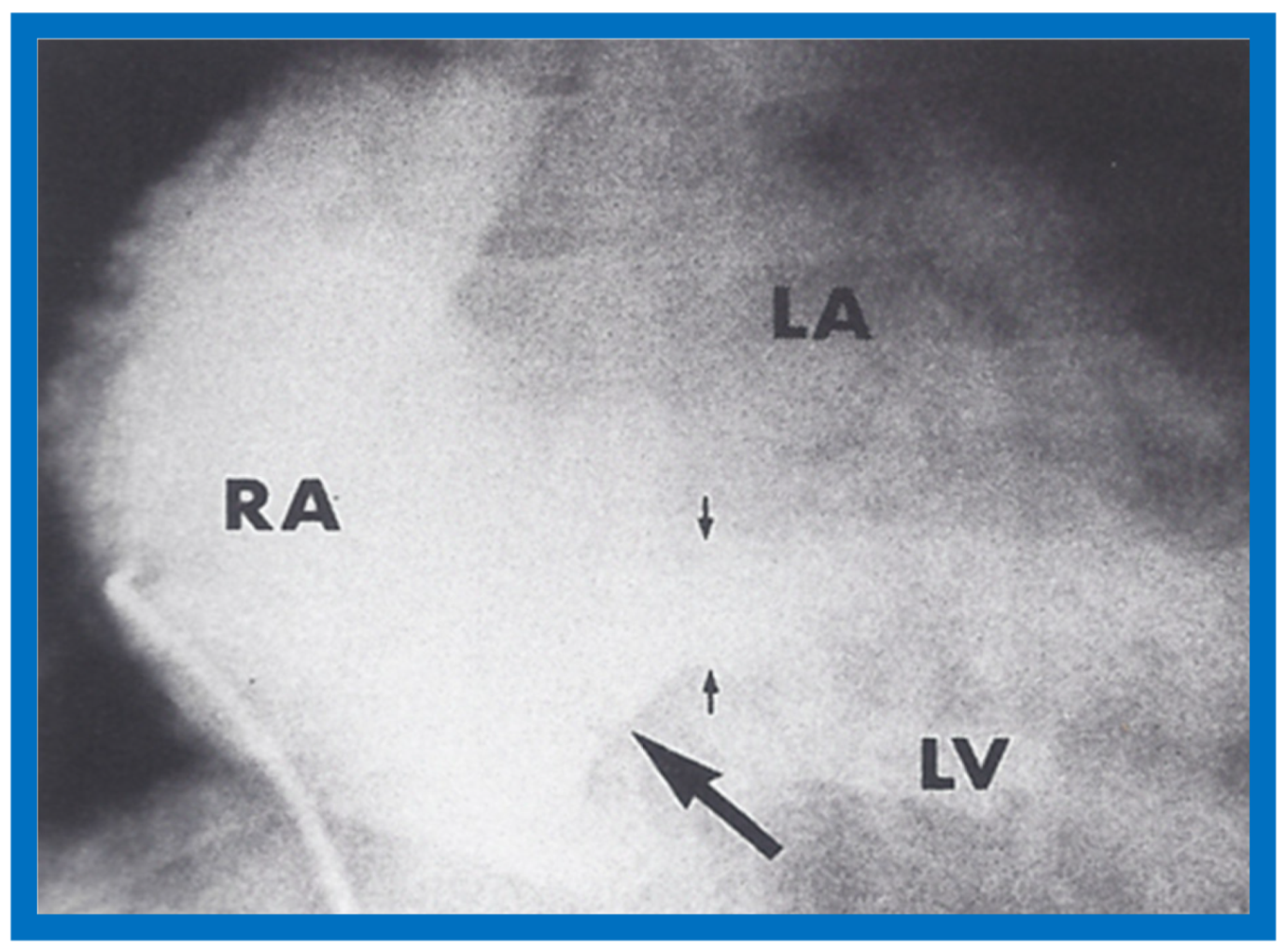
14. Echocardiographic Demonstration of Atrioventricular Type of Tricuspid Atresia
The author reported on the clinical, radiographic, ECG, echocardiographic and hemodynamic features of a rare case of common atrioventricular canal (currently called atrioventricular septal defect) mimicking tricuspid atresia in an eight-year-old child [
15]. The clinical, radiographic and ECG characteristics were similar to those of classic tricuspid atresia. Hemodynamic data secured at cardiac catheterization were also similar to those seen with tricuspid atresia. A two-dimensional echocardiogram demonstrated an ostium primum atrial septal defect with a common atrioventricular valve and a small RV (
Figure 50a,b); the entry into the RV appeared to be occluded by a leaflet of the common atrioventricular valve. Left ventricular cineangiogram in postero-anterior view demonstrated “gooseneck” deformity, similar to that seen in atrioventricular canal defects [
15]. However, right atrial angiography resulted in direct emptying of the contrast material into the left ventricle via an ostium primum atrial septal defect (
Figure 51). The floor of the right atrium seemed to be formed by a leaflet of the common atrioventricular valve (
Figure 51). Thus, the two-dimensional echocardiographic and right atrial cineangiographic features appeared to be distinctive, and could be utilized to distinguish this anomaly from other varieties of tricuspid atresia.
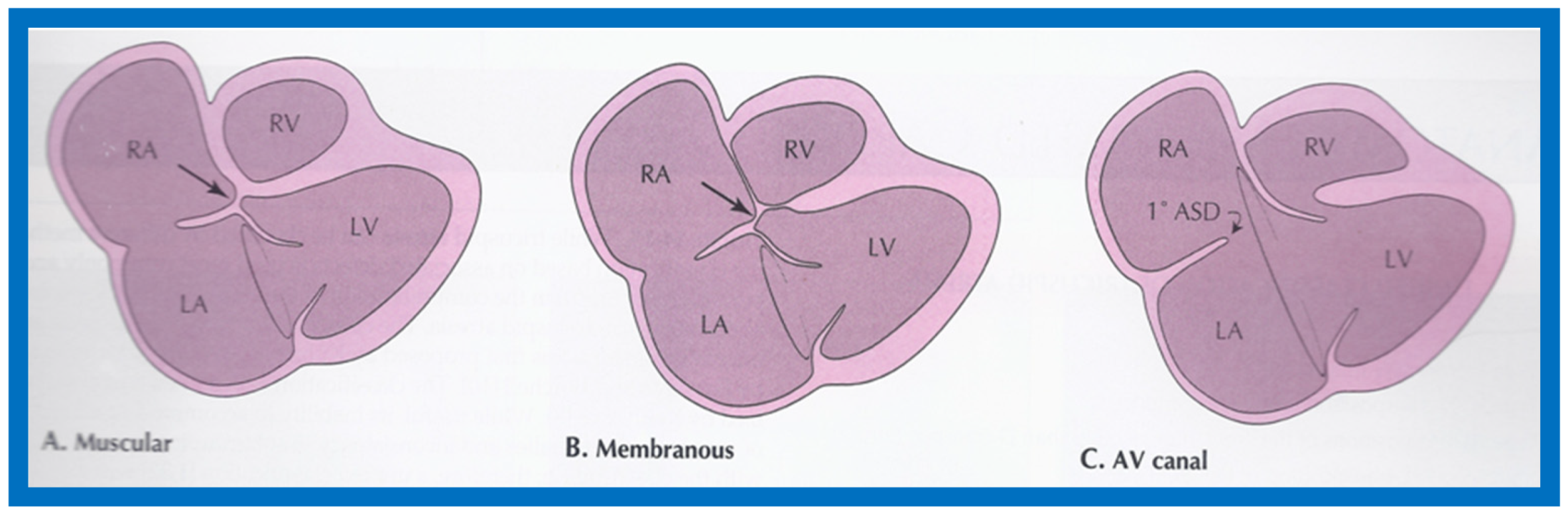
The reported anomaly is definitely different from classic tricuspid atresia, but has physiologic effects similar to classic tricuspid atresia. A detailed review of the literature at that time suggested that this anomaly is extremely rare, with only one brief mention of a similar case by Van Praagh by that time [
50]. Evaluation of crux cordis (Figure 54) on two-dimensional echocardiogram (subcostal four-chamber view) may help to distinguish these anomalies from each other. In muscular type of tricuspid atresia, a dense band of echoes is seen where the normal tricuspid valve should be (
Figure 52a). In membranous types of tricuspid atresia, a thin membrane is seen instead (
Figure 52b). In both types, the anterior leaflet of the detectable atrioventricular valve is attached to the left side of interatrial septum (
Figure 52a,b). In the atrioventricular canal type of tricuspid atresia, the crux cordis is abnormal and cannot be identified, and a large atrioventricular valve leaflet occludes the entry of the RA into the RV (
Figure 52c). It was concluded that two-dimensional echocardiographic and angiographic features help differentiate atrioventricular canal type of tricuspid atresia from classic tricuspid atresia cases [
15].
15. Review: Doppler Echocardiography in Noninvasive Diagnosis of Heart Disease
The author reviewed the role of Doppler echocardiography in noninvasive diagnoses of heart disease in infants and children in the late 1980s [
16]. The purpose of that review was to describe the principles of Doppler echocardiography and its clinical applications. Doppler is the study of low magnitude echoes from blood cells which are rejected in regular, imaging echocardiography. Doppler, by using modified Bernoulli equation and measured arm blood pressure, along with some assumptions, facilitates in providing flow and pressure measurements from the heart chambers and the blood vessels. Thus, Doppler supplements the anatomic information provided by the imaging echocardiography, and should be performed in conjunction with regular echocardiographic study.
The discussion began by explaining ultrasound, its transmission into the body producing echoes, and the rejection of low intensity echoes from blood cells in conventional imaging echocardiography, which were studied by applying the principle of Doppler (apparent shift of transmitted frequency by moving blood cells) and analysis of frequency shift by Fourier transformation or Chrisp-Z methodology built into the echo-Doppler equipment. There are many types of Doppler, including pulsed Doppler, continuous wave Doppler, high pulsed rate frequency Doppler and color Doppler. Discussion of color flow Doppler imaging was not included in that review. Each type of Doppler has its own advantages and disadvantages. This is followed by a discussion of how Doppler data is acquired. The clinical application of Doppler to include calculation of cardiac output/index, qualitative and quantitative estimation of intracardiac shunts (atrial and ventricular septal defect and patent ductus arteriosus), the detection and quantification of semilunar and atrioventricular valve stenosis and insufficiency were briefly discussed, with examples of Doppler images for most of the lesions included in the discussion. It was concluded that Doppler studies should be performed in conjunction with imaging echocardiography, and that it is a useful adjunct to it [
16].
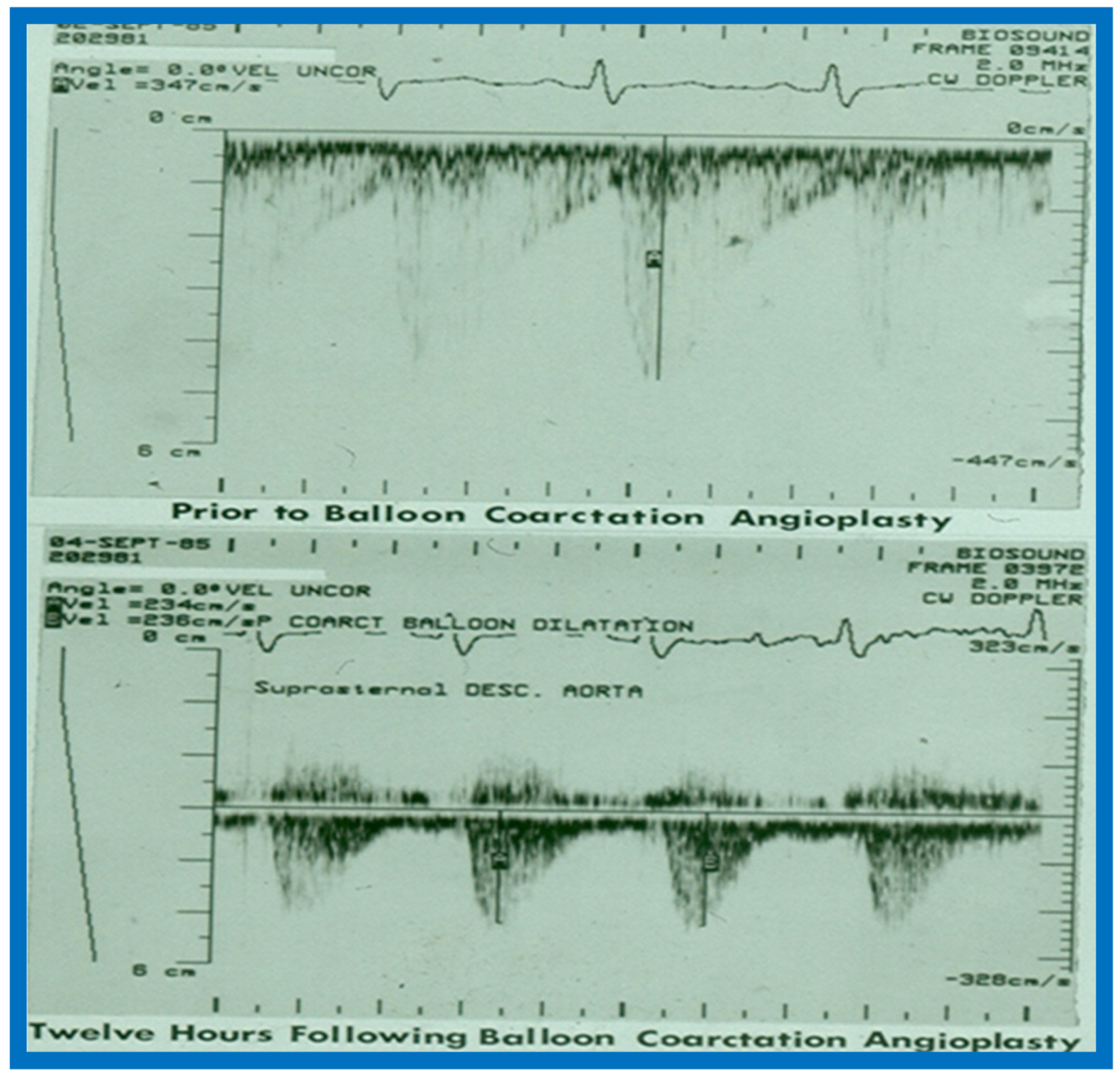
16. Echo-Doppler Studies in the Evaluation of the Results of Balloon Angioplasty of Aortic Coarctation
This study sought to appraise the usefulness of echo-Doppler studies in evaluating immediate and follow-up results of balloon angioplasty of native aortic coarctation [
17]. Echo-Doppler data prior to and immediately following angioplasty were available for 19 infants and children, and such data at follow-up (3 to 22 months; mean 12 months) were accessible for review in 18 patients. There was no significant change (
p > 0.1) in left ventricular (LV) end-diastolic dimension, LV posterior wall thickness in diastole and LV shortening fraction either immediately after balloon angioplasty or at follow-up. However, the Doppler flow velocity (3.2 ± 0.85 vs. 2.5 ± 0.5 m/s) and the calculated pressure gradients (∆P = 4V
2) across the coarctation 43.3 ± 21.9 vs. 26.5 ± 10.3 mmHg) decreased immediately after (
p < 0.01) balloon angioplasty, as well as at follow-up (
p < 0.02). But there was not a good correlation between the Doppler derived and catheterization-measured gradients (
r = 0.49–0.78). It was also observed that pandiastolic anterograde descending aortic flow shortened/disappeared (
Figure 53 and
Figure 54) in all patients who had successful balloon angioplasty. It was concluded that echo-Doppler studies are useful in demonstrating effectiveness of relief of aortic obstruction by balloon angioplasty, but are not predictive of exact residual gradients. This prompted us to conduct more extensive study to evaluate this issue [
18], which will be discussed in the next section.
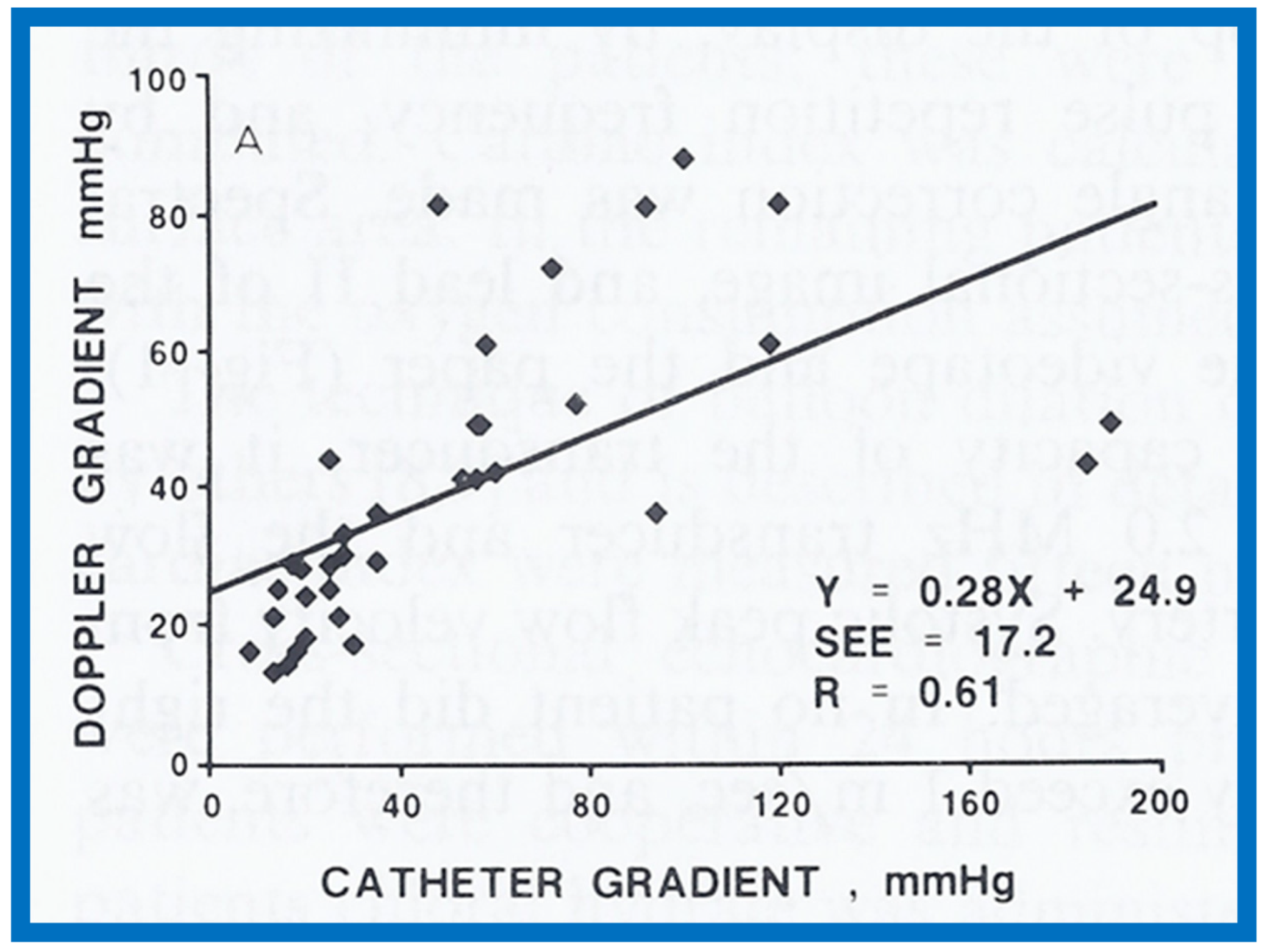
17. Value of Doppler in the Prediction of Pressure Gradients across Coarctation of the Aorta
Given the inability of Doppler to predict gradients across the coarctation site, as described in the preceding study [
17] and reports with contradictory findings [
51,
52], with the former suggesting excellent correlation [
51] and the latter indicating poor relationships [
52], we decided to examine this issue with a study involving a sizable group of patients with aortic coarctation [
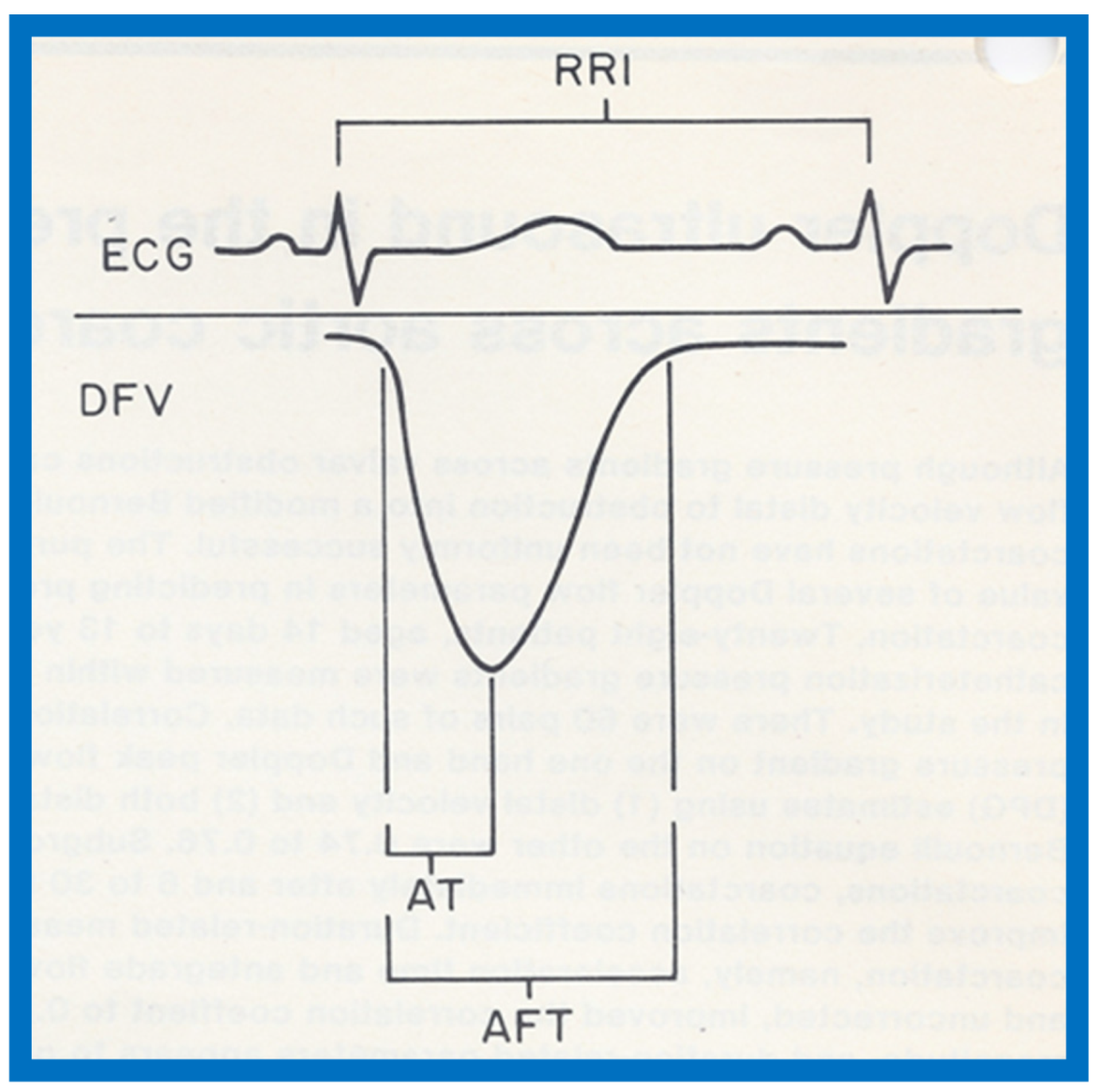
18]. Sixty pairs of data sets with Doppler variables and catheterization-measured pressure gradients recorded within 24 h of each other from twenty-eight patients, aged 14 days to 13 years (4.5 ± 3.9 years), were included in the study [
18]. Doppler pressure gradients were estimated using distal velocity alone (∆P = 4V
2) and both distal and proximal velocities (∆P = 4[V
22 − V
12]) in the modified Bernoulli equation. Duration-related measures of Doppler flow signal distal to the coarctation site, namely, acceleration time (AT) and antegrade flow time (AFT) (
Figure 55), were also measured.
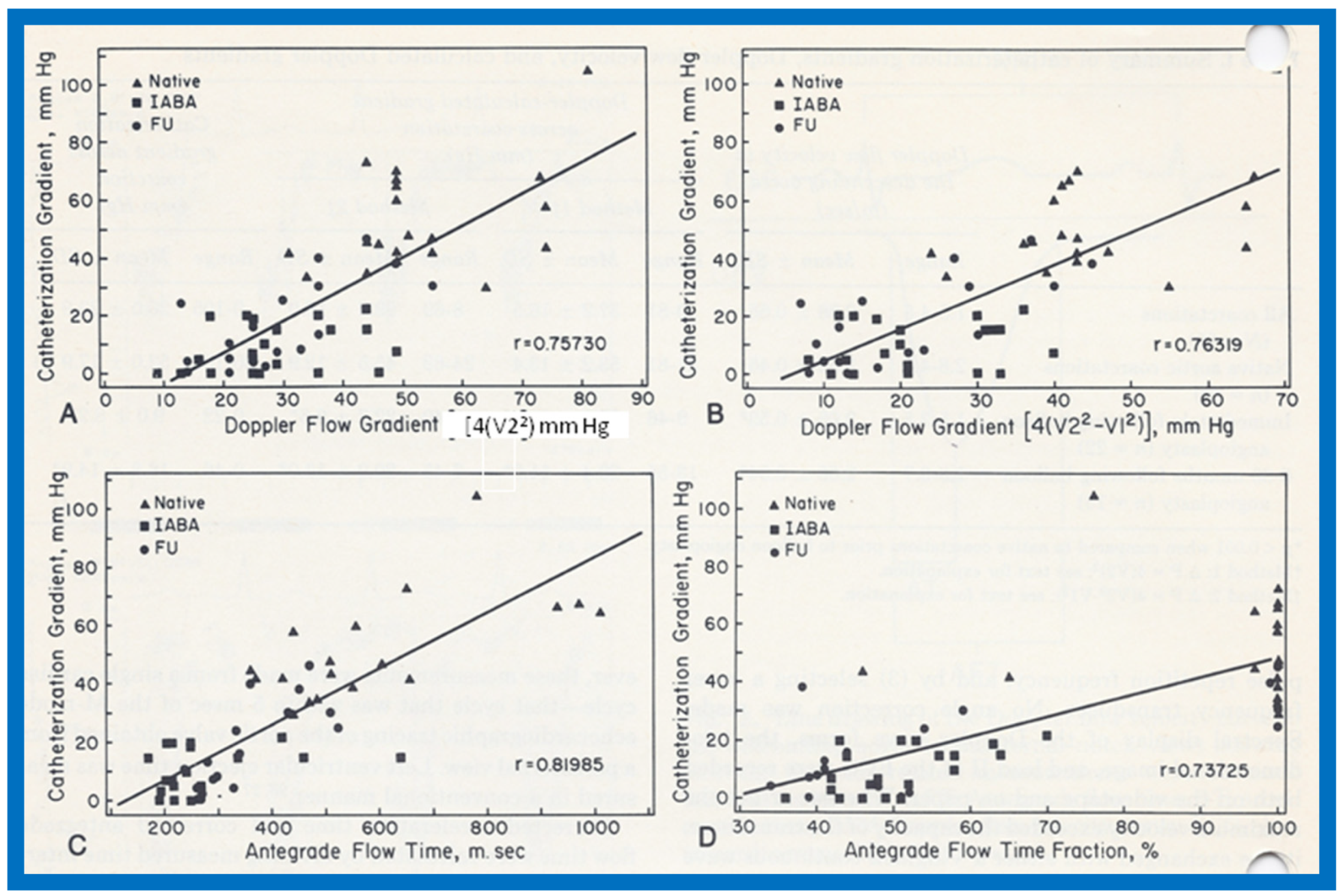
A comparison of the Doppler-derived (∆P = 4V
2) peak instantaneous and catheterization-measured peak-to-peak gradients resulted in a correlation coefficient of 0.757. (
Figure 56A). The inclusion of both proximal and distal velocities (∆P = 4[V
22 − V
12]) in the modified Bernoulli equation (
Figure 56B) did not significantly increase the correlation (
r = 0.763). A comparison of the catheterization data with antegrade flow time (
r = 0.82) and antegrade flow time fraction (
r = 0.737) showed marginal, if any, improvement in the correlation coefficients (
Figure 56C,D). Separating into subgroups of native, immediate postballoon and follow-up postballoon did not improve the correlation coefficients (Tables II and III from [
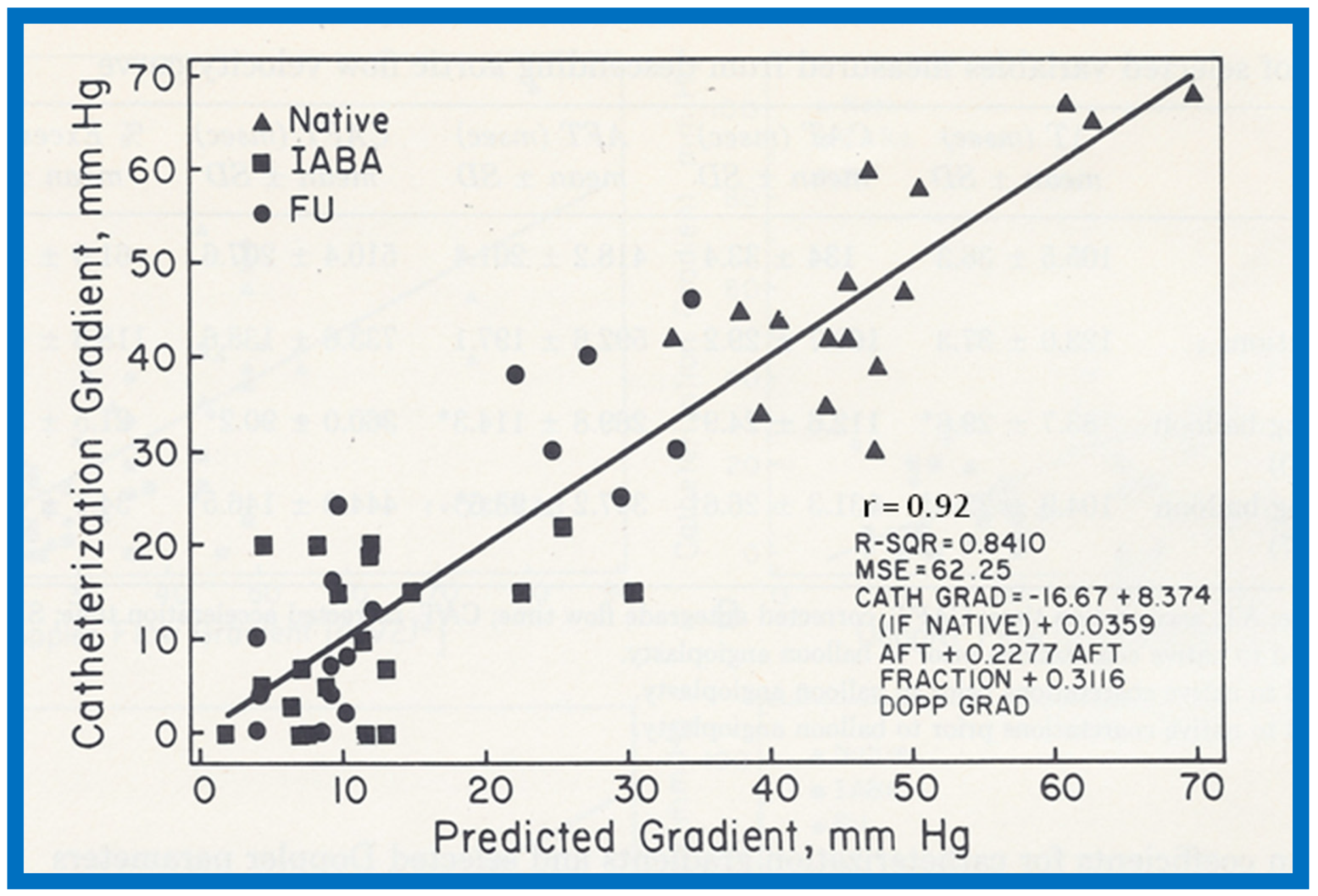
18]). However, a blend of magnitude and duration related Doppler curves (using the method of “All Possible Subsets Regression”; Catheterization gradient = 0.31DPV + 0.22 AFT fraction + 0.04 AFT − 16.67) [
18] improved the correlation coefficient to 0.92 (
Figure 57). It was also observed that peak gradients in excess of 25 mmHg were seen in the presence of pandiastolic flow in the descending aortic Doppler curve with 100% specificity and 80% sensitivity (
Figure 58).
It was further noted that the Doppler flow velocity magnitude and calculated gradients improved (
p < 0.001) following balloon angioplasty of native aortic coarctation; this was similar to reduction in peak-to-peak pressure gradients by catheterization. A discussion of possible reasons for the lack of correlation between Doppler and catheter gradients included peak-to-peak vs. peak instantaneous gradients and possible collateral vessel flow in aortic coarctation. It was concluded that (i) the magnitude and duration related Doppler velocity recordings are helpful in estimating coarctation gradients, and (ii) Doppler is useful in demonstrating the relief of obstruction by balloon angioplasty [
18].
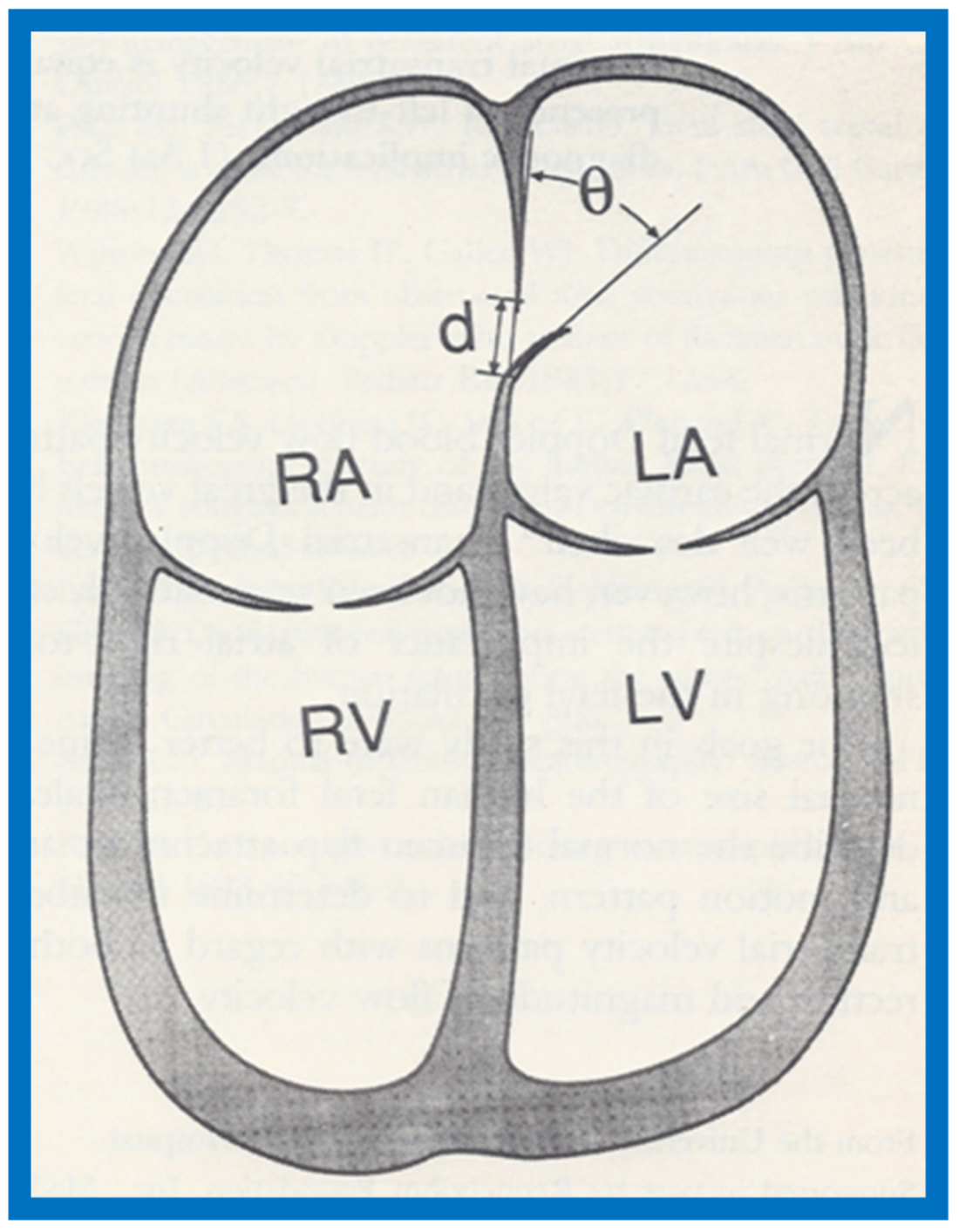
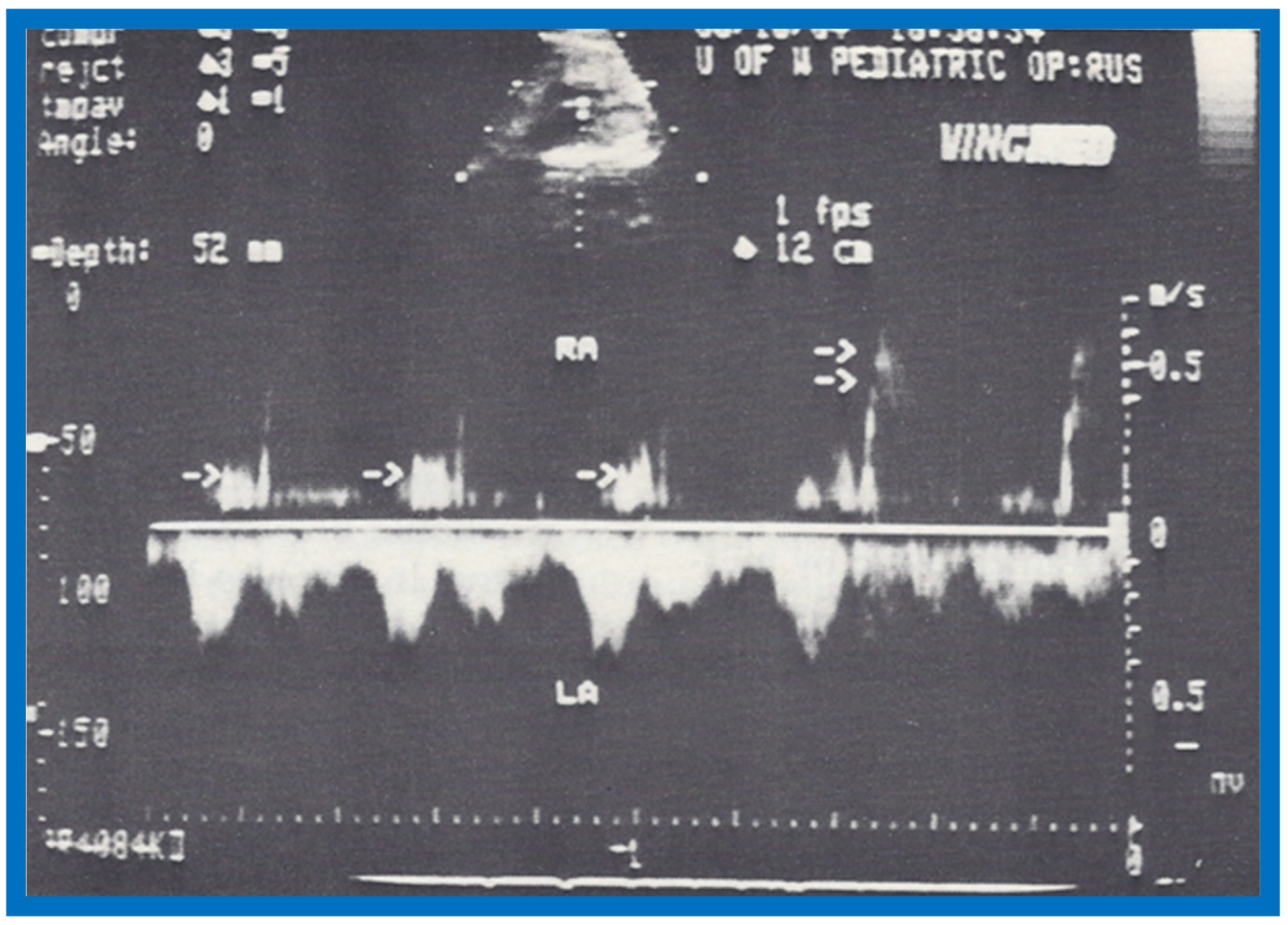
18. Foramen Ovale and Transatrial Doppler Velocity Patterns in the Normal Fetus
Despite the importance of foramen ovale (FO) in fetal circulation, the size of and shunt velocity patterns across the FO in the fetus had not been thoroughly investigated as of the mid-/late-1980s. Therefore, we endeavored to define the normal size of FO and the Doppler velocity patterns across the atrial septum in the normal fetus. Normal human fetal ultrasound studies in 48 consecutive fetuses were examined and the size of FO, foramen flap angle (
Figure 59), its motion and flow characteristics across it were scrutinized [
19].
The maximal FO diameter was similar to the diameter of the Ao at all gestational ages (
Figure 60); there was no more than 1.0 mm difference between the size of FO and Ao in any study. When the size of FO is expressed as a percentage (%) of aortic root, it was 96%, with a range of 77% to 125%. The angle of attachment of foramen flap at the junction of FO with the rim of the FO varied from 30° to 50° degrees; a minimum of 30° angle was seen at some point in the cardiac cycle. A redundant FO flap was seen in only three fetuses. The transatrial Doppler flow velocities with sample volume placed across FO on the left atrial side of the FO (
Figure 61) were available for review in seventeen patients. A triphasic pattern was seen in systole with predominantly right-to-left flow (right atrium [RA] to LA) in all fetuses (
Figure 61). Right-to-left flow velocity varied from 15 to 40 cm/s with a mean of 23 cm/s, and was always less than or equal to mitral valve A wave velocity. Left-to-right flow was also seen in late diastole in all studies (
Figure 61; single arrows in the first three beats). The left-to-right flow was also documented by color flow imaging in some of these babies. The left-to-right flow velocity was lower and ranged between 5 to 20 cm/s with a mean of 13 cm/s.
Our study showed that the size of normal foramen ovale is similar to aortic root diameter, and that the foramen flap angle reaches 30 degrees or greater. Right-to-left flow is as anticipated for fetal circulatory physiology; the left-to-right flow documented in this study was unexpected and may be related instantaneous pressure difference between atria, as previously shown in patients with tricuspid atresia [
53]. These finding of left-to-right flow across the foramen ovale may have implications in conditions such as total anomalous pulmonary venous connection and severe left heart obstructive lesions [
19].
The author’s contributions to the echocardiography literature from 1991 to the current date will be detailed in Part II of this review.