Amblyopia and Routine Eye Exam in Children: Parent’s Perspective
Abstract
:1. Introduction
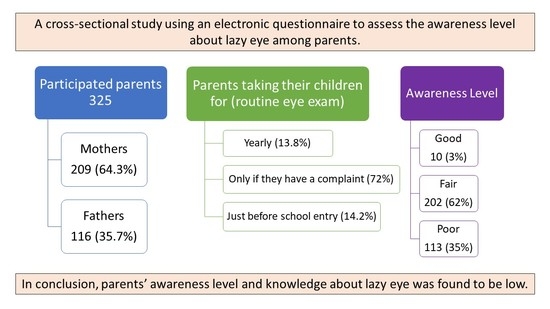
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Instruments
2.4. Procedure
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barrett, B.T.; Bradley, A.; McGraw, P.V. Understanding the Neural Basis of Amblyopia. Neuroscientist 2004, 10, 106–117. Available online: https://pubmed.ncbi.nlm.nih.gov/15070485/ (accessed on 26 April 2021).
- Basheikh, A.; Alhibshi, N.; Bamakrid, M.; Baqais, R.; Basendwah, M.; Howldar, S. Knowledge and attitudes regarding amblyopia among parents in Jeddah, Saudi Arabia: A cross-sectional study. BMC Res. Notes 2021, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gunnlaugsdottir, E.; Arnarsson, A.; Jonasson, F. Prevalence and causes of visual impairment and blindness in Icelanders aged 50 years and older: The Reykjavik Eye Study. Acta Ophthalmol. 2008, 86, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Hansen, E.; Flage, T.; Rosenberg, T.; Rudanko, S.-L.; Viggosson, G.; Riise, R. Visual Impairment in Nordic Children: III. Diagnses. Acta Ophthalmol. 1992, 70, 597–604. Available online: https://pubmed.ncbi.nlm.nih.gov/14714829/ (accessed on 27 April 2021).
- Levi, D.M.; Knill, D.C.; Bavelier, D. Stereopsis and amblyopia: A mini-review HHS Public Access. Vis Res. 2012, 2012, 17–30. [Google Scholar]
- Bardisi, W.M.; Bin Sadiq, B.M. Vision screening of preschool children in Jeddah, Saudi Arabia. Eye Care Rev. 2002, 1, 7–10. [Google Scholar]
- de Zárate, B.R.; Tejedor, J. Current Concepts in the Management of Amblyopia. Acta Ophthalmol. 2007, 403–414. Available online: http://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/19668517 (accessed on 26 April 2021).
- Ehrlich, M.I.; Reinecke, R.D.; Simons, K. Preschool Vision Screening for Amblyopia and Strabismus. Programs, Methods, Guidelines, 1983. Surv. Ophthalmol. 1983, 28, 145–163. Available online: https://0-doi-org.brum.beds.ac.uk/10.1016/0039-6257(83)90092-9 (accessed on 26 April 2021). [CrossRef]
- Shaikh, A.G.; Otero-Millan, J.; Kumar, P.; Ghasia, F.F. Abnormal Fixational Eye Movements in Amblyopia. PLoS ONE 2016, 1, e0149953. [Google Scholar] [CrossRef]
- Tailor, V.; Bossi, M.; Greenwood, J.A.; Dahlmann-Noor, A. Childhood Amblyopia: Current Management and New Trends. Br. Med. Bull. 2016, 119, 75–86. Available online: https://pubmed.ncbi.nlm.nih.gov/27543498/ (accessed on 26 April 2021).
- McKee, S.P.; Levi, D.M.; Movshon, J.A. The Pattern of Visual Deficits in Amblyopia. J. Vis. 2003, 3, 380–405. Available online: https://pubmed.ncbi.nlm.nih.gov/12875634/ (accessed on 26 April 2021).
- Hess, R.; Howell, E. The threshold Contrast Sensitivity Function in Strabismic Amblyopia: Evidence for a Two Type Classification. Vis. Res. 1977, 17, 1049–1055. Available online: https://0-doi-org.brum.beds.ac.uk/10.1016/0042-6989(77)90009-8 (accessed on 26 April 2021). [CrossRef]
- Weakley, D.R. The Association between Nonstrabismic Anisometropia, Amblyopia, and Subnormal Binocularity. Ophthalmology 2001, 108, 163–171. Available online: https://0-doi-org.brum.beds.ac.uk/10.1016/s0161-6420(00)00425-5 (accessed on 26 April 2021). [CrossRef]
- Bradley, A.; Freeman, R.D. Contrast sensitivity in anisometropic amblyopia. Investig. Ophthalmol. Vis. Sci. 1981, 21, 467–476. [Google Scholar]
- Montés-Micó, R.; Ferrer-Blasco, T. Contrast Sensitivity Function in Children: Normalized Notation for the Assessment and Diagnosis of Diseases. Doc. Ophthalmol. 2001, 103, 175–186. Available online: https://0-doi-org.brum.beds.ac.uk/10.1023/a:1013082523019 (accessed on 26 April 2021). [CrossRef]
- Abrahamsson, M.; Sjostrand, J. Contrast Sensitivity and Acuity Relationship in Strabismic and Anisometropic Amblyopia. Br. J. Ophthalmol. 1988, 72, 44–49. Available online: https://0-doi-org.brum.beds.ac.uk/10.1136/bjo.72.1.44 (accessed on 26 April 2021). [CrossRef] [Green Version]
- Campos, E.C. Amblyopia Revisited: Evidence for the Heterogeneity of the Syndrom. Int. Ophthalmol. 1989, 13, 327–330. Available online: https://0-doi-org.brum.beds.ac.uk/10.1007/bf02279869 (accessed on 26 April 2021). [CrossRef]
- Birch, E.E. Amblyopia and Binocular Vision. Prog. Retin. Eye Res. 2013, 33, 67–84. Available online: https://pubmed.ncbi.nlm.nih.gov/23201436/ (accessed on 26 April 2021).
- Levi, D.M. Visual Processing in Amblyopia: Human Studies. Strabismus 2006, 14, 11–19. [Google Scholar] [CrossRef]
- Agrawal, R.; Conner, I.P.; Odom, J.V.; Schwartz, T.L.; Mendola, J.D. Relating Binocular and Monocular Vision in Strabismic and Anisometropic Amblyopia. Arch. Ophthalmol. 2006, 124, 844–850. [Google Scholar] [CrossRef] [Green Version]
- Rutstein, R.P.; Corliss, D. Relationship between Anisometropia, Amblyopia, and Binocularity. Optom. Vis. Sci. 1999, 76, 229–233. Available online: https://pubmed.ncbi.nlm.nih.gov/10333185/ (accessed on 26 April 2021).
- Carlton, J.; Kaltenthaler, E. Amblyopia and Quality of Life: A Systematic Review. Eye 2011, 25, 403–413. Available online: https://pubmed.ncbi.nlm.nih.gov/21274010/ (accessed on 26 April 2021).
- Al-Yahya, A.; Al-Odan, K.; Allam, K.; Al-Onazi, B.; Mousa, A.; Al-Saleh, A.A. Compliance to Patching in the Treatment of Amblyopia. Saudi J. Ophthalmol. 2012, 26, 305–307. Available online: https://0-doi-org.brum.beds.ac.uk/10.1016/j.sjopt.2012.05.003 (accessed on 26 April 2021). [CrossRef] [Green Version]
- Bogdanici, S.T.; Roman, A.; Bogdanici, C. School Integration for Patients with Amblyopia. Rom. J. Ophthalmol. 2015, 59, 48–51. [Google Scholar]
- Olson, R.J.; Scott, W.E. A Practical Approach to Occlusion Therapy for Amblyopia. Semin. Ophthalmol. 1997, 12, 161–165. Available online: https://0-doi-org.brum.beds.ac.uk/10.3109/08820539709059814 (accessed on 26 April 2021). [CrossRef]
- The Pediatric Eye Disease Investigator Group. A Randomized trial of Atropine vs Patching for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2002, 120, 268–278. Available online: https://pubmed.ncbi.nlm.nih.gov/11879129/ (accessed on 26 April 2021).
- Granet, D.B.; Christian, W.; Gomi, C.F.; Banuelos, L.; Castro, E. Treatment Options for Anisohyperopia. J. Pediatr. Ophthalmol. Strabismus 2006, 43, 207–211. Available online: https://pubmed.ncbi.nlm.nih.gov/16915898/ (accessed on 22 April 2021).
- Ganesh, A.; Al-Zuhaibi, S.; Al-Harthi, I.; Cooymans, P.; Al-Busaidi, A.; Al-Farsi, Y. Compliance of Amblyopic Patients with Occlusion Therapy: A Pilot Study. Oman J. Ophthalmol. 2009, 2, 67–72. Available online: https://0-doi-org.brum.beds.ac.uk/10.4103/0974-620x.53035 (accessed on 26 April 2021). [CrossRef]
- Moseley, M.J.; Fielder, A.R.; Irwin, M.; Jones, H.S.; Auld, R.J. Effectiveness of Occlusion Therapy in Ametropic Amblyopia: A Pilot Study. Br. J. Ophthalmol. 1997, 81, 956–961. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.-J.; Kim, S.-J. Effectiveness of Binocularity-Stimulating Treatment in Children with Residual Amblyopia following Occlusion. BMC Ophthalmol. 2018, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Fotouhi, A.; Yekta, A.; Pakzad, R.; Ostadimoghaddam, H.; Khabazkhoob, M. Global and Regional Estimates of Prevalence of Refractive Errors: Systematic Review and Meta-Analysis. J. Curr. Ophthalmol. 2017, 30, 3–22. Available online: https://pubmed.ncbi.nlm.nih.gov/29564404/ (accessed on 26 April 2021).
- Al-Rowaily, M.A. Prevalence of refractive errors among pre-school children at King Abdulaziz Medical City, Riyadh, Saudi Arabia. Saudi J. Ophthalmol. 2010, 24, 45–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Wadaani, F.A.; Amin, T.T.; Ali, A.; Khan, A.R. Prevalence and Pattern of Refractive Errors among Primary School Children in Al Hassa, Saudi Arabia. Glob. J. Health Sci. 2012, 5, 125–134. Available online: https://pubmed.ncbi.nlm.nih.gov/23283044/ (accessed on 26 April 2021).
- Abolfotouh, A.M.; Badawi, I.; Faheem, Y. Prevalence of Amblyopia among Schoolboys in Abha City, Asir Region, Saudi Arabia. J. Egypt. Public Health Assoc. 1994, 69, 19–30. Available online: https://europepmc.org/article/med/7775892 (accessed on 22 April 2021).
- Aldebasi, Y.H. Prevalence of Amblyopia in Primary School Children in Qassim Province, Kingdom of Saudi Arabia. Middle East Afr. J. Ophthalmol. 2015, 22, 86. [Google Scholar] [CrossRef] [Green Version]
- Rafiei, M.; Rivakani, F.; Torabi, L.; Alaeddini, F.; Safiri, S. Community-Based Amblyopia Screening Program for Early Detection in Iran: A Repeated Cross-Sectional Study from 1996 to 2013. Public Health 2015, 142, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Bronsard, A.; Geneau, R.; Shirima, S.; Courtright, P.; Mwende, J. Why are Children Brought Late for Cataract Surgery? Qualitative Findings from Tanzania. Ophthalmic Epidemiol. 2008, 15, 383–388. [Google Scholar] [CrossRef]
- Alsaqr, A.M.; Masmali, A.M. The awareness of amblyopia among parents in Saudi Arabia. Ther. Adv. Ophthalmol. 2019, 11, 2515841419868103. [Google Scholar] [CrossRef] [Green Version]
- Wallace, D.K.; Morse, C.L.; Melia, M.; Sprunger, D.T.; Repka, M.X.; Lee, K.A.; Christiansen, S.P. American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision Screening in the Primary Care and Community Setting; II. Comprehensive Ophthalmic Ex-amination. Ophthalmology 2018, 125, 184–227. [Google Scholar]
- Freedman, H. Vision Screening. Ophthalmology 2006, 113, 1248–1249. [Google Scholar] [CrossRef]
- Alsaqr, A.M.; Ibrahim, G.; Abu Sharha, A.; Fagehi, R. Investigating the visual status of preschool children in Riyadh, Saudi Arabia. Middle East Afr. J. Ophthalmol. 2017, 24, 190–194. [Google Scholar] [CrossRef]
- Nirmalan, P.K.; Sheeladevi, S.; Tamilselvi, V.; Victor, A.C.L.; Vijayalakshmi, P.; Rahmathullah, L. Perceptions of Eye Diseases and Eye Care Needs of Children among Parents in Rural South India: The Kariapatti Pediatric Eye Evaluation Project (KEEP). Indian J. Ophthalmol. 2004, 52, 163–167. Available online: https://journals.lww.com/ijo/Fulltext/2004/52020/Perceptions_of_Eye_Diseases_and_Eye_Care_Needs_of.15.aspx (accessed on 26 April 2021).
- Loudon, S.; Passchier, J.; Chaker, L.; De Vos, S.; Fronius, M.; Harrad, R.; Looman, C.; Simonsz, B.; Simonsz, H. Psychological causes of non-compliance with electronically monitored occlusion therapy for amblyopia. Br. J. Ophthalmol. 2009, 93, 1499–1503. [Google Scholar] [CrossRef]
- Karlica, D.; Matijević, S.; Galetović, D.; Znaor, L. Parents’ influence on the treatment of amblyopia in children. Acta Clin. Croat. 2009, 48, 427–430. [Google Scholar]
- Su, Z.; Marvin, E.K.; Wang, B.Q.; van Zyl, T.; Elia, M.D.; Garza, E.N.; Salchow, D.J.; Forster, S.H. Identifying barriers to follow-up eye care for children after failed vision screening in a primary care setting. J. Am. Assoc. Pediatric Ophthalmol. Strabismus 2013, 17, 385–390. [Google Scholar] [CrossRef]
- Senthilkumar, D.; Balasubramaniam, S.M.; Kumaran, S.E.; Ramani, K.K. Parents’ Awareness and Perception of Children’s Eye Diseases in Chennai, India. Optom. Vis. Sci. 2013, 90, 1462–1466. Available online: https://journals.lww.com/00006324-201312000-00017 (accessed on 22 April 2021).
- Ebeigbe, J.A.; Emedike, C.M. Parents’ awareness and perception of children’s eye diseases in Nigeria. J. Optom. 2016, 10, 104–110. [Google Scholar] [CrossRef]
- Alzahrani, N. Awareness, perceptions and knowledge of amblyopia among pediatrics and oph-thalmology clinics attendees in king abdulaziz university hospital, jeddah. Int. J. Adv. Res. 2018, 6, 1506–1517. [Google Scholar] [CrossRef] [Green Version]
- Alshaheen, A.; Yaqub, A.O.; Adi, M. Amblyopia: Parents’ Awareness and Perceptions in Alhassa Region of Saudi Arabia. Indo Am. J. Pharm. Sci. 2018, 5, 16847–16857. [Google Scholar]
- Raosoft Inc. RaoSoft Sample Size Calculator. 2004. Available online: http://www.raosoft.com/samplesize.html (accessed on 8 September 2021).
- Alhaddab, M.M.; Moukaddem, A.; Albaqami, B.D. Awareness, Knowledge, and Perception of Amblyopia among Parents Attending Pediatric and Ophthalmology Clinics at Kasch Riyadh. Int. J. Adv. Res. (IJAR) 2019. Available online: https://0-doi-org.brum.beds.ac.uk/10.21474/ijar01/10032 (accessed on 8 September 2021). [CrossRef] [Green Version]
- Sullivan, G.M.; Artino, A. Analyzing and Interpreting Data from Likert-Type Scales. J. Grad. Med. Educ. 2013, 5, 541–542. [Google Scholar] [CrossRef] [Green Version]
- Plackett, R.L. Karl Pearson and the Chi-squared Test, International Statistical Review/Revue Internationale de Statistique. JSTOR 1983, 51, 59–72. [Google Scholar]
- Al-Lahim, W.A.; Al-Ghofaili, R.S.; Mirghani, H. Evaluation of Awareness and Attitudes towards Common Eye Diseases among the General Population of Northwestern Saudi Arabia. J. Hosp. Med. 2018, 70, 1983–1989. [Google Scholar]
- Ebeigbe, J.A.; Emedike, C.M. Concienciacixn y Percepción de los Padres Sobre las Enfermedades Oculares Infantiles en Nigeria. 2017. Available online: https://pubmed.ncbi.nlm.nih.gov/27423689/ (accessed on 26 April 2021).
- Singh, A.; Rana, V.; Patyal, S.; Kumar, S.; Mishra, S.; Sharma, V. To Assess Knowledge and Attitude of Parents toward Children Suffering from Strabismus in Indian Subcontinent. Indian J. Ophthalmol. 2017, 65, 603–606. Available online: http://www.ijo.in/text.asp?2017/65/7/603/211125 (accessed on 26 April 2021).



| Frequency | Percent | ||
|---|---|---|---|
| Gender | Male | 116 | 35.7 |
| Female | 209 | 64.3 | |
| Age | 20 to less than 35 years | 76 | 23.4 |
| 35–50 years | 200 | 61.5 | |
| Above 50 years | 49 | 15.1 | |
| Marital Status | Married | 294 | 90.5 |
| Separated | 25 | 7.7 | |
| Widow/widower | 6 | 1.8 | |
| Occupational status | Employed | 202 | 62.2 |
| Unemployed | 12 | 3.7 | |
| Housewife | 28 | 8.6 | |
| Retired | 66 | 20.3 | |
| Other | 17 | 5.2 | |
| Education | Less than High school diploma/least | 33 | 10.2 |
| High school diploma/least | 11 | 3.4 | |
| College degree | 217 | 66.8 | |
| Diploma | 20 | 6.2 | |
| Master’s Degree | 35 | 10.8 | |
| PhD | 7 | 2.2 | |
| Do any of your children have amblyopia? | No | 286 | 88 |
| Yes | 39 | 12 | |
| Do you or your partner have any eye diseases? | No | 228 | 70.2 |
| Yes | 97 | 29.8 | |
| Do any of your children have eye diseases? | No | 220 | 67.7 |
| Yes | 105 | 32.3 | |
| Have you been diagnosed with amblyopia before? | No | 302 | 92.9 |
| Yes | 23 | 7.1 | |
| Correct Answers | % | ||
|---|---|---|---|
| n | |||
| Awareness | What is the definition of amblyopia? | 56 | 17.3% |
| What are the causes of amblyopia? | 54 | 16.7% | |
| Which age group can amblyopia affect? | 226 | 69.8% | |
| The eye of my child externally looks healthy, so is there a need for an eye examination? | 144 | 44.4% | |
| Most cases are discovered accidentally, so is it essential for an ophthalmologist to screen and examine the child’s eye? | 280 | 86.4% | |
| Can a pediatrician diagnose amblyopia? | 116 | 35.8% | |
| Does closing the eyes for a short time or pressing them while watching TV considered a sign that indicates the possibility of amblyopia? | 166 | 51.2% | |
| Is it difficult for parents to notice this problem because the child cannot know that his/her vision is weak? | 174 | 53.7% | |
| Is it essential to examine the child’s visual acuity before school entrance to ensure the normal development of vision? | 299 | 92.3% | |
| What is the recommended number of vision screenings for a child aged (6–12) years? | 181 | 55.9% | |
| Do you take your child for a routine vision screening? | 45 | 13.9% | |
| Is there a treatment for amblyopia? | 183 | 56.5% | |
| Do you think the treatment must be at an early age? | 248 | 76.5% | |
| What is the best age range to treat amblyopia? | 110 | 34.0% | |
| Do you think amblyopia becomes worse if left untreated at an early age? | 256 | 79.0% | |
| Level of Awareness | n | % |
|---|---|---|
| Poor | 113 | 35 |
| Fair | 202 | 62 |
| Good | 10 | 3 |
| Total | 325 | 100 |
| Gender | Level of Awareness | ||||
|---|---|---|---|---|---|
| Poor n (%) | Fair n (%) | Good n (%) | Total n (%) | p-Value * | |
| Male | 43 (37.1) | 72 (62) | 1 (0.9) | 116 (100) | 0.207 |
| Female | 70 (33.5) | 130 (62.2) | 9 (4.3) | 209 (100) | |
| Level of Awareness | ||||
|---|---|---|---|---|
| Poor n (%) | Fair n (%) | Good n (%) | p-Value * | |
| The Presence of Eye Diseases in Children | ||||
| Yes | 32 (28.3) | 67 (33.2) | 6 (60) | 0.111 |
| No | 81 (71.7) | 135 (66.8) | 4 (40) | |
| Total n (%) | 113 (100) | 202 (100) | 10 (100) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alatawi, A.; Alali, N.; Alamrani, A.; Hashem, F.; Alhemaidi, S.; Alreshidi, S.; Albalawi, H. Amblyopia and Routine Eye Exam in Children: Parent’s Perspective. Children 2021, 8, 935. https://0-doi-org.brum.beds.ac.uk/10.3390/children8100935
Alatawi A, Alali N, Alamrani A, Hashem F, Alhemaidi S, Alreshidi S, Albalawi H. Amblyopia and Routine Eye Exam in Children: Parent’s Perspective. Children. 2021; 8(10):935. https://0-doi-org.brum.beds.ac.uk/10.3390/children8100935
Chicago/Turabian StyleAlatawi, Alhanouf, Naif Alali, Abrar Alamrani, Faris Hashem, Seham Alhemaidi, Shaker Alreshidi, and Hani Albalawi. 2021. "Amblyopia and Routine Eye Exam in Children: Parent’s Perspective" Children 8, no. 10: 935. https://0-doi-org.brum.beds.ac.uk/10.3390/children8100935