Modesty and Security: Attributes Associated with Comfort and Willingness to Engage in Telelactation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedures
2.2. Measures
2.2.1. Breastfeeding Initiation
2.2.2. Willingness to Use Telelactation Services
2.2.3. Beliefs Regarding Use of Telelactation Services
2.3. Participant Characteristics
3. Analyses
4. Results
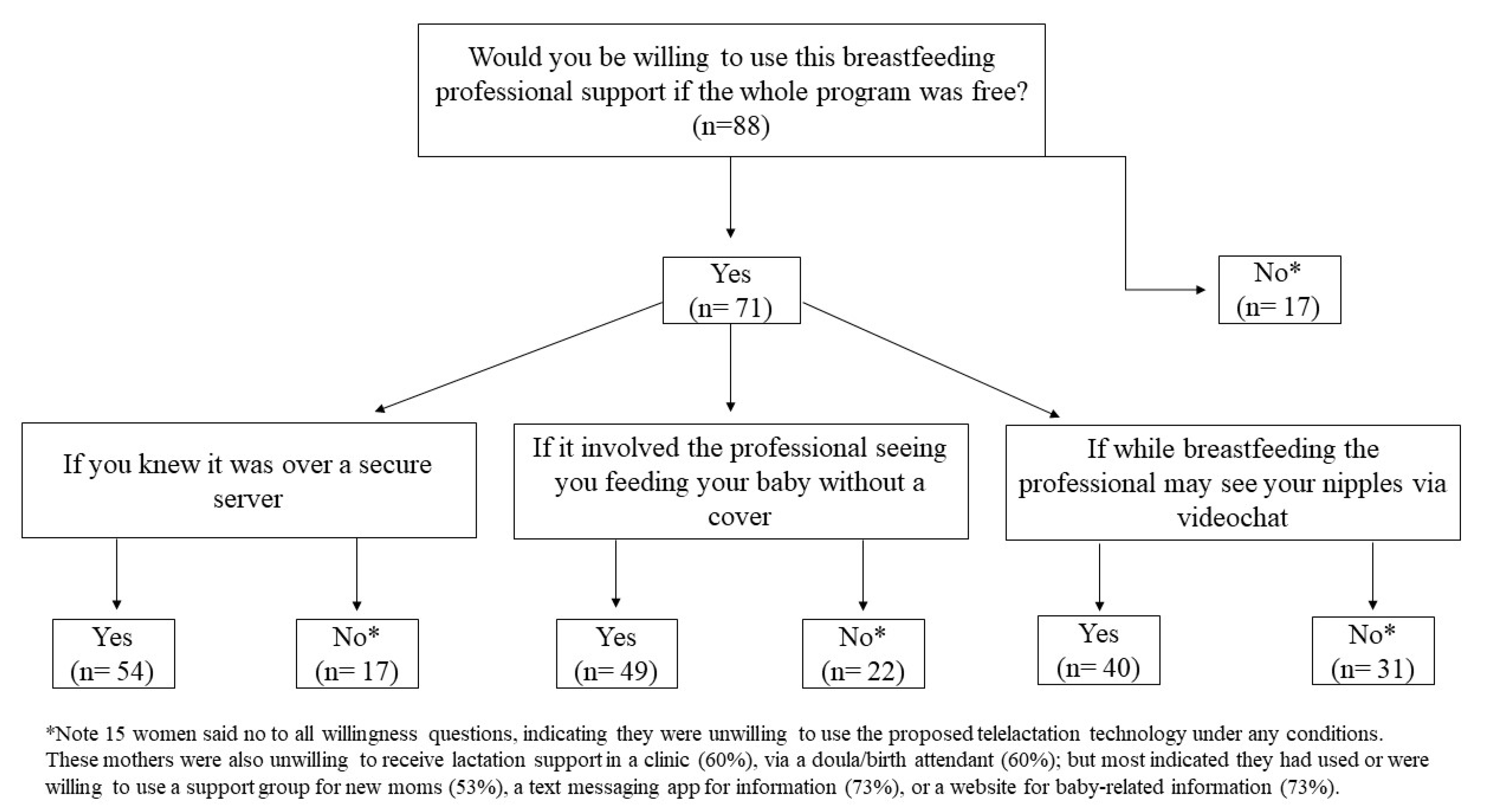
4.1. Willingness and Beliefs Regarding Telelactation Use
4.2. Participant Characteristics and Willingness and Beliefs Variables
4.3. Participant Characteristics and Discomfort
4.4. Post Hoc Analysis
5. Discussion
Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Louis-Jacques, A.; Stuebe, A. Long-term maternal benefits of breastfeeding: Longer durations of breastfeeding are associated with improved health outcomes for mothers and should be supported by ob/gyns. J. Contemp. OB GYN 2018, 63, 26–30. [Google Scholar]
- BEidelman, A.I.; Schanler, R.J. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef] [Green Version]
- Feltner, C.; Weber, R.P.; Stuebe, A.; Grodensky, C.A.; Orr, C.; Viswanathan, M. Breastfeeding Programs and Policies, Breastfeeding Uptake, and Maternal Health Outcomes in Developed Countries; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2018.
- Breastfeeding Expert Work Group; American College of Obstetricians & Gynecologists Committee on Obstetric Practice. Committee Opinion No. 658: Optimizing support for breastfeeding as part of obstetric practice. J. Obstet. Gynecol. 2016, 127, e86. [Google Scholar] [CrossRef] [PubMed]
- Schafer, E.J.; Buch, E.D.; Campo, S.; Ashida, S. From initiation to cessation: Turning points and coping resources in the breastfeeding experience of first-time mothers. Women Health 2019, 59, 449–463. [Google Scholar] [CrossRef]
- Hinsliff-Smith, K.; Spencer, R.; Walsh, D. Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6–8 weeks). Midwifery 2014, 30, e14–e19. [Google Scholar] [CrossRef]
- Hornsby, P.P.; Gurka, K.K.; Conaway, M.R.; Kellams, A.L. Reasons for early cessation of breastfeeding among women with low income. Breastfeed. Med. 2019, 14, 375–381. [Google Scholar] [CrossRef]
- Morrison, A.H.; Gentry, R.; Anderson, J.J. Mothers’ Reasons for Early Breastfeeding Cessation. Am. J. Matern. Child Nurs. 2019, 44, 325–330. [Google Scholar] [CrossRef]
- Teich, A.S.; Barnett, J.; Bonuck, K. Women’s perceptions of breastfeeding barriers in early postpartum period: A qualitative analysis nested in two randomized controlled trials. Breastfeed. Med. 2014, 9, 9–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grubesic, T.H.; Durbin, K.M. Breastfeeding support: A geographic perspective on access and equity. J. Hum. Lact. 2017, 33, 770–780. [Google Scholar] [CrossRef]
- Eden, A.R.; Anstey, E.H.; Orriola, D.J. Growing the IBCLC workforce: A Florida needs assessment. Hum. Lact. 2018, 34, 148–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friesen, C.A.; Hormuth, L.J.; Petersen, D.; Babbitt, T. Using videoconferencing technology to provide breastfeeding support to low-income women: Connecting hospital-based lactation consultants with clients receiving care at a community health center. J. Hum. Lact. 2015, 31, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Habibi, M.F.; Nicklas, J.; Spence, M.; Hedberg, S.; Magnuson, E.; Kavanagh, K.F. Remote lactation consultation: A qualitative study of maternal response to experience and recommendations for survey development. J. Hum. Lact. 2012, 28, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Habibi, M.F.; Springer, C.M.; Spence, M.L.; Hansen-Petrik, M.B.; Kavanagh, K.F. Use of Videoconferencing for Lactation Consultation: An Online Cross-Sectional Survey of Mothers’ Acceptance in the United States. J. Hum. Lact. 2018, 34, 313–321. [Google Scholar] [CrossRef]
- Kapinos, K.; Kotzias, V.; Bogen, D.; Ray, K.; Demirci, J.; Rigas, M.A.; Uscher-Pines, L. The Use of and Experiences With Telelactation Among Rural Breastfeeding Mothers: Secondary Analysis of a Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e13967. [Google Scholar] [CrossRef]
- Marcucci, B. Use of Telehealth to Increase Breastfeeding Exclusivity and Duration. Clin. Lact. 2018, 9, 66–71. [Google Scholar] [CrossRef]
- Rojjanasrirat, W.; Nelson, E.-L.; Wambach, K.A. A pilot study of home-based videoconferencing for breastfeeding support. J. Hum. Lact. 2012, 28, 464–467. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Mehrotra, A.; Bogen, D.L. The emergence and promise of telelactation. Am. J. Obstet. Gynecol. 2017, 217, 176–178.e171. [Google Scholar] [CrossRef]
- Demirci, J.; Kotzias, V.; Bogen, D.L.; Ray, K.N.; Uscher-Pines, L. Telelactation via mobile app: Perspectives of rural mothers, their care providers, and lactation consultants. Telemed. Health 2019, 25, 853–858. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Ghosh-Dastidar, B.; Bogen, D.L.; Ray, K.N.; Demirci, J.R.; Mehrotra, A.; Kapinos, K.A. Feasibility and Effectiveness of Telelactation Among Rural Breastfeeding Women. Acad. Pediatrics 2019. [Google Scholar] [CrossRef]
- Parasuraman, A. Technology Readiness Index (TRI) a multiple-item scale to measure readiness to embrace new technologies. J. Serv. Res. 2000, 2, 307–320. [Google Scholar] [CrossRef]
- Parasuraman, A.; Colby, C.L. An Updated and Streamlined Technology Readiness Index:TRI 2.0. J. Serv. Res. 2015, 18, 59–74. [Google Scholar] [CrossRef]
- Project, P. Pew Internet and American Life Project. Available online: https://www.loc.gov/item/lcwaN0003976/ (accessed on 21 May 2020).
- Sriraman, N.K.; Kellams, A. Breastfeeding: What are the Barriers? Why Women Struggle to Achieve Their Goals. J. Women Health 2016, 25, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Breastfeeding among U.S. Children Born 2000–2016, CDC National Immunization Survey. Available online: https://www.cdc.gov/breastfeeding/data/nis_data/results.html (accessed on 1 December 2020).
- Centers for Disease Control and Prevention. Rates of Any and Exclusive Breastfeeding by Socio-demographics among Children Born in 2016. Available online: https://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2016.htm (accessed on 14 December 2019).
- Deubel, T.F.; Miller, E.M.; Hernandez, I.; Boyer, M.; Louis-Jacques, A. Perceptions and Practices of Infant Feeding among African American Women. Ecol. Food Nutr. 2019, 58, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Louis-Jacques, A.; Deubel, T.F.; Taylor, M.; Stuebe, A.M. Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin. Perinatol. 2017, 41, 299–307. [Google Scholar] [CrossRef] [Green Version]
- Hunt, A.T. Telelactation and Breastfeeding Outcomes among Low-Income Mothers in Mississippi: A Retrospective Cohort Study; ProQuest 2018; Dissertation University of Nevada: Las Vegas, NV, USA, 2018. [Google Scholar]
- Bartick, M.C.; Jegier, B.J.; Green, B.D.; Schwarz, E.B.; Reinhold, A.G.; Stuebe, A.M. Disparities in Breastfeeding: Impact on Maternal and Child Health Outcomes and Costs. J. Pediatrics 2017, 181, 49–55.e46. [Google Scholar] [CrossRef]
- Marhefka, S.L.; Lockhart, E.; Turner, D.; Wang, W.; Dolcini, M.M.; Baldwin, J.A.; Roig-Romero, R.M.; Lescano, C.M.; Glueckauf, R.L. Social Determinants of Potential eHealth Engagement Among People Living with HIV Receiving Ryan White Case Management: Health Equity Implications from Project TECH. AIDS Behav. 2020, 24, 1463–1475. [Google Scholar] [CrossRef]
- Ahmed, A.; Ouzzani, M. Development and assessment of an interactive web-based breastfeeding monitoring system (LACTOR). Matern. Child Health J. 2013, 17, 809–815. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Breastfeeding Toolkit. 2016. Available online: https://www.acog.org/-/media/project/acog/acogorg/files/pdfs/publications/breastfeedingtoolkit2020.pdf (accessed on 3 March 2021).
- Office on Women’s Health in the U.S. Department of Health and Human Services. Breastfeeding. Available online: https://www.womenshealth.gov/breastfeeding (accessed on 29 May 2020).
- National Center for Immunization and Respiratory Diseases (NCIRD), Centers for Disease Control and Prevention. Coronavirus Disease 2019: Considerations for Inpatient Obstetric Healthcare Settings. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance.html (accessed on 16 April 2020).
- Stuebe, A. Should Infants Be Separated from Mothers with COVID-19? First, Do No Harm. Breastfeed. Med. 2020, 15. ahead of print. [Google Scholar] [CrossRef] [Green Version]
- Davenport, M.H.; Meyer, S.; Meah, V.L.; Strynadka, M.C.; Khurana, R. Moms Are Not OK: COVID-19 and Maternal Mental Health. Front. Glob. Women Health 2020, 1, 1. [Google Scholar] [CrossRef]
- Hermann, A.; Deligiannidis, K.M.; Bergink, V.; Monk, C.; Fitelson, E.M.; Robakis, T.K.; Birndorf, C. Response to SARS-Covid-19-related visitor restrictions on labor and delivery wards in New York City. Arch. Women Ment. Health 2020, 23, 793–794. [Google Scholar] [CrossRef] [Green Version]
- Fetters, A. COVID-19 Is Upending Parents’ Birth Plans. In The Atlantic; Emerson Collective: Palo Alto, CA, USA, 2020. [Google Scholar]
- Riley, T.; Sully, E.; Ahmed, Z.; Biddlecom, A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int. Perspect. Sex. Reprod. Health 2020, 46, 46. [Google Scholar] [CrossRef] [PubMed]
- Capanna, F.; Haydar, A.; McCarey, C.; Bernini Carri, E.; Bartha Rasero, J.; Tsibizova, V.; Helmer, H.; Makatsarya, A.; Di Renzo, G. Preparing an obstetric unit in the heart of the epidemic strike of COVID-19: Quick reorganization tips. J. Matern. Fetal Neonatal Med. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, A. Breastfeeding as a public health responsibility: A review of the evidence. J. Hum. Nutr. Diet. 2017, 30, 759–770. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [Green Version]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S. Shared decision making: A model for clinical practice. J. Gen. Intern. Med. 2012, 27, 1361–1367. [Google Scholar] [CrossRef] [Green Version]
- Marhefka, S.; Lockhart, E.; Turner, D. Achieve Research Continuity During Social Distancing by Rapidly Implementing Individual and Group Videoconferencing with Participants: Key Considerations, Best Practices, and Protocols. AIDS Behav. 2020. [Google Scholar] [CrossRef] [Green Version]
- Office for Civil Rights, D. Notification of Enforcement Discretion for Telehealth Remote Communications during the COVID-19 Nationwide Public Health Emergency. Available online: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (accessed on 16 April 2020).
- Chetwynd, E.M.; Wasser, H.M.; Poole, C. Breastfeeding Support Interventions by International Board Certified Lactation Consultants: A Systemic Review and Meta-Analysis. J. Hum. Lact. 2019, 35, 424–440. [Google Scholar] [CrossRef]
- Haase, B.; Brennan, E.; Wagner, C.L. Effectiveness of the IBCLC: Have we Made an Impact on the Care of Breastfeeding Families Over the Past Decade? J. Hum. Lact. 2019, 35, 441–452. [Google Scholar] [CrossRef] [PubMed]

| Would You Be Willing to Use This Professional Breastfeeding Support Program If: |
|---|
| It cost $300 a month and there would be little or no wait times for help |
| It cost $210 a month and there might be a 5–10 min wait time for help |
| The first session was free |
| The professional spoke English but was from a different culture |
| The professional spoke English but lived outside the United States |
| Your doctor suggested it |
| It provided info on local resources |
| While breastfeeding the professional may see your nipples via videochat |
| It involved the professional seeing you feeding your baby without a cover |
| You knew it was over a secure server |
| The whole program was free |
| Characteristics | |
|---|---|
| Age (years, mean ± SD) | 29.3 ± 5.05 |
| N (%) | |
| Married | 48 (54.5) |
| Working (full or part time or self-employed) | 29 (33.0) |
| Income USD 50 K or more | 33 (37.5) |
| Race/Ethnicity * | |
| Black 1 | 22 (25.0) |
| White 1 | 45 (51.1) |
| Hispanic 1 | 22 (25.0) |
| Has access to… | |
| Desktop, laptop, netbook, or notebook computer | 72 (81.8) |
| Tablet computer (iPad, Samsung Galaxy, Windows Tablet) | 58 (65.9) |
| Mobile phone with text messaging | 82 (93.2) |
| Smart mobile phone (iPhone or Android) | 83 (94.3) |
| Use the Internet to videochat (Skype, Oovo, FaceTime) | 47 (53.4) |
| Willing (probably yes or definitely yes vs. other responses) to use telelactation if… | |
| The whole program was free | 71 (80.7) |
| You knew it was over a secure server | 56 (63.6) |
| It involved the professional seeing you feeding your baby without a cover | 49 (55.7) |
| While breastfeeding the professional may see your nipples via Videochat | 40 (45.5) |
| Beliefs (agree or strongly agree vs. other responses) about using mobile phone for telelactation | |
| Videochat can provide access to breastfeeding support wherever women need it | 57 (64.8) |
| If you use video-based breastfeeding support over a computer or Internetyou can never be sure who will have access | 43 (48.9) |
| I do not feel comfortable with accessing video-based breastfeeding support online | 23 (26.1) |
| Videochat is good for some things, but not for getting help with breastfeeding | 19 (21.6) |
| Women will not develop a personal relationship with breastfeeding support professional | 18 (20.5) |
| Use of (or willingness to use) other lactation support services | |
| Website for baby-related information | 80 (90.9) |
| Text4Baby (a service that gives useful information to mothers via text) | 67 (76.1) |
| Breastfeeding consulting at clinic | 58 (65.9) |
| Breastfeeding help from a doula or traditional birth attendant | 58 (65.9) |
| Support group for new moms | 56 (63.6) |
| Willing (Probably Yes or Definitely Yes vs. Other Responses) to Use Telelactation If… | Belief (Agree or Strongly Agree vs. Other Responses) about Using Mobile Phone for Telelactation | |||||
|---|---|---|---|---|---|---|
| The Whole Program Was Free | You Knew It Was over a Secure Server | It Involved the Professional Seeing You Feeding Your Baby without a Cover | While Breastfeeding the Professional May See Your Nipples | Videochat Can Provide Access to Breastfeeding Support Wherever Women Need It | Women Will Not Develop a Personal Relationship with the Breastfeeding Support Professional | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | NS | NS | NS | NS | 1.17 (1.05–1.30) ** | NS |
| Married 1 | 3.69 (1.17–1.60) * | 7.50 (2.79–20.15) *** | 6.23 (2.46–15.79) *** | 5.00 (1.99–12.60) ** | 4.20 (1.65–10.68) ** | NS |
| Income 2 | NS | 4.03 (1.44–11.31) ** | 3.20 (1.26–8.13) * | 3.32 (1.35–8.16) ** | 5.02 (1.69–14.92) ** | NS |
| Black 3 | NS | 0.36 (0.14–0.98) * | 0.35 (0.13–0.95) * | NS | NS | NS |
| White 3 | NS | 4.60 (1.79–11.83) ** | 3.77 (1.55–9.15) ** | 4.36 (1.73–10.45) ** | 2.69 (1.09–6.65) * | 0.29 (0.09–0.90) * |
| Has used Videochat | NS | 3.44 (1.28–8.55) ** | 3.68 (1.52–8.93) ** | 2.39 (1.01–5.67) * | NS | NS |
| Attributes | Full Model 3 OR (95% CI) | Final Model 4 OR (95% CI) |
|---|---|---|
| Willing to use telelactation if while breastfeeding the professional may see your nipples 1 | 0.19 (0.03–1.04) | 0.20 (0.05–0.89) * |
| Willing to use telelactation if it involved the professional seeing you feeding your baby without a cover 1 | 1.18 (0.28–4.87) | -- |
| Agree if you use video-based breastfeeding support over a computer or Internet you can never be sure who will have access 2 | 6.49 (1.83–23.06) ** | 6.32 (1.82–21.98) ** |
| Agree videochat can provide access to breastfeeding support wherever women need it 2 | 0.28 (0.08–0.98) * | 0.29 (0.08–0.99) * |
|
|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Louis-Jacques, A.F.; Schafer, E.J.; Livingston, T.A.; Logan, R.G.; Marhefka, S.L. Modesty and Security: Attributes Associated with Comfort and Willingness to Engage in Telelactation. Children 2021, 8, 271. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040271
Louis-Jacques AF, Schafer EJ, Livingston TA, Logan RG, Marhefka SL. Modesty and Security: Attributes Associated with Comfort and Willingness to Engage in Telelactation. Children. 2021; 8(4):271. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040271
Chicago/Turabian StyleLouis-Jacques, Adetola F., Ellen J. Schafer, Taylor A. Livingston, Rachel G. Logan, and Stephanie L. Marhefka. 2021. "Modesty and Security: Attributes Associated with Comfort and Willingness to Engage in Telelactation" Children 8, no. 4: 271. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040271






