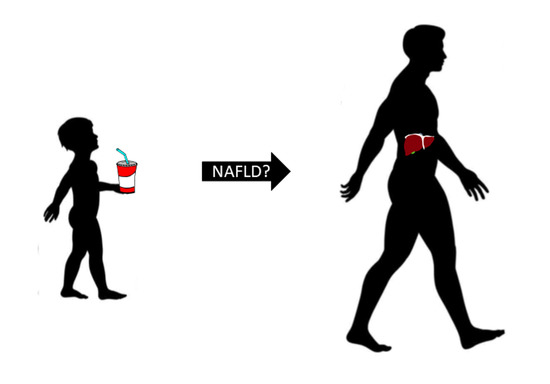
Associations between Free Sugar and Sugary Beverage Intake in Early Childhood and Adult NAFLD in a Population-Based UK Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Free Sugar and Sugary Beverage Intake at Three Years of Age
2.3. Assessment of Liver Outcomes
2.4. Covariates
2.5. Inclusion/Exclusion
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Welsh, J.A.; Karpen, S.; Vos, M.B. Increasing Prevalence of Nonalcoholic Fatty Liver Disease among United States Adolescents, 1988–1994 to 2007–2010. J. Pediatr. 2013, 162, 496–500.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldstein, A.E.; Charatcharoenwitthaya, P.; Treeprasertsuk, S.; Benson, J.T.; Enders, F.B.; Angulo, P. The natural history of non-alcoholic fatty liver disease in children: A follow-up study for up to 20 years. Gut 2009, 58, 1538–1544. [Google Scholar] [CrossRef]
- Vernon, G.; Baranova, A.; Younossi, Z.M. Systematic review: The epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharmacol. Ther. 2011, 34, 274–285. [Google Scholar] [CrossRef]
- Hagström, H.; Höijer, J.; Ludvigsson, J.F.; Bottai, M.; Ekbom, A.; Hultcrantz, R.; Stephansson, O.; Stokkeland, K. Adverse outcomes of pregnancy in women with non-alcoholic fatty liver disease. Liver Int. 2016, 36, 268–274. [Google Scholar] [CrossRef]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: New York, NY, USA, 2015. [Google Scholar]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: New York, NY, USA, 2003. [Google Scholar]
- Welsh, J.A.; Wang, Y.; Figueroa, J.; Brumme, C. Sugar intake by type (added vs. naturally occurring) and physical form (liquid vs. solid) and its varying association with children’s body weight, NHANES 2009–2014. Pediatr. Obes. 2018, 13, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Scientific Advisory Committee on Nutrition; Carbohydrates and Health: London, UK, 2015.
- Roberts, C.; Steer, T.; Maplethorpe, N.; Cox, L.; Meadows, S.; Nicholson, S.; Polly, P.; Gillian, S. National Diet and Nutrition Survey: Results from Years 7 and 8 (Combined) of the Rolling Programme (2014/2015–2015/2016); Public Health England: London, UK, 2018.
- Emmett, P.M.; Jones, L.R. Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutr. Rev. 2015, 73 (Suppl. 3), 175–206. [Google Scholar] [CrossRef] [Green Version]
- Mosca, A.; Nobili, V.; De Vito, R.; Crudele, A.; Scorletti, E.; Villani, A.; Alisi, A.; Byrne, C.D. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J. Hepatol. 2017, 66, 1031–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sullivan, J.S.; Le, M.T.; Pan, Z.; Rivard, C.; Love-Osborne, K.; Robbins, K.; Johnson, R.J.; Sokol, R.J.; Sundaram, S.S. Oral fructose absorption in obese children with non-alcoholic fatty liver disease. Pediatr. Obes. 2014, 10, 188–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdelmalek, M.F.; Suzuki, A.; Guy, C.D.; Unalp-Arida, A.; Colvin, R.; Johnson, R.J.; Diehl, A.M. for the Nonalcoholic Steatohepatitis Clinical Research Network Increased fructose consumption is associated with fibrosis severity in patients with nonalcoholic fatty liver disease. Hepatology 2010, 51, 1961–1971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwimmer, J.B.; Ugalde-Nicalo, P.; Welsh, J.A.; Angeles, J.E.; Cordero, M.; Harlow, K.E.; Alazraki, A.; Durelle, J.; Knight-Scott, J.; Newton, K.P.; et al. Effect of a low free sugar diet vs usual diet on nonalcoholic fatty liver disease in adolescent boys: A randomized clinical trial. JAMA 2019, 321, 256–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, C.; Scholtens, P.A.; Lalanne, A.; Weenen, H.; Nicklaus, S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite 2011, 57, 796–807. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.; Golding, J.; Macleod, J.; Lawlor, D.A.; Fraser, A.; Henderson, J.; Molloy, L.; Ness, A.; Ring, S.; Smith, G.D. Cohort profile: The ‘children of the 90s’—The index offspring of the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 2013, 42, 111–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraser, A.; Macdonald-Wallis, C.; Tilling, K.; Boyd, A.; Golding, J.; Smith, G.D.; Henderson, J.; MacLeod, J.; Molloy, L.; Ness, A.; et al. Cohort Profile: The Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int. J. Epidemiol. 2012, 42, 97–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Northstone, K.; Lewcock, M.; Groom, A.; Boyd, A.; Macleod, J.; Timpson, N.; Wells, N. The Avon Longitudinal Study of Parents and Children (ALSPAC): An update on the enrolled sample of index children in 2019. Wellcome Open Res. 2019, 4, 51. [Google Scholar] [CrossRef] [Green Version]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- University of Bristol. Explore Data and Samples. Available online: http://www.bristol.ac.uk/alspac/researchers/our-data/ (accessed on 7 April 2021).
- Avon Longitudinal Study of Parents and Children. Available online: http://www.bristol.ac.uk/alspac/ (accessed on 7 April 2021).
- Wrieden, W.L.; Longbottom, P.J.; Adamson, A.J.; Ogston, S.A.; Payne, A.; Haleem, M.A.; Barton, K.L. Estimation of typical food portion sizes for children of different ages in Great Britain. Br. J. Nutr. 2008, 99, 1344–1353. [Google Scholar] [CrossRef] [Green Version]
- Holland, B.; Welch, A.; Unwin, I.; Buss, D.; Paul, A.; Southgate, D. McCance and Widdowson’s the Composition of Foods; Royal Society of Chemistry: London, UK, 1991. [Google Scholar]
- Geurtsen, M.L.; Santos, S.; Gaillard, R.; Felix, J.F.; Jaddoe, V.W.V. Associations Between Intake of Sugar-Containing Beverages in Infancy with Liver Fat Accumulation at School Age. Hepatology 2021, 73, 560–570. [Google Scholar] [CrossRef]
- Voortman, T.; Jong, J.C.K.-D.; Geelen, A.; Villamor, E.; Moll, A.H.; De Jongste, J.C.; Raat, H.; Hofman, A.; Jaddoe, V.W.V.; Franco, O.H.; et al. The Development of a Diet Quality Score for Preschool Children and Its Validation and Determinants in the Generation R Study. J. Nutr. 2014, 145, 306–314. [Google Scholar] [CrossRef]
- Prati, D.; Taioli, E.; Zanella, A.; Della Torre, E.; Butelli, S.; Del Vecchio, E.; Vianello, L.; Zanuso, F.; Mozzi, F.; Milani, S.; et al. Updated Definitions of Healthy Ranges for Serum Alanine Aminotransferase Levels. Ann. Intern. Med. 2002, 137, 1–10. [Google Scholar] [CrossRef]
- Karlas, T.; Petroff, D.; Sasso, M.; Fan, J.G.; Mi, Y.Q.; de Lédinghen, V.; Kumar, M.; Lupsor-Platon, M.; Han, K.-H.; Cardoso, A.C.; et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J. Hepatol. 2017, 66, 1022–1030. [Google Scholar] [CrossRef]
- Bigornia, S.J.; LaValley, M.P.; Noel, E.S.; Moore, L.L.; Ness, A.R.; Newby, P.K. Sugar-sweetened beverage consumption and central and total adiposity in older children: A prospective study accounting for dietary reporting errors. Public Health Nutr. 2014, 18, 1155–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howe, L.D.; Tilling, K.; Galobardes, B.; Smith, G.D.; Ness, A.R.; Lawlor, D.A. Socioeconomic disparities in trajectories of adiposity across childhood. Pediatr. Obes. 2011, 6 (Suppl. 3), e144–e153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- North American Association for the Study of Obesity, National Heart Lung and Blood Institute Obesity Education Initiative. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; National Institutes of Health, National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2000.
- World Health Organization. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee; World Health Organization: New York, NY, USA, 1995. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub.: Washington, DC, USA, 2013. [Google Scholar]
- Kriston, L.; Hölzel, L.; Weiser, A.-K.; Berner, M.M.; Härter, M. Meta-analysis: Are 3 Questions Enough to Detect Unhealthy Alcohol Use? Ann. Intern. Med. 2008, 149, 879–888. [Google Scholar] [CrossRef]
- Sterne, J.A.; Smith, G.D. Sifting the evidence—What’s wrong with significance tests? Phys. Ther. 2001, 81, 1464–1469. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.L.; Howe, L.D.; Fraser, A.; Macdonald-Wallis, C.; Callaway, M.P.; Sattar, N.; Day, C.P.; Tilling, K.; Lawlor, A.D. Childhood Energy Intake Is Associated with Nonalcoholic Fatty Liver Disease in Adolescents. J. Nutr. 2015, 145, 983–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, L.; Mander, A.P.; Jones, L.R.; Emmett, P.M.; Jebb, S.A. Is sugar-sweetened beverage consumption associated with increased fatness in children? Nutrition 2007, 23, 557–563. [Google Scholar] [CrossRef]
- Stanhope, K.L.; Schwarz, J.M.; Keim, N.L.; Griffen, S.C.; Bremer, A.A.; Graham, J.L.; Hatcher, B.; Cox, C.L.; Dyachenko, A.; Zhang, W.; et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Investig. 2009, 119, 1322–1334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwarz, J.-M.; Noworolski, S.M.; Erkin-Cakmak, A.; Korn, N.J.; Wen, M.J.; Tai, V.W.; Jones, G.M.; Palii, S.P.; Velasco-Alin, M.; Pan, K.; et al. Effects of Dietary Fructose Restriction on Liver Fat, De Novo Lipogenesis, and Insulin Kinetics in Children With Obesity. Gastroenterology 2017, 153, 743–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papandreou, D.; Karabouta, Z.; Pantoleon, A.; Rousso, I. Investigation of anthropometric, biochemical and dietary parameters of obese children with and without non-alcoholic fatty liver disease. Appetite 2012, 59, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Mager, D.R.; Patterson, C.; So, S.; Rogenstein, C.D.; Wykes, L.J.; Roberts, A.E. Dietary and physical activity patterns in children with fatty liver. Eur. J. Clin. Nutr. 2010, 64, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.E.; Ramos–Roman, M.A.; Browning, J.D.; Parks, E.J. Increased De Novo Lipogenesis Is a Distinct Characteristic of Individuals With Nonalcoholic Fatty Liver Disease. Gastroenterology 2014, 146, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and BMI in children and adolescents: Reanalyses of a meta-analysis. Am. J. Clin. Nutr. 2009, 89, 438–439. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes. Rev. 2013, 14, 606–619. [Google Scholar] [CrossRef]
- Abeysekera, K.W.M.; Fernandes, G.S.; Hammerton, G.; Portal, A.J.; Gordon, F.H.; Heron, J.; Hickman, M. Prevalence of steatosis and fibrosis in young adults in the UK: A population-based study. Lancet Gastroenterol. Hepatol. 2020, 5, 295–305. [Google Scholar] [CrossRef] [Green Version]
- Elizondo-Montemayor, L.; Ugalde-Casas, P.A.; Lam-Franco, L.; Bustamante-Careaga, H.; Serrano-González, M.; Gutiérrez, N.G.; Martínez, U. Association of ALT and the metabolic syndrome among Mexican children. Obes. Res. Clin. Pr. 2014, 8, e79–e87. [Google Scholar] [CrossRef]
- Romeo, S.; Kozlitina, J.; Xing, C.; Pertsemlidis, A.; Cox, D.; Pennacchio, L.A.; Boerwinkle, E.; Cohen, J.C.; Hobbs, H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008, 40, 1461–1465. [Google Scholar] [CrossRef] [Green Version]


| Variable | Overall | Q1 | Q2 | Q3 | Q4 | Q5 | p-Value |
|---|---|---|---|---|---|---|---|
| N = 3095 | (0.14%–11.5%) | (11.5%–13.5%) | (13.5%–15.3%) | (15.3%–17.7%) | (17.7%–36.5%) | ||
| Free sugars (g) at 3 years | 43.5 (33.6, 54.7) | 28.5 (23.2, 33.6) | 38.4 (32.5, 44.5) | 43.6 (37.3, 50.3) | 50.9 (43.9, 59.0) | 64.9 (52.9, 78.3) | <0.001 |
| TEI (kJ) at 3 years | 5072 (4346, 5858) | 4849 (4074, 5515) | 5095 (4377, 5842) | 5049 (4342, 5800) | 5187 (4486, 6011) | 5287 (4430, 6297) | <0.001 |
| Sugary beverages/day | 1.6 (1.3, 2.0) | 1.4 (0.8, 1.6) | 1.5 (1.1, 1.7) | 1.6 (1.4, 1.9) | 1.7 (1.4, 2.2) | 1.9 (1.5, 2.4) | <0.001 |
| Male sex | 1200 (38.8%) | 234 (37.8%) | 241 (38.9%) | 243 (39.3%) | 250 (40.4%) | 232 (37.5%) | 0.839 |
| Maternal education | |||||||
| CSE/None | 257 (8.3%) | 46 (7.4%) | 40 (6.5%) | 47 (7.6%) | 49 (7.9%) | 75 (12.1%) | <0.001 |
| Vocational | 206 (6.7%) | 43 (6.9%) | 34 (5.5%) | 33 (5.3%) | 39 (6.3%) | 57 (9.2%) | |
| O-level | 1042 (33.7%) | 180 (29.1%) | 197 (31.8%) | 193 (31.2%) | 226 (36.5%) | 246 (39.7%) | |
| A-level | 895 (28.9%) | 202 (32.6%) | 194 (31.3%) | 186 (30.0%) | 170 (27.5%) | 143 (23.1%) | |
| Degree | 657 (21.2%) | 140 (22.6%) | 144 (23.3%) | 153 (24.7%) | 131 (21.2%) | 89 (14.4%) | |
| Maternal BMI | |||||||
| Underweight | 117 (3.8%) | 27 (4.4%) | 32 (5.2%) | 20 (3.2%) | 18 (2.9%) | 20 (3.2%) | 0.09 |
| Normal | 2239 (72.3%) | 442 (71.4%) | 419 (67.7%) | 474 (76.6%) | 458 (74.0%) | 446 (72.1%) | |
| Overweight | 392 (12.7%) | 68 (11.0%) | 98 (15.8%) | 65 (10.5%) | 83 (13.4%) | 78 (12.6%) | |
| Obese | 122 (3.9%) | 29 (4.7%) | 26 (4.2%) | 20 (3.2%) | 21 (3.4%) | 26 (4.2%) | |
| Breastfeeding duration | |||||||
| Never | 468 (15.1%) | 84 (13.6%) | 74 (12.0%) | 80 (12.9%) | 89 (14.4%) | 141 (22.8%) | <0.001 |
| <3 m | 613 (19.8%) | 113 (18.3%) | 118 (19.1%) | 121 (19.5%) | 130 (21.0%) | 131 (21.2%) | |
| 3–5 m | 512 (16.5%) | 107 (17.3%) | 105 (17.0%) | 110 (17.8%) | 116 (18.7%) | 74 (12.0%) | |
| >6 m | 1378 (44.5%) | 284 (45.9%) | 303 (48.9%) | 288 (46.5%) | 262 (42.3%) | 241 (38.9%) | |
| AUDIT-C at 24 yrs | 5 (4, 7) | 5 (3, 7) | 5 (4, 7) | 5 (4, 7) | 6 (4, 7) | 5 (3, 7) | 0.024 |
| BMI at 24 yrs | |||||||
| Underweight | 90 (2.9%) | 16 (2.6%) | 19 (3.1%) | 19 (3.1%) | 18 (3.0%) | 18 (2.9%) | |
| Normal | 1846 (60.2%) | 373 (61.3%) | 359 (58.5%) | 386 (62.6%) | 365 (59.5%) | 363 (59.2%) | 0.7780 |
| Overweight | 762 (24.9%) | 147 (24.4%) | 156 (25.4%) | 147 (23.8%) | 159 (25.9%) | 153 (25.0%) | |
| Obese | 369 (12.0%) | 73 (12.0%) | 80 (13.0%) | 65 (10.5%) | 72 (11.7%) | 79 (12.9%) | |
| Severe hepatic steatosis 1 | 304 (9.8%) | 56 (9.0%) | 52 (8.4%) | 61 (9.9%) | 63 (10.2%) | 72 (11.6%) | 0.378 |
| Q1 (0.14–11.5) | Q2 (11.5–13.5) | Q3 (13.5–15.3) | Q4 (15.3–17.7) | Q5 (17.7–36.6) | Per Quintile | p-Trend | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | n | REF | OR | 95% CL | OR | 95% CL | OR | 95% CL | OR | 95% CL | OR | 95% CL | ||||||
| 1 | 3095 | 1.00 | 0.90 | 0.61 | 1.34 | 1.08 | 0.74 | 1.58 | 1.11 | 0.76 | 1.62 | 1.28 | 0.88 | 1.85 | 1.07 | 0.99 | 1.17 | 0.103 |
| 2 | 2742 | 1.00 | 0.81 | 0.53 | 1.23 | 0.98 | 0.65 | 1.47 | 1.01 | 0.67 | 1.50 | 1.09 | 0.73 | 1.62 | 1.04 | 0.95 | 1.14 | 0.394 |
| 3 | 2715 | 1.00 | 0.67 | 0.41 | 1.08 | 1.04 | 0.65 | 1.66 | 0.99 | 0.62 | 1.58 | 1.14 | 0.72 | 1.82 | 1.07 | 0.96 | 1.19 | 0.204 |
| 4 | 2685 | 1.00 | 0.77 | 0.50 | 1.18 | 0.99 | 0.66 | 1.49 | 0.99 | 0.66 | 1.49 | 1.09 | 0.73 | 1.63 | 1.05 | 0.95 | 1.15 | 0.355 |
| Continuous SB/Day | <1/Day | 1–2/Day | >2/Day | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | n | OR | 95% CL | REF | OR | 95% CL | OR | 95% CL | |||
| 1 | 3088 | 1.04 | 0.87 | 1.24 | 1.00 | 1.25 | 0.89 | 1.77 | 1.23 | 0.82 | 1.84 |
| 2 | 2739 | 1.04 | 0.86 | 1.25 | 1.00 | 1.18 | 0.81 | 1.70 | 1.19 | 0.77 | 1.83 |
| 3 | 2715 | 0.92 | 0.73 | 1.15 | 1.00 | 1.03 | 0.68 | 1.57 | 0.98 | 0.60 | 1.60 |
| 4 | 2682 | 1.03 | 0.85 | 1.25 | 1.00 | 1.19 | 0.82 | 1.73 | 1.20 | 0.78 | 1.86 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekkarie, A.; Welsh, J.A.; Northstone, K.; Stein, A.D.; Ramakrishnan, U.; Vos, M.B. Associations between Free Sugar and Sugary Beverage Intake in Early Childhood and Adult NAFLD in a Population-Based UK Cohort. Children 2021, 8, 290. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040290
Sekkarie A, Welsh JA, Northstone K, Stein AD, Ramakrishnan U, Vos MB. Associations between Free Sugar and Sugary Beverage Intake in Early Childhood and Adult NAFLD in a Population-Based UK Cohort. Children. 2021; 8(4):290. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040290
Chicago/Turabian StyleSekkarie, Ahlia, Jean A. Welsh, Kate Northstone, Aryeh D. Stein, Usha Ramakrishnan, and Miriam B. Vos. 2021. "Associations between Free Sugar and Sugary Beverage Intake in Early Childhood and Adult NAFLD in a Population-Based UK Cohort" Children 8, no. 4: 290. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040290