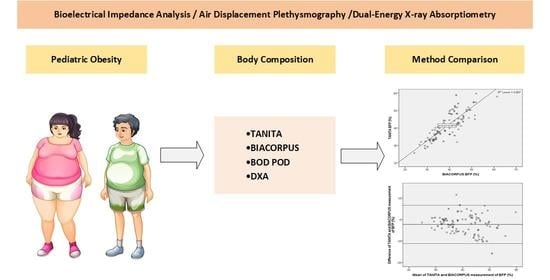
Comparison of Bioelectrical Impedance-Based Methods on Body Composition in Young Patients with Obesity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Recruitment
2.2. Anthropometric Measurements
2.3. Measurements of Body Composition
2.4. TANITA and BIACORPUS
2.5. BOD POD
2.6. DXA
2.7. Statistics
3. Results
3.1. General Characteristics of the Study Population
3.2. Comparison of Bioelectric Impedance-Based Methods
3.3. Comparison of BOD POD- and DXA-Based Determination of Body Composition
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Blüher, M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Bhupathiraju, S.N.; Hu, F.B. Epidemiology of Obesity and Diabetes and Their Cardiovascular Complications. Circ. Res. 2016, 118, 1723–1735. [Google Scholar] [CrossRef]
- Cercato, C.; Fonseca, F.A. Cardiovascular Risk and Obesity. Diabetol. Metab. Syndr. 2019, 11, 1–15. [Google Scholar]
- Allott, E.H.; Hursting, S.D. Obesity and Cancer: Mechanistic Insights from Transdisciplinary Studies. Endocr. Relat. Cancer 2015, 22, R365–R386. [Google Scholar] [CrossRef] [Green Version]
- de Siqueira, J.V.V.; Almeida, L.G.; Zica, B.O.; Brum, I.B.; Barceló, A.; de Siqueira Galil, A.G. Impact of Obesity on Hospitalizations and Mortality, Due to COVID-19: A Systematic Review. Obes. Res. Clin. Pract. 2020. [Google Scholar] [CrossRef]
- Kass, D.A.; Duggal, P.; Cingolani, O. Obesity Could Shift Severe COVID-19 Disease to Younger Ages. Lancet 2020, 395, 1544–1545. [Google Scholar] [CrossRef]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Ward, Z.J.; Long, M.W.; Resch, S.C.; Giles, C.M.; Cradock, A.L.; Gortmaker, S.L. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N. Engl. J. Med. 2017, 377, 2145–2153. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, M.M.; Zaepfel, A.; Bjornstad, P.; Nadeau, K.J. Age-Related Consequences of Childhood Obesity. Gerontology 2014, 60, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S. Consequences of Childhood Obesity. Ann. Acad. Med. Singap. 2009, 38, 75–81. [Google Scholar]
- Must, A.; Jacques, P.F.; Dallal, G.E.; Bajema, C.J.; Dietz, W.H. Long-Term Morbidity and Mortality of Overweight Adolescents. N. Engl. J. Med. 1992, 327, 1350–1355. [Google Scholar] [CrossRef]
- Ward, L.C. Bioelectrical Impedance Analysis for Body Composition Assessment: Reflections on Accuracy, Clinical Utility, and Standardisation. Eur. J. Clin. Nutr. 2019, 73, 194–199. [Google Scholar] [CrossRef]
- Fields, D.A.; Gunatilake, R.; Kalaitzoglou, E. Air Displacement Plethysmography: Cradle to Grave. Nutr. Clin. Pract. 2015, 30, 219–226. [Google Scholar] [CrossRef]
- Shepherd, J.A.; Ng, B.K.; Sommer, M.J.; Heymsfield, S.B. Body Composition by DXA. Bone 2017, 104, 101–105. [Google Scholar] [CrossRef]
- Mast, M.; Körtzinger, I.; König, E.; Müller, M.J. Gender Differences in Fat Mass of 5-7-Year Old Children. Int. J. Obes. 1998, 22, 878–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, L.W.; Liao, Y.S.; Lu, H.K.; Hsiao, P.L.; Chen, Y.Y.; Chi, C.C.; Hsieh, K.C. Validation of Two Portable Bioelectrical Impedance Analyses for the Assessment of Body Composition in School Age Children. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Lohman, T.G.; Going, S.B. Body Composition Assessment for Development of an International Growth Standard for Preadolescent and Adolescent Children. Food Nutr. Bull. 2006, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weber, D.R.; Leonard, M.B.; Zemel, B.S. Body Composition Analysis in the Pediatric Population. Pediatr. Endocrinol. Rev. 2012, 10, 130–139. [Google Scholar]
- Wells, J.C.K.; Williams, J.E.; Chomtho, S.; Darch, T.; Grijalva-Eternod, C.; Kennedy, K.; Haroun, D.; Wilson, C.; Cole, T.J.; Fewtrell, M.S. Body-Composition Reference Data for Simple and Reference Techniques and a 4-Component Model: A New UK Reference Child. Am. J. Clin. Nutr. 2012, 96, 1316–1326. [Google Scholar] [CrossRef] [Green Version]
- Kreissl, A.; Jorda, A.; Truschner, K.; Skacel, G.; Greber-Platzer, S. Clinically Relevant Body Composition Methods for Obese Pediatric Patients. BMC Pediatr. 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; Von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Percentiles of Body Mass Index in Children and Adolescents Evaluated from Different Regional German Studies. Monatsschr. Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef] [Green Version]
- Horsak, B.; Artner, D.; Baca, A.; Pobatschnig, B.; Greber-Platzer, S.; Nehrer, S.; Wondrasch, B. The Effects of a Strength and Neuromuscular Exercise Programme for the Lower Extremity on Knee Load, Pain and Function in Obese Children and Adolescents: Study Protocol for a Randomised Controlled Trial. Trials 2015, 16, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wohlfahrt-Veje, C.; Tinggaard, J.; Winther, K.; Mouritsen, A.; Hagen, C.P.; Mieritz, M.G.; De Renzy-Martin, K.T.; Boas, M.; Petersen, J.H.; Main, K.M. Body Fat throughout Childhood in 2647 Healthy Danish Children: Agreement of BMI, Waist Circumference, Skinfolds with Dual X-Ray Absorptiometry. Eur. J. Clin. Nutr. 2014, 68, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Martin Bland, J.; Altman, D.G. Statistical Methods for Assessing Agreenebt between Two Methods of Clinical Measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Comparing Methods of Measurement: Why Plotting Difference against Standard Method Is Misleading. Lancet 1995, 346, 1085–1087. [Google Scholar] [CrossRef] [Green Version]
- Lazzer, S.; Boirie, Y.; Meyer, M.; Vermorel, M. Evaluation of Two Foot-to-Foot Bioelectrical Impedance Analysers to Assess Body Composition in Overweight and Obese Adolescents. Br. J. Nutr. 2003, 90, 987–992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minderico, C.S.; Silva, A.M.; Keller, K.; Branco, T.L.; Martins, S.S.; Palmeira, A.L.; Barata, J.T.; Carnero, E.A.; Rocha, P.M.; Teixeira, P.J.; et al. Usefulness of Different Techniques for Measuring Body Composition Changes during Weight Loss in Overweight and Obese Women. Br. J. Nutr. 2008, 99, 432–441. [Google Scholar] [CrossRef] [Green Version]
- Leonard, M.B.; Elmi, A.; Mostoufi-Moab, S.; Shults, J.; Burnham, J.M.; Thayu, M.; Kibe, L.; Wetzsteon, R.J.; Zemel, B.S. Effects of Sex, Race, and Puberty on Cortical Bone and the Functional Muscle Bone Unit in Children, Adolescents, and Young Adults. J. Clin. Endocrinol. Metab. 2010, 95, 1681–1689. [Google Scholar] [CrossRef]
- Kirchengast, S. Gender Differences in Body Composition from Childhood to Old Age: An Evolutionary Point of View. J. Life Sci. 2010, 2, 1–10. [Google Scholar] [CrossRef]
- Brantlov, S.; Ward, L.C.; Jødal, L.; Rittig, S.; Lange, A. Critical Factors and Their Impact on Bioelectrical Impedance Analysis in Children: A Review. J. Med. Eng. Technol. 2017, 41, 22–35. [Google Scholar] [CrossRef]
- Leskinen, T.; Eloranta, A.M.; Tompuri, T.; Saari, A.; Ollila, H.; Mäkelä, J.; Niinikoski, H.; Lagström, H. Changes in Body Composition by Age and Obesity Status in Preschool-Aged Children: The STEPS Study. Eur. J. Clin. Nutr. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sim, P.Y.; Su, T.T.; Majid, H.A.; Nahar, A.M.; Jalaludin, M.Y. A Comparison Study of Portable Foot-to-Foot Bioelectrical Impedance Scale to Measure Body Fat Percentage in Asian Adults and Children. Biomed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Eisenmann, J.C.; Heelan, K.A.; Welk, G.J. Assessing Body Composition among 3- to 8-Year-Old Children: Anthropometry, BIA, and DXA. Obes. Res. 2004, 12, 1633–1640. [Google Scholar] [CrossRef] [PubMed]
- Verney, J.; Metz, L.; Chaplais, E.; Cardenoux, C.; Pereira, B.; Thivel, D. Bioelectrical Impedance Is an Accurate Method to Assess Body Composition in Obese but Not Severely Obese Adolescents. Nutr. Res. 2016, 36, 663–670. [Google Scholar] [CrossRef]
- Lyons-Reid, J.; Ward, L.C.; Kenealy, T.; Cutfield, W. Bioelectrical Impedance Analysis—an Easy Tool for Quantifying Body Composition in Infancy? Nutrients 2020, 12, 920. [Google Scholar] [CrossRef] [Green Version]
- Lim, J.S.; Hwang, J.S.; Lee, J.A.; Kim, D.H.; Park, K.D.; Jeong, J.S.; Cheon, G.J. Cross-Calibration of Multi-Frequency Bioelectrical Impedance Analysis with Eight-Point Tactile Electrodes and Dual-Energy X-Ray Absorptiometry for Assessment of Body Composition in Healthy Children Aged 6-18 Years. Pediatr. Int. 2009, 51, 263–268. [Google Scholar] [CrossRef]


| Characteristics | All Patients (n = 123) | Study 1 (n = 67) | Study 2 (n = 44) | Study 3 (n = 12) |
| Male (absolute; %) | 78 (63) | 43 (64) | 28 (64) | 7 (58) |
| Age (years) | 13.6 ± 2.6 | 13.4 ± 2.6 | 13.3 ± 2.4 | 15.9 ± 1.4 |
| Height (cm) | 165.2 ± 12.1 | 165.0 ± 12.7 | 164.2 ± 11.4 | 169.8 ± 10.4 |
| Weight (kg) | 97.5 ± 27.6 | 98.0 ± 28.7 | 94.0 ± 27.1 | 107.4 ± 21.8 |
| BMI (kg/m2) | 35.2 ± 7.0 | 35.4 ± 7.5 | 34.3 ± 6.8 | 37.0 ± 4.7 |
| All Patients (n = 123) | Study 1 (n = 67) | Study 2 (n = 44) | Study 3 (n = 12) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TANITA | BIACORPUS | p-Value | TANITA | BIACORPUS | p-Value | TANITA | BIACORPUS | p-Value | TANITA | BIACORPUS | p-Value | |
| BFP (%) | 41.4 ± 7.8 | 39.1 ± 6.7 | 0.000 | 41.6 ± 8.1 | 39.4 ± 6.8 | 0.000 | 40.7 ± 7.7 | 37.9 ± 6.0 | 0.000 | 43.0 ± 7.0 | 42.1 ± 8.2 | 0.481 |
| FM (kg) | 41.6 ± 17.8 | 38.6 ± 14.3 | 0.000 | 41.8 ± 18.5 | 39.0 ± 14.6 | 0.000 | 39.3 ± 17.4 | 36.3 ± 13.8 | 0.001 | 48.6 ± 14.5 | 45.2 ± 12.7 | 0.252 |
| FFM (kg) | 56.2 ± 14.2 | 58.9 ± 16.2 | 0.000 | 56.2 ± 14.3 | 59.1 ± 16.9 | 0.000 | 54.7 ± 13.6 | 57.7 ± 15.4 | 0.001 | 61.3 ± 15.9 | 62.1 ± 15.6 | 0.520 |
| All Patients (n = 123) | All Patients (n = 123) | |||||
|---|---|---|---|---|---|---|
| Parameter | Male (n = 78) | Female (n = 45) | p-value | Male (n = 78) | Female (n = 45) | p-value |
| TANITA | BIACORPUS | |||||
| BFP (%) | 39.9 ± 8.1 | 43.9 ± 6.9 | 0.007 | 36.5 ± 5.3 | 43.6 ± 6.6 | 0.000 |
| FM (kg) | 42.6 ± 18.8 | 39.8 ± 16.1 | 0.408 | 38.2 ± 13.7 | 39.4 ± 15.3 | 0.638 |
| FFM (kg) | 60.8 ± 14.3 | 48.1 ± 9.7 | 0.000 | 64.9 ± 16.0 | 48.5 ± 10.1 | 0.000 |
| Study 1 (n = 67) | Study 1 (n = 67) | |||||
| Parameter | Male (n = 43) | Female (n = 24) | p-value | Male (n = 43) | Female (n = 24) | p-value |
| TANITA | BIACORPUS | |||||
| BFP (%) | 39.9 ± 8.4 | 44.5 ± 6.8 | 0.024 | 36.8 ± 5.6 | 44.0 ± 6.2 | 0.000 |
| FM (kg) | 42.5 ± 19.4 | 40.5 ± 17.1 | 0.682 | 38.5 ± 14.1 | 39.9 ± 15.8 | 0.700 |
| FFM (kg) | 60.9 ± 13.9 | 48.8 ± 10.8 | 0.000 | 65.0 ± 16.7 | 48.5 ± 10.3 | 0.000 |
| Study 2 (n = 44) | Study 2 (n = 44) | |||||
| Parameter | Male (n = 28) | Female (n = 16) | p-value | Male (n = 28) | Female (n = 16) | p-value |
| TANITA | BIACORPUS | |||||
| BFP (%) | 39.9 ± 8.2 | 42.1 ± 6.6 | 0.362 | 36.8 ± 4.9 | 41.4 ± 6.3 | 0.002 |
| FM (kg) | 40.8 ± 18.8 | 36.6 ± 14.7 | 0.443 | 36.4 ± 13.8 | 36.0 ± 14.3 | 0.912 |
| FFM (kg) | 58.8 ± 14.0 | 47.5 ± 9.3 | 0.006 | 63.3 ± 15.5 | 48.1 ± 9.5 | 0.001 |
| Study 3 (n = 12) | Study 3 (n = 12) | |||||
| Parameter | Male (n = 7) | Female (n = 5) | p-value | Male (n = 7) | Female (n = 5) | p-value |
| TANITA | BIACORPUS | |||||
| BFP (%) | 40.6 ± 5.4 | 46.5 ± 8.0 | 0.158 | 37.7 ± 5.1 | 48.3 ± 8.0 | 0.017 |
| FM (kg) | 50.0 ± 15.0 | 46.5 ± 15.2 | 0.698 | 43.2 ± 11.7 | 48.1 ± 14.8 | 0.528 |
| FFM (kg) | 68.2 ± 17.6 | 51.6 ± 5.5 | 0.072 | 70.8 ± 14.0 | 50.0 ± 7.8 | 0.014 |
| Parameter | TANITA | BIACORPUS | BOD POD | DXA |
|---|---|---|---|---|
| BFP (%) | 46.3 ± 7.3 | 46.0 ± 8.0 | 48.5 ± 4.8 | 46.8 ± 3.4 |
| FM (kg) | 53.2 ± 16.3 | 48.6 ± 12.1 | 50.6 ± 8.0 | 51.5 ± 7.7 |
| FFM (kg) | 56.1 ± 11.2 | 56.6 ± 12.5 | 54.5 ± 12.2 | 56.6 ± 10.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thajer, A.; Skacel, G.; Truschner, K.; Jorda, A.; Vasek, M.; Horsak, B.; Strempfl, J.; Kautzky-Willer, A.; Kainberger, F.; Greber-Platzer, S. Comparison of Bioelectrical Impedance-Based Methods on Body Composition in Young Patients with Obesity. Children 2021, 8, 295. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040295
Thajer A, Skacel G, Truschner K, Jorda A, Vasek M, Horsak B, Strempfl J, Kautzky-Willer A, Kainberger F, Greber-Platzer S. Comparison of Bioelectrical Impedance-Based Methods on Body Composition in Young Patients with Obesity. Children. 2021; 8(4):295. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040295
Chicago/Turabian StyleThajer, Alexandra, Gabriele Skacel, Katharina Truschner, Anselm Jorda, Martin Vasek, Brian Horsak, Johanna Strempfl, Alexandra Kautzky-Willer, Franz Kainberger, and Susanne Greber-Platzer. 2021. "Comparison of Bioelectrical Impedance-Based Methods on Body Composition in Young Patients with Obesity" Children 8, no. 4: 295. https://0-doi-org.brum.beds.ac.uk/10.3390/children8040295