Three Cases of Lymphocytic Infiltration of the Eyelid
Abstract
:1. Introduction
2. Case Report
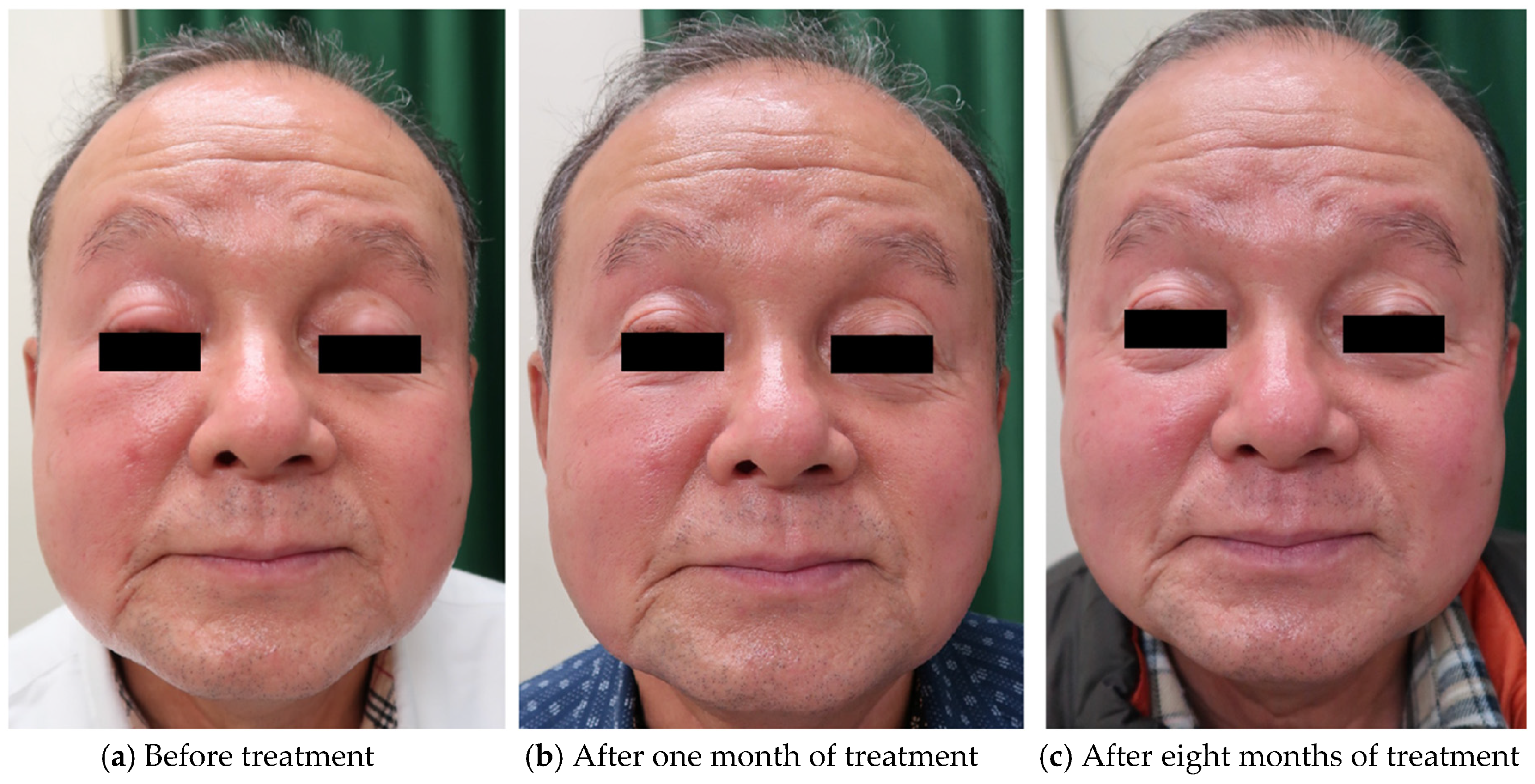
2.1. Case 1
2.2. Case 2
2.3. Case 3
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jessner, M.; Kanof, B. Lymphocytiv infiltration of the skin. Arch. Dermatol. 1953, 68, 447–449. [Google Scholar]
- Toonstra, J.; Wildschut, A.; Boer, J.; Smeenk, G.; Willemze, R.; van der Putte, S.C.; Boonstra, H.; van Vloten, W.A. Jessner’s lymphocytic infiltration of the skin. A clinical study of 100 patients. Arch. Dermatol. 1989, 125, 1525–1530. [Google Scholar] [CrossRef] [PubMed]
- Cabral, F.; Lubbe, L.C.; Nóbrega, M.M.; Obadia, D.L.; Souto, R.; Gripp, A.C. Morbihan disease: A therapeutic challenge. An. Bras. Dermatol. 2017, 92, 847–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, L.A.; Cohen, D.E. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch. Dermatol. 2012, 148, 1395–1398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagasaka, T.; Koyama, T.; Matsumura, K.; Chen, K.R. Persistent lymphoedema in Morbihan disease: Formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin. Exp. Dermatol. 2008, 33, 764–767. [Google Scholar] [CrossRef] [PubMed]
- De Vasconcelos, R.C.F.; Eid, N.T.; Eid, R.T.; Moriya, F.S.; Braga, B.B.; Michalany, A.O. Morbihan syndrome: A case report and literature review. An. Bras. Dermatol. 2016, 91, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Ranu, H.; Lee, J.; Hee, T.H. THERAPEUTIC HOTLINE: Successful treatment of Morbihan’s disease with oral prednisolone and doxycycline. Dermatol. Ther. 2010, 23, 682–685. [Google Scholar] [CrossRef] [PubMed]
- Willemze, R.; Dijkstra, A.; Meijer, C.J.L.M. Lymphocytic infiltration of the skin (Jessner): A T-cell lymphoproliferative disease. Br. J. Dermatol. 1984, 110, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Tomasini, D.; Mentzel, T.; Hantschke, M.; Cerri, A.; Paredes, B.; Rütten, A.; Schärer, L.; Kutzner, H. Plasmacytoid dendritic cells: An overview of their presence and distribution in different inflammatory skin diseases, with special emphasis on Jessner’s lymphocytic infiltrate of the skin and cutaneous lupus erythematosus. J. Cutan. Pathol. 2010, 37, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.T.; Harrington, D.W. Jessner Lymphocytic Infiltration of The Skin; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Higgins, C.; Pwakeel, R.; Cerio, R. Childhood Jessner’s lymphocytic infiltrate of the skin. Br. J. Dermatol. 1994, 131, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Lipsker, D.; Mitschler, A.; Grosshans, E.; Cribier, B. Could Jessner’s Lymphocytic Infiltrate of the Skin Be a Dermal Variant of Lupus Erythematosus? An Analysis of 210 Cases. Dermatology 2006, 213, 15–22. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sugioka, K.; Hayashi, A.; Ichishi, M.; Sugimoto, Y.; Habe, K.; Yamanaka, K. Three Cases of Lymphocytic Infiltration of the Eyelid. Dermatopathology 2021, 8, 124-129. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology8020018
Sugioka K, Hayashi A, Ichishi M, Sugimoto Y, Habe K, Yamanaka K. Three Cases of Lymphocytic Infiltration of the Eyelid. Dermatopathology. 2021; 8(2):124-129. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology8020018
Chicago/Turabian StyleSugioka, Kyoko, Akinobu Hayashi, Masako Ichishi, Yasuko Sugimoto, Koji Habe, and Keiichi Yamanaka. 2021. "Three Cases of Lymphocytic Infiltration of the Eyelid" Dermatopathology 8, no. 2: 124-129. https://0-doi-org.brum.beds.ac.uk/10.3390/dermatopathology8020018





