99mTc Labelling Strategies for the Development of Potential Nitroimidazolic Hypoxia Imaging Agents
Abstract
:1. Design of 99mTc-Radiopharmaceuticals
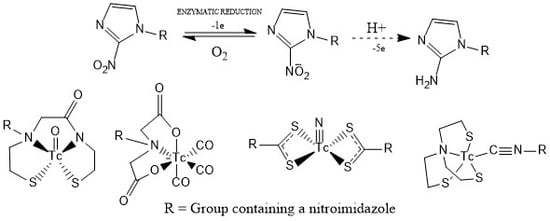
2. Hypoxia Imaging Agents
3. Nitroimidazoles as Bioreductive Pharmacophores
4. Labelling Strategies of Nitroimidazoles with [99mTc]Tc
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fani, M.; Maecke, H.R. Radiopharmaceutical development of radiolabelled peptides. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 11–30. [Google Scholar] [CrossRef]
- Decristoforo, C.; Mather, S.J. Technetium-99m somatostatin analogues: Effect of labelling methods and peptide sequence. Eur. J. Nucl. Med. 1999, 26, 869–876. [Google Scholar] [CrossRef]
- Bangard, M.; Béhé, M.; Guhlke, S.; Otte, R.; Bender, H.; Maecke, H.R.; Biersack, H.J. Detection of somatostatin receptor-positive tumours using the new 99mTc-tricine-HYNIC-d-Phe1-Tyr3-octreotide: First results in patients an comparison with 111In-DTPA-d-Phe1-octreotide. Eur. J. Nucl. Med. 2000, 2, 628–637. [Google Scholar] [CrossRef]
- Alberto, R. Future Trends in the Development of Technetium Radiopharmaceuticals. In Tc-99m Radiopharmaceuticals: Status and Trends; Radioisotopes and Radiopharmaceutical Series No. 1; International Atomic Energy Agency: Vienna, Austria, 2009; pp. 347–358. [Google Scholar]
- Banerjee, S.R.; Pullambhatla, M.; Foss, C.A.; Falk, A.; Byun, Y.; Nimmagadda, S.; Mease, R.C.; Pomper, M.G. Effect of Chelators on the Pharmacokinetics of 99mTc-Labeled Imaging Agents for the Prostate-Specific Membrane Antigen (PSMA). J. Med. Chem. 2013, 56, 6108–6121. [Google Scholar] [CrossRef]
- Höckel, M.; Vaupel, P. Tumour Hypoxia: Definitions and Current Clinical, Biologic, and Molecular Aspects. J. Natl. Cancer Inst. 2001, 93, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Grimes, D.R.; Warren, D.R.; Warren, S. Hypoxia imaging and radiotherapy: Bridging the resolution gap. Br. J. Radiol. 2017, 90, 20160939. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.D. Hypoxia sensitizers: Implications for radiation therapy. N. Engl. J. Med. 1979, 301, 1429–1432. [Google Scholar] [CrossRef] [PubMed]
- Rasey, J.S.; Grunbaum, Z.; Magee, S.; Nelson, N.J.; Olive, P.L.; Durand, R.E.; Krohn, K.A. Characterization of Radiolabeled Fluoromisonidazole as a Probe for Hypoxic Cells. Radiat. Res. 1987, 111, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Li, X.; Zou, H.; Sun, X.; Shen, B. 18F-Fluoromisonidazole in tumour hypoxia imaging. Oncotarget 2017, 8, 94969–94979. [Google Scholar]
- Wilson, W.R.; Hay, M.P. Targeting hypoxia in cancer therapy. Nat. Rev. Cancer. 2011, 11, 393–410. [Google Scholar] [CrossRef]
- Ricardo, C.L.; Kumar, P.; Wiebe, L.I. Bifunctional Metal—Nitroimidazole Complexes for Hypoxia Theranosis in Cancer. J. Diagn. Imaging Ther. 2015, 2, 103–158. [Google Scholar] [CrossRef]
- Tocher, J.H.; Edwards, D.I. Evidence for the direct interaction of reduced metronidazole derivatives with DNA bases. Biochem. Pharmacol. 1994, 48, 1089–1094. [Google Scholar] [CrossRef]
- Edwards, D.I. Nitroimidazole drugs-action and resistance mechanisms. 1. Mechanism of action. J. Antimicrob. Chemother. 1993, 31, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Wardman, P. Reduction potentials of one-electron couples involving free radicals in aqueous solutions. J. Phys. Chem. Ref. Data 1989, 18, 1664–1672. [Google Scholar] [CrossRef]
- Nunn, A.D. Radiopharmaceuticals for imaging myocardial perfusion. Semin. Nucl. Med. 1990, 20, 111–118. [Google Scholar] [CrossRef]
- Duatti, A. Role of 99mTc in Diagnostic Imaging. In Tc-99m Radiopharmaceuticals: Status and Trends; Radioisotopes and Radiopharmaceutical Series No. 1; International Atomic Energy Agency: Vienna, Austria, 2009; pp. 7–18. [Google Scholar]
- Nosco, D.L.; Beaty-Nosco, J.A. Chemistry of technetium radiopharmaceuticals 1: Chemistry behind de development oftechnetium-99m compounds to determine kidney function. Coord. Chem. Rev. 1999, 184, 91–123. [Google Scholar] [CrossRef]
- Qi, Y.; Li, G.; Chi, X.; Du, L.; Huang, K.; Zhang, H.; Huang, B. Preparation of 99mTc-EDTA-MN and Its Bioimaging in Mouse. Chin. J. Lung Cancer 2015, 18, 422–426. [Google Scholar]
- Ruan, Q.; Zhang, X.; Lin, X.; Duan, X.; Zhang, J. Novel 99mTc labelled complexes with 2-nitroimidazole isocyanide: Design, synthesis and evaluation as potential tumour hypoxia imaging agents. Medchemcomm 2018, 9, 988–994. [Google Scholar] [CrossRef]
- Mazzi, U. Technetium in Medicine. In Technetium-99m Pharmaceuticals: Preparation and Quality Control in Nuclear Medicine; Zolle, I., Ed.; Springer: Berlin/Heidelberg, Germany, 2007; pp. 7–58. [Google Scholar]
- Linder, K.E.; Chan, Y.W.; Cyr, J.E.; Nowotnik, D.P.; Eckelman, W.C.; Nunn, A.D. Synthesis, characterization, and in vitro evaluation of Nitroimidazole-BATO complexes: New technetium compounds designed for imaging hypoxic tissue. Bioconjug. Chem. 1993, 4, 326–333. [Google Scholar] [CrossRef]
- Ramalingam, K.; Raju, N.; Nanjappan, P.; Linder, K.E.; Pirro, J.; Zeng, W.; Rumsey, W.; Nowotnik, D.P.; Nunn, A.D. The synthesis and in vitro evaluation of a 99m-Technetium-nitroimidazole complex based on a bis(amine-phenol) ligand: Comparison to BMS-181321. J. Med. Chem. 1994, 37, 4155–4163. [Google Scholar] [CrossRef]
- Hsia, C.C.; Huang, F.L.; Hung, G.U.; Shen, L.H.; Chen, C.L.; Wang, H.E. The biological characterization of 99mTc-BnAO-NI as a SPECT probe for imaging hypoxia in a sarcoma-bearing mouse model. Appl. Radiat. Isot. 2011, 69, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Jia, H.M.; Fang, D.C.; Feng, Y.; Zhang, J.Y.; Fan, W.B.; Zhu, L. The interconversion mechanism between TcO3+ and TcO2+ core of 99mTc labeled amine-oxime(AO)complexes. Theor. Chem. Acc. 2008, 121, 271–278. [Google Scholar] [CrossRef]
- Brauers, G.; Archer, C.M.; Burke, J.F. The chemical characterization of the tumour imaging agent 99mTc-HL91. Eur. J. Nucl. Med. 1997, 24, 943. [Google Scholar]
- Huang, H.; Zhou, H.; Li, Z.; Wang, X.; Chu, T. Effect of a second nitroimidazole redox centre on the accumulationof a hypoxia marker: Synthesis and in vitro evaluation of 99mTc-labeled bisnitroimidazole propylene amine oxime complexes. Bioorg. Med. Chem. Lett. 2012, 22, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Huang, H.; Chu, T.J. In vitro and in vivo evaluation of technetium-99m-labeled propylene amine oxime complexes containing nitroimidazole and nitrotriazole groups as hypoxia markers. Label. Compd. Radiopharm. 2016, 59, 14–23. [Google Scholar] [CrossRef]
- Mei, L.; Wang, Y.; Chu, T. 99mTc/Re complexes bearing bisnitroimidazole or mononitroimidazole a potential bioreductive markers for tumour: Synthesis, physicochemical characterization and biological evaluation. Eur. J. Med. Chem. 2012, 58, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Chu, T. In vivo click reaction between Tc-99m-labeled azadibenzocyclooctyne-MAMA and 2-nitroimidazole-azidefor tumour hypoxia targeting. Bioorg. Med. Chem. Lett. 2015, 25, 4453–4456. [Google Scholar] [CrossRef]
- Li, N.; Zhu, H.; Chu, T.; Yang, Z. Preparation and biological evaluation of 99mTc-N4IPA for single photon emission computerized tomography imaging of hypoxia in mouse tumour. Eur. J. Med. Chem. 2013, 69, 223–231. [Google Scholar] [CrossRef]
- Nakayama, M.; Xu, L.C.; Koga, Y.; Harada, K.; Sugii, A.; Nakayama, H.; Tomiguchi, S.; Kojima, A.; Ohyama, Y.; Takahashi, O.I. Hydroxamamide as a Chelating Moiety for the Preparation of 99mTc-radiopharmaceuticals III. Characterization of various 99mTc-hydroxamamides. Appl. Radiat. Isot. 1997, 48, 571–577. [Google Scholar] [CrossRef]
- Joyard, Y.; Le Joncour, V.; Castel, H.; Diouf, C.B.; Bischoff, L.; Papamicaël, C.; Levacher, V.; Vera, P.; Bohn, P. Synthesis and biological evaluation of a novel 99mTc labelled 2-nitroimidazole derivative as a potential agent for imaging tumour hypoxia. Bioorg. Med. Chem. Lett. 2013, 23, 3704–3708. [Google Scholar] [CrossRef]
- Li, Z.; Lin, X.; Zhang, J.; Wang, X.; Jin, Z.; Zhang, W.; Zhang, Y. Kit formulation for preparation and biological evaluation of a novel 99mTc-oxo complex with metronidazole xanthate for imaging tumour hypoxia. Nucl. Med. Biol. 2016, 43, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, Q.; Guan, Y.; Liu, S.; Chen, Q.; Li, X. Synthesis and Biological Evaluation of a New Nitroimidazole-99mTc-Complex for Imaging of Hypoxia in Mice Model CD 1. Med. Sci. Monit. 2016, 22, 3778–3791. [Google Scholar] [CrossRef] [PubMed]
- Alberto, R.; Schibli, R.; Egli, A.; Schubiger, A.P.; Ulrich, A.; Kaden, T.A. A novel organometallic aqua complex of technetium for the labelling of biomolecules. Synthesis of [99mTc(OH2)3(CO)3]+ from [99mTcO4]− in aqueous solution and its reaction with a bifunctional ligand. J. Am. Chem. Soc. 1998, 120, 7987–7988. [Google Scholar] [CrossRef]
- Mallia, M.B.; Subramanian, S.; Mathur, A.; Sarma, H.D.; Venkatesh, M.; Banerjee, S. Synthesis and evaluation of 2-, 4-, 5-substituted nitroimidazole-iminodiacetic acid-99mTc(CO)3 complexes to target hypoxic tumours. J. Label. Compd. Radiopharm. 2010, 53, 535–542. [Google Scholar] [CrossRef]
- Mallia, M.B.; Kumar, C.; Mathur, A.; Sarma, H.D.; Banerjee, S. On the structural modification of 2-nitroimidazole-99mTc(CO)3 complex, a hypoxiamarker, for improving in vivo pharmacokinetics. Nucl. Med. Biol. 2012, 39, 1236–1242. [Google Scholar] [CrossRef]
- Mallia, M.B.; Subramanian, S.; Mathur, A.; Sarma, H.D.; Venkatesh, M.; Banerjee, S. A study on nitroimidazole-99mTc(CO)3 complexes as hypoxia marker: Some observations towards possible improvement in in vivo efficacy. Nucl. Med. Biol. 2014, 41, 600–610. [Google Scholar] [CrossRef]
- Mallia, M.B.; Mittal, S.; Sarma, H.; Banerjee, S. Modulation of in vivo distribution through chelator: Synthesis and evaluation of a 2-nitroimidazole—Dipicolylamine—99mTc(CO)3 complex for detecting tumour hypoxia. Bioorg. Med. Chem. Lett. 2016, 26, 46–50. [Google Scholar] [CrossRef]
- Giglio, J.; Dematteis, S.; Fernández, S.; Cerecetto, H.; Rey, A. Synthesis and evaluation of a new 99mTc(I)-tricarbonyl complex bearing the 5-nitroimidazol-1-yl moiety as potentialhypoxia imaging agent. J. Label. Compd. Radiopharm. 2014, 57, 403–409. [Google Scholar] [CrossRef]
- Fernández, S.; Giglio, J.; Rey, A.M.; Cerecetto, H. Influence of ligand denticity on the properties of novel 99mTc(I)-carbonyl complexes. Application to the development of radiopharmaceuticals for imaging hypoxic tissue. Bioorg. Med. Chem. 2012, 20, 4040–4048. [Google Scholar] [CrossRef]
- Baldas, J.; Bonnyman, J. Substitution reactions of 99mTcNCl4−—A route to a new class of 99mTc-radiopharmaceuticals. Int. J. Appl. Radiat. Isot. 1985, 36, 133–139. [Google Scholar] [CrossRef]
- Giglio, J.; Fernández, S.; Rey, A.; Cerecetto, H. Synthesis and biological characterisation of novel dithiocarbamate containing 5-nitroimidazole 99mTc-complexes as potential agents for targeting hypoxia. Bioorg. Med. Chem. Lett. 2011, 21, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Ruan, Q.; Zhang, X.; Duan, X.; Teng, Y.; Zhang, J. 99mTc labelled complexes with secnidazole xanthate: Synthesis and evaluation as potential radiotracers to target tumour hypoxia. Appl. Radiat. Isot. 2018, 140, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Mathur, A.; Mallia, M.B.; Banerjee, S.; Sarma, H.D.; Pillai, M.R.A. Preparation and evaluation of a 99mTcN–PNP complex of sanazole analogue for detecting tumour hypoxia. Bioorg. Med. Chem. Lett. 2013, 23, 1394–1397. [Google Scholar] [CrossRef] [PubMed]
- Pietzsch, H.J.; Gupta, A.; Syhre, R.; Leibnitz, P.; Spies, H. Mixed-ligandtechnetium(III) complexes with tetradentate/monodentate NS3/isocyanide coordination: A new nonpolar technetium chelate system for thedesign of neutral and lipophilic complexes stable in vivo. Bioconjug. Chem. 2001, 12, 538–544. [Google Scholar] [CrossRef]
- Giglio, J.; Fernández, S.; Pietzsch, H.J.; Dematteis, S.; Moreno, M.; Pacheco, J.P.; Cerecetto, H.; Rey, A. Synthesis, in vitro and in vivo characterization of novel 99mTc-‘4+1′-labeled 5-nitroimidazole derivatives as potential agents for imaging hypoxia. Nucl. Med. Biol. 2012, 39, 679–686. [Google Scholar] [CrossRef]
- Vats, K.; Mallia, M.B.; Mathur, A.; Sarma, H.D.; Banerjee, S. ‘4+1′ Mixed Ligand Strategy for the Preparation of 99mTc-Radiopharmaceuticals for Hypoxia Detecting Applications. Chem. Sel. 2017, 2, 2910–2916. [Google Scholar]
- Adams, G.E.; Flockhart, I.R.; Smithen, C.E.; Stratford, I.J.; Wardman, P.; Watts, M.E. Electron-affinic sensitization. VII. A correlation between structures, one-electron reduction potentials, and efficiencies of nitroimidazoles as hypoxic cell radiosensitizers. Radiat. Res. 1976, 67, 9–20. [Google Scholar] [CrossRef]








| Compound | SERP (in mV) |
|---|---|
| 2-nitroimidazoles | −235 to −447 |
| 4-nitroimidazoles | −375 to −554 |
| 5-nitroimidazoles | −354 to −447 |
| Structure | Log Po/w | Hypoxia/Oxia Ratio “In Vitro” | Tumour/Blood | Tumour/Muscle | Animal Model |
|---|---|---|---|---|---|
| Compound 2 | 1.59 | 4.3 (S180 cells) | 0.62 ± 0.43 (4 h) | 4.15 ± 1.17 (4 h) | mice-bearing H22 tumours |
| Compound 3 | 1.10 | 8.7 (S180 cells) | 1.08 ± 0.59 (2 h) 0.81 ± 0.34 (4 h) | 2.25 ± 0.59 (2 h) 3.24 ± 0.65 (4 h) | mice-bearing H22 tumours |
| Compound 4 | 0.69 ± 0.01 | - | 0.51 ± 0.11 (2 h) | 1.63 ± 0.24 (2 h) | Kunming mice bearing murine sarcoma tumour |
| Compound 5 | 0.28 ± 0.03 | - | 0.64 ± 0.16 (2 h) | 2.73 ± 0.47 (2 h) | Kunming mice bearing murine sarcoma tumour |
| Structure | Log Po/w | Tumour Uptake | Muscle Uptake | Blood Uptake | Tumour/Blood Ratio | Tumour/Muscle Ratio |
|---|---|---|---|---|---|---|
| Compound 11 | 0.48 | 0.71 ± 0.08 | 0.50 ± 0.03 | 1.82 ± 0.08 | 0.39 ± 0.01 | 1.40 ± 0.09 |
| Compound 13 | 0.28 | 0.31 ± 0.04 | 0.13 ± 0.01 | 1.28 ± 0.15 | 0.24 ± 0.05 | 2.38 ± 0.15 |
| Compound 14 | 0.06 | 0.38 ± 0.03 | 0.10 ± 0.01 | 1.04 ± 0.11 | 0.37 ± 0.08 | 3.80 ± 0.23 |
| Compound 15 | 0.38 | 1.01 ± 0.11 | 0.49 ± 0.06 | 1.11 ± 0.13 | 0.91 ± 0.04 | 2.14 ± 0.35 |
| FMISO | - | 3.25 ± 0.08 | 1.32 ± 0.10 | 2.18 ± 0.15 | 1.37 ± 0.20 | 2.52 ± 0.30 |
| Structure | Log Po/w | UPP (%) | Tumour Uptake | Muscle Uptake | Blood Uptake | Tumour/Blood Ratio | Tumour/Muscle Ratio | Model |
|---|---|---|---|---|---|---|---|---|
| Compound 16 | −0.75 | 15 | 0.50 ± 0.10 | 0.30 ± 0.10 | 2.20 ± 0.10 | 0.20 ± 0.10 | 1.70 ± 0.20 | 3LL Lewis murine lung carcinoma |
| Compound 17 | −0.44 | 13 | 0.22 ± 0.07 | 0.09 ± 0.03 | 0.29 ± 0.04 | 0.76 ± 0.10 | 2.40 ± 0.11 | 3LL Lewis murine lung carcinoma |
| Compound 18 | 0.39 | - | 0.47 ± 0.02 | - | 0.44 ± 0.02 | 1.10 ± 0.07 | - | Swiss mice bearing fibrosarcoma tumour |
| Compound 19 | 0.15 | - | 0.33 ± 0.05 | 0.07 ± 0.01 | 0.38 ± 0.03 | 0.90 ± 0.06 | 4.70 ± 0.10 | Swiss mice bearing fibrosarcoma tumour |
| Compound 20 | −0.53 | - | 0.34 ± 0.04 | 0.24 ± 0.04 | 0.40 ± 0.08 | 0.90 ± 0.07 | 1.40 ± 0.08 | Swiss mice bearing fibrosarcoma tumour |
| Compound 21 | 0.63 | 31 | 1.00 ± 0.09 | - | - | 0.30 ± 0.17 | 1.29 ± 0.10 | 3LL Lewis murine lung carcinoma |
| Compound 24 | 0.70 | 12 | 2.20 ± 0.05 | 0.90 ± 0.60 | 3.80 ± 1.00 | 0.60 ± 0.20 | 2.40 ± 0.90 | 3LL Lewis murine lung carcinoma |
| FMISO | −0.40 | - | 3.25 ± 0.08 | 1.32 ± 0.10 | 2.18 ± 0.15 | 1.37 ± 0.20 | 2.52 ± 0.70 | 3LL Lewis murine lung carcinoma |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giglio, J.; Rey, A. 99mTc Labelling Strategies for the Development of Potential Nitroimidazolic Hypoxia Imaging Agents. Inorganics 2019, 7, 128. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics7110128
Giglio J, Rey A. 99mTc Labelling Strategies for the Development of Potential Nitroimidazolic Hypoxia Imaging Agents. Inorganics. 2019; 7(11):128. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics7110128
Chicago/Turabian StyleGiglio, Javier, and Ana Rey. 2019. "99mTc Labelling Strategies for the Development of Potential Nitroimidazolic Hypoxia Imaging Agents" Inorganics 7, no. 11: 128. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics7110128