Breast Cancer Stem Cell Active Copper(II) Complexes with Naphthol Schiff Base and Polypyridyl Ligands
Abstract
:1. Introduction
2. Results and Discussion
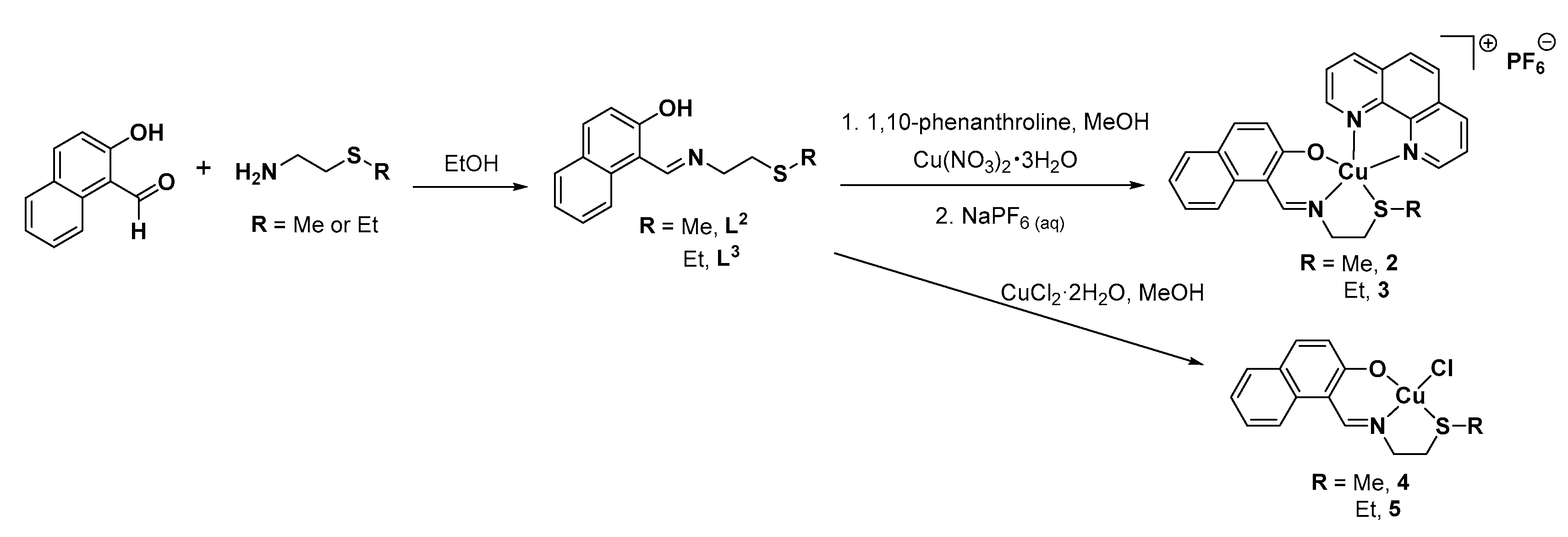
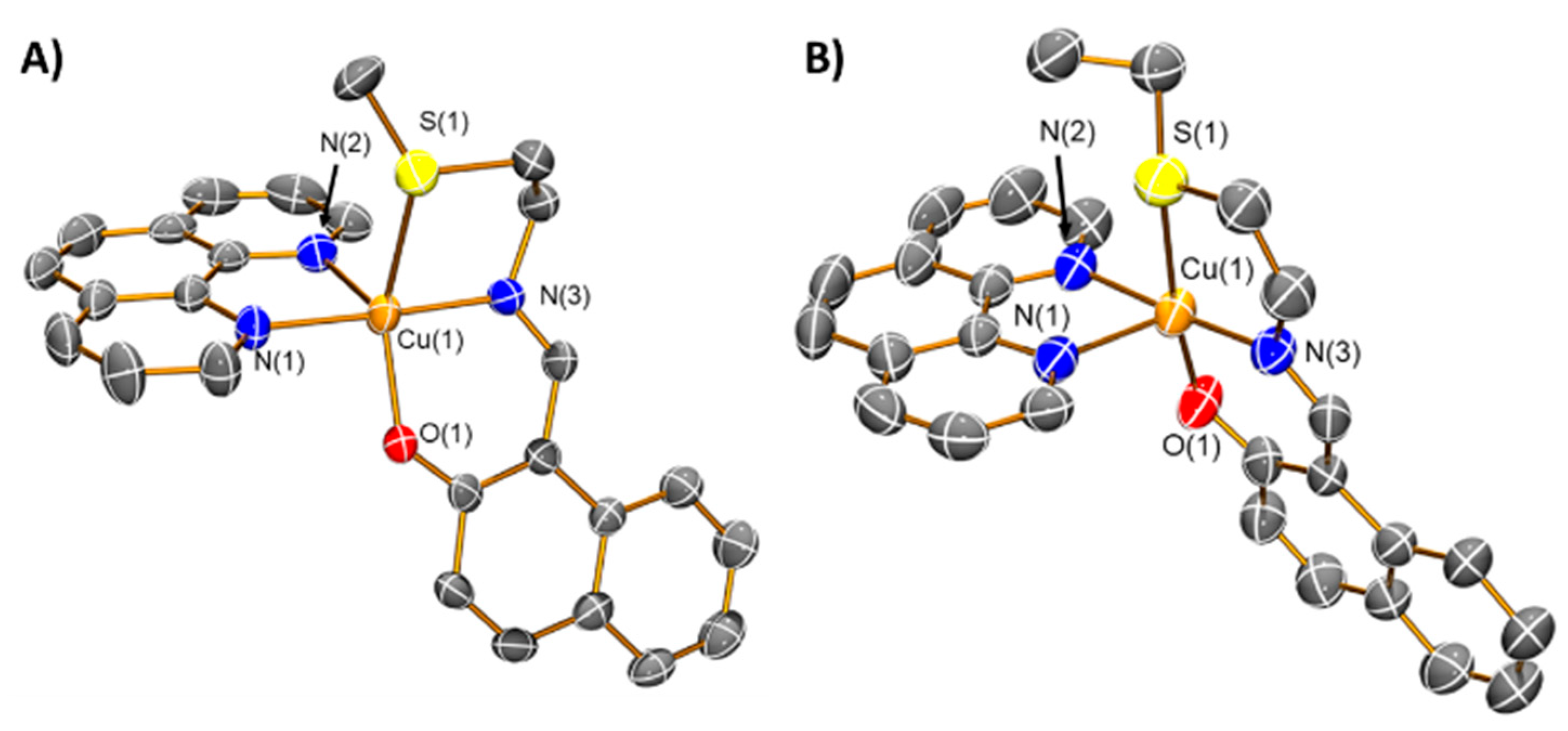
2.1. Synthesis and Characterisation of the Ligands and Copper(II) Complexes
2.2. Lipophilicity and Solution Stability of the Copper(II) Complexes
2.3. In Vitro Cytotoxicity of the Copper(II) Complexes
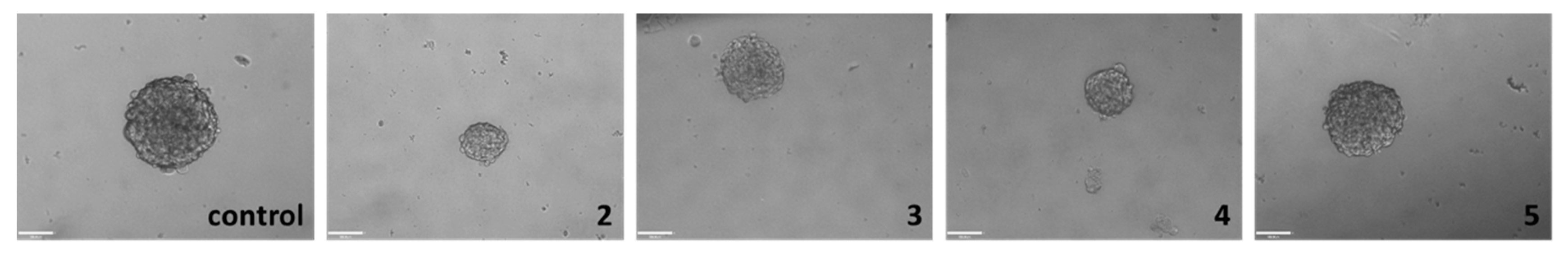
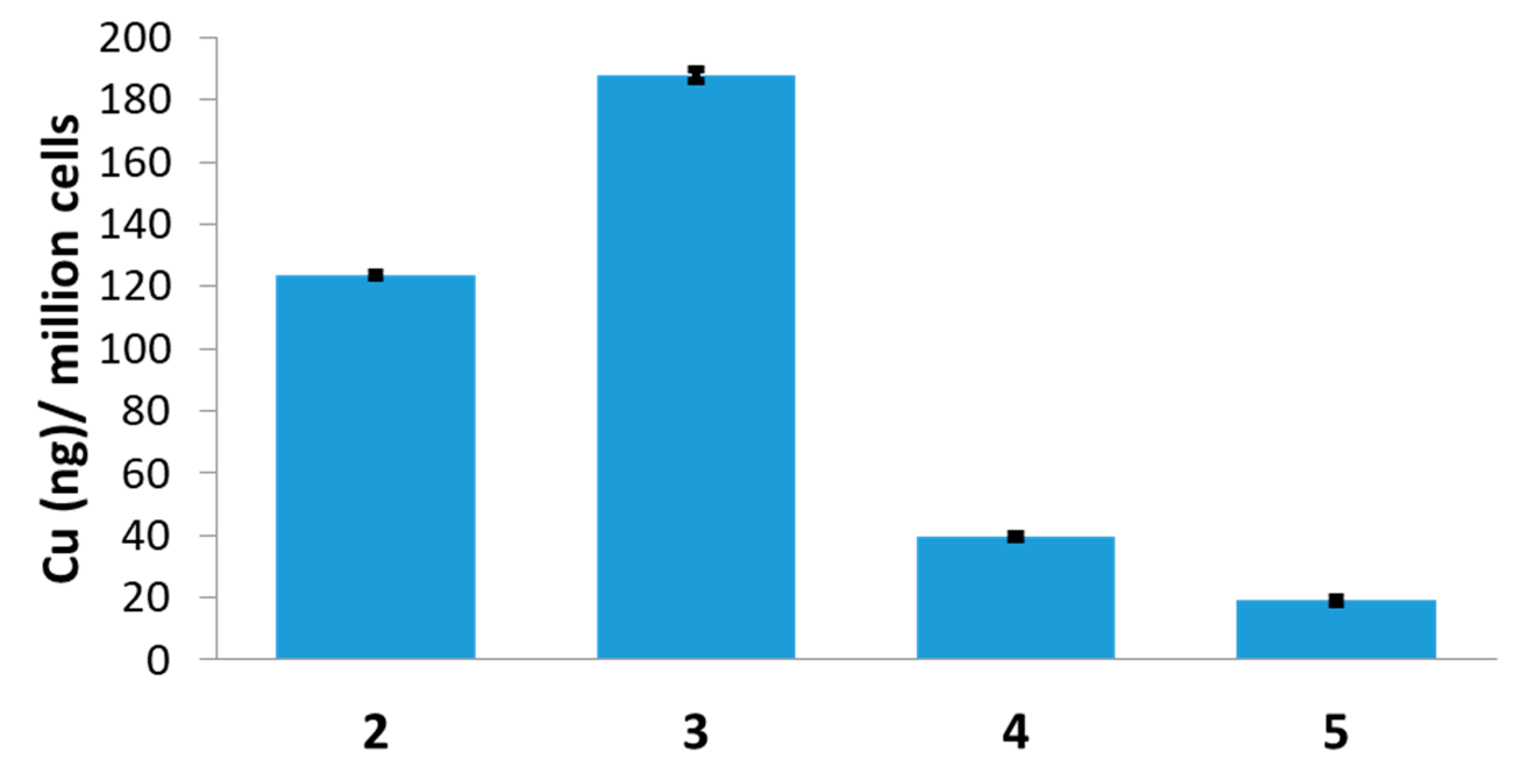
2.4. Mechanism of Action of the Copper(II) Complexes
3. Materials and Methods
3.1. General Procedures
3.2. Synthesis of (E)-1-(((2-(Methylthio)ethyl)imino)methyl)naphthalen-2-ol, L2
3.3. Synthesis of (E)-1-(((2-(Ethylthio)ethyl)imino)methyl)naphthalen-2-ol, L3
3.4. Synthesis of [Cu(L2)1,10-Phenanthroline][PF6], 2
3.5. Synthesis of [Cu(L3)1,10-Phenanthroline][PF6], 3
3.6. Synthesis of [Cu(L2)Cl], 4
3.7. Synthesis of [Cu(L3)Cl], 5
3.8. X-ray Single Crystal Diffraction Analysis
3.9. Measurement of Water-Octanol Partition Coefficient (LogP)
3.10. Cell Lines and Cell Culture Conditions
3.11. Cytotoxicity MTT Assay
3.12. Tumorsphere Formation and Viability Assay
3.13. Cellular Uptake
3.14. Intracellular ROS Assay
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Still 1 in 4 Deaths Caused by Cancer in the EU. Available online: https://ec.europa.eu/eurostat/documents/2995521/7149996/3-03022016-BP-EN.pdf/0bbc3389-8c0d-44a0-9b0c-2a0bff49f466 (accessed on 3 February 2016).
- Luengo-Fernandez, R.; Leal, J.; Gray, A.; Sullivan, R. Economic burden of cancer across the European Union: A population-based cost analysis. Lancet Oncol. 2013, 14, 1165–1174. [Google Scholar] [CrossRef]
- Al-Hajj, M.; Wicha, M.S.; Benito-Hernandez, A.; Morrison, S.J.; Clarke, M.F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl. Acad. Sci. USA 2003, 100, 3983–3988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, P.B.; Chaffer, C.L.; Weinberg, R.A. Cancer stem cells: Mirage or reality? Nat. Med. 2009, 15, 1010–1012. [Google Scholar] [CrossRef] [PubMed]
- Balic, M.; Lin, H.; Young, L.; Hawes, D.; Giuliano, A.; McNamara, G.; Datar, R.H.; Cote, R.J. Most early disseminated cancer cells detected in bone marrow of breast cancer patients have a putative breast cancer stem cell phenotype. Clin. Cancer Res. 2006, 12, 5615–5621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owens, T.W.; Naylor, M.J. Breast cancer stem cells. Front. Physiol. 2013, 4, 225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calcagno, A.M.; Salcido, C.D.; Gillet, J.P.; Wu, C.P.; Fostel, J.M.; Mumau, M.D.; Gottesman, M.M.; Varticovski, L.; Ambudkar, S.V. Prolonged drug selection of breast cancer cells and enrichment of cancer stem cell characteristics. J. Natl. Cancer Inst. 2010, 102, 1637–1652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips, T.M.; McBride, W.H.; Pajonk, F. The response of CD24−/low/CD44+ breast cancer-initiating cells to radiation. J. Natl. Cancer Inst. 2006, 98, 1777–1785. [Google Scholar] [CrossRef] [Green Version]
- Laws, K.; Suntharalingam, K. The Next Generation of Anticancer Metallopharmaceuticals: Cancer Stem Cell-Active Inorganics. ChemBioChem 2018, 19, 2246–2253. [Google Scholar] [CrossRef]
- Boodram, J.N.; McGregor, I.J.; Bruno, P.M.; Cressey, P.B.; Hemann, M.T.; Suntharalingam, K. Breast Cancer Stem Cell Potent Copper(II)-Non-Steroidal Anti-Inflammatory Drug Complexes. Angew. Chem. Int. Ed. 2016, 55, 2845–2850. [Google Scholar] [CrossRef]
- Eskandari, A.; Boodram, J.N.; Cressey, P.B.; Lu, C.; Bruno, P.M.; Hemann, M.T.; Suntharalingam, K. The breast cancer stem cell potency of copper(II) complexes bearing nonsteroidal anti-inflammatory drugs and their encapsulation using polymeric nanoparticles. Dalton Trans. 2016, 45, 17867–17873. [Google Scholar] [CrossRef] [Green Version]
- Lu, C.; Eskandari, A.; Cressey, P.B.; Suntharalingam, K. Cancer Stem Cell and Bulk Cancer Cell Active Copper(II) Complexes with Vanillin Schiff Base Derivatives and Naproxen. Chem. Eur. J. 2017, 23, 11366–11374. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Laws, K.; Eskandari, A.; Suntharalingam, K. A reactive oxygen species-generating, cyclooxygenase-2 inhibiting, cancer stem cell-potent tetranuclear copper(II) cluster. Dalton Trans. 2017, 46, 12785–12789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marzano, C.; Pellei, M.; Tisato, F.; Santini, C. Copper complexes as anticancer agents. Anticancer Agents Med. Chem. 2009, 9, 185–211. [Google Scholar] [CrossRef] [PubMed]
- Santini, C.; Pellei, M.; Gandin, V.; Porchia, M.; Tisato, F.; Marzano, C. Advances in Copper Complexes as Anticancer Agents. Chem. Rev. 2014, 114, 815–862. [Google Scholar] [CrossRef]
- Galindo-Murillo, R.; Garcia-Ramos, J.C.; Ruiz-Azuara, L.; Cheatham, T.E., 3rd; Cortes-Guzman, F. Intercalation processes of copper complexes in DNA. Nucleic Acids Res. 2015, 43, 5364–5376. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Azuara, L.; Bravo-Gomez, M.E. Copper compounds in cancer chemotherapy. Curr. Med. Chem. 2010, 17, 3606–3615. [Google Scholar] [CrossRef]
- Vertiz, G.; Garcia-Ortuno, L.E.; Bernal, J.P.; Bravo-Gomez, M.E.; Lounejeva, E.; Huerta, A.; Ruiz-Azuara, L. Pharmacokinetics and hematotoxicity of a novel copper-based anticancer agent: Casiopeina III-Ea, after a single intravenous dose in rats. Fundam. Clin. Pharmacol. 2014, 28, 78–87. [Google Scholar] [CrossRef]
- Wehbe, M.; Leung, A.W.Y.; Abrams, M.J.; Orvig, C.; Bally, M.B. A Perspective—Can copper complexes be developed as a novel class of therapeutics? Dalton Trans. 2017, 46, 10758–10773. [Google Scholar] [CrossRef]
- Silva-Platas, C.; Villegas, C.A.; Oropeza-Almazan, Y.; Carranca, M.; Torres-Quintanilla, A.; Lozano, O.; Valero-Elizondo, J.; Castillo, E.C.; Bernal-Ramirez, J.; Fernandez-Sada, E.; et al. Ex Vivo Cardiotoxicity of Antineoplastic Casiopeinas Is Mediated through Energetic Dysfunction and Triggered Mitochondrial-Dependent Apoptosis. Oxid. Med. Cell Longev. 2018, 2018, 8949450. [Google Scholar] [CrossRef] [Green Version]
- Diehn, M.; Cho, R.W.; Lobo, N.A.; Kalisky, T.; Dorie, M.J.; Kulp, A.N.; Qian, D.; Lam, J.S.; Ailles, L.E.; Wong, M.; et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 2009, 458, 780–783. [Google Scholar] [CrossRef]
- Shi, X.; Zhang, Y.; Zheng, J.; Pan, J. Reactive oxygen species in cancer stem cells. Antioxid. Redox Signal. 2012, 16, 1215–1228. [Google Scholar] [CrossRef] [Green Version]
- Kaur, P.; Johnson, A.; Northcote-Smith, J.; Lu, C.; Suntharalingam, K. Immunogenic Cell Death of Breast Cancer Stem Cells Induced by an Endoplasmic Reticulum-Targeting Copper(II) Complex. ChemBioChem 2020, 21, 3618–3624. [Google Scholar] [CrossRef] [PubMed]
- Dhar, S.; Chakravarty, A.R. Efficient visible light induced nuclease activity of a ternary mono-1,10-phenanthroline copper(II) complex containing 2-(methylthio)ethylsalicylaldimine. Inorg. Chem. 2003, 42, 2483–2485. [Google Scholar] [CrossRef] [PubMed]
- Reddy, P.A.; Santra, B.K.; Nethaji, M.; Chakravarty, A.R. Metal-assisted light-induced DNA cleavage activity of 2-(methylthio)phenylsalicylaldimine Schiff base copper(II) complexes having planar heterocyclic bases. J. Inorg. Biochem. 2004, 98, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Waring, M.J. Lipophilicity in drug discovery. Expert Opin. Drug Discov. 2010, 5, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Eskandari, A.; Suntharalingam, K. A reactive oxygen species-generating, cancer stem cell-potent manganese(II) complex and its encapsulation into polymeric nanoparticles. Chem. Sci. 2019, 10, 7792–7800. [Google Scholar] [CrossRef] [PubMed]
- Dontu, G.; Abdallah, W.M.; Foley, J.M.; Jackson, K.W.; Clarke, M.F.; Kawamura, M.J.; Wicha, M.S. In vitro propagation and transcriptional profiling of human mammary stem/progenitor cells. Genes Dev. 2003, 17. [Google Scholar] [CrossRef] [Green Version]
- Sheldrick, G. SADABS: Program for Absorption Correction Using Area Detector Data; University of Göttingen: Göttingen, Germany, 1996. [Google Scholar]
- Sheldrick, G. A short history of SHELX. Acta Cryst. Sect. A 2008, 64, 112–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheldrick, G.M. Crystal structure refinement withSHELXL. Acta Crystallogr. Sect. C 2015, 71, 3–8. [Google Scholar] [CrossRef]
- Dolomanov, O.V.; Bourhis, L.J.; Gildea, R.J.; Howard, J.A.K.; Puschmann, H. OLEX2: A complete structure solution, refinement and analysis program. J. Appl. Crystallogr. 2009, 42, 339–341. [Google Scholar] [CrossRef]
- Farrugia, L.J. WinGXandORTEP for Windows: An update. J. Appl. Cryst. 2012, 45, 849–854. [Google Scholar] [CrossRef]

| Compound | HMLER IC50 [μM] | HMLER-ShEcad IC50 [μM] | Mammosphere IC50 [μM] |
|---|---|---|---|
| 2 | 3.19 ± 0.11 | 3.40 ± 0.05 | 4.14 ± 0.20 |
| 3 | 3.25 ± 0.18 | 3.43 ± 0.10 | 6.08 ± 0.88 |
| 4 | 7.57 ± 0.23 | 12.70 ± 0.14 | 42.55 ± 8.13 |
| 5 | 8.87 ± 0.54 | 12.90 ± 0.14 | 49.10 ± 4.38 |
| salinomycin 1 | 11.40 ± 0.40 | 4.20 ± 0.30 | 18.50 ± 1.50 |
| L2 | 12.91 ± 0.71 | 32.41 ± 0.95 | 64.29 ± 0.20 |
| L3 | 11.20 ± 0.10 | 20.41 ± 0.35 | 52.06 ± 0.31 |
| CuCl2·2H2O 1 | 47.55 ± 0.18 | 47.92 ± 1.80 | n.d. |
| dichloro(1,10-phenanthroline)copper(II) 1 | 4.90 ± 0.17 | 7.86 ± 0.26 | 9.49 ± 0.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Northcote-Smith, J.; Johnson, A.; Singh, K.; Ortu, F.; Suntharalingam, K. Breast Cancer Stem Cell Active Copper(II) Complexes with Naphthol Schiff Base and Polypyridyl Ligands. Inorganics 2021, 9, 5. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics9010005
Northcote-Smith J, Johnson A, Singh K, Ortu F, Suntharalingam K. Breast Cancer Stem Cell Active Copper(II) Complexes with Naphthol Schiff Base and Polypyridyl Ligands. Inorganics. 2021; 9(1):5. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics9010005
Chicago/Turabian StyleNorthcote-Smith, Joshua, Alice Johnson, Kuldip Singh, Fabrizio Ortu, and Kogularamanan Suntharalingam. 2021. "Breast Cancer Stem Cell Active Copper(II) Complexes with Naphthol Schiff Base and Polypyridyl Ligands" Inorganics 9, no. 1: 5. https://0-doi-org.brum.beds.ac.uk/10.3390/inorganics9010005





