Furcation Involvement Classification: A Comprehensive Review and a New System Proposal
Abstract
:1. Introduction
2. Classification of Furcation Lesions
- Degree I: horizontal attachment loss < 3 mm of the total width of the furcation area.
- Degree II: horizontal attachment loss > 3 mm but not encompassing the total width of the furcation area.
- Degree III: “through and through” destruction of the periodontal tissue in the furcation area.
- Subclass A: vertical bone loss 3 mm or less.
- Subclass B: vertical bone loss from 4 to 6 mm.
- Subclass C: bone loss from the fornix of 7 mm or more.
Limitations
- The reference point for the classification is the horizontal attachment loss. However, the subjectivity in the term “early or incipient lesion” (grade I) and the absence of the precise numerical values to identify the horizontal attachment loss create difficulties in the classification between grade I and II.
- In Glickman’s grade III and IV furcation lesion the inter-radicular bone is completely absent, with the difference that in grade IV the furcation entrance is exposed. In this case, grade III and IV would represent a single group considering that the reference point of this classification is the horizontal attachment loss and it is the same for both groups. The difference between them could be represented by creating two subgroups.
- In grade I and II furcation lesions the relationship with gingival margin (clinical exposition of the furcation) is not considered. In such cases, a furcation lesion with incipient bone loss (Glickman’s grade I) but clinically exposed for the presence of gingival recession cannot be classified as grade I but neither as grade IV. The same problem arises for Glickman’s grade II.
- The classification systems quantifying the horizontal attachment loss give rise to the same problem: in none of them one can clearly differentiate between grade I and II since both use the same reference point (less or greater than one third—less or greater than two or three millimeters) [3,11,19], which means that it is not clear in which group furcation involvements with measures of one 1/3 or 2–3 mm will be included.
- When the furcation lesion is partially or not clinically exposed it is difficult to measure the vertical bone loss [4,7,15,16]. In these cases, a routine radiographic image could help only in cases where the inter-radicular bone loss is completely absent (grade III Glickman), and this will be in turn more precise in lower molars, because the overlapping of structures in upper molars makes diagnosis difficult.
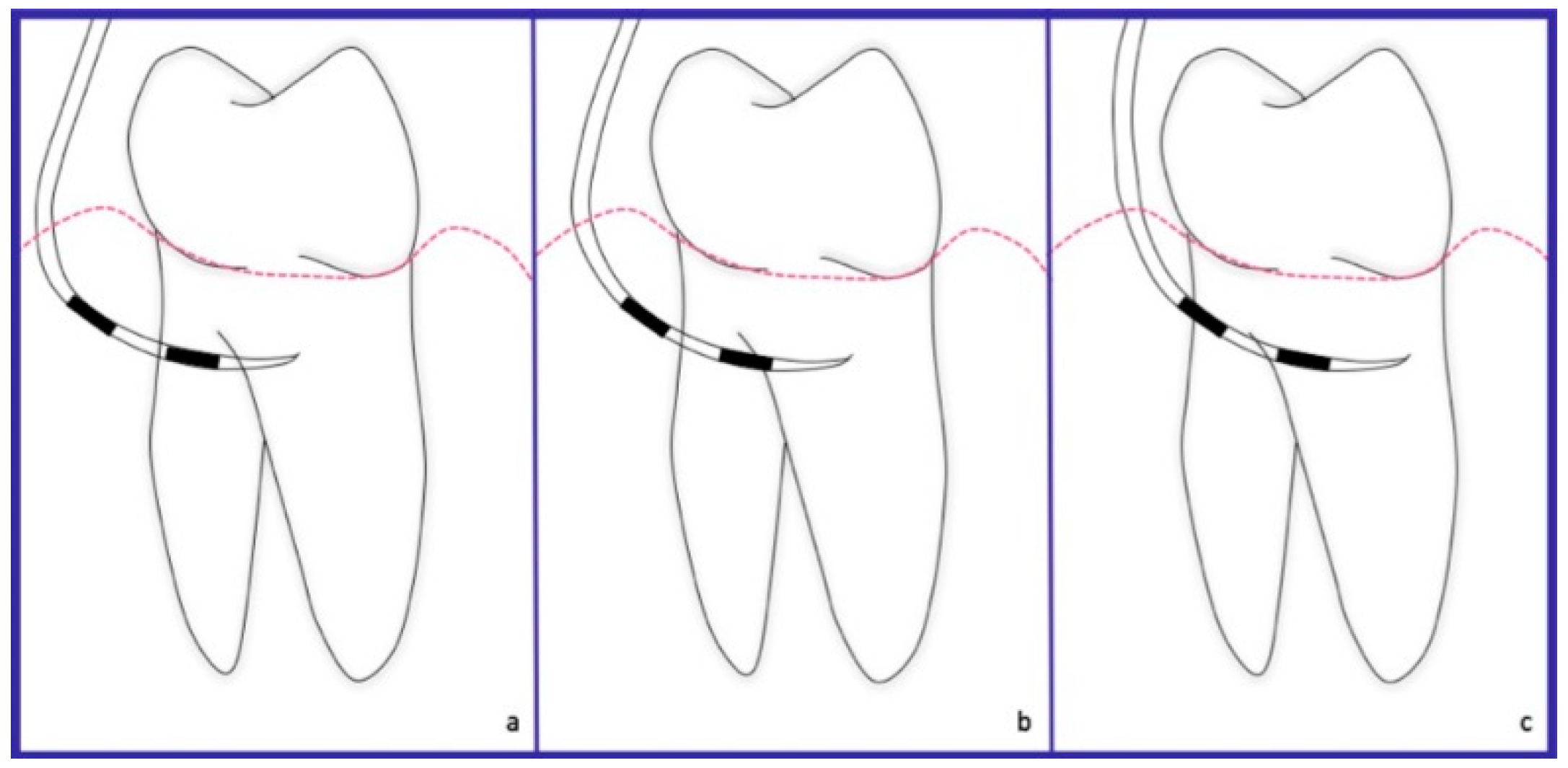
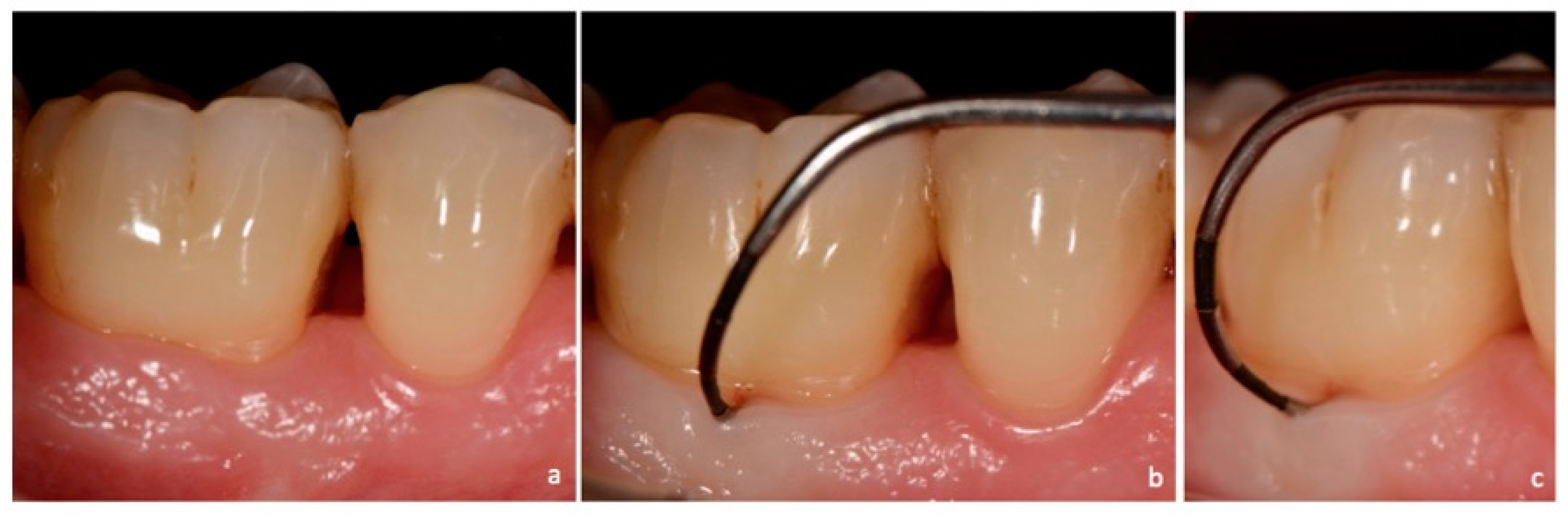
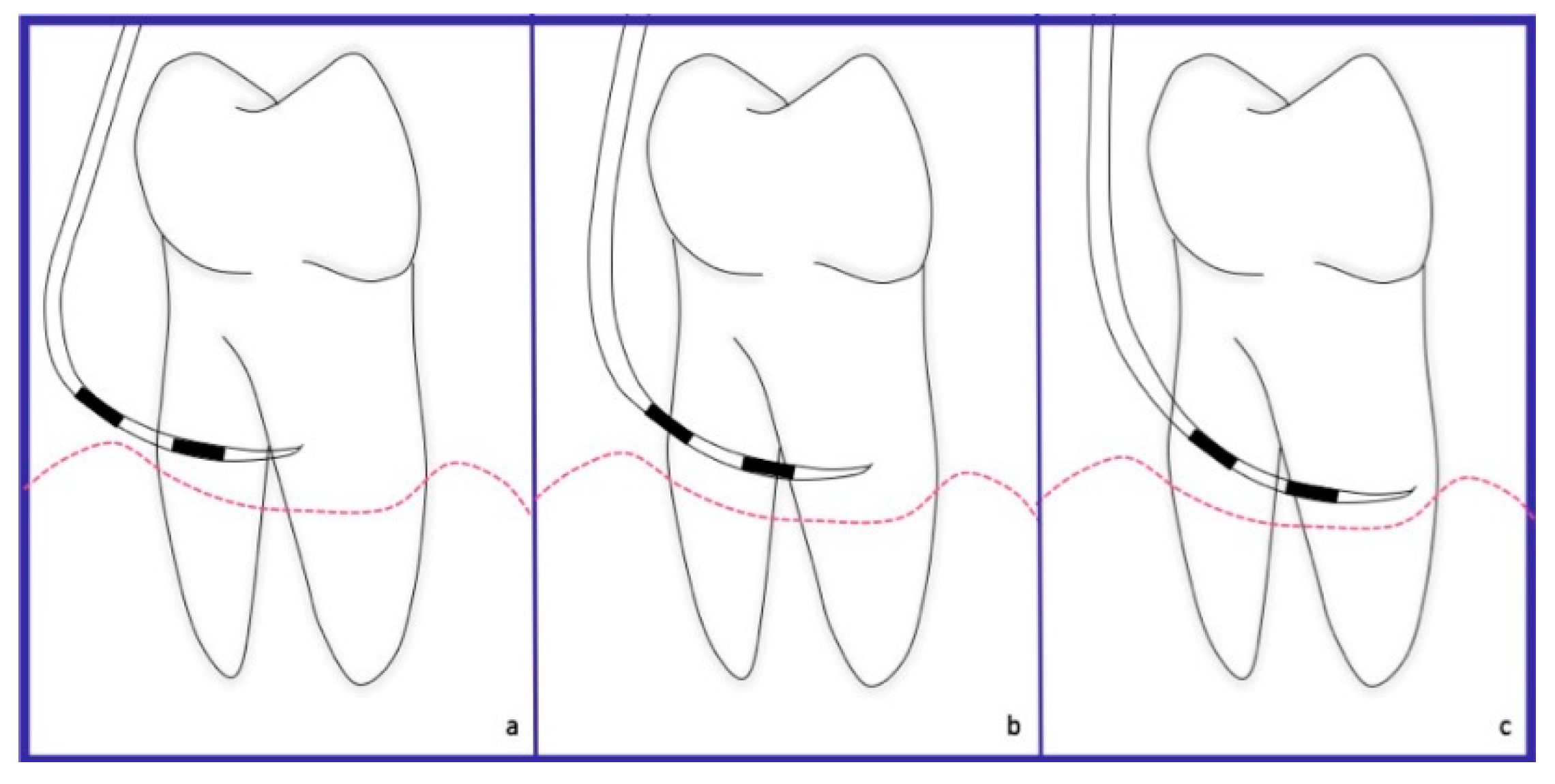
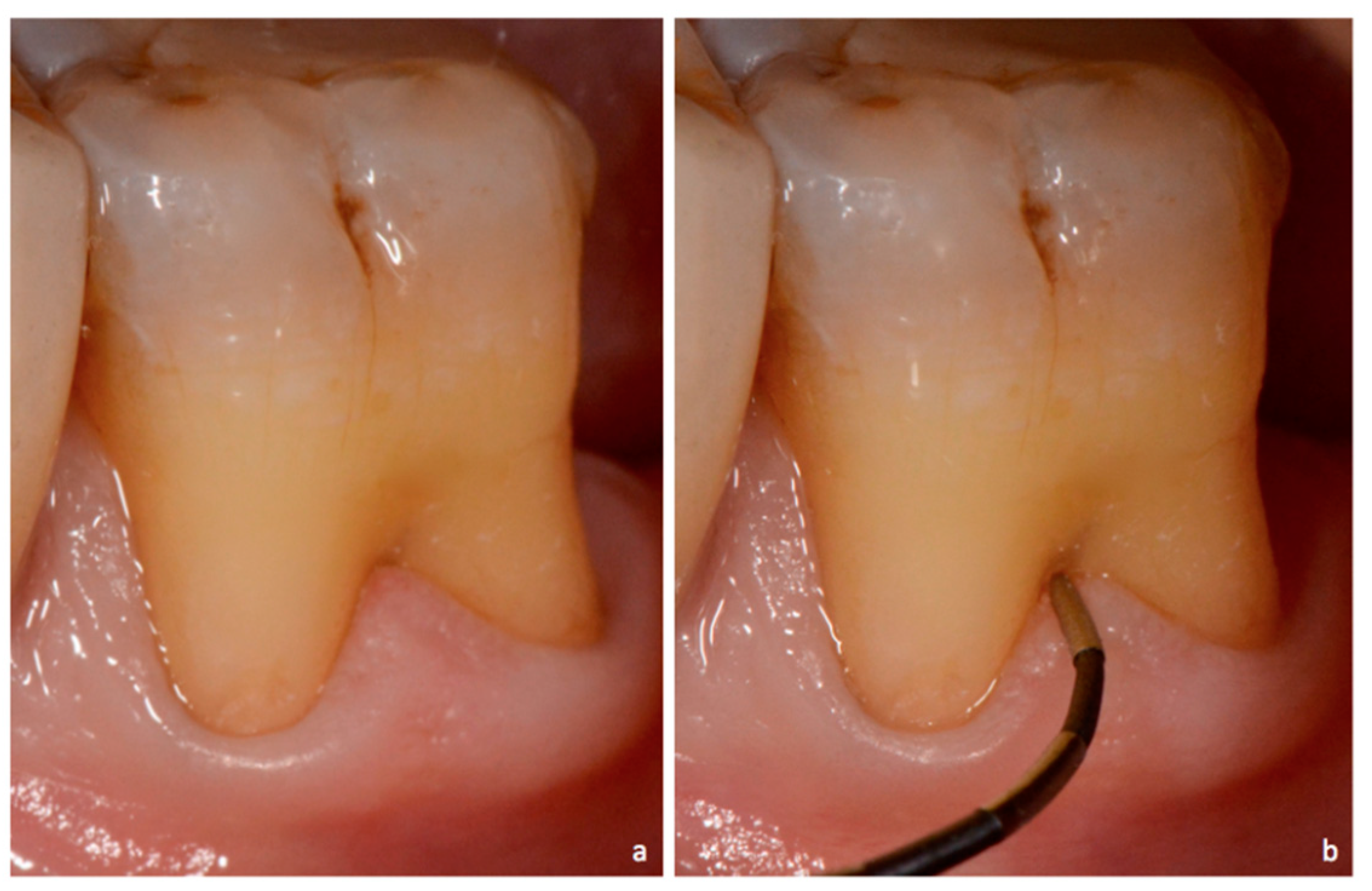
3. Proposed Classification System for Furcation Lesions
- -
- -
- -
Marking Guidelines
4. Discussion
4.1. Diagnosis
4.2. Prognosis and Treatment
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Academy of Periodontology. Glossary of Periodontal Terms, 4th ed.; American Academy of Periodontology: Chicago, LA, USA, 2001; Available online: https://members.perio.org/libraries/glossary (accessed on 2 November 2017).
- Glickman, I. Clinical Periodontology: Prevention, Diagnosis, and Treatment of Periodontal Disease in the Practice of General Dentistry, 4th ed.; Saunders: Philadelphia, PA, USA, 1972; pp. 242–245. ISBN 0721641377. [Google Scholar]
- Hamp, S.E.; Nyman, S.; Lindhe, J. Periodontal treatment of multirooted teeth. Results after 5 years. J. Clin. Periodontol. 1975, 2, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Tarnow, D.; Fletcher, P. Classification of the vertical component of furcation involvement. J. Periodontol. 1985, 55, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Heins, P.J.; Canter, S.R. The furca involvement: A classification of bony deformities. Periodontics 1968, 6, 84–86. [Google Scholar] [PubMed]
- Easley, J.R.; Drennan, G.A. Morphological classification of the furca. J. Can. Dent. Assoc. 1969, 35, 104–107. [Google Scholar] [PubMed]
- Hou, G.L.; Chen, Y.M.; Tsai, C.C.; Weisgold, A.S. A new classification of molar furcation involvement based on the root trunk and horizontal and vertical bone loss. Int. J. Periodontics Restor. Dent. 1998, 18, 257–265. [Google Scholar] [CrossRef]
- Goldman, H.M. Therapy of the incipient bifurcation involvement. J. Periodontol. 1958, 29, 112–116. [Google Scholar] [CrossRef]
- Staffileno, H.J. Surgical management of furca invasión. Dent. Clin. N. Am. 1969, 13, 103–119. [Google Scholar] [PubMed]
- Rosenberg, M.M. Management of osseous defects, furcation involvements, and periodontal-pulpal lesions. In Clinical Dentistry, Periodontal and Oral Surgery; Clark, J.W., Ed.; Harper and Row: Philadelphia, PA, USA, 1986. [Google Scholar]
- Ramfjord, S.P.; Ash, M.M. Periodontology and Periodontics; Saunders: Philadelphia, PA, USA, 1979; pp. 247–309. ISBN 13-978-0721674605. [Google Scholar]
- Goldman, H.M.; Cohen, D.W. Periodontal Therapy, 6th ed.; C. V. Mosby: St. Louis, IL, USA, 1988; p. 921. ISBN 13-9780801618741. [Google Scholar]
- Richetti, P.A. A furcation classification based upon pulp chamber relationships and vertical radiographic bone loss. Int. J. Periodontics Restorative Dent. 1982, 2, 50–59. [Google Scholar]
- Tal, H.; Lemmer, J. Furcal defects in dry mandibles part II: Severity of furcal defects. J. Periodontol. 1982, 53, 364–367. [Google Scholar] [CrossRef] [PubMed]
- Eskow, R.N.; Kapin, S.H. Furcation invasions: Correlating a classification system with therapeutic considerations. Part I. Examination, diagnosis, classification. Compend. Contin. Educ. Dent. 1984, 5, 477–487. [Google Scholar]
- Fedi, P.F., Jr. The Periodontal Syllabus, 2nd ed.; Lea and Febiger: Philadelphia, PA, USA, 1985; pp. 169–170. ISBN 13-978-0781779722. [Google Scholar]
- Grant, D.A.; Stern, I.B.; Listgarten, M.A. Periodontics, 6th ed.; C. V. Mosby: St. Louis, IL, USA, 1988; p. 931. [Google Scholar]
- Basaraba, N. Furcation invasions. In Periodontal Diseases; Schluger, S., Yuodelis, R., Page, R.C., Johnson, R.H., Eds.; Lea and Febiger: Philadelphia, PA, USA, 1990; ISBN 13-978-0812110845. [Google Scholar]
- Carnevale, G.; Pontoriero, R.; Lindhe, J. Treatment of furcation—involved teeth. In Clinical Periodontology and Implant Dentistry, 5th ed.; Lindhe, J., Lang, N.P., Karring, T., Eds.; Munksgaard: Copenhagen, Denmark, 2012; Volume 2, pp. 823–847. ISBN 978-1-118-35561-9. [Google Scholar]
- Nevins, M.; Cappetta, E.G. Treatment of maxillary furcations. In Periodontal Therapy—Clinical Approaches and Evidence of Success; Nevins, M., Mellonig, J.T., Eds.; Quintessence: Chicago, IL, USA, 1998; ISBN 13-978-0867153095. [Google Scholar]
- Walter, C.; Kaner, D.; Berndt, D.C.; Weiger, R.; Zitzmann, N.U. Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. J. Clin. Periodontol. 2009, 36, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Bower, R.C. Furcation morphology relative to periodontal treatment. Furcation entrance arquitecture. J. Periodontol. 1979, 50, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Matia, J.I.; Bissada, N.F.; Maybury, J.E.; Ricchetti, P. Efficiency of scaling of the molar furcation area with and without surgical access. Int. J. Periodontics Restor. Dent. 1986, 6, 25–35. [Google Scholar]
- Fleischer, H.C.; Melloning, J.T.; Brayer, W.K.; Gray, J.L.; Barnet, J.D. Scaling and root planing in multirroted teeth. J. Periodontol. 1989, 60, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Muller, H.P.; Eger, T.; Lange, D.E. Management of furcation-involved teeth. A retrospective analysis. J. Clin. Periodontol. 1995, 22, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Moriarty, J.D.; Hutchens, L.H.; Scheitler, L.E. Histological evaluation of periodontal probe penetration in untreated facial molar furcations. J. Clin. Periodontol. 1989, 16, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Muller, H.P.; Eger, T. Furcation diagnosis. J. Clin. Periodontol. 1999, 26, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Zappa, U.; Grosso, L.; Simona, C.; Graf, H.; Case, D. Clinical furcation diagnoses and interradicular bone defects. J. Periodontol. 1993, 64, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Nordland, P.; Garrett, S.; Kiger, R.; Vanooteghem, R.; Hutchens, L.H.; Egelberg, J. The effect of plaque control and root debridement in molar teeth. J. Clin. Periodontol. 1987, 14, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Loos, B.; Nylund, K.; Claffey, N.; Egelberg, J. Clinical effect of root debridement in molar and non-molar teeth. J. Clin. Periodontol. 1989, 16, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, L.; Wasserman, B. A long-term survey of tooth loss in 600 treated periodontal patients. J. Periodontol. 1978, 49, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Ross, I.F.; Thompson, R. A long term study of root retention in the treatment of maxillary molars with furcation involvement. J. Periodontol. 1978, 49, 238–244. [Google Scholar] [CrossRef] [PubMed]
- McFall, W.T. Tooth loss in 100 treated patients with periodontal disease. A long-term study. J. Periodontol. 1982, 53, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.R.; Greco, G.W.; Mc Fall, W.T. Tooth loss in patients with moderate periodontitis after treatment and long term maintenance care. J. Periodontol. 1989, 60, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.L.; Burgett, F.G.; Shyr, Y.; Ramfjord, S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J. Periodontol. 1994, 65, 25–29. [Google Scholar] [CrossRef] [PubMed]
- McGuire, M.K.; Nunn, M.E. Prognosis versus actual outcome. III. The effectiveness of clinical parameters in accurately predicting tooth survival. J. Periodontol. 1996, 67, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Nunn, M.E.; Fan, J.; Su, X.; Levine, R.A.; Lee, H.J.; McGuire, M.K. Development of prognostic indicators using classification and regression trees for survival. Periodontol. 2000 2012, 58, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Clin. Periodontol. 2018, 45, S149–S161. [Google Scholar] [CrossRef] [PubMed]
- Salvi, G.E.; Mischler, D.C.; Schmidlin, K.; Matuliene, G.; Pjetursson, B.E.; Bragger, U.; Lang, N.P. Risk factors associated with the longevity of multi-rooted teeth. Long-term outcomes after active and supportive periodontal therapy. J. Clin. Periodontol. 2014, 41, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, G.; Cairo, F.; Tonetti, M.S. Long-term effects of supportive therapy in periodontal patients treated with fibre retention osseous resective surgery. II: Tooth extractions during active and supportive therapy. J. Clin. Periodontol. 2007, 34, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, G.; Pontoriero, R.; di Febo, G. Long-term effects of root-resective therapy in furcation-involved molars. A 10-year longitudinal study. J. Clin. Periodontol. 1998, 25, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Papapanou, P.N.; Tonetti, M. Diagnosis and epidemiology of periodontal osseous lesions. Periodontology 2000, 22, 8–21. [Google Scholar] [CrossRef]
- Greenberg, J.; Laster, L.; Listgarten, M.A. Transgingival probing as a potential estimator of alveolar bone level. J. Periodontol. 1976, 47, 514–517. [Google Scholar] [CrossRef] [PubMed]





| Authors | Description |
|---|---|
| Glickman, I. [2] | Grade I: Incipient lesion. Suprabony pocket and slight bone loss in the furcation area. Grade II: Loss of interradicular bone and pocket formation but a portion of the alveolar bone and periodontal ligament remain intact. Grade III: Through-and-through lesion. Grade IV: Through-and-through lesion with gingival recession, leading to a clearly visible furcation area. |
| Goldman, H.M. [8] | Grade I: Incipient lesion. Grade II: Cul-de-sac lesion. Grade III: Through-and-through lesion. |
| Staffileno, H.J. [9] | Class I: Furcations with a soft tissue lesion extending to furcal level but with minor degree of osseous destruction. Class II: Furcations with a soft tissue lesion and variable degree of osseous destruction but not a through-and-through communication through the furca. Class II F: Furcations with osseous destruction from facial aspect only. Class II L: Furcations with osseous destruction from lingual aspect only. Class II M: Furcations with osseous destruction from mesial aspect only. Class II D: Furcations with osseous destruction from distal aspect only. Class III: Furcations with osseous destruction with through-and-through communication. |
| Easley, J.R. et al. [6] | Class I: Incipient involvement, but there is no horizontal component to the furca. Class II: Type 1. Horizontal attachment loss into the furcation. Type 2. Vertical attachment loss into the furcation. Class III: Through-and-through attachment loss into the furcation. Type 1. Horizontal attachment loss into the furcation. Type 2. Vertical attachment loss into the furcation. |
| Hamp, S.E. et al. [3] | Degree I: Horizontal attachment loss < 3 mm. Degree II: Horizontal attachment loss > 3mm not encompassing the total width of the furcation area. Degree III: Horizontal through-and-through destruction of the periodontal tissue in the furcation area. |
| Rosemberg, M.M. [10] | Horizontal Degree I: Probing < 4 mm. Degree II: Probing > 4 mm. Degree III: Two or three furcations classified as degree II are found. Vertical Shallow: Slight lateral extension of an interradicular defect, from the center of the trifurcation in a horizontal direction. Deep: Internal furcation involvement but not penetrating the adjacent furcation. |
| Ramjford, S.P. et al. [11] | Class I: Tissue destruction < 2 mm (1/3 of tooth width) into the furcation. Class II: Tissue destruction > 2 mm (>1/3 of tooth width). Class III: Through-and-through involvement. |
| Goldman, H.M. et al. [12] | Degree I: Involves furcation entrance. Degree II: Involvement extends under the roof of furcation. Degree III: Through-and-through involvement. |
| Richietti, P.A. [13] | Class I: 1 mm of horizontal invasion. Class Ia. 1–2 mm of horizontal invasion. Class II: 2–4 mm of horizontal invasion. Class IIa. 4–6 mm of horizontal invasion. Class III: >6 mm of horizontal invasion. |
| Tal, H. et al. [14] | Furction involvement index (FII) scores: Furcal rating 1: Depth of the furcation is 0 mm. Furcal rating 2: Depth of the furcation is 1–2 mm. Furcal rating 3: Depth of the furcation is 3 mm. Furcal rating 4: Depth of the furcation is 4 mm or more. |
| Tarnow, D. et al. [4] | For each class of horizontal classification (I–III), a subclass based on the vertical bone resorption was added: Subclass A: 0–3 mm. Subclass B: 4–6 mm. Subclass C: >7 mm. |
| Eskow, R.N. et al. [15] | Furcation involvement is classified as grade I subclasses A, B, and C (vertical involvement): Subclass A: Vertical destruction > 1/3. Subclass B: Vertical destruction of 2/3. Subclass C: Vertical destruction beyond apical third of interradicular height. |
| Fedi, P.F. [16] | Glickman + Hamp classifications Grades are the same as Glickman’s classification (I–IV). Grade II is subdivided into degrees I and II. Degree I. Vertical bone loss 1–3 mm. Degree II. Vertical bone loss > 3 mm, but not communicate through-and-through. |
| Grant, D.A. et al. [17] | Class I: Involvement of the flute only. Class II: Involvement partially under the roof. Class III: Through-and-through loss. |
| Basaraba, N. [18] | Class I: Initial furcation involvement. Class II: Partial furcation involvement. Class III: Communicating furcation involvement. |
| Carnevale, G. et al. [19] | Degree I: Horizontal attachment loss < 1/3 Degree II: Horizontal attachment loss > 1/3. Degree III: Horizontal through-and-through destruction. |
| Hou, G.L. et al. [7] | Classification based on root trunk length and horizontal and vertical bone loss. Types of root trunk: Type A: Furcation involving cervical third of root length. Type B: Furcation involving cervical third and cervical two thirds of root length. Type C: Furcation involving cervical two thirds of root length. Classes of furcation: Class I: Horizontal loss of 3 mm. Class II: Horizontal loss > 3 mm. Class III: Horizontal “ through-and-through” loss. Subclasses by radiographic assessment of the periapical view: Sub-class ‘a’. Suprabony defect. Sub-class ‘b’. Infrabony defect. Classification of furcation: AI, AII, AIII. Type A root trunks with class I, class II and class III furcations. BI, BII, BIII. Type B root trunks with class I, class II and class III furcations. CI, CII, CIII. Type C root trunks with class I, class II and class III furcations. |
| Nevins, M. et al. [20] | Class I: Incipient or early loss of attachment. Class II: A deeper invasion and loss of attachment that does not extend to a complete invasion. Class III: Complete loss of periodontium extending from buccal to lingual surface. Diagnosed radiographically and clinically. |
| Glossary of periodontal terms. [1] | Class I: Minimal but notable bone loss in furcation. Class II: Variable degree of bone destruction but not extending completely through furcation. Class III: Bone resorption extending completely through furcation. |
| Walter, C.et al. [21] | Modification of the Hamp et al. classification (degree II is divided into degrees II and II–III) Degree I: Horizontal attachment loss < 1/3 of the width of the tooth. Degree II: Horizontal loss of support > 3 mm, < 6 mm. Degree II–III: Horizontal loss of support > 6 mm, but not extending completely through furcation. Degree III: Horizontal through-and-through destruction. |
| Type/Grade of Furcation Lesion | Characteristics |
|---|---|
| NEI | The furcation lesion is not clinically exposed. The horizontal attachment loss is 2 mm or less. |
| NEII | The furcation lesion is not clinically exposed. The horizontal attachment loss is 3 mm or more. |
| NEIII | The furcation lesion is not clinically exposed. The horizontal attachment loss is total, with through and through opening of the furcation. |
| EI | The furcation lesion is clinically exposed. The horizontal attachment loss is 2 mm or less. |
| EII | The furcation lesion is clinically exposed. The horizontal attachment loss is 3 mm or more. |
| EIII | The furcation lesion is clinically exposed. The horizontal attachment loss is total, with through and through opening of the furcation. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pilloni, A.; Rojas, M.A. Furcation Involvement Classification: A Comprehensive Review and a New System Proposal. Dent. J. 2018, 6, 34. https://0-doi-org.brum.beds.ac.uk/10.3390/dj6030034
Pilloni A, Rojas MA. Furcation Involvement Classification: A Comprehensive Review and a New System Proposal. Dentistry Journal. 2018; 6(3):34. https://0-doi-org.brum.beds.ac.uk/10.3390/dj6030034
Chicago/Turabian StylePilloni, Andrea, and Mariana A. Rojas. 2018. "Furcation Involvement Classification: A Comprehensive Review and a New System Proposal" Dentistry Journal 6, no. 3: 34. https://0-doi-org.brum.beds.ac.uk/10.3390/dj6030034





