Management of Dental Avulsion Injuries: A Survey of Dental Support Staff in Cairns, Australia
Abstract
:1. Introduction
- Reimplantation of the avulsed tooth promptly.
- A subsequent appointment involving a comprehensive clinical and radiographic assessment of the tooth in question.
- Root canal therapy if indicated.
2. Methodology
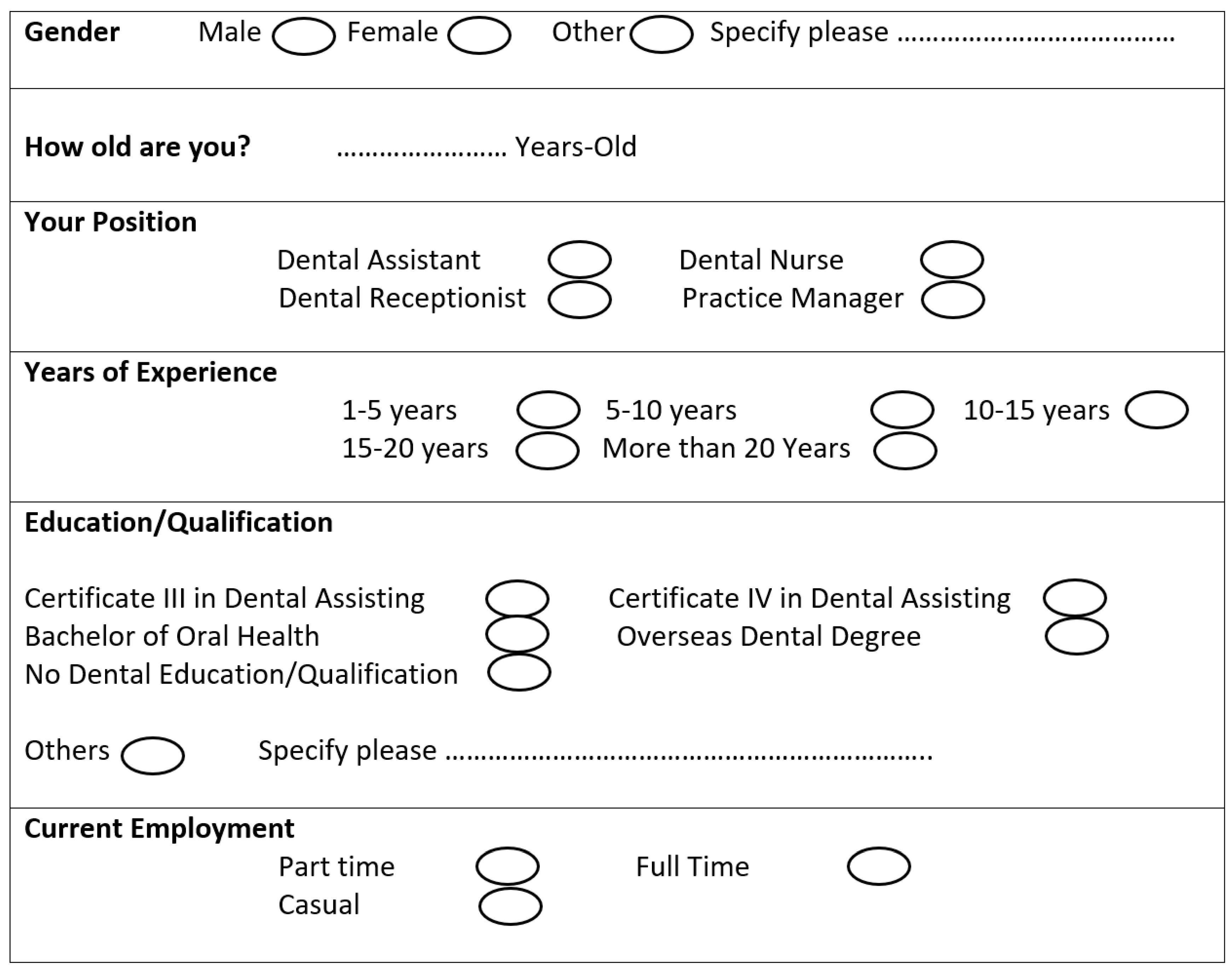
- Demographics including gender, age, years of experience and level of qualification.
- Multiple choice and open-ended questions in relation to the knowledge and management of avulsed teeth.
- Dental avulsion education, including questions regarding prior training or education about dental avulsion.
3. Statistical Method
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey
Appendix A.1. Demographic Information
Appendix A.2. Knowledge and Management of Avulsed Tooth (Knocked-out Tooth from Socket)
- How urgently does a child with a knocked-out tooth need dental treatment?
- Immediately
- Within few hours when dentist is free
- The next day appointment
- Not sure
- Do you expect the knocked-out tooth in this child is a permanent or baby tooth?
- Permanent tooth
- Baby tooth
- Not sure
- Should a permanent knocked-out tooth re-implanted into socket?
- Yes
- No
- Not sure
- Should a baby knocked-out tooth re-implanted into socket?
- Yes
- No
- Not sure
- If the knocked-out tooth is dirty, what advice do you give to clean the dirt?
- Rinse the tooth under running water
- Rinse the tooth with dairy milk
- Wash it with patient’s saliva outside the mouth
- Gently scrub with toothbrush or a clean tissue
- Not sure
- How should they hold the knocked-out tooth while cleaning?
- Hold from crown
- Hold from root
- Doesn’t matter where to hold
- Not sure
- If the knocked-out tooth is not re-implanted into socket, what is the best way to transport it to the clinic?
- Place it in an ice pack
- Place it in patient’s mouth between cheek and teeth
- Wrap it in a paper tissue
- Place it in a liquid medium (next question)
- Not sure
- Which liquid medium is best for storage of the tooth?
- Fresh dairy milk
- Fresh water
- Patient’s saliva
- Salt solution
- Alcohol
- Mouthwash
- Not sure
Appendix A.3. Dental Avulsion Education
- Have you ever had a training or information session for dental avulsion?
- Yes
- No
- Have you ever been supplied with a poster or brochure about management of dental avulsion?
- Yes
- No
- How confident are you in management of dental avulsion?
- Very confident
- To some degree
- Not confident at all
- Do you feel you need more awareness in management of dental avulsion?
- Yes
- No
References
- Flores, M.T.; Andersson, L.; Andreasen, J.O.; Bakland, L.K.; Malmgren, B.; Barnett, F.; Bourguignon, C.; DiAngelis, A.; Hicks, L.; Sigurdsson, A.; et al. Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth. Dent Traumatol. 2007, 23, 130–136. [Google Scholar] [CrossRef]
- Petrovic, B.B.; Markoviä, D.; Peric, T.; Blagojevic, D. Factors related to treatment and outcomes of avulsed teeth. Dent. Traumatol. 2009, 26, 52–59. [Google Scholar] [CrossRef]
- Glendor, U. Epidemiology of traumatic dental injuries—A 12 year review of the literature. Dent. Traumatol. 2008, 24, 603–611. [Google Scholar] [CrossRef]
- Zaleckienė, V.; Peciuliene, V.; Brukiene, V.; Drukteinis, S. Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija 2014, 16, 7–14. [Google Scholar]
- Andersson, L.; Andreasen, J.O.; Day, P.F.; Heithersay, G.; Trope, M.; DiAngelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2012, 28, 88–96. [Google Scholar] [CrossRef]
- Khinda, V.I.; Brar, G.S.; Kallar, S.; Khurana, H. Clinical and Practical Implications of Storage Media used for Tooth Avulsion. Int. J. Clin. Pediatr. Dent. 2017, 10, 158–165. [Google Scholar] [CrossRef]
- Cvek, M.; Granath, L.E.; Hollender, L. Treatment of non-vital permanent incisors with calcium hydroxide. 3. Variation of occurrence of ankylosis of reimplanted teeth with duration of extra-alveolar period and storage environment. Odontol. Rev. 1974, 25, 43–56. [Google Scholar]
- Poi, W.R.; Sonoda, C.K.; Men-Martins, C.; Melo, M.E.; Pellizzer, E.P.; De Mendonça, M.R.; Panzarini, S.R. Storage Media For Avulsed Teeth: A Literature Review. Braz. Dent. J. 2013, 24, 437–445. [Google Scholar] [CrossRef]
- Qazi, S.R.; Nasir, K.S. First-aid knowledge about tooth avulsion among dentists, doctors and lay people. Dent. Traumatol. 2009, 25, 295–299. [Google Scholar] [CrossRef]
- Sigalas, E.; Regan, J.D.; Kramer, P.R.; Witherspoon, D.E.; Opperman, L.A. Survival of human periodontal ligament cells in media proposed for transport of avulsed teeth. Dent. Traumatol. 2004, 20, 21–28. [Google Scholar] [CrossRef]
- Kinoshita, S.; Kojima, R.; Taguchi, Y.; Noda, T. Tooth replantation after traumatic avulsion: A report of 10 cases. Dent. Traumatol. 2002, 18, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Majorana, A.; Bardellini, E.; Conti, G.; Keller, E.; Pasini, S. Root resorption in dental trauma: 45 cases followed for 5 years. Dent. Traumatol. 2003, 19, 262–265. [Google Scholar] [CrossRef] [PubMed]
- De Vasconcellos, L.G.O.; Brentel, A.S.; Vanderlei, A.D.; De Vasconcellos, L.M.R.; Valera, M.C.; De Araújo, M.A.M. Knowledge of general dentists in the current guidelines for emergency treatment of avulsed teeth and dental trauma prevention. Dent. Traumatol. 2009, 25, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.; Bodin, I.; Sorensen, S. Progression of root resorption following replantation of human teeth after extended extraoral storage. Dent. Traumatol. 1989, 5, 38–47. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Lauridsen, E.; Gerds, T.A.; Ahrensburg, S.S. Dental Trauma Guide: A source of evidence-based treatment guidelines for dental trauma. Dent. Traumatol. 2012, 28, 142–147. [Google Scholar] [CrossRef]
- Holan, G.; Ram, D. Aspiration of an avulsed primary incisor. A case report. Int. J. Paediatr. Dent. 2008, 10, 150–152. [Google Scholar] [CrossRef]
- Khan, A.; Goyal, A.; Somaiya, V.; Rathesh, A.; Sathiyamoorthy, J.; Larkin, K.; Currell, S.D.; Nimmo, A.; Nimmo, A.J. Knowledge of Australian primary education providers towards dental avulsion injuries: A cross-sectional study. Aust. Dent. J. 2020, 65, 46–52. [Google Scholar] [CrossRef]
- Halawany, H.S.; Aljazairy, Y.H.; Alhussainan, N.S.; AlMaflehi, N.; Jacob, V.; Abraham, N.B. Knowledge about tooth avulsion and its management among dental assistants in Riyadh, Saudi Arabia. BMC Oral Health 2014, 14, 46. [Google Scholar] [CrossRef] [Green Version]
- Cohenca, N.; Forrest, J.L.; Rotstein, I. Knowledge of oral health professionals of treatment of avulsed teeth. Dent. Traumatol. 2006, 22, 296–301. [Google Scholar] [CrossRef]
- Andersson, L. Epidemiology of Traumatic Dental Injuries. J. Endod. 2013, 39, S2–S5. [Google Scholar] [CrossRef]
- Yigit, Y.; Helvacioglu-Yigit, D.; Kan, B.; Ilgen, C.; Yilmaz, S. Dentofacial traumatic injuries: A survey of knowledge and attitudes among emergency medicine physicians in Turkey. Dent. Traumatol. 2019, 35, 20–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Association of Dental Traumatology. Author Guidelines. Wiley Online Library. Updated 21 November 2020. Available online: https://0-onlinelibrary-wiley-com.brum.beds.ac.uk/page/journal/16009657/homepage/ForAuthors.html (accessed on 14 September 2020).
- Hassan, Z.A.; Schattner, P.; Mazza, D. Doing a Pilot Study: Why Is It Essential? Malays. Fam. Physician 2006, 1, 70–73. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pubmed/27570591 (accessed on 27 August 2020). [PubMed]
- Van Teijlingen, E.; Hundley, V. The importance of pilot studies. Nurs. Stand. 2002, 16, 33–36. [Google Scholar] [CrossRef] [Green Version]
- Australian Bureau of Statistics. Sample Size Calculator. Abs.gov.au; Published 2020. Available online: https://www.abs.gov.au/websitedbs/D3310114.nsf/home/Sample+Size+Calculator (accessed on 28 August 2020).
- Sanders, J.; Stacy, A. Margin of Error Calculator. Good Calculators. Updated 2020. Available online: https://goodcalculators.com/margin-of-error-calculator/ (accessed on 14 September 2020).
- Yunus, G.Y.; Nalwar, A.; Divya Priya, G.K.; Veeresh, D.J. Influence of educational intervention on knowledge and attitude toward emergency management of traumatic dental injuries among nursing students in Da-vangere, India: Pre- and post-design. J. Indian Assoc. Public Health Dent. 2015, 13, 228–233. Available online: http://www.jiaphd.org/article.asp?issn=2319-5932;year=2015;volume=13;issue=3;spage=228;epage=233;aulast=Yunus (accessed on 30 August 2020). [CrossRef]
- Grewal, N.; Shangdiar, G.D.; Samita, G. Efficacy of a comprehensive dental education program regarding management of avulsed permanent teeth as a valid indicator of increased success rate of treatment of avulsion in a North Indian population. Contemp. Clin. Dent. 2015, 6, 477–482. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pmc/articles/PMC4678544/ (accessed on 30 August 2020). [CrossRef]
- Nagata, J.Y.; Góis, V.L.D.A.; Münchow, E.A.; Albuquerque, M.T.P. Dental trauma education intervention as a positive influence among undergraduate students. Eur. J. Dent. 2018, 12, 502–507. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/pmc/articles/PMC6178679/#:~:text=Conclusions%3A,especially%20in%20cases%20of%20avulsion (accessed on 30 August 2020). [CrossRef] [PubMed]
- Levin, L.; Zadik, Y. Education on and prevention of dental trauma: It’s time to act! Dent. Traumatol. 2011, 28, 49–54. [Google Scholar] [CrossRef] [Green Version]
- Raoof, M.; Shokouhinejad, N.; Izadi, A.; Nourzadeh, M.; Afkham, A.; Forghani, F.-R.; Tavallaie, M.; Mohammadalizadeh, S. Long-term effect of an educational intervention regarding dental trauma first aid: A phase II study. Dent. Traumatol. 2014, 30, 296–301. [Google Scholar] [CrossRef]
- Skapetis, T.; Gerzina, T.; Hu, W.C.Y. Managing dental emergencies: A descriptive study of the effects of a multimodal educational intervention for primary care providers at six months. BMC Med. Educ. 2012, 12, 103. [Google Scholar] [CrossRef] [Green Version]
- Young, C.; Wong, K.Y.; Cheung, L.K. Effectiveness of Educational Poster on Knowledge of Emergency Management of Dental Trauma–Part 1. Cluster Randomised Controlled Trial for Primary and Secondary School Teachers. PLoS ONE 2013, 8, e74833. [Google Scholar] [CrossRef] [Green Version]
- Young, C.; Wong, K.Y.; Cheung, L.K. Effectiveness of Educational Poster on Knowledge of Emergency Management of Dental Trauma—Part 2: Cluster Randomised Controlled Trial for Secondary School Students. PLoS ONE 2014, 9, e101972. [Google Scholar] [CrossRef] [Green Version]
- Ghaderi, F.; Adl, A.; Ranjbar, Z. Effect of a leaflet given to parents on knowledge of tooth avulsion. Eur. J. Paediatr. Dent. 2013, 14, 13–16. Available online: http://admin.ejpd.eu/download/EJPD_2013_01_02.pdf (accessed on 30 August 2020).
- Arikan, V.; Sönmez, H. Knowledge level of primary school teachers regarding traumatic dental injuries and their emergency management before and after receiving an informative leaflet. Dent. Traumatol. 2011, 28, 101–107. [Google Scholar] [CrossRef]
| Number | Percentage (%) | |
|---|---|---|
| Gender | ||
| Male | 7 | 11.7 |
| Female | 53 | 88.3 |
| Age | ||
| Below 20 | 0 | 0 |
| 20 to 39 | 33 | 55 |
| 40 to 50 | 12 | 20 |
| Above 50 | 15 | 25 |
| Years of Experience | ||
| 1–5 years | 12 | 20 |
| 5–10 years | 18 | 30 |
| 10–15 years | 9 | 15 |
| 15–20 year | 3 | 5 |
| More than 20 years | 18 | 30 |
| Education/Qualification | ||
| Certificate III in Dental Assisting | 29 | 48.3 |
| Certificate IV in Dental Assisting | 11 | 18.3 |
| Bachelor of Oral Health | 7 | 11.7 |
| Overseas Dental Degree | 3 | 5 |
| No Dental Education/Qualification | 6 | 10 |
| Other | 4 | 6.7 |
| Current Employment | ||
| Part time | 11 | 18.3 |
| Full time | 30 | 50 |
| Casual | 21 | 35 |
| Number | Percentage (%) | |
|---|---|---|
| Previous Avulsion Training | ||
| Yes | 25 | 41.7 |
| No | 35 | 58.3 |
| Received Poster/Brochure about Avulsion Management | ||
| Yes | 13 | 21.7 |
| No | 47 | 78.3 |
| Number | Percentage (%) | |
|---|---|---|
| Urgency for Dental Treatment | ||
| Immediately | 55 | 91.7 |
| Within few hours when dentist is free | 5 | 8.3 |
| The next day appointment | 0 | 0 |
| Not sure | 0 | 0 |
| Awareness of Patient’s Dental Age | ||
| Permanent tooth | 49 | 81.7 |
| Baby tooth | 4 | 6.7 |
| Not sure | 7 | 11.7 |
| Replantation of Permanent Tooth | ||
| Yes | 55 | 91.7 |
| No | 1 | 1.7 |
| Not sure | 4 | 6.7 |
| Replantation of Deciduous Tooth | ||
| Yes | 2 | 3.3 |
| No | 51 | 85 |
| Not sure | 7 | 11.7 |
| Management of an Avulsed Tooth Which Appears Soiled | ||
| Rinse the tooth under running water | 6 | 10 |
| Rinse the tooth with fresh milk | 33 | 55 |
| Wash it with patient saliva outside the mouth | 18 | 30 |
| Gently scrub with toothbrush or a clean tissue | 1 | 1.7 |
| Not sure | 2 | 3.3 |
| Handling of an Avulsed Tooth While Cleaning | ||
| Hold from crown | 53 | 88.3 |
| Hold from root | 0 | 0 |
| Doesn’t matter where to hold | 2 | 3.3 |
| Not sure | 5 | 8.3 |
| Number | Percentage (%) | |
|---|---|---|
| Technique to Transport Tooth | ||
| Ice pack | 1 | 1.7 |
| Patient’s mouth between cheek and teeth | 21 | 35 |
| Paper tissue | 0 | 0 |
| Liquid medium | 33 | 55 |
| Not sure | 5 | 8.3 |
| Liquid Medium Used to Transport Tooth | ||
| Fresh milk | 39 | 65 |
| Fresh water | 1 | 1.7 |
| Patient’s saliva | 17 | 28.3 |
| Saline | 2 | 3.3 |
| Alcohol | 0 | 0 |
| Mouthwash | 0 | 0 |
| Not sure | 1 | 1.7 |
| Number | Percentage (%) | |
|---|---|---|
| Confidence Level | ||
| Very confident | 10 | 16.7 |
| To some degree | 40 | 66.7 |
| Not confident at all | 10 | 16.7 |
| Willingness to Receive Additional Training | ||
| Yes | 52 | 86.7 |
| No | 8 | 13.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abraham, Y.; Christy, R.; Gomez-Kunicki, A.; Cheng, T.; Eskarous, S.; Samaan, V.; Khan, A.; Sholapurkar, A. Management of Dental Avulsion Injuries: A Survey of Dental Support Staff in Cairns, Australia. Dent. J. 2021, 9, 4. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010004
Abraham Y, Christy R, Gomez-Kunicki A, Cheng T, Eskarous S, Samaan V, Khan A, Sholapurkar A. Management of Dental Avulsion Injuries: A Survey of Dental Support Staff in Cairns, Australia. Dentistry Journal. 2021; 9(1):4. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010004
Chicago/Turabian StyleAbraham, Yannis, Roshini Christy, Americo Gomez-Kunicki, Ting Cheng, Silvia Eskarous, Verona Samaan, Ahsen Khan, and Amar Sholapurkar. 2021. "Management of Dental Avulsion Injuries: A Survey of Dental Support Staff in Cairns, Australia" Dentistry Journal 9, no. 1: 4. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010004






