Complex Implant-Prosthetic Rehabilitation Following Sports Trauma with 14 Years of Follow-Up: Case Report
Abstract
:1. Introduction
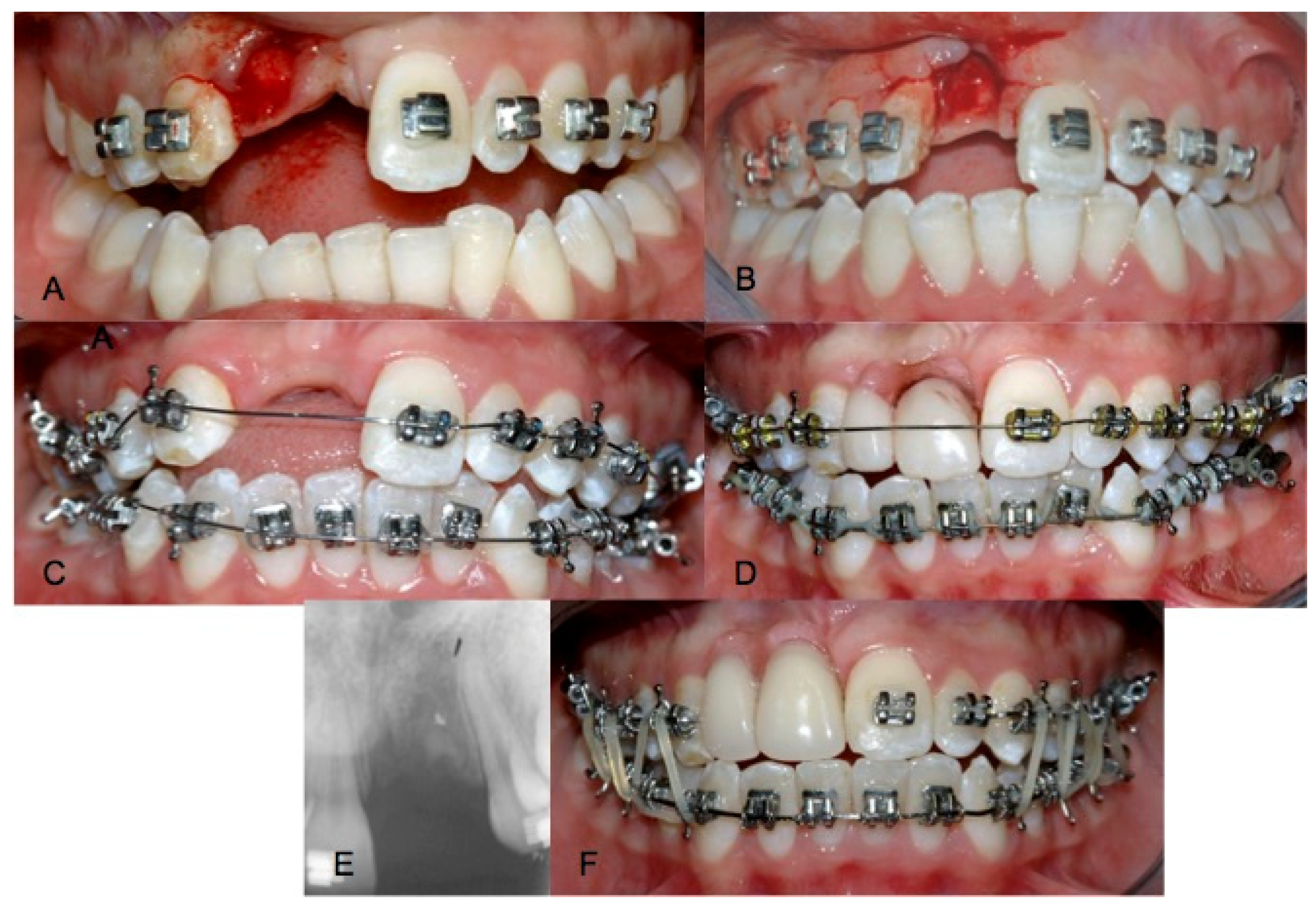
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethical Statement
References
- Giannetti, L.; Murri, A.; Vecci, F.; Gatto, R. Dental avulsion: Therapeutic protocols and oral health-related quality of life. Eur. J. Paediatr. Dent. 2007, 8, 69–75. [Google Scholar]
- Myers, G.L. Evaluation and diagnosis of the traumatized dentition. Dent. Traumatol. 2019, 35, 302–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spinas, E.; Mameli, A.; Giannetti, L. Traumatic Dental Injuries Resulting from Sports Activities; Immediate Treatment and Five Years Follow-Up: An Observational Study. Open Dent. J. 2018, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Reddy, L.V.; Bhattacharjee, R.; Misch, E.; Sokoya, M.; Ducic, Y. Dental Injuries and Management. Facial Plast Surg. 2019, 35, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Giannetti, L.; Diago, A.M.D.; Silingardi, G.; Spinas, E. Superficial infiltration to treat white hypomineralized defects of enamel: Clinical trial with 12-month follow-up. J. Biol. Regul. Homeost. Agents 2018, 32, 1335–1338. [Google Scholar] [PubMed]
- Bissinger, R.; Müller, D.D.; Reymus, M.; Khazaei, Y.; Hickel, R.; Bücher, K.; Kühnisch, J. Treatment outcomes after uncomplicated and complicated crown fractures in permanent teeth. Clin. Oral Investig. 2020, 25, 133–143. [Google Scholar] [CrossRef]
- Giannetti, L.; Diago, A.M.D.; Corciolani, E.; Spinas, E. Deep infiltration for the treatment of hypomineralized enamel lesions in a patient with molar incisor hypomineralization: A clinical case. J. Biol. Regul. Homeost. Agents 2018, 32, 751–754. [Google Scholar]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed.; Blackwell Munksgaard: Oxford, UK, 2007; pp. 383–420. [Google Scholar]
- Giannetti, L.; Murri, A. Clinical evidence and literature to compare two different therapeutic protocols in tooth avulsion. Eur. J. Paediatr. Dent. 2006, 7, 122–130. [Google Scholar]
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; Di Angelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. Guidelines for the Management of Traumatic Dental Injuries: 2. Avulsion of Permanent Teeth. Pediatr. Dent. 2016, 38, 369–376. [Google Scholar]
- Andreasen, J.O.; Schwartz, O.; Kofoed, T.; Daugaard-Jensen, J. Transplantation of premolars as an approach for replacing avulsed teeth. Pediatr. Dent. 2009, 31, 129–132. [Google Scholar]
- Norris, R.T.; Caesar, R.R. Esthetic substitution and autotransplantation of teeth in the maxillary anterior region. Semin. Orthod. 2013, 19, 3–12. [Google Scholar] [CrossRef]
- Spinas, E.; Generali, L.; Mameli, A.; Demontis, C.; Martinelli, D.; Giannetti, L. Delayed tooth replantation and inflammatory root resorption in childhood and adolescence. J. Biol. Regul. Homeost. Agents 2019, 33, 623–627. [Google Scholar] [PubMed]
- Gautam, R.; Nene, P.; Mehta, K.; Nene, S.; Hegde, A.; Jaju, R. Treatment strategies for missing maxillary central incisor—An orthodontist’s perspective. J. Prosthodont. 2014, 23, 509–513. [Google Scholar] [CrossRef]
- Waggoner, W.F.; Kupietzky, A. Anterior esthetic fixed appliances for the preschooler: Considerations and a technique for placement. Paediatr. Dent. 2001, 23, 147–150. [Google Scholar]
- Giannetti, L.; Spinas, E.; Diago, A.M.D.; Consolo, U.; Generali, L. Implant conometric connection through innovative prosthetic abutment: Biological, clinical, surgical, and prosthetic aspects. J. Biol. Regul. Homeost. Agents 2019, 33, 287–290. [Google Scholar]
- Jung, R.E.; Heitz-Mayfield, L.; Schwarz, F.; Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 3-Aesthetics of peri-implant soft tissues. Clin. Oral Implants Res. 2018, 29 (Suppl. S15), 14–17. [Google Scholar] [CrossRef] [Green Version]
- Giannetti, L.; Diago, A.M.D.; Vecci, F.; Consolo, U. Mini-implants in growing patients: A case report. Pediatr. Dent. 2010, 32, 239–244. [Google Scholar]
- Cope, J.B.; McFadden, D. Temporary replacement of missing maxillary lateral incisors with orthodontic miniscrew implants in growing pa- tients: Rationale, clinical technique, and long-term results. J. Orthod. 2014, 41 (Suppl. S1), 62–74. [Google Scholar] [CrossRef]
- Giannetti, L.; Apponi, R.; Diago, A.M.D.; Mintrone, F. Rehabilitation of a patient with mini-implants after avulsion of the upper incisors: A 13-year follow up. Dent. Traumatol. 2020. [Google Scholar] [CrossRef]
- Giannetti, L.; Spinas, E.; Diago, A.M.D. Tooth avulsion with extra oral time in less than 60 minutes: Two different therapeutic protocols with 13-year follow-up. J. Biol. Regul. Homeost. Agents 2019, 33, 629–631. [Google Scholar]
- Waldon, K.; Barber, S.K.; Spencer, R.J.; Duggal, M.S. Indications for the use of auto-transplantation of teeth in the child and adolescent. Eur. Arch. Paediatr. Dent. 2012, 13, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Aresu, M.; Canargiu, F.; Giannetti, L. Preventive treatment of post-traumatic dental infraocclusion: Study on the knowledge of dental decoronation in a sample of Italian dental students and dentists. Eur. J. Paediatr. Dent. 2015, 16, 279–283. [Google Scholar] [PubMed]
- Bohner, L.; Hanisch, M.; Kleinheinz, J.; Jung, S. Dental implants in growing patients: A systematic review. Br. J. Oral Maxillofac. Surg. 2019, 57, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Kamatham, R.; Avisa, P.; Vinnakota, D.N.; Nuvvula, S. Adverse effects of implants in children and adolescents: A systematic review. J. Clin. Pediatr. Dent. 2019, 43, 69–77. [Google Scholar] [CrossRef]
- Pomini, M.C.; Samra, A.P.B.; Fischborn, A.R.; Kozlowski, V.A., Jr.; Alves, F.B.T. The use of mini-implants for provisional prosthetic rehabilitation in growing patients: A critical review. J. Prosthodont. Res. 2020. [Google Scholar] [CrossRef]
- Giannetti, L.; Forabosco, E.; Spinas, E.; Re, D.; Diago, A.M.D. Single tooth anaesthesia: A new approach to the paediatric patient. A clinical experimental study. Eur. J. Paediatr. Dent. 2018, 19, 40–43. [Google Scholar]
- Bucher, K.; Neumann, C.; Thiering, E.; Hickel, R.; Kuhnisch, J. International Association of Dental Traumatology Complications and survival rates of teeth after dental trauma over a 5-year period. Clin. Oral Investig. 2013, 17, 1311–1318. [Google Scholar] [CrossRef]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar] [CrossRef]
- Fernandes, L.M.; Neto, J.C.L.; Lima, T.F.R.; Magno, M.B.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.F.D. The use of mouthguards and prevalence of dento-alveolar trauma among athletes: A systematic review and meta-analysis. Dent. Traumatol. 2019, 35, 54–72. [Google Scholar] [CrossRef]
- Spinas, E.; Aresu, M.; Giannetti, L. Use of mouth guard in basketball: Observational study of a group of teenagers with and without motivational reinforcement. Eur. J. Paediatr. Dent. 2014, 15, 392–396. [Google Scholar]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murri dello Diago, A.; Apponi, R.; Colombini, V.; Mordini, L.; Ideo, F. Complex Implant-Prosthetic Rehabilitation Following Sports Trauma with 14 Years of Follow-Up: Case Report. Dent. J. 2021, 9, 6. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010006
Murri dello Diago A, Apponi R, Colombini V, Mordini L, Ideo F. Complex Implant-Prosthetic Rehabilitation Following Sports Trauma with 14 Years of Follow-Up: Case Report. Dentistry Journal. 2021; 9(1):6. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010006
Chicago/Turabian StyleMurri dello Diago, Alberto, Roberto Apponi, Vittorio Colombini, Lorenzo Mordini, and Francesca Ideo. 2021. "Complex Implant-Prosthetic Rehabilitation Following Sports Trauma with 14 Years of Follow-Up: Case Report" Dentistry Journal 9, no. 1: 6. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9010006





