Assessment of Tooth Preparations Submitted to Dental Laboratories for Fabrication of Monolithic Zirconia Crowns
Abstract
:1. Introduction
2. Materials and Methods
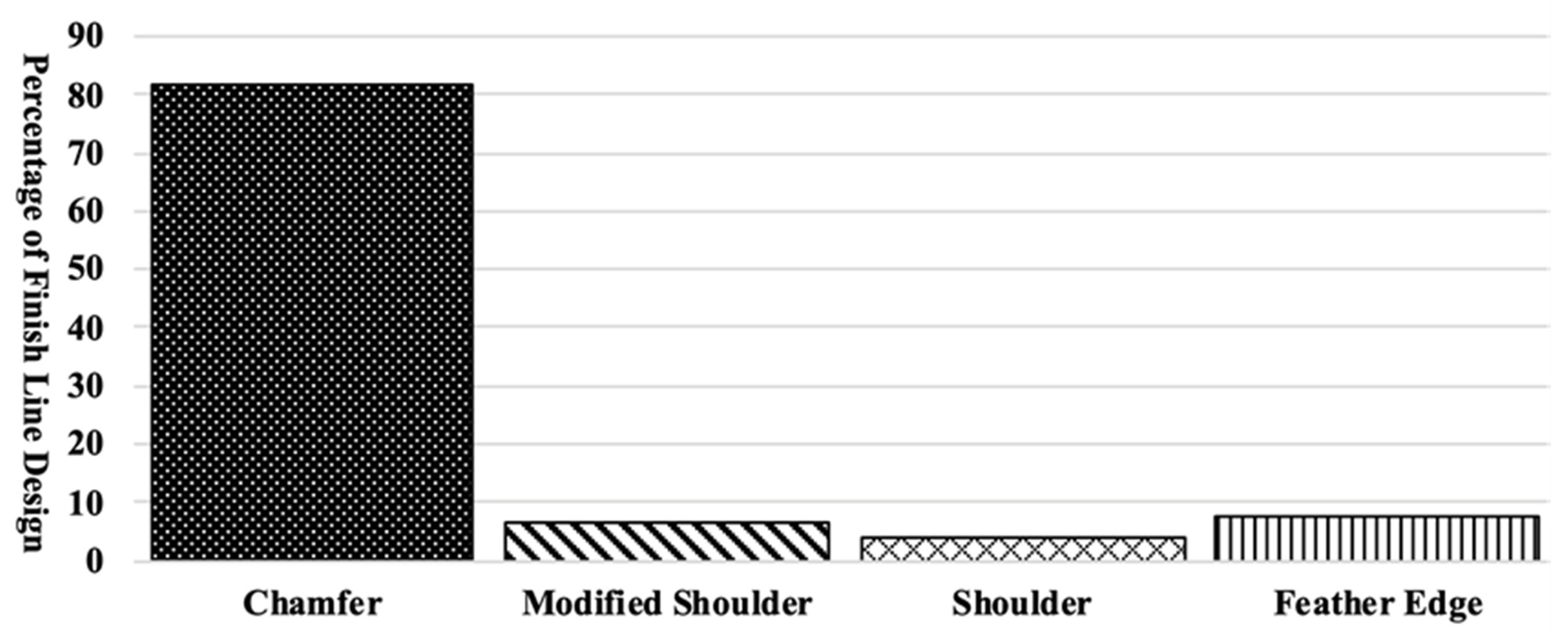
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martins, L.M.; Lorenzoni, F.C.; Melo AO, D.; Silva LM, D.; Oliveira JL, G.D.; Oliveira PC, G.D.; Bonfante, G. Internal fit of two all-ceramic systems and metal-ceramic crowns. J. Appl. Oral. Sci. 2012, 20, 235–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ditolla, M.C. Why Dentists Love BruxZir Solid Zirconia. Available online: https://www.dentaltown.com/magazine/article/3861/why-dentists-love-bruxzir-solid-zirconia (accessed on 26 May 2021).
- Donovan, T.E. Factors essential for successful all-Ceramic restorations. J. Am. Dent. Assoc. 2008, 139, 14S–18S. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. Is the rush to all-ceramic crowns justified? J. Am. Dent. Assoc. 2014, 145, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Makhija, S.K.; Lawson, N.C.; Gilbert, G.H.; Litaker, M.S.; McClelland, J.A.; Louis, D.R.; Gordan, V.V.; Pihlstrom, D.J.; Meyerowitz, C.; Mungia, R. Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J. Dent. 2016, 55, 40–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Withrow, D. By the Numbers: What Dentists Prescribed in 2015. Chairside Dental Magazine 2019. Available online: https://glidewelldental.com/education/chairside-dental-magazine/volume-11-issue-3/digital-impressions (accessed on 8 April 2019).
- Goodacre, C.J.; Campagni, W.V.; Aquilino, S.A. Tooth preparations for complete crowns: An art form based on scientific principles. J. Prosthet Dent. 2001, 85, 363–376. [Google Scholar] [CrossRef] [Green Version]
- Souza RO, A.; Özcan, M.; Pavanelli, C.A.; Buso, L.; Lombardo GH, L.; Michida, S.M.A.; Mesquita, A.M.M.; Bottino, M.A. Marginal and internal discrepancies related to margin design of ceramic crowns fabricated by a CAD/CAM system. J. Prosthodont 2012, 21, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.R.; Asiri, W.; Hefne, M.J. Effect of anatomic, semi-anatomic and non-anatomic occlusal surface tooth preparations on the adaptation of zirconia copings. J. Adv. Prosthodont. 2014, 6, 444–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shillingburg, H.T.; Hobo, S.; Whitsett, L.D. Principles of Tooth Preparations, Fundamentals of Fixed Prosthodontics, 4th ed.; Quintessence Pub Co.: Chicago, IL, USA, 1981; pp. 131–148. [Google Scholar]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Principles of Tooth Preparation; Contemporary Fixed Prosthodontics, 4th ed.; Mosby: St. Louis, MO, USA, 1995; pp. 209–257. [Google Scholar]
- Wilson, A.H., Jr.; Chan, D.C. The relationship between preparation convergence and retention of extracoronal retainers. J. Prosthodont. 1994, 3, 74–78. [Google Scholar] [CrossRef]
- Tiu, J.; Lin, T.; Al-Amleh, B.; Waddell, J.N. Convergence angles and margin widths of tooth preparations by New Zealand dental students. J. Prosthet. Dent. 2016, 116, 74–79. [Google Scholar] [CrossRef]
- Tiu, J.; Al-Amleh, B.; Waddell, J.N. Reporting numeric values of complete crowns. Part 1: Clinical preparation parameters. J. Prosthet. Dent. 2015, 114, 67–74. [Google Scholar] [CrossRef]
- Alammari, M.R.; Abdelnabi, M.H.; Swelem, A.A. Effect of total occlusal convergence on fit and fracture resistance of zirconia-reinforced lithium silicate crowns. Clin. Cosmet. Investig. Dent. 2018, 31, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mou, S.H.; Chai, T.; Wang, J.S.; Shiau, Y.Y. Influence of different convergence angles and tooth preparation heights on the internal adaptation of Cerec crowns. J. Prosthet. Dent. 2002, 87, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Mou, S.H.; Chai, T.; Wang, J.S.; Shiau, Y.Y. Microtensile bond strength of different components of core veneered all-ceramic restorations. Dent. Mater. 2005, 21, 984–991. [Google Scholar]
- Esquivel-Upshaw, J.; Rose, W.; Oliveira, E.; Yang, M.; Clark, A.E.; Anusavice, K. Randomized controlled clinical trial of bilayer ceramic and metal-ceramic crown performance. J. Prosthodont. 2013, 22, 166–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmadzadeh, A.; Golmohammadi, F.; Mousavi, N. Effect of Marginal Design on Fracture Resistance of IPS e. max all Ceramic Restorations: Chamfer Versus Shoulder Finish Lines. J. Islam. Dental. Assoc. Iran. 2015, 27, 64–69. [Google Scholar]
- Dhima, M.; Carr, A.B.; Salinas, T.J.; Lohse, C.; Berglund, L.; Nan, K.A. Evaluation of fracture resistance in aqueous environment under dynamic loading of lithium disilicate restorative systems for posterior applications. Part 2. J. Prosthodont. 2014, 23, 353–357. [Google Scholar] [CrossRef]
- Heintze, S.D.; Rousson, V. Survival of zirconia- and metal-supported fixed dental prostheses: A systematic review. Int. J. Prosthodont. 2010, 23, 493–502. [Google Scholar]
- Flinn, B.D.; Raigrodski, A.J.; Mancl, L.A.; Toivola, R.; Kuykendall, T. Influence of aging on flexural strength of translucent zirconia for monolithic restorations. J. Prosthet. Dent. 2017, 117, 303–309. [Google Scholar] [CrossRef]
- Lin, W.S.; Ercoli, C.; Feng, C.; Morton, D. The effect of core material, veneering porcelain, and fabrication technique on the biaxial flexural strength and Weibull analysis of selected dental ceramics. J. Prosthodont. 2012, 21, 353–362. [Google Scholar] [CrossRef]
- Baladhandayutham, B.; Lawson, N.C.; Burgess, J.O. Fracture load of ceramic restorations after fatigue loading. J. Prosthet. Dent. 2015, 114, 266–271. [Google Scholar] [CrossRef]
- Nakamura, K.; Harada, A.; Inagaki, R.; Kanno, T.; Niwano, Y.; Milleding, P.; Örtengren, U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta. Odontol. Scand. 2015, 73, 602–608. [Google Scholar] [CrossRef]
- Weigl, P.; Sander, A.; Wu, Y.; Felber, R.; Lauer, H.C.; Rosentritt, M. In-vitro performance and fracture strength of thin monolithic zirconia crowns. J. Adv. Prosthodont. 2018, 10, 79–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Euán, R.; Figueras-Álvarez, O.; Cabratosa-Termes, J.; Oliver-Parra, R. Marginal adaptation of zirconium dioxide copings: Influence of the CAD/CAM system and the finish line design. J. Prosthet. Dent. 2014, 11, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Re, D.; Cerutti, F.; Augusti, G.; Cerutti, A.; Augusti, D. Comparison of marginal fit of Lava CAD/CAM crown-copings with two finish lines. Int. J. Esthet. Dent. 2014, 9, 426–435. [Google Scholar] [PubMed]
- Euán, R.; Figueras-Álvarez, O.; Cabratosa-Termes, J.; Brufau-de Barberà, M.; Gomes-Azevedo, S. Comparison of the marginal adaptation of zirconium dioxide crowns in preparations with two different finish lines. J. Prosthodont. 2012, 2, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Mitov, G.; Anastassova-Yoshida, Y.; Nothdurft, F.P.; Von See, C.; Pospiech, P. Influence of the preparation design and artificial aging on the fracture resistance of monolithic zirconia crowns. J. Adv. Prosthodont. 2016, 8, 30–36. [Google Scholar] [CrossRef] [Green Version]
- Renne, W.; McGill, S.T.; Forshee, K.V.; DeFee, M.R.; Mennito, A.S. Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J. Prosthet. Dent. 2012, 108, 310–315. [Google Scholar] [CrossRef]
- Walton, C.B.; Leven, M.M. A preliminary report of photoelastic tests of strain within jacket crowns. J. Am. Dent. Assoc. 1955, 50, 44–48. [Google Scholar] [CrossRef]
- Craig, R.G.; el-Ebrashi, M.K.; Peyton, F.A. Experimental stress analysis of dental restorations. Part II. Two-dimensional photoelastic stress analysis of crowns. J. Prosthet. Dent. 1967, 17, 292–302. [Google Scholar] [CrossRef]
- Nicholls, J.I. Crown retention. I. Stress analysis of symmetric restorations. J. Prosthet. Dent. 1974, 31, 179–184. [Google Scholar]
- Sadid-Zadeh, R.; Li, R.; Miller, L.M.; Simon, M. Effect of Fabrication Technique on the Marginal Discrepancy and Resistance of Lithium Disilicate Crowns: An In Vitro Study. J. Prosthodont. 2019. [Google Scholar] [CrossRef]
- Tjan, A.H.L.; Sarkissian, R. Effect of preparation finish on retention and fit of complete crowns. J. Prosthet. Dent. 1986, 56, 283–288. [Google Scholar] [CrossRef]
- Tuntiprawon, M. Effect of surface roughness on marginal seating and retention of complete metal crowns. J. Prosthet. Dent. 1999, 81, 142–147. [Google Scholar] [CrossRef]
- Felton, D.A.; Kanoy, B.E.; White, J.T. The effect of surface roughness of crown preparations on retention of cemented castings. J. Prosthet. Dent. 1987, 58, 292–296. [Google Scholar] [CrossRef]
- Sinhori, B.S.; de Andrada, M.A.C.; Carpena Lopes, G.; Monteiro Junior, S.; Baratieri, L.N. Influence of Teeth Preparation Finishing on the Adaptation of Lithium Disilicate Crowns. Int. J. Biomater. 2017, 2017, 2078526. [Google Scholar]
- Kim, J.H.; Cho, B.H.; Lee, J.H.; Kwon, S.J.; Yi, Y.A.; Shin, Y.; Roh, B.-D.; Seo, D.G. Influence of preparation design on fit and ceramic thickness of CEREC 3 partial ceramic crowns after cementation. Acta. Odontol. Scand. 2015, 7, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Sadid-Zadeh, R.; Li, R.; Patel, R.; Makowka, S.; Miller, L.M. Impact of Occlusal Intercuspal Angulation on the Quality of CAD/CAM Lithium Disilicate Crowns. J. Prosthodont. 2019. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. Frequently encountered errors in tooth preparations for crowns. J. Am. Dent. Assoc. 2007, 138, 1373–1375. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.B.; Wildgoose, D.G.; Winstanley, R.B. Comparison of convergence angles achieved in posterior teeth prepared for full veneer crowns. Eur. J. Prosthodont. Restor. Dent. 2005, 13, 100–104. [Google Scholar]
- Ali, A.; AlWazzan, K.A.; AlAmri, M.D.; AlShahrani, A.; AlShahrani, M.; AlQahtani, H. Assessment of convergence angle of full veneer preparations carried out by practitioners with different levels of experience. Saudi. Den. J. 2009, 21, 37–44. [Google Scholar]
- Winkelmeyer, C.; Wolfart, S.; Marotti, J. Analysis of tooth preparations for zirconia-based crowns and fixed dental prostheses using stereolithography data sets. J. Prosthet. Dent. 2016, 116, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007, 38, 745–753. [Google Scholar] [PubMed]
- May, L.G.; Kelly, J.R.; Bottino, M.A.; Hill, T. Effects of cement thickness and bonding on the failure loads of CAD/CAM ceramic crowns: Multi-physics FEA modeling and monotonic testing. Dent. Mater 2012, 28, e99–e109. [Google Scholar] [CrossRef]
- Tuntiprawon, M.; Wilson, T. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust. Dent. J. 1995, 40, 17–21. [Google Scholar] [CrossRef] [PubMed]

| Max. Premolar | Mand. Premolar | Max. 1st Molar | Mand. 1st Molar | Max. 2nd Molar | Mand. 2nd Molar | Total | |
|---|---|---|---|---|---|---|---|
| Number of evaluated preparations | 79 | 34 | 72 | 100 | 45 | 62 | 392 |
| Number of preparations with unacceptable OCD | 27 | 17 | 63 | 69 | 37 | 60 | 273 |
| Number of preparations with unacceptable TOC | 59 | 31 | 67 | 96 | 42 | 55 | 350 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sadid-Zadeh, R.; Sahraoui, H.; Lawson, B.; Cox, R. Assessment of Tooth Preparations Submitted to Dental Laboratories for Fabrication of Monolithic Zirconia Crowns. Dent. J. 2021, 9, 112. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9100112
Sadid-Zadeh R, Sahraoui H, Lawson B, Cox R. Assessment of Tooth Preparations Submitted to Dental Laboratories for Fabrication of Monolithic Zirconia Crowns. Dentistry Journal. 2021; 9(10):112. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9100112
Chicago/Turabian StyleSadid-Zadeh, Ramtin, Hadjer Sahraoui, Brian Lawson, and Robert Cox. 2021. "Assessment of Tooth Preparations Submitted to Dental Laboratories for Fabrication of Monolithic Zirconia Crowns" Dentistry Journal 9, no. 10: 112. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9100112





