Management of the Sequelae of a Sport-Related Traumatic Dental Injury Using Ultrasound Examination in the Diagnosis and Follow-Up
Abstract
:1. Introduction
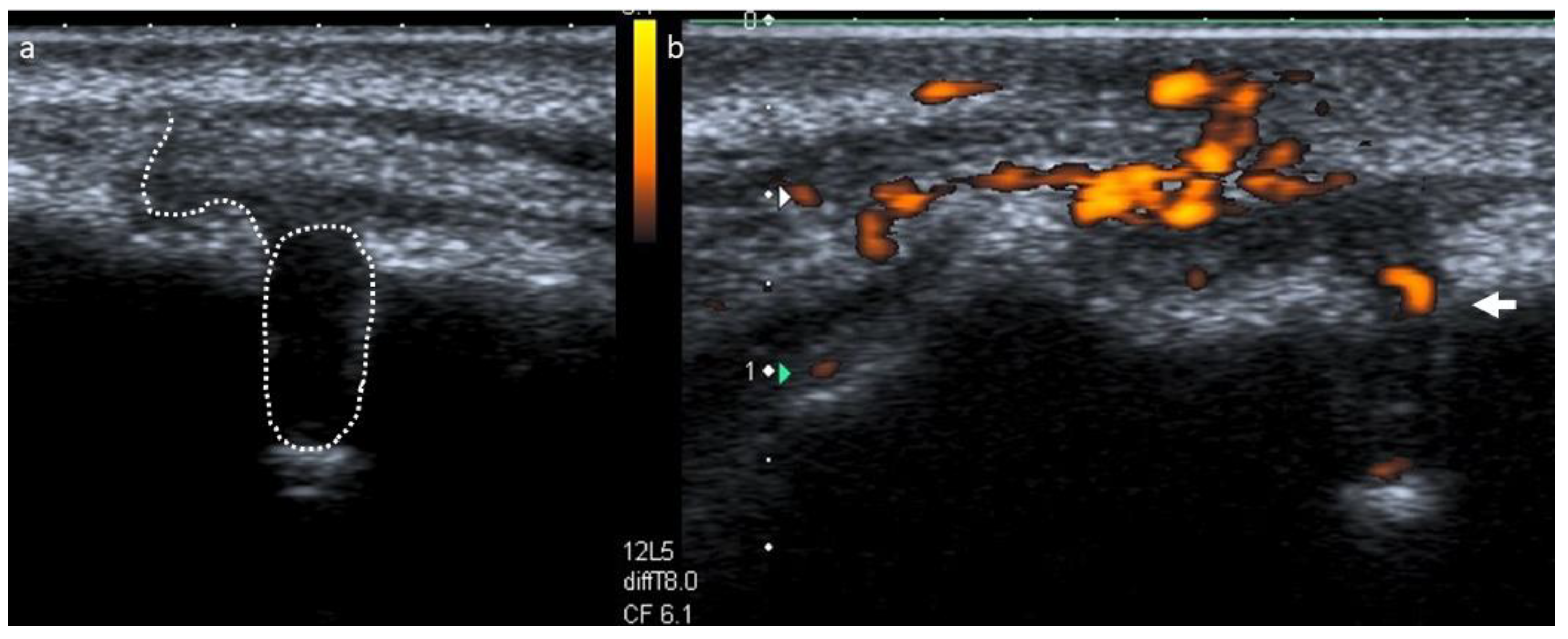
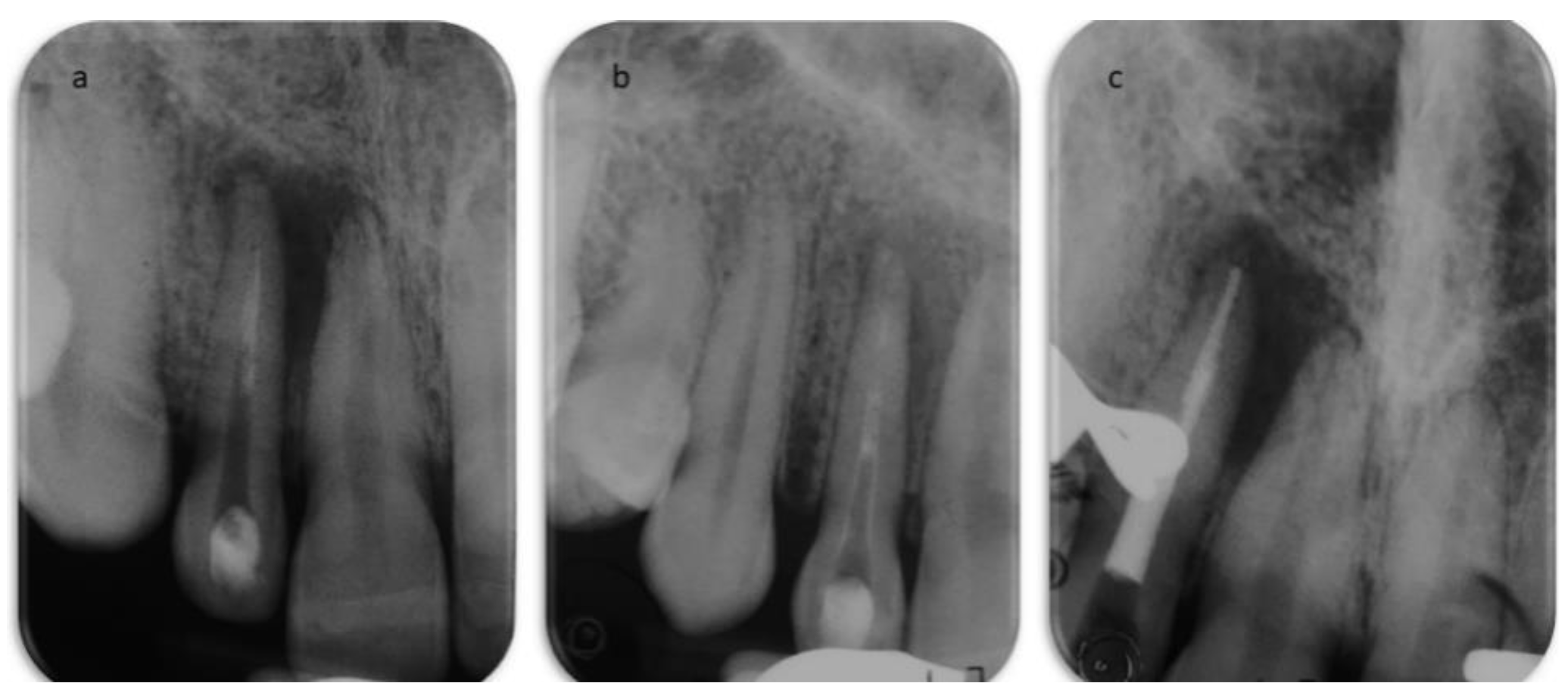
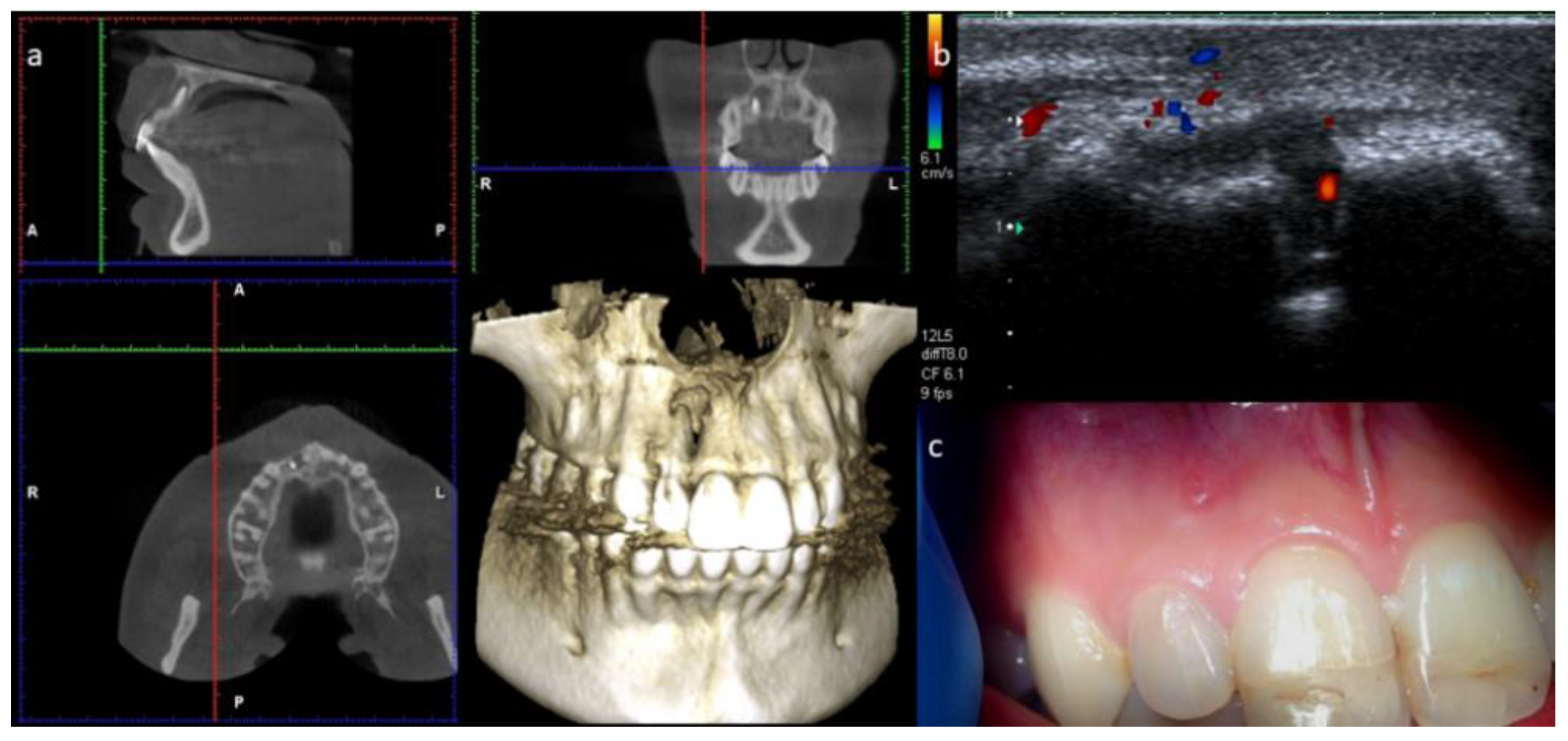
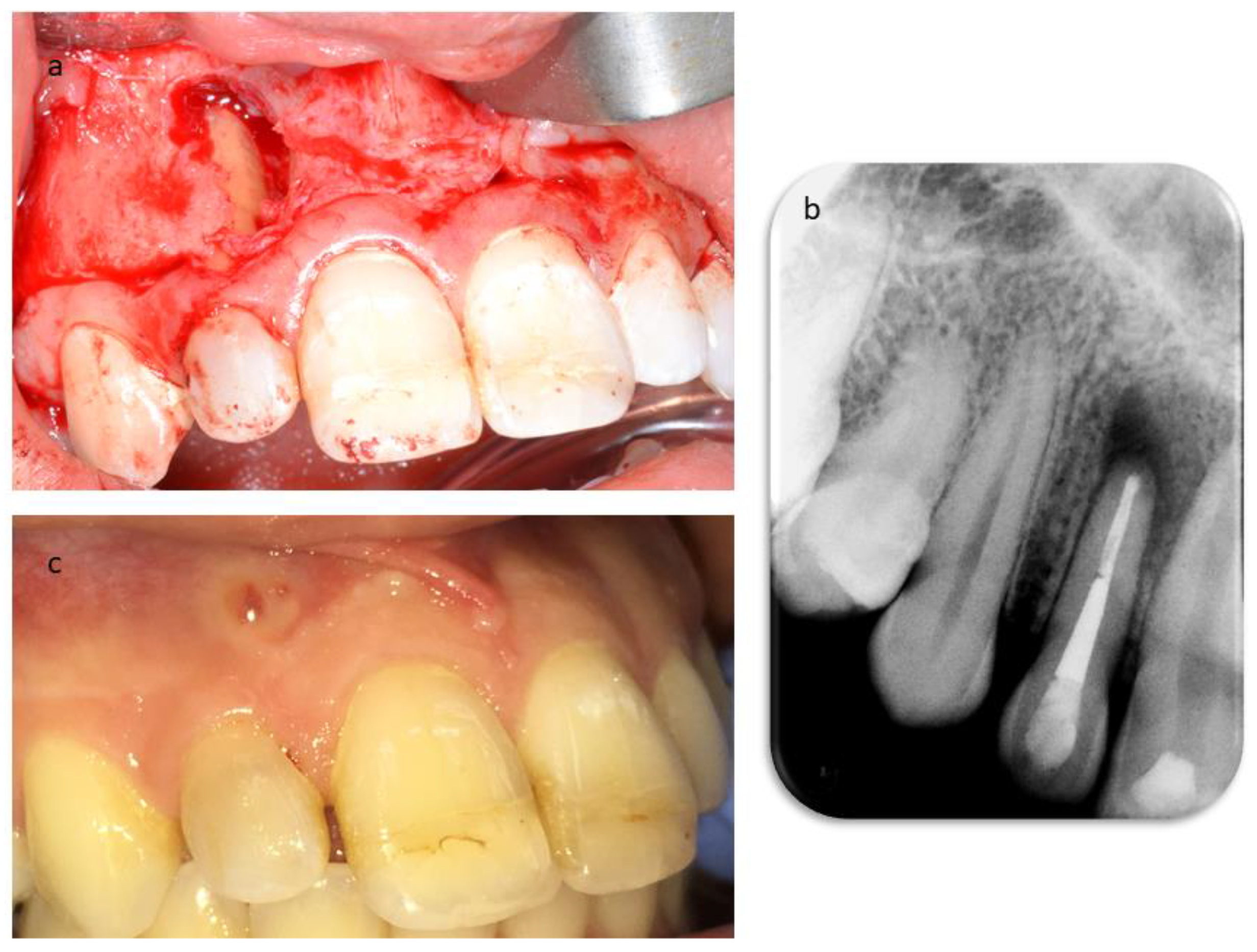
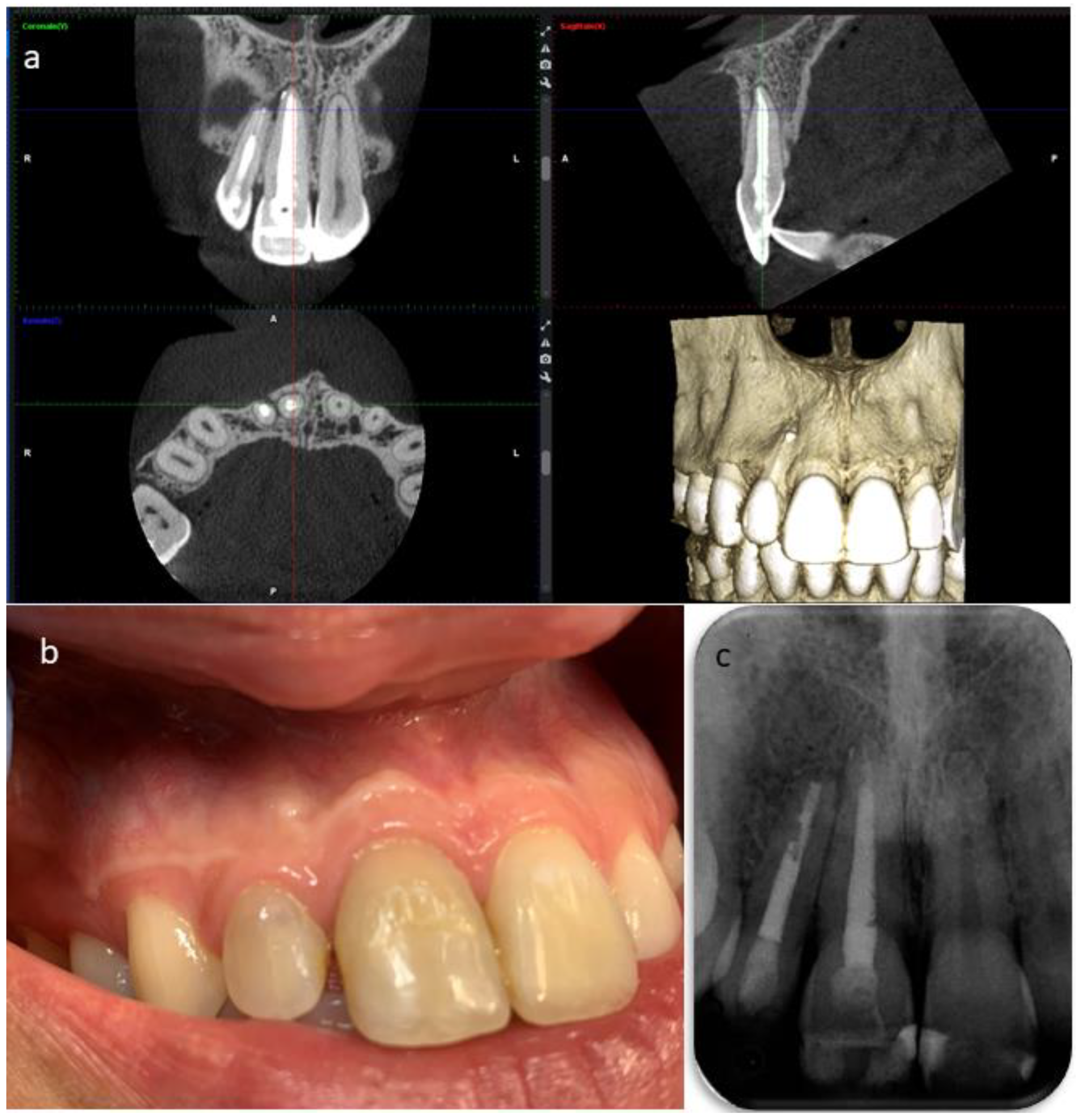
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spinas, E.; Mameli, A.; Giannetti, L. Traumatic dental injuries resulting from sports activities; immediate treatment and five years follow-up: An observational study. Open Dent. J. 2018, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Aresu, M.; Giannetti, L. Use of mouth guard in basketball: Observational study of a group of teenagers with and without motivational reinforcement. Eur. J. Paediatr. Dent. 2014, 15, 392–396. [Google Scholar] [PubMed]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar] [PubMed]
- Trope, M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent. Clin. N. Am. 2010, 54, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Peddis, N.; Musu, D.; Ideo, F.; Rossi-Fedele, G.; Cotti, E. Interaction of biologic therapy with apical periodontitis and periodontitis: A systematic review. Aust. Dent. J. 2019, 64, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Corbella, S.; Sequeira-Byron, P.; Tsesis, I.; Rosen, E.; Lolato, A.; Taschieri, S. Endodontic procedures for retreatment of periapical lesions. Cochrane Database Syst. Rev. 2016, 10, 1–66. [Google Scholar] [CrossRef]
- Musu, D.; Rossi-Fedele, G.; Campisi, G.; Cotti, E. Ultrasonography in the diagnosis of bone lesions of the jaws: A systematic review of the literature. Oral Med. Oral Surg. Oral Pathol. Oral Radiol. 2016, 122, e19–e29. [Google Scholar] [CrossRef]
- Cotti, E.; Campisi, G.; Garau, V.; Puddu, G. A new technique for the study of periapical bone lesions: Ultrasound real time imaging. Int. Endod. J. 2002, 35, 148–152. [Google Scholar] [CrossRef]
- Cotti, E.; Campisi, G.; Ambu, R.; Dettori, C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int. Endod. J. 2003, 36, 556–563. [Google Scholar] [CrossRef]
- Cotti, E.; Simbola, V.; Dettori, C.; Campisi, G. Echographic evaluation of bone lesions of endodontic origin: Report of two cases in the same patient. J. Endod. 2006, 32, 901–905. [Google Scholar] [CrossRef]
- Cotti, E.; Esposito, S.A.; Musu, D.; Campisi, G.; Shemesh, H. Ultrasound examination with color power Doppler to assess the early response of apical periodontitis to the endodontic treatment. Clin. Oral Investig. 2018, 22, 131–140. [Google Scholar] [CrossRef]
- Musu, D.; Shemesh, H.; Boccuzzi, M.; Dettori, C.; Cotti, E. The effectiveness of ultrasound examination to assess the healing process of bone lesions of the jaws: A systematic review. Clin. Oral Investig. 2020, 24, 3739–3747. [Google Scholar] [CrossRef]
- Andersson, L. IADT guidelines for treatment of traumatic dental injuries. Dent. Traumat. 2012, 28. [Google Scholar] [CrossRef]
- Gorni, F.G.; Gagliani, M.M. The outcome of endodontic retreatment: A 2-yr follow-up. J. Endod. 2004, 30, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Spinas, E.; Generali, L.; Mameli, A.; Demontis, C.; Martinelli, D.; Giannetti, L. Delayed tooth replantation and inflammatory root resorption in childhood and adolescence. J. Biol Regul. Homeost. Agents 2019, 33, 623–627. [Google Scholar]
- Jafarzadeh, H.; Abbott, P.V. Review of pulp sensibility tests. Part Ι: General information and thermal tests. Int. Endod. J. 2010, 43, 738–762. [Google Scholar] [CrossRef] [PubMed]
- Jafarzadeh, H.; Abbott, P.V. Review of pulp sensibility tests. Part II: Electric pulp tests and test cavities. Int. Endod. J. 2010, 43, 945–958. [Google Scholar] [CrossRef]
- Bastos, J.V.; Goulart, E.M.A.; de Souza Côrtes, M.I. Pulpal response to sensibility tests after traumatic dental injuries in permanent teeth. Dent. Traumatol. 2014, 30, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Aresu, M.; Canargiu, F. Prosthetic rehabilitation interventions in adolescents with fixed bridges: A 5-year observational study. Eur. J. Paediatr. Dent. 2013, 14, 59–62. [Google Scholar] [PubMed]
- Spinas, E. A biological conservative approach to complex traumatic dento-alveolar lesions. J. Clin. Pediatr. Dent. 2003, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 2: Tooth survival. Int. Endod. J. 2011, 44, 610–625. [Google Scholar] [CrossRef]
- Ricucci, D.; Loghin, S.; Gonçalves, L.S.; Rôças, I.N.; Siqueira, J.F., Jr. Histobacteriologic conditions of the apical root canal system and periapical tissues in teeth associated with sinus tracts. J. Endod. 2018, 44, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Cotti, E.; Musu, D.; Goddi, A.; Dettori, C.; Campisi, G.; Shemesh, H. Ultrasound examination to visualize and trace sinus tracts of endodontic origin. J. Endod. 2019, 45, 1184–1191. [Google Scholar] [CrossRef]
- Baumgartner, J.C.; Picket, A.B.; Muller, J.T. Microscopic examination of oral sinus tracts and their associated periapical lesions. J. Endod. 1984, 10, 146–152. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musu, D.; Bardini, G.; Ideo, F.; Mezzena, S.; Cotti, E. Management of the Sequelae of a Sport-Related Traumatic Dental Injury Using Ultrasound Examination in the Diagnosis and Follow-Up. Dent. J. 2021, 9, 27. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9030027
Musu D, Bardini G, Ideo F, Mezzena S, Cotti E. Management of the Sequelae of a Sport-Related Traumatic Dental Injury Using Ultrasound Examination in the Diagnosis and Follow-Up. Dentistry Journal. 2021; 9(3):27. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9030027
Chicago/Turabian StyleMusu, Davide, Giulia Bardini, Francesca Ideo, Silvia Mezzena, and Elisabetta Cotti. 2021. "Management of the Sequelae of a Sport-Related Traumatic Dental Injury Using Ultrasound Examination in the Diagnosis and Follow-Up" Dentistry Journal 9, no. 3: 27. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9030027





