Combined Management of Apical Root Fracture and Avulsion of Two Maxillary Permanent Central Incisors: A Case Report
Abstract
:1. Introduction
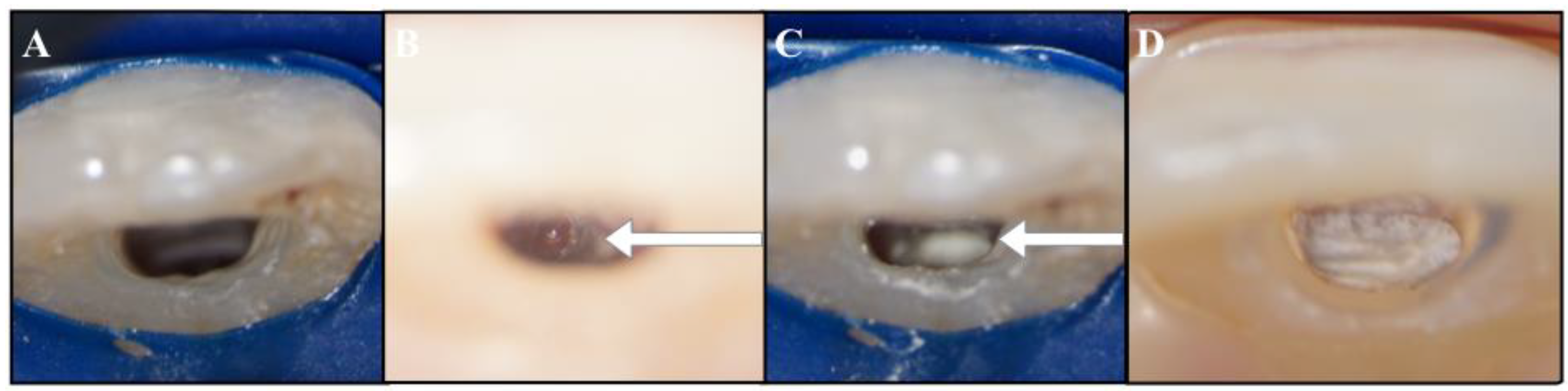
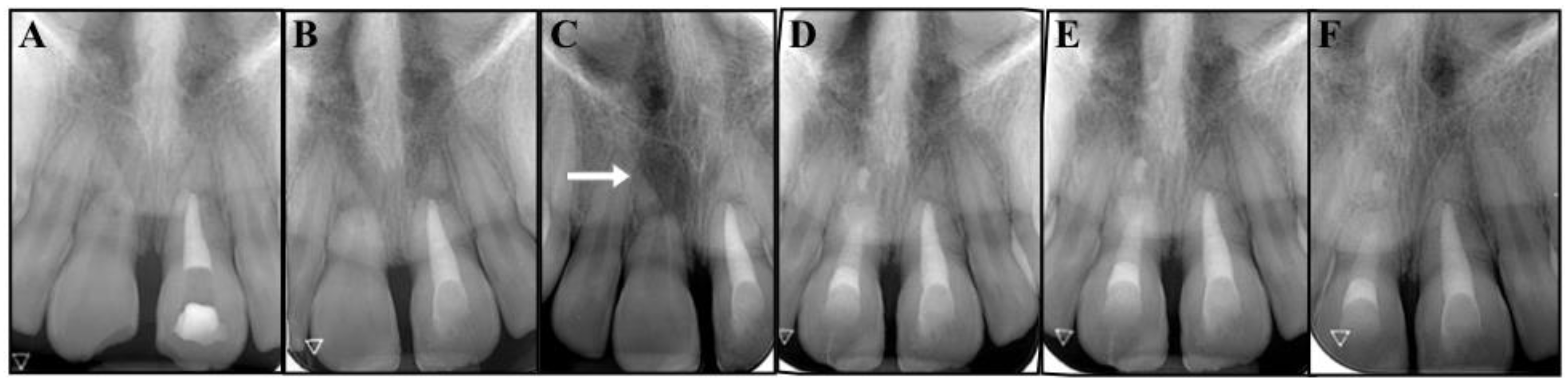
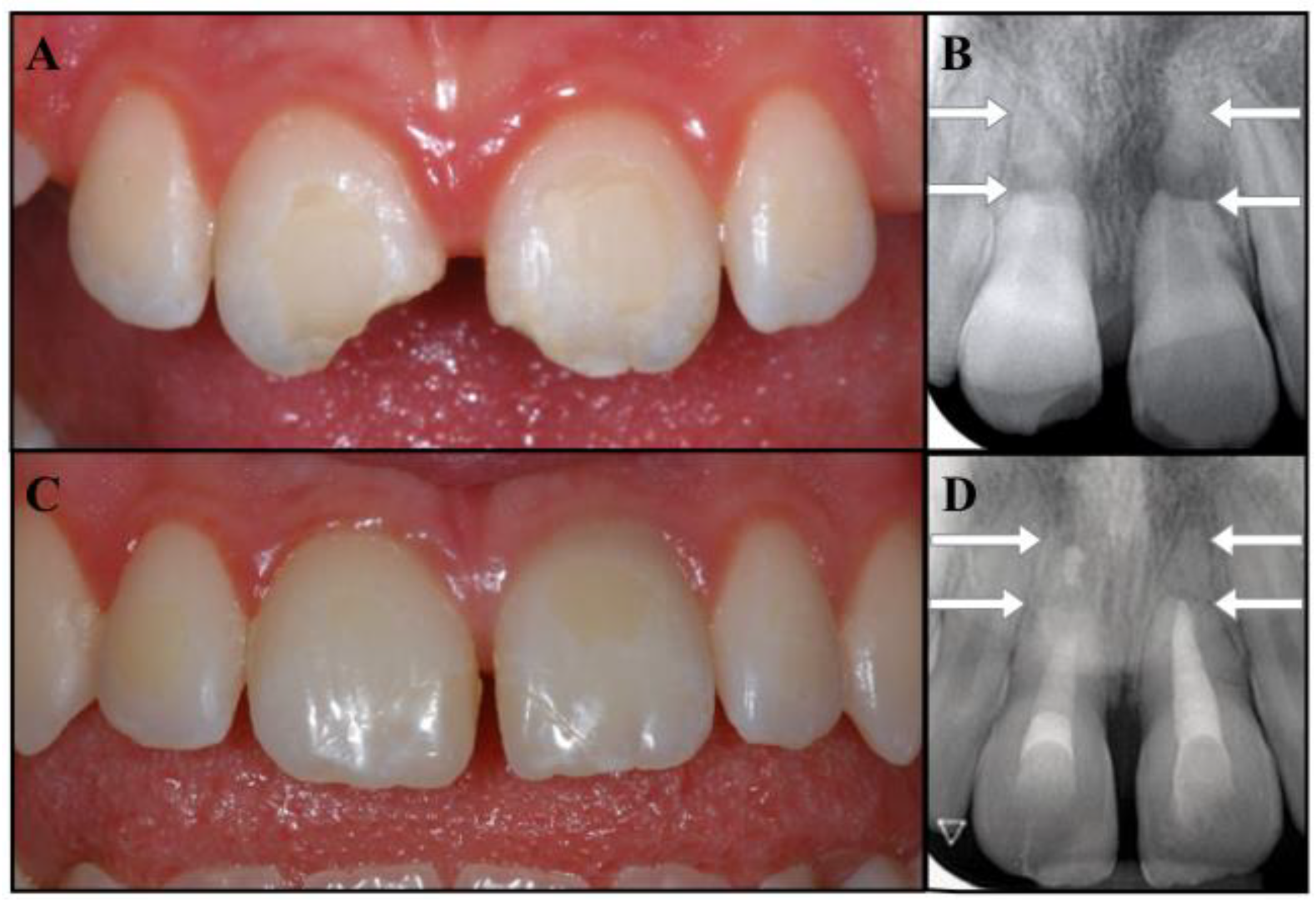
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; Di Angelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. Guidelines for the management of traumatic dental injuries: 2. avulsion of permanent teeth. Pediatr. Dent. 2017, 39, 412–419. [Google Scholar] [CrossRef]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 2. avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Gassner, R.; Bösch, R.; Tuli, T.; Emshoff, R. Prevalence of dental trauma in 6000 patients with facial injuries implications for prevention. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 87, 27–33. [Google Scholar] [CrossRef]
- Glendor, U.; Halling, A.; Andersson, L.; Eilert-Petersson, E. Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed. Dent. J. 1996, 20, 15–28. [Google Scholar]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Textbook and color atlas of traumatic injuries to the teeth. Stomatol. Edu. J. 2019, 6, 279. [Google Scholar] [CrossRef]
- Andersson, L.; Bodin, I. Avulsed human teeth replanted within 15 minutes—A long-term clinical follow-up study. Dent. Traumatol. 1990, 6, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.J.; Kenny, D.J. Avulsed permanent teeth: A review of the literature and treatment guidelines. Endod. Dent. Traumatol. 1997, 13, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.J.; Kenny, D.J. Survival of avulsed permanent maxillary incisors in children following delayed replantation. Dent. Traumatol. 1997, 13, 269–275. [Google Scholar] [CrossRef]
- Petrovic, B.; Marković, D.; Peric, T.; Blagojevic, D. Factors related to treatment and outcomes of avulsed teeth. Dent. Traumatol. 2010, 26, 52–59. [Google Scholar] [CrossRef]
- Pohl, Y.; Filippi, A.; Kirschner, H. Results after replantation of avulsed permanent teeth. I. endodontic considerations. Dent. Traumatol. 2005, 21, 80–92. [Google Scholar] [CrossRef]
- Spinas, E.; Generali, L.; Mameli, A.; Demontis, C.; Martinelli, D.; Giannetti, L. Delayed tooth replantation and inflammatory root resorption in childhood and adolescence. J. Biol. Regul. Homeost. Agents 2019, 33, 623–627. [Google Scholar]
- Çalişkan, M.K.; Pehlivan, Y. Prognosis of root-fractured permanent incisors. Endod. Dent. Traumatol. 1996, 12, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.F.; Hicks, L.; et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 1. fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Pipi, L.; Mezzena, S.; Giannetti, L. Use of orthodontic methods in the treatment of dental luxations: A scoping review. Dent. J. 2021, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Trope, M.; Langer, I.; Maltz, D.; Tronstad, L. Resistance to fracture of restored endodontically treated teeth. Dent. Traumatol. 1986, 2, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review-part I: Chemical, physical, and antibacterial properties. J. Endod. 2010, 36, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M. Mineral trioxide aggregate: A comprehensive literature review—Part II: Leakage and biocompatibility investigations. J. Endod. 2010, 36, 190–202. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–413. [Google Scholar] [CrossRef]
- Palma, P.J.; Marques, J.A.; Antunes, M.; Falacho, R.I.; Sequeira, D.; Roseiro, L.; Santos, J.M.; Ramos, J.C. Effect of restorative timing on shear bond strength of composite resin/calcium silicate–based cements adhesive interfaces. Clin. Oral Investig. 2020. [Google Scholar] [CrossRef]
- Hiremath, G.; Kidiyoor, K.H. Avulsion and storage media. J. Investig. Clin. Dent. 2011, 2, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Poi, W.R.; Sonoda, C.K.; Martins, C.M.; Melo, M.E.; Pellizzer, E.P.; De Mendonça, M.R.; Panzarini, S.R. Storage media for avulsed teeth: A literature review. Braz. Dent. J. 2013, 24, 437–445. [Google Scholar] [CrossRef]
- Andersson, L.; Malmgren, B. The problem of dentoalveolar ankylosis and subsequent replacement resorption in the growing patient. Aust. Endod. J. 1999, 25, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Mihaela, H.; Maria, M.; Benjamin, S.; Ruben, P.; Caroline, O.A.; Oana, A.; Raluca, R.; Mihaela, B.; Reinhilde, J. Irradiation provided by dental radiological procedures in a pediatric population. Eur. J. Radiol. 2018, 103, 112–117. [Google Scholar] [CrossRef]
- Oenning, A.C.; Jacobs, R.; Pauwels, R.; Stratis, A.; Hedesiu, M.; Salmon, B. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr. Radiol. 2018, 48, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Trope, M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent. Clin. N. Am. 2010, 54, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Corbella, S.; Ferrara, G.; El Kabbaney, A.; Taschieri, S. Apexification, apexogenesis and regenerative endodontic procedures: A review of the literature. Minerva Stomatol. 2014, 63, 375–389. [Google Scholar] [PubMed]
- Witherspoon, D.E.; Small, J.C.; Regan, J.D.; Nunn, M. Retrospective analysis of open apex teeth obturated with mineral trioxide aggregate. J. Endod. 2008, 34, 1171–1176. [Google Scholar] [CrossRef] [PubMed]
- Kerekes, K.; Heide, S.; Jacobsen, I. Follow-up examination of endodontic treatment in traumatized juvenile incisors. J. Endod. 1980, 6, 744–748. [Google Scholar] [CrossRef]
- Guerrero, F.; Mendoza, A.; Ribas, D.; Aspiazu, K. Apexification: A systematic review. J. Conserv. Dent. 2018, 21, 462. [Google Scholar] [CrossRef]
- Albadri, S.; Chau, Y.S.; Jarad, F. The use of mineral trioxide aggregate to achieve root end closure: Three case reports. Dent. Traumatol. 2013, 29, 469–473. [Google Scholar] [CrossRef]
- Lin, J.C.; Lu, J.X.; Zeng, Q.; Zhao, W.; Li, W.Q.; Ling, J.Q. Comparison of mineral trioxide aggregate and calcium hydroxide for apexification of immature permanent teeth: A systematic review and meta-analysis. J. Formos. Med. Assoc. 2016, 115, 523–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidal, K.; Martin, G.; Lozano, O.; Salas, M.; Trigueros, J.; Aguilar, G. Apical closure in apexification: A review and case report of apexification treatment of an immature permanent tooth with biodentine. J. Endod. 2016, 42, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Bardini, G.; Casula, L.; Ambu, E.; Musu, D.; Mercadè, M.; Cotti, E. A 12-month follow-up of primary and secondary root canal treatment in teeth obturated with a hydraulic sealer. Clin. Oral Investig. 2020. [Google Scholar] [CrossRef] [PubMed]
- Palma, P.J.; Marques, J.A.; Santos, J.; Falacho, R.I.; Sequeira, D.; Diogo, P.; Caramelo, F.; Ramos, J.C.; Santos, J.M. Tooth discoloration after regenerative endodontic procedures with calcium silicate-based cements-an ex vivo study. Appl. Sci. 2020, 10, 5793. [Google Scholar] [CrossRef]
- Możyńska, J.; Metlerski, M.; Lipski, M.; Nowicka, A. Tooth discoloration induced by different calcium silicate–based cements: A systematic review of In vitro studies. J. Endod. 2017, 43, 1593–1601. [Google Scholar] [CrossRef]
- Lenherr, P.; Allgayer, N.; Weiger, R.; Filippi, A.; Attin, T.; Krastl, G. Tooth discoloration induced by endodontic materials: A laboratory study. Int. Endod. J. 2012, 45, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Poi, W.R.; Manfrin, T.M.; Holland, R.; Sonoda, C.K. Repair characteristics of horizontal root fracture: A case report. Dent. Traumatol. 2002, 18, 98–102. [Google Scholar] [CrossRef]
- Kucukyilmaz, E.; Botsali, M.; Keser, G. Treatments of horizontal root fractures: Four case reports. J. Pediatr. Dent. 2013, 1, 19. [Google Scholar] [CrossRef] [Green Version]
- Malmgren, B.; Hübel, S. Transient discoloration of the coronal fragment in intra-alveolar root fractures. Dent. Traumatol. 2012, 28, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Pipi, L.; Dettori, C. Extrusive luxation injuries in young patients: A retrospective study with 5-year follow-up. Dent. J. 2020, 8, 136. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardini, G.; Musu, D.; Mezzena, S.; Dettori, C.; Cotti, E. Combined Management of Apical Root Fracture and Avulsion of Two Maxillary Permanent Central Incisors: A Case Report. Dent. J. 2021, 9, 39. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040039
Bardini G, Musu D, Mezzena S, Dettori C, Cotti E. Combined Management of Apical Root Fracture and Avulsion of Two Maxillary Permanent Central Incisors: A Case Report. Dentistry Journal. 2021; 9(4):39. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040039
Chicago/Turabian StyleBardini, Giulia, Davide Musu, Silvia Mezzena, Claudia Dettori, and Elisabetta Cotti. 2021. "Combined Management of Apical Root Fracture and Avulsion of Two Maxillary Permanent Central Incisors: A Case Report" Dentistry Journal 9, no. 4: 39. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040039





