Third Molar Extraction: Irrigation and Cooling with Water or Sterile Physiological Solution: A Double-Blind Randomized Study
Abstract
:1. Introduction
1.1. Impacted Third Molars: Definition, Epidemiology and Etiology
1.2. How Can We Reduce the Risk of Complications
1.3. Aim of the Study
2. Materials and Methods
2.1. Study Population
- need for extraction of partially or totally impacted lower third molar(s);
- tolerance of normal surgical procedures;
- good general health;
- informed consent to participation in the study.
- uncontrolled periodontal disease;
- uncontrolled diabetes;
- bone diseases (Paget’s disease, therapy with bisphosphonates, multiple myeloma, metastatic cancer to bone);
- a history of radiotherapy to the head and neck region;
- need for systemic corticosteroids or other therapies that might interfere with postoperative recovery;
- allergy to penicillin;
- inability to return to follow-up visits and complete the study protocol as established by the investigators;
- smoker patients were ineligible for this trial;
- pregnancy and or breastfeeding;
- acute inflammatory diseases.
2.2. Surgical Procedure
2.3. Postoperative Pain Rating
2.4. Postoperative Swelling
- the distance from the tragus to the pogonion (the most prominent point on the chin);
- the distance from the tragus to the lateral canthus of the homolateral eye;
- the distance from the tragus to the labial commissure on the homolateral side;
- the distance from the gonion (the meeting point of lines tangent to the posterior margin of the ramus and to the inferior margin of the mandible) to the homolateral nasal wing;
2.5. Postoperative Trismus
2.6. Severity of Systemic Inflammation
2.7. Statistical Analyses
3. Results
3.1. Postoperative Pain
3.2. Postoperative Swelling and Trismus
3.3. Severity of Systemic Inflammation
3.4. Local and Systemic Complications of the Procedure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chiapasco, M. Manuale Illustrato di Chirurgia Orale, 3rd ed.; Elsevier Masson: Milan, Italy, 2014. [Google Scholar]
- Blondeau, F.; Daniel, N.G. Extraction of impacted mandibular third molars: Operative complications and their risk factors. J. Can. Dent. Assoc. 2007, 73, 325. [Google Scholar]
- Graziani, F.; D’Aiuto, F.; Arduino, P.; Tonelli, M.; Gabriele, M. Perioperative dexamethasone reduces post-surgical sequelae of wisdom tooth removal. A split-mouth randomized double-masked clinical trial. Int. J. Oral Maxillofac. Surg. 2006, 35, 241–246. [Google Scholar] [CrossRef]
- Contar, C.; Oliveira, P.; Kanegusuku, K.; Berticelli, R.; Azevedo-Alanis, L.; Machado, M. Complications in third molar removal: A retrospective study of 588 patients. Med. Oral Patol. Oral Cir. Bucal 2009, 15, e74–e78. [Google Scholar] [CrossRef] [Green Version]
- Torres, M.A.F.; Albiol, J.G.; Aytés, L.B.; Escoda, C.G. Evaluation of the indication for surgical extraction of third molars according to the oral surgeon and the primary care dentist. Experience in the Master of Oral Surgery and Implantology at Barcelona University Dental School. Med. Oral Patol. Oral Cir. Bucal 2008, 13, 499–504. [Google Scholar]
- Al-Asfour, A. Postoperative Infection after Surgical Removal of Impacted Mandibular Third Molars: An Analysis of 110 Consecutive Procedures. Med. Princ. Pr. 2009, 18, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Satılmış, T.; Garip, H.; Arpacı, E.; Şener, C.; Göker, K. Assessment of combined local anestesia and ketamine for pain, swelling and trismus after surgical extraction of third molars. J. Oral Maxillofac. Surg. 2009, 67, 1206–1210. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, H.; Sugiura, M. Clinical postoperative findings after removal of impacted mandibular third molars: Prediction of postoperative facial swelling and pain based on preoperative variables. Br. J. Oral Maxillofac. Surg. 2004, 42, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Danda, A.K.; Tatiparthi, M.K.; Narayanan, V.; Siddareddi, A.; Danda, A.K.; Tatiparthi, M.K.; Narayanan, V.; Siddareddi, A. Influence of primary and secondary closure of surgical wound after impacted mandibular third molar removal on postoperative pain and swelling—A comparative and split mouth study. J. Oral Maxillofac. Surg. 2010, 68, 309–312. [Google Scholar] [CrossRef]
- Chiapasco, M.; De Cicco, L.; Marrone, G. Side effects and complications associated with third molar surgery. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 412–420. [Google Scholar] [CrossRef]
- Lysell, L.; Rohlin, M. A study of indications used for removal of the mandibular third molar. Int. J. Oral Maxillofac. Surg. 1988, 17, 161–164. [Google Scholar] [CrossRef]
- Goldberg, M.H.; Nemarich, A.N.; Marco, W.P., 2nd. Complications after mandibular third molar surgery: A statistical analysis of 500 consecutive procedures in private practice. J. Am. Dent. Assoc. 1985, 111, 277–279. [Google Scholar] [CrossRef] [PubMed]
- Lyons, C.J.; Bruce, R.A.; Frederickson, G.C.; Small, G.S. Age of Patients and Morbidity Associated with Mandibular Third Molar Surgery. J. Am. Dent. Assoc. 1980, 101, 240–245. [Google Scholar] [CrossRef]
- Osborn, T.P.; Frederickson, G.; Small, I.A.; Torgerson, T.S. A prospective study of complications related to mandibular third molar surgery. J. Oral Maxillofac. Surg. 1985, 43, 767. [Google Scholar] [CrossRef]
- Stanley, H.R.; Alattar, M.; Collett, W.K.; Stringfellow, H.R., Jr.; Spiegel, E.H. Pathological sequelaeof neglected impacted third molar. J. Oral Pathol. 1988, 17, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Nordenram, A.; Hultin, M.; Kjellman, O.; Ramstrom, G. Indications for surgical removal of third molars: Study of 2630 cases. Swed. Dent. J. 1987, 11, 23–29. [Google Scholar] [PubMed]
- Alling, C.C.; Catone, G.A. Management of impacted teeth. J. Oral Maxillofac. Surg. 1993, 51 (Suppl. 1), 3–6. [Google Scholar] [CrossRef]
- Lytle, J.J. Etiology and Indications for the Management of Impacted Teeth. Oral Maxillofac. Surg. Clin. N. Am. 1993, 5, 63–75. [Google Scholar] [CrossRef]
- Shepherd, J.P.; Brickley, M. Surgical removal of third molars. BMJ 1994, 309, 620–621. [Google Scholar] [CrossRef] [Green Version]
- Precious, D.S.; Mercier, P.; Payette, F. Risks and benefits of removal of impacted third molars: Critical review of the literature. J. Can. Dent. Assoc. 1992, 58, 17–27. [Google Scholar]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of Third Molar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Lucchiari, N.; Frigo, A.C.; Stellini, E.; Coppe, M.; Berengo, M.; Bacci, C. Complications after mandibular third molar extraction. Quintessence Int. 1995, 26, 779. [Google Scholar]
- Lucchiari, N.; Frigo, A.C.; Stellini, E.; Coppe, M.; Berengo, M.; Bacci, C. In Vitro Assessment with the Infrared Thermometer of Temperature Differences Generated during Implant Site Preparation: The Traditional Technique Versus the Single-Drill Technique. Clin. Implant. Dent. Relat. Res. 2014, 18, 182–191. [Google Scholar] [CrossRef]
- Peterson, I. Principles of Oral and Maxillofacial Surgery, 2nd ed.; BC Decker Inc.: London, UK, 2004. [Google Scholar]
- Kirk, D.G.; Liston, P.N.; Tong, D.C.; Love, R.M. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Al-Khateeb, T.; Nusair, Y. Effect of the proteolytic enzyme serrapeptase on swelling, pain and trismus after surgical extraction of mandibular third molars. Int. J. Oral Maxillofac. Surg. 2008, 37, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Sisk, A.L.; Hammer, W.B.; Shelton, D.W.; Joy, E.D. Complications following removal of impacted third molars: The role of the experience of the surgeon. J. Oral Maxillofac. Surg. 1986, 44, 855–859. [Google Scholar] [CrossRef]
- Voegelin, T.C.; Suter, V.G.A.; Bornstein, M.M. Complications during and after surgical removal of mandibular third molars. Impact of patient related and anatomical factors. Schweiz. Mon. Zahnmed. 2008, 118, 192–198. [Google Scholar]
- Chuang, S.-K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Risk Factors for Inflammatory Complications Following Third Molar Surgery in Adults. J. Oral Maxillofac. Surg. 2008, 66, 2213–2218. [Google Scholar] [CrossRef]
- Baqain, Z.H.; Abu Karaky, A.; Sawair, F.; Khaisat, A.; Duaibis, R.; Rajab, L.D. Frequency Estimates and Risk Factors for Postoperative Morbidity After Third Molar Removal: A Prospective Cohort Study. J. Oral Maxillofac. Surg. 2008, 66, 2276–2283. [Google Scholar] [CrossRef]
- Larsen, P. Alveolar osteitis after surgical removal of impacted mandibular third molars: Identification of the patient at risk. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 393. [Google Scholar] [CrossRef]
- Sweet, J.B.; Butler, D.P. The relationship of smoking to localized osteitis. J. Oral Surg. 1979, 37, 732–735. [Google Scholar]
- Heng, C.K.; Badner, V.M.; Clemens, D.L.; Mercer, L.T.; Mercer, D.W. The relationship of cigarette smoking to postoperative complications from dental extractions among female inmates. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Benediktsdóttir, I.S.; Wenzel, A.; Petersen, J.K.; Hintze, H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 97, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Queral-Godoy, E.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 99, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Chaparro-Avendaño, A.V.; Pérez-García, S.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Morbidity of third molar extraction in patients between 12 and 18 years of age. Med. Oral Patol. Oral Cir. Bucal 2005, 10, 422–431. [Google Scholar]
- Manani, G.; Bacci, C.; Zanette, G.; Facco, E. Contemporary state of sedation in dentistry. Dent. Cadoms 2012, 80, 351–426. [Google Scholar]
- Ohnhaus, E.E.; Adler, R. Methodological problems in the measurement of pain: A comparison between the verbal rating scale and the visual analogue scale. Pain 1975, 1, 379–384. [Google Scholar] [CrossRef]
- Quiding, H.; Oksala, E.; Happonen, R.P.; Lehtimäki, K.; Ojala, T. The visual analogue scale in multiple-dose evaluations of analgesics. J. Clin. Pharmacol. 1981, 21, 424–429. [Google Scholar] [CrossRef]
- Scott, J.; Huskisson, E.C. Graphic representation of pain. Pain 1976, 2, 175–184. [Google Scholar] [CrossRef]
- Sisk, A.L.; Bonnington, G.J. Evaluation of methylprednisolone and flurbiprofen for inhibition of the postoperative inflammatory response. Oral Surg. Oral Med. Oral Pathol. 1985, 60, 137–145. [Google Scholar] [CrossRef]
- Berain, R.; Hollander, O. The effect of metylprednisolone on pain, trismus and swelling after removal of third molars. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 134–138. [Google Scholar]
- Messer, E.J.; Keller, J.J. The use of intraoral dexamethasone after extraction of mandibular third molars. Oral Surg. Oral Med. Oral Pathol. 1975, 40, 594–598. [Google Scholar] [CrossRef]
- Pedersen, A.; Mærsk-Møller, O. Volumetric determination of extraoral swelling from stereophotographs. A method study in the buccal area. Int. J. Oral Surg. 1985, 14, 229–234. [Google Scholar] [CrossRef]
- Skjelbred, P.; Løkken, P. Post-operative pain and inflammatory reaction reduced by injection of a corticosteroid. A controlled trial in bilateral oral surgery. Eur. J. Clin. Pharmacol. 1982, 21, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Üstün, Y.; Erdoǧan, Ö.; Esen, E.; Karsli, E.D. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2003, 96, 535–539. [Google Scholar] [CrossRef]
- Van Gool, A.V.; Ten Bosch, J.J.; Boering, G. A photographic method of assessing swelling following third molar removal. Int. J. Oral Surg. 1975, 4, 121–129. [Google Scholar] [CrossRef]
- Stahl, W.M. Acute phase protein response to tissue injury. Crit. Care Med. 1987, 15, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Smith, M.R.; Evans, R.T.; Bellamy, M.C.; Guillou, P.J. Serum PCR and IL-6 levels after trauma. Not predictive of septic complications in 31 patients. Acta Orthop. Scand. 1998, 69, 184–188. [Google Scholar] [CrossRef] [Green Version]
- Canellas, J.V.D.S.; Fraga, S.R.G.; Santoro, M.F.; Netto, J.N.S.; Tinoco, E.M.B. Intrasocket interventions to prevent alveolar osteitis after mandibular third molar surgery: A systematic review and network meta-analysis. J. Cranio Maxillofac. Surg. 2020, 48, 902–913. [Google Scholar] [CrossRef]
- Gazal, G. Management of an emergency tooth extraction in diabetic patients on the dental chair. Saudi Dent. J. 2020, 32, 1–6. [Google Scholar] [CrossRef]
- Bacci, C.; Cassetta, G.; Emanuele, B.; Berengo, M. Randomized Split-Mouth Study on Postoperative Effects of Palmitoylethanolamide for Impacted Lower Third Molar Surgery. ISRN Surg. 2011, 2011, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
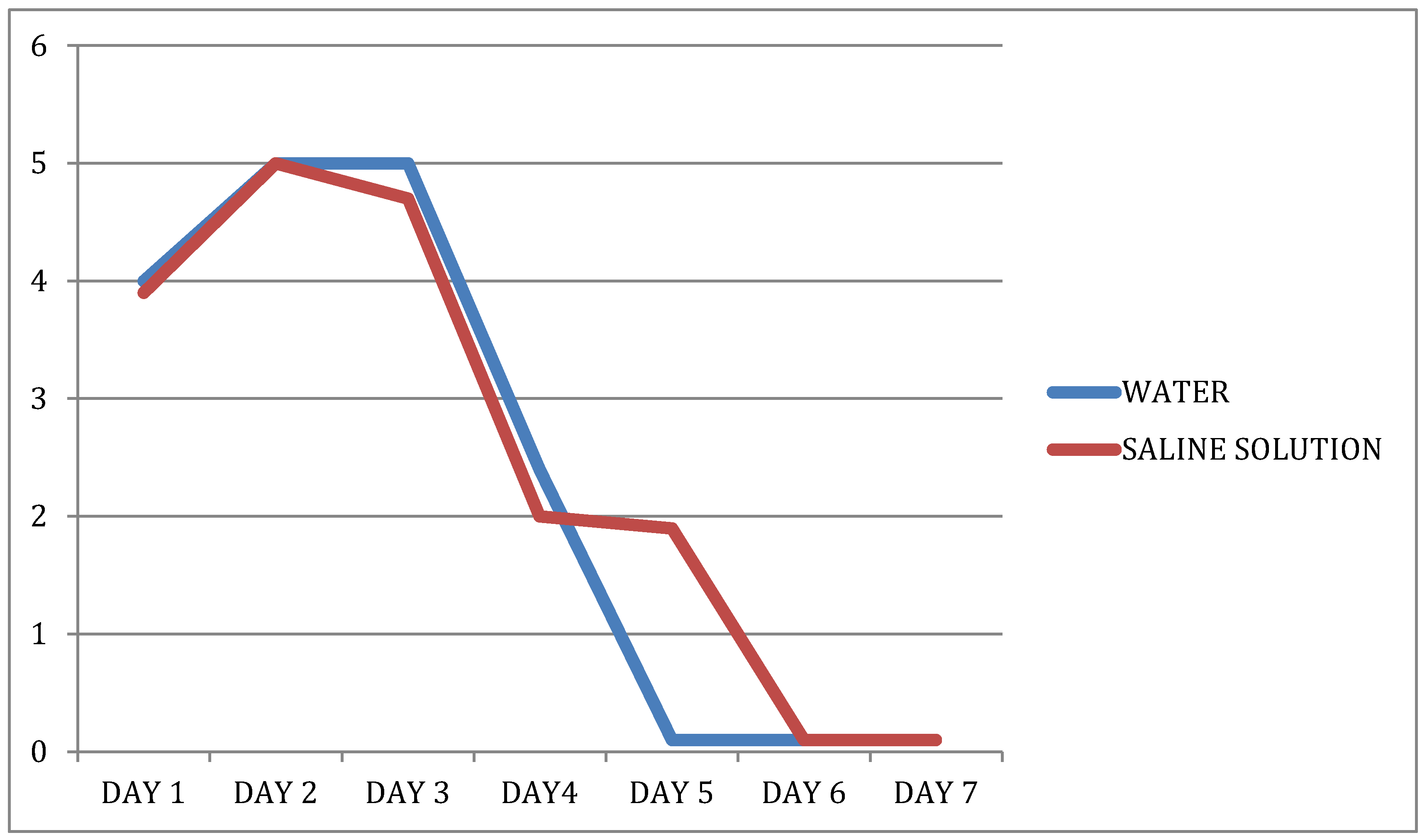
| DAY | Water | Saline Solution | p Value Group | p Value Time | p Value Group × Time |
|---|---|---|---|---|---|
| 1 | 4.00 (0.00–9.40) | 3.85 (0.00–8.00) | 0.5214 | <0.0001 | 0.8355 |
| 2 | 5.00 (0.00–9.40) | 5.00 (0.00–9.00) | |||
| 3 | 4.85 (0.00–8.00) | 4.50 (0.00–8.50) | |||
| 4 | 3.00 (0.00–7.00) | 2.15 (0.00–7.30) | |||
| 5 | 0.00 (0.00–5.00) | 2.00 (0.00–7.00) | |||
| 6 | 0.00 (0.00–9.00) | 0.00 (0.00–9.00) | |||
| 7 | 0.00 (0.00–7.00) | 0.00 (0.00–8.00) |
| Water | Saline Solution | p Value (Wilcoxon’s Test) | |||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | Difference | T1 | T2 | Difference | ||
| Tragus to Pogonion | 14.60 (12.40–17.00) | 15.35 (12.60–17.30) | −0.55 (−1.10–0.10) | 14.05 (12.30–16.40) | 14.75 (13.00–16.50) | −0.60 (−2.00–0.10) | 0.5968 |
| Tragus to lateral canthus | 7.80 (7.00–8.60) | 8.20 (7.0–9.30) | −0.50 (−0.90–0.00) | 7.50 (6.80–8.50) | 8.00 (7.00–9.00) | −0.40 (−1.10–0.00) | 0.9133 |
| Tragus to labial commissure | 11.40 (9.80–12.60) | 11.90 (10.40–13.80) | −0.40 (−1.80–0.00) | 11.00 (9.80–12.00) | 11.45 (10.30–12.40) | −0.40 (−0.70–0.00) | 0.6224 |
| Gonion to nasal wing | 9.70 (7.20–11.00) | 10.30 (8.70–11.50) | −0.40 (−2.00–0.20) | 9.50 (7.60–10.50) | 10.00 (8.50–11.40) | −0.35 (−1.90–0.00) | 1.0000 |
| Mouth opening | 5.00 (4.00–6.50) | 3.50 (2.00–6.00) | 1.30 (0.40–3.50) | 5.00 (4.00–6.00) | 3.10 (2.00–4.20) | 1.50 (0.30–3.40) | 0.4640 |
| 20 patients | <2.9 mg/L (baseline) | <2.9 mg/L (postoperatively) |
| 1 patient | <2.9 mg/L (baseline) | 3.5 mg/L (postoperatively) |
| 1 patient | <2.9 mg/L (baseline) | 9.5 mg/L (postoperatively) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sbricoli, L.; Cerrato, A.; Frigo, A.C.; Zanette, G.; Bacci, C. Third Molar Extraction: Irrigation and Cooling with Water or Sterile Physiological Solution: A Double-Blind Randomized Study. Dent. J. 2021, 9, 40. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040040
Sbricoli L, Cerrato A, Frigo AC, Zanette G, Bacci C. Third Molar Extraction: Irrigation and Cooling with Water or Sterile Physiological Solution: A Double-Blind Randomized Study. Dentistry Journal. 2021; 9(4):40. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040040
Chicago/Turabian StyleSbricoli, Luca, Alessia Cerrato, Anna Chiara Frigo, Gastone Zanette, and Christian Bacci. 2021. "Third Molar Extraction: Irrigation and Cooling with Water or Sterile Physiological Solution: A Double-Blind Randomized Study" Dentistry Journal 9, no. 4: 40. https://0-doi-org.brum.beds.ac.uk/10.3390/dj9040040






