The Phytochemistry of Cherokee Aromatic Medicinal Plants
Abstract
:1. Introduction
2. Cherokee Aromatic Medicinal Plants and Their Phytochemical Constituents
3. Cherokee Aromatic Medicinal Plants Currently in Use as Herbal Medicines
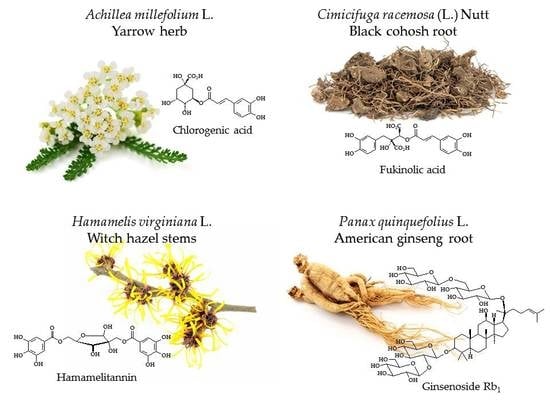
3.1. Achillea millefolium L.
3.2. Caulophyllum thalictroides (L.) Michx.
3.3. Cimicifuga racemosa (L.) Nutt. (syn. Actaea racemosa L.)
3.4. Hamamelis virginiana L.
3.5. Hydrastis canadensis L.
3.6. Juncus effusus L.
3.7. Panax quinquefolius L.
3.8. Sanguinaria canadensis L.
3.9. Scutellaria lateriflora L.
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Yuan, H.; Ma, Q.; Ye, L.; Piao, G. The traditional medicine and modern medicine from natural products. Molecules 2016, 21, 559. [Google Scholar] [CrossRef] [PubMed]
- Qin, G.; Xu, R. Recent advances on bioactive natural products from Chinese medicinal plants. Med. Res. Rev. 1998, 18, 375–382. [Google Scholar] [CrossRef]
- Patwardhan, B.; Vaidya, A.D.B.; Chorghade, M. Ayurveda and natural products drug discovery. Curr. Sci. 2004, 86, 789–799. [Google Scholar]
- Duke, J.A.; Bogenschutz-Godwin, M.J.; Ottesen, A.R. Duke’s Handbook of Medicinal Plants of Latin America; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar]
- Atanasov, A.G.; Waltenberger, B.; Pferschy-Wenzig, E.M.; Linder, T.; Wawrosch, C.; Uhrin, P.; Temml, V.; Wang, L.; Schwaiger, S.; Heiss, E.H.; et al. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015, 33, 1582–1614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeCorte, B.L. Underexplored opportunities for natural products in drug discovery. J. Med. Chem. 2016, 59, 9295–9304. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, L.C.S.; Feitosa, L.M.; da Silveira, F.F.; Boechat, N. Current antimalarial therapies and advances in the development of semi-synthetic artemisinin derivatives. An. Acad. Bras. Cienc. 2018, 90, 1251–1271. [Google Scholar] [CrossRef] [PubMed]
- Bunkar, A.R. Therapeutic uses of Rauwolfia serpentina. Int. J. Adv. Sci. Res. 2017, 2, 23–26. [Google Scholar]
- Monzote Fidalgo, L. Essential oil from Chenopodium ambrosioides as a promising antileishmanial agent. Nat. Prod. Commun. 2007, 2, 1257–1262. [Google Scholar]
- Cave, A.A. The Pequot War; University of Massachusetts Press: Amherst, MA, USA, 1996. [Google Scholar]
- Roundtree, H.C. Pocahantas’s People: The Powhatan Indians of Virginia through Four Centuries; University of Oklahoma Press: Norman, OK, USA, 1990. [Google Scholar]
- Ehle, J. Trail of Tears: The Rise and Fall of the Cherokee Nation; Anchor Books: New York, NY, USA, 1988. [Google Scholar]
- Brown, D. Bury My Heart at Wounded Knee: An Indian History of the American West; Picador: New York, NY, USA, 2007. [Google Scholar]
- Moerman, D.E. Native American Ethnobotany; Timber Press, Inc.: Portland, OR, USA, 1998. [Google Scholar]
- Hutchens, A.R. Indian Herbalogy of North America; Shambala Publications: Boulder, CO, USA, 1991. [Google Scholar]
- Hamel, P.B.; Chiltoskey, M.U. Cherokee Plants and Their Uses—A 400 Year History; Herald Publishing Company: Sylva, NC, USA, 1975. [Google Scholar]
- Garrett, J.T. The Cherokee Herbal; Bear & Company: Rochester, VT, USA, 2003. [Google Scholar]
- Mooney, J. The sacred formulas of the Cherokees. In Seventh Annual Report of the Bureau of Ethnology; Powell, J.W., Ed.; Government Printing Office: Washington, DC, USA, 1891; pp. 301–397. [Google Scholar]
- Banks, W.H. Ethnobotany of the Cherokee Indians. Ph.D. Thesis, University of Tennessee, Knoxville, TN, USA, 1953. [Google Scholar]
- Cozzo, D.N. Ethnobotanical Classifiction System and Medical Ethnobotany of the Eastern Band of the Cherokee Indians. Ph.D. Thesis, University of Georgia, Athens, GA, USA, 2004. [Google Scholar]
- Winston, D. Nvwoti; Cherokee medicine and ethnobotany. J. Am. Herb. Guild 2001, 2, 45–49. [Google Scholar]
- Core, E.L. Ethnobotany of the southern Appalachian Aborigines. Econ. Bot. 1967, 21, 199–214. [Google Scholar] [CrossRef]
- Ray, L.E. Podophyllum peltatum and observations on the Creek and Cherokee Indians: William Bartram’s preservation of Native American pharmacology. Yale J. Biol. Med. 2009, 82, 25–36. [Google Scholar] [PubMed]
- Vanhaelen, M.; Lejoly, J.; Hanocq, M.; Molle, L. Climatic and geographical aspects of medicinal plant constituents. In The Medicinal Plant Industry; Wijesekera, R.O.B., Ed.; CRC Press: Boca Raton, FL, USA, 1991; pp. 59–76. [Google Scholar]
- Royce, C.C. Map of the Former Territorial Limits of the Cherokee Nation of “Indians”; Map Showing the Territory Originally Assigned Cherokee “Nation of” Indians. Available online: https://www.loc.gov/item/99446145/ (accessed on 24 October 2018).
- Abou-Zaid, M.M.; Nozzolillo, C. 1-O-galloyl-α-l-rhamnose from Acer rubrum. Phytochemistry 1999, 52, 1629–1631. [Google Scholar] [CrossRef]
- Abou-Zaid, M.M.; Helson, B.V.; Nozzolillo, C.; Arnason, J.T. Ethyl m-digallate from red maple, Acer rubrum L., as the major resistance factor to forest tent caterpillar, Malacosoma disstria Hbn. J. Chem. Ecol. 2001, 27, 2517–2527. [Google Scholar] [CrossRef] [PubMed]
- Ma, H. Phytochemical and Biological Investigation of Gallotannins from Red Maple (Acer rubrum) Species. Ph.D. Thesis, University of Rhode Island, Kingston, RI, USA, 2014. [Google Scholar]
- Wan, C.; Yuan, T.; Xie, M.; Seeram, N.P. Acer rubrum phenolics include A-type procyanidins and a chalcone. Biochem. Syst. Ecol. 2012, 44, 1–3. [Google Scholar] [CrossRef]
- Wan, C.; Yuan, T.; Li, L.; Kandhi, V.; Cech, N.B.; Xie, M.; Seeram, N.P. Maplexins, new α-glucosidase inhibitors from red maple (Acer rubrum) stems. Bioorg. Med. Chem. Lett. 2012, 22, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Yuan, T.; Wan, C.; Liu, K.; Seeram, N.P. New maplexins F-I and phenolic glycosides from red maple (Acer rubrum) bark. Tetrahedron 2012, 68, 959–964. [Google Scholar] [CrossRef]
- González-Sarrías, A.; Yuan, T.; Seeram, N.P. Cytotoxicity and structure activity relationship studies of maplexins A–I, gallotannins from red maple (Acer rubrum). Food Chem. Toxicol. 2012, 50, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, H.; Yuan, T.; Seeram, N.P. Red maple (Acer rubrum) aerial parts as a source of bioactive phenolics. Nat. Prod. Commun. 2015, 10, 1409–1412. [Google Scholar] [PubMed]
- Bailey, A.E.; Asplund, R.O.; Ali, M.S. Isolation of methyl gallate as the antitumor principle of Acer saccharinum. J. Nat. Prod. 1986, 49, 1149–1150. [Google Scholar] [CrossRef] [PubMed]
- Bin Muhsinah, A.; Ma, H.; DaSilva, N.A.; Yuan, T.; Seeram, N.P. Bioactive glucitol-core containing gallotannins and other phytochemicals from silver maple (Acer saccharinum) leaves. Nat. Prod. Commun. 2017, 12, 83–84. [Google Scholar]
- Falk, A.J.; Smolenski, S.J.; Bauer, L.; Bell, C.L. Isolation and identification of three new flavones from Achillea millefolium L. J. Pharm. Sci. 1975, 64, 1838–1842. [Google Scholar] [CrossRef] [PubMed]
- Benetis, R.; Radušienė, J.; Janulis, V. Variability of phenolic compounds in flowers of Achillea millefolium wild populations in Lithuania. Medicina 2008, 44, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Glasl, S.; Mucaji, P.; Werner, I.; Presser, A.; Jurenitsch, J. Sesquiterpenes and flavonoid aglycones from a Hungarian taxon of the Achillea millefolium group. Z. Naturforsch. 2002, 57, 976–982. [Google Scholar] [CrossRef]
- Vitalini, S.; Beretta, G.; Iriti, M.; Orsenigo, S.; Basilico, N.; Dall’Acqua, S.; Iorizzi, M.; Fico, G. Phenolic compounds from Achillea millefolium L. and their bioactivity. Acta Biochim. Pol. 2011, 58, 203–209. [Google Scholar] [PubMed]
- Dias, M.I.; Barros, L.; Dueñas, M.; Pereira, E.; Carvalho, A.M.; Alves, R.C.; Oliveira, M.B.P.P.; Santos-Buelga, C.; Ferreira, I.C.F.R. Chemical composition of wild and commercial Achillea millefolium L. and bioactivity of the methanolic extract, infusion and decoction. Food Chem. 2013, 141, 4152–4160. [Google Scholar] [CrossRef] [PubMed]
- Dall’Acqua, S.; Bolego, C.; Cignarella, A.; Gaion, R.M.; Innocenti, G. Vasoprotective activity of standardized Achillea millefolium extract. Phytomedicine 2011, 18, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Tozyo, T.; Yoshimura, Y.; Sakurai, K.; Uchida, N.; Takeda, Y.; Nakai, H.; Ishi, H. Novel antitumor sesquiterpenoids in Achillea millefolium. Chem. Pharm. Bull. 1994, 42, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, G.; Vegeto, E.; Dall’Acqua, S.; Ciana, P.; Giorgetti, M.; Agradi, E.; Sozzi, A.; Fico, G.; Tomè, F. In vitro estrogenic activity of Achillea millefolium L. Phytomedicine 2007, 14, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Pires, J.M.; Mendes, F.R.; Negri, G.; Duarte-Almeida, J.M.; Carlini, E.A. Antinociceptive peripheral effect of Achillea millefolium L. and Artemisia vulgaris L.: Both plants known popularly by brand names of analgesic drugs. Phyther. Res. 2009, 23, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Guédon, D.; Abbe, P.; Lamaison, J.L. Leaf and flower head flavonoids of Achillea millefolium L. subspecies. Biochem. Syst. Ecol. 1993, 21, 607–611. [Google Scholar] [CrossRef]
- Csupor-Löffler, B.; Hajdú, Z.; Zupkó, I.; Réthy, B.; Falkay, G.; Forgo, P.; Hohmann, J. Antiproliferative effect of flavonoids and sesquiterpenoids from Achillea millefolium s.l. on cultured human tumour cell lines. Phyther. Res. 2009, 23, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Candan, F.; Unlu, M.; Tepe, B.; Daferera, D.; Polissiou, M.; Sökmen, A.; Akpulat, H.A. Antioxidant and antimicrobial activity of the essential oil and methanol extracts of Achillea millefolium subsp. millefolium Afan. (Asteraceae). J. Ethnopharmacol. 2003, 87, 215–220. [Google Scholar] [CrossRef]
- Santoro, G.F.; Cardoso, M.G.; Gustavo, L.; Guimarães, L.G.L.; Mendonça, L.Z.; Soares, M.J. Trypanosoma cruzi: Activity of essential oils from Achillea millefolium L., Syzygium aromaticum L. and Ocimum basilicum L. on epimastigotes and trypomastigotes. Exp. Parasitol. 2007, 116, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Bimbiraitė, K.; Ragižinskienė, O.; Maruška, A.; Kornyšova, O. Comparison of the chemical composition of four yarrow (Achillea millefolium L.) morphotypes. Biologija 2008, 54, 208–212. [Google Scholar] [CrossRef]
- Bocevska, M.; Sovová, H. Supercritical CO2 extraction of essential oil from yarrow. J. Supercrit. Fluids 2007, 40, 360–367. [Google Scholar] [CrossRef]
- Barghamadi, A.; Mehrdad, M.; Sefidkon, F.; Yamini, Y.; Khajeh, M. Comparison of the volatiles of Achillea millefolium L. obtained by supercritical carbon dioxide extraction and hydrodistillation Methods. J. Essent. Oil Res. 2009, 21, 259–264. [Google Scholar] [CrossRef]
- Figueiredo, A.C.; Barroso, J.G.; Pais, M.S.S.; Scheffer, J.J.C. Composition of the essential oils from leaves and flowers of Achillea millefolium L. ssp. millefolium. Flavour Fragr. J. 1992, 7, 219–222. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, S.; Zhang, S.; Gorenstein, D. Triterpenoid saponins from the fruits of Aesculus pavia. Phytochemistry 2006, 67, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, S. Cytotoxic triterpenoid saponins from the fruits of Aesculus pavia L. Phytochemistry 2007, 68, 2075–2086. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zhang, M.; Wu, Y.; Wan, A.; Zhang, R. Bioactive saponins from the fruits of Aesculus pavia L. Fitoterapia 2011, 82, 1106–1109. [Google Scholar] [CrossRef] [PubMed]
- Curir, P.; Galeotti, F.; Dolci, M.; Barile, E.; Lanzotti, V. Pavietin, a coumarin from Aesculus pavia with antifungal activity. J. Nat. Prod. 2007, 70, 1668–1671. [Google Scholar] [CrossRef] [PubMed]
- Ferracini, C.; Curir, P.; Dolci, M.; Lanzotti, V.; Alma, A. Aesculus pavia foliar saponins: Defensive role against the leafminer Cameraria ohridella. Pest Manag. Sci. 2010, 66, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Lanzotti, V.; Termolino, P.; Dolci, M.; Curir, P. Paviosides A–H, eight new oleane type saponins from Aesculus pavia with cytotoxic activity. Bioorg. Med. Chem. 2012, 20, 3280–3286. [Google Scholar] [CrossRef] [PubMed]
- Beier, R.C.; Norman, J.O.; Reagor, J.C.; Rees, M.S.; Mundy, B.P. Isolation of the major component in white snakeroot that is toxic after microsomal activation: Possible explanation of sporadic toxicity of white snakeroot plants and extracts. Nat. Toxins 1993, 1, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.T.; Davis, T.Z.; Gerdner, D.R.; Stegelmeier, B.L.; Evans, T.J. Quantitative method for the measurement of three benzofuran ketones in rayless goldenrod (Isocoma pluriflora) and white snakeroot (Ageratina altissima) by high-performance liquid chromatography (HPLC). J. Agric. Food Chem. 2009, 57, 5639–5643. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.T.; Davis, T.Z.; Gardner, D.R.; Colegate, S.M.; Cook, D.; Green, B.T.; Meyerholtz, K.A.; Wilson, C.R.; Stegelmeier, B.L.; Evans, T.J. Tremetone and structurally related compounds in white snakeroot (Ageratina altissima): A plant associated with trembles and milk sickness. J. Agric. Food Chem. 2010, 58, 8560–8565. [Google Scholar] [CrossRef] [PubMed]
- Fritsch, R.M.; Keusgen, M. Occurrence and taxonomic significance of cysteine sulphoxides in the genus Allium L. (Alliaceae). Phytochemistry 2006, 67, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Sobolewska, D.; Michalska, K.; Podolak, I.; Grabowska, K. Steroidal saponins from the genus Allium. Phytochem. Rev. 2016, 15, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Calvey, E.M.; White, K.D.; Matusik, J.E.; Sha, D.; Block, E. Allium chemistry: Identification of organosulfur compounds in ramp (Allium tricoccum) homogenates. Phytochemistry 1998, 49, 359–364. [Google Scholar] [CrossRef]
- Chen, S.; Snyder, J.K. Molluscicidal saponins from Allium vineale. Tetrahedron Lett. 1987, 28, 5603–5606. [Google Scholar] [CrossRef]
- Chen, S.; Snyder, J.K. Diosgenin-bearing mulluscicidal saponins from Allium vineale: An NMR approach for the structural assignment of oligosaccharide units. J. Org. Chem. 1989, 54, 3679–3689. [Google Scholar] [CrossRef]
- Demirtas, I.; Erenler, R.; Elmastas, M.; Goktasoglu, A. Studies on the antioxidant potential of flavones of Allium vineale isolated from its water-soluble fraction. Food Chem. 2013, 136, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Satyal, P.; Craft, J.D.; Dosoky, N.S.; Setzer, W.N. The chemical compositions of the volatile oils of garlic (Allium sativum) and wild garlic (Allium vineale). Foods 2017, 6, 63. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; O’Neill, T.; Webster, D.; Johnson, J.A.; Gray, C.A. Anti-mycobacterial diynes from the Canadian medicinal plant Aralia nudicaulis. J. Ethnopharmacol. 2012, 140, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Davé, P.C.; Vogler, B.; Setzer, W.N. Chemical compositions of the leaf essential oils of Aralia spinosa from three habitats in Northern Alabama. Am. J. Plant Sci. 2011, 02, 507–510. [Google Scholar] [CrossRef]
- Wolf, S.J.; Denford, K.E. Flavonoid variation in Arnica cordifolia: An apomictic polyploid complex. Biochem. Syst. Ecol. 1983, 11, 111–114. [Google Scholar] [CrossRef]
- Merfort, I.; Wendisch, D. Sesquiterpene lactones of Arnica cordifolia, subgenus austromontana. Phytochemistry 1993, 34, 1436–1437. [Google Scholar] [CrossRef]
- Nematollahi, F.; Rustaiyan, A.; Larijani, K.; Madimi, M.; Masoudi, S. Essential oil composition of Artemisia biennis Willd. and Pulicaria undulata (L.) C.A. Mey., two Compositae herbs growing wild in Iran. J. Essent. Oil Res. 2006, 18, 339–341. [Google Scholar] [CrossRef]
- Lopes-Lutz, D.; Alviano, D.S.; Alviano, C.S.; Kolodziejczyk, P.P. Screening of chemical composition, antimicrobial and antioxidant activities of Artemisia essential oils. Phytochemistry 2008, 69, 1732–1738. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.Y.; Jun, D.Y.; Kim, Y.H.; Min, B.-S.; Min, B.K.; Woo, M.H. Monoterpenoids from the aerial parts of Aruncus dioicus var. kamtschaticus and their antioxidant and cytotoxic activities. Bioorg. Med. Chem. Lett. 2011, 21, 3252–3256. [Google Scholar] [PubMed]
- Han, C.R.; Jun, D.Y.; Woo, H.J.; Jeong, S.-Y.; Woo, M.-H.; Kim, Y.H. Induction of microtubule-damage, mitotic arrest, Bcl-2 phosphorylation, Bak activation, and mitochondria-dependent caspase cascade is involved in human Jurkat T-cell apoptosis by aruncin B from Aruncus dioicus var. kamtschaticus. Bioorg. Med. Chem. Lett. 2012, 22, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.T.; Jeong, S.Y.; Vu, V.D.; Min, B.S.; Kim, Y.H.; Woo, M.H. Cytotoxic and anti-oxidant constituents from the aerial parts of Aruncus dioicus var. kamtschaticus. Nat. Prod. Sci. 2013, 19, 66–70. [Google Scholar]
- Vo, Q.H.; Nguyen, P.H.; Zhao, B.T.; Thi, Y.N.; Nguyen, D.H.; Kim, W.I.; Seo, U.M.; Min, B.S.; Woo, M.H. Bioactive constituents from the n-butanolic fraction of Aruncus dioicus var. kamtschaticus. Nat. Prod. Sci. 2014, 20, 274–280. [Google Scholar]
- Fusani, P.; Piwowarski, J.P.; Zidorn, C.; Kiss, A.K.; Scartezzini, F.; Granica, S. Seasonal variation in secondary metabolites of edible shoots of Buck’s beard [Aruncus dioicus (Walter) Fernald (Rosaceae)]. Food Chem. 2016, 202, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Iwashina, T.; Kitajima, J. Chalcone and flavonol glycosides from Asarum canadense (Aristolochiaceae). Phytochemistry 2000, 55, 971–974. [Google Scholar] [CrossRef]
- Bauer, L.; Bell, C.L.; Gearien, J.E.; Takeda, H. Constituents of the rhizome of Asarum canadense. J. Pharm. Sci. 1967, 56, 336–343. [Google Scholar] [CrossRef]
- Motto, M.G.; Secord, N.J. Composition of the essential oil from Asarum canadense. J. Agric. Food Chem. 1985, 33, 789–791. [Google Scholar] [CrossRef]
- Bélanger, A.; Collin, G.; Garneau, F.-X.; Gagnon, H.; Pichette, A. Aromas from Quebec. II. Composition of the essential oil of the rhizomes and roots of Asarum canadense L. J. Essent. Oil Res. 2010, 22, 164–169. [Google Scholar] [CrossRef]
- Garneau, F.; Collin, G.; Gagnon, H. Chemical composition and stability of the hydrosols obtained during essential oil production. I. The case of Melissa officinalis L. and Asarum canadense L. Am. J. Essent. Oils Nat. Prod. 2014, 2, 54–62. [Google Scholar]
- Abe, F.; Yamauchi, T. An androstane bioside and 3’-thiazolidinone derivatives of doubly-linked cardenolide glycosides from the roots of Asclepias tuberosa. Chem. Pharm. Bull. 2000, 48, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Abe, F.; Yamauchi, T. Pregnane glycosides from the roots of Asclepias tuberosa. Chem. Pharm. Bull. 2000, 48, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Warashina, T.; Noro, T. 8,14-Secopregnane glycosides from the aerial parts of Asclepias tuberosa. Phytochemistry 2009, 70, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Warashina, T.; Noro, T. 8,12;8,20-Diepoxy-8,14-secopregnane glycosides from the aerial parts of Asclepias tuberosa. Chem. Pharm. Bull. 2010, 58, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Warashina, T.; Umehara, K.; Miyase, T.; Noro, T. 8,12;8,20-Diepoxy-8,14-secopregnane glycosides from roots of Asclepias tuberosa and their effect on proliferation of human skin fibroblasts. Phytochemistry 2011, 72, 1865–1875. [Google Scholar] [CrossRef] [PubMed]
- Lebreton, P.; Markham, K.R.; Swift, W.T., III; Mabry, T.J. Flavonoids of Baptista australis (Leguminosae). Phytochemistry 1967, 6, 1675–1680. [Google Scholar] [CrossRef]
- Markham, K.R.; Swift, W.T.; Mabry, T.J. A new isoflavone glycoside from Baptisia australis. J. Org. Chem. 1968, 33, 462–464. [Google Scholar] [CrossRef] [PubMed]
- Fraser, A.M.; Robins, D.J. Incorporation of enantiomeric [1 2H]cadaverines into the quinolizindine alkaloids (+)-sparteine and (−)-N-methylcytisine in Baptisia australis. J. Chem. Soc. Chem. Commun. 1986, 1986, 545–547. [Google Scholar] [CrossRef]
- Zenk, M.H.; Rueffer, M.; Amann, M.; Deus-Neumann, B. Benzylisoquinoline biosynthesis by cultivated plant cells and isolated enzymes. J. Nat. Prod. 1985, 48, 725–738. [Google Scholar] [CrossRef] [Green Version]
- Woods, K.E.; Jones, C.D.; Setzer, W.N. Bioactivities and compositions of Betula nigra essential oils. J. Med. Act. Plants 2013, 2, 1–9. [Google Scholar]
- Hua, Y.; Bentley, M.D.; Cole, B.J.W.; Murray, K.D.; Alford, A.R. Triterpenes from the outer bark of Betula nigra. J. Wood Chem. Technol. 1991, 11, 503–516. [Google Scholar] [CrossRef]
- Wollenweber, E. Rare methoxy flavonoids from buds of Betula nigra. Phytochemistry 1976, 15, 438–439. [Google Scholar] [CrossRef]
- Wollenweber, E. New flavonoids from Betula nigra. Phytochemistry 1977, 16, 295. [Google Scholar] [CrossRef]
- Tellez, M.R.; Dayan, F.E.; Schrader, K.K.; Wedge, D.E.; Duke, S.O. Composition and some biological activities of the essential oil of Callicarpa americana (L.). J. Agric. Food Chem. 2000, 48, 3008–3012. [Google Scholar] [CrossRef] [PubMed]
- Cantrell, C.L.; Klun, J.A.; Bryson, C.T.; Kobaisy, M.; Duke, S.O. Isolation and identification of mosquito bite deterrent terpenoids from leaves of American (Callicarpa americana) and Japanese (Callicarpa japonica) beautyberry. J. Agric. Food Chem. 2005, 53, 5948–5953. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.F.; Cantrell, C.L.; Klun, J.A.; Kramer, M. Repellency of two terpenoid compounds isolated from Callicarpa americana (Lamiaceae) against Ixodes scapularis and Amblyomma americanum ticks. Exp. Appl. Acarol. 2007, 41, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Jones, W.P.; Lobo-Echeverri, T.; Mi, Q.; Chai, H.-B.; Soejarto, D.D.; Cordell, G.A.; Swanson, S.M.; Kinghorn, A.D. Cytotoxic constituents from the fruiting branches of Callicarpa americana collected in southern Florida. J. Nat. Prod. 2007, 70, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.P.; Chang, N.; Knaak, L.E. Anthocyanins in Calycanthus floridus. Am. Midl. Nat. 1969, 82, 633–637. [Google Scholar] [CrossRef]
- Miller, E.R.; Taylor, G.W.; Eskew, M.H. The volatile oil of Calycanthus floridus. J. Am. Chem. Soc. 1914, 36, 2182–2187. [Google Scholar] [CrossRef]
- Collins, R.P.; Halim, A.F. Essential leaf oils in Calycanthus floridus. Planta Med. 1971, 20, 241–243. [Google Scholar] [CrossRef] [PubMed]
- Akhlaghi, H. Chemical composition of the essential oil from flowers of Calycanthus floridus L. var. oblongifolius (Nutt.) D.E. Boufford & S.A. Spongberg from Iran. J. Pharm. Heal. Sci. 2014, 2, 111–114. [Google Scholar]
- Akhlaghi, H. Chemical composition of the essential oil from stems of Calycanthus floridus L. var. oblongifolius from Iran. Chem. Nat. Compd. 2008, 44, 661–662. [Google Scholar] [CrossRef]
- Woldemariam, T.Z.; Betz, J.M.; Houghton, P.J. Analysis of aporphine and quinolizidine alkaloids from Caulophyllum thalictroides by densitometry and HPLC. J. Pharm. Biomed. Anal. 1997, 15, 839–843. [Google Scholar] [CrossRef]
- Betz, J.M.; Andrzejewski, D.; Troy, A.; Casey, R.E.; Obermeyer, W.R.; Page, S.W.; Woldemariam, T.Z. Gas chromatographic determination of toxic quinolizidine alkaloids in blue cohosh Caulophyllum thalictroides (L.) Michx. Phytochem. Anal. 1998, 9, 232–236. [Google Scholar] [CrossRef]
- Kennelly, E.J.; Flynn, T.J.; Mazzola, E.P.; Roach, J.A.; McCloud, T.G.; Danford, D.E.; Betz, J.M. Detecting potential teratogenic alkaloids from blue cohosh rhizomes using an in vitro rat embryo culture. J. Nat. Prod. 1999, 62, 1385–1389. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Khan, I.A. Alkaloids and saponins from blue cohosh. Phytochemistry 2008, 69, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Madgula, V.L.M.; Ali, Z.; Smillie, T.; Khan, I.; Walker, L.A.; Khan, S.I. Alkaloids and saponins as cytochrome P450 inhibitors from blue cohosh (Caulophyllum thalictroides) in an in vitro assay. Planta Med. 2009, 75, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Jhoo, J.-W.; Sang, S.; He, K.; Cheng, X.; Zhu, N.; Stark, R.E.; Zheng, Q.Y.; Rosen, R.T.; Ho, C.-T. Characterization of the triterpene saponins of the roots and rhizomes of blue cohosh (Caulophyllum thalictroides). J. Agric. Food Chem. 2001, 49, 5969–5974. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, Y.; Watanabe, K.; Mimaki, Y. Triterpene glycosides from the underground parts of Caulophyllum thalictroides. J. Nat. Prod. 2009, 72, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Jung, J.-C.; Ali, Z.; Khan, I.A.; Oh, S. Anti-inflammatory effect of triterpene saponins isolated from blue cohosh (Caulophyllum thalictroides). Evid. Based Complement. Altern. Med. 2012, 2012, 798192. [Google Scholar] [CrossRef] [PubMed]
- Warnhoff, E.W.; Pradhan, S.K.; Ma, J.C. Ceanothus alkaloids I. Isolation, separation, and characterization. Can. J. Chem. 1965, 53, 2594–2602. [Google Scholar] [CrossRef]
- Klein, F.K.; Rapoport, H. Ceanothus alkaloids. Americine. J. Am. Chem. Soc. 1968, 90, 2398–2404. [Google Scholar] [CrossRef] [PubMed]
- Servis, R.E.; Kosak, A.I.; Tschesche, R.; Frohberg, E.; Fehlhaber, H.-W. Peptide alkaloids from Ceanothus americanus L. (Rhamnaceae). J. Am. Chem. Soc. 1969, 91, 5619–5624. [Google Scholar] [CrossRef]
- Steinberg, K.M.; Satyal, P.; Setzer, W.N. Chemical composition of the bark essential oil of Cercis canadensis L. (Fabaceae). Am. J. Essent. Oils Nat. Prod. 2017, 5, 15–17. [Google Scholar]
- Bowers, M.D.; Boockvar, K.; Collinge, S.K. Iridoid glycosides of Chelone glabra (Scrophulariaceae) and their sequestration by larvae of a wawfly, Tenthredo grandis (Tenthredinidae). J. Chem. Ecol. 1993, 19, 815–823. [Google Scholar] [CrossRef] [PubMed]
- St. Pyrek, J. Sesquiterpene lactones of Cinchorium intybus and Leontodon autumnalis. Phytochemistry 1985, 24, 186–188. [Google Scholar] [CrossRef]
- Kisiel, W.; Zielińska, K. Guaianolides from Cichorium intybus and structure revision of Cichorium sesquiterpene lactones. Phytochemistry 2001, 57, 523–527. [Google Scholar] [CrossRef]
- Bischoff, T.A.; Kelley, C.J.; Karchesy, Y.; Laurantos, M.; Nguyen-Dinh, P.; Arefi, A.G. Antimalarial activity of lactucin lnd lactucopicrin: Sesquiterpene lactones isolated from Cichorium intybus L. J. Ethnopharmacol. 2004, 95, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Wesołowska, A.; Nikiforuk, A.; Michalska, K.; Kisiel, W.; Chojnacka-Wójcik, E. Analgesic and sedative activities of lactucin and some lactucin-like guaianolides in mice. J. Ethnopharmacol. 2006, 107, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Nørbæk, R.; Nielsen, K.; Kondo, T. Anthocyanins from flowers of Cichorium intybus. Phytochemistry 2002, 60, 357–359. [Google Scholar] [CrossRef]
- He, K.; Zheng, B.; Kim, C.H.; Rogers, L.; Zheng, Q. Direct analysis and identification of triterpene glycosides by LC/MS in black cohosh, Cimicifuga racemosa, and in several commercially available black cohosh products. Planta Med. 2000, 66, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Bedir, E.; Khan, I.A. Cimiracemoside A: A new cyclolanostanol xyloside from the rhizome of Cimicifuga racemosa. Chem. Pharm. Bull. 2000, 48, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Lai, G.F.; Wang, Y.-F.; Fan, L.-M.; Cao, J.-X.; Luo, S.-D. Triterpenoid glycoside from Cimicifuga racemosa. J. Asian Nat. Prod. Res. 2005, 7, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Shao, Y.; Harris, A.; Wang, M.; Zhang, H.; Cordell, G.A.; Bowman, M.; Lemmo, E. Triterpene glycosides from Cimicifuga racemosa. J. Nat. Prod. 2000, 63, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Mimaki, Y.; Sakagami, H.; Sashida, Y. Cycloartane glycosides from the rhizomes of Cimicifuga racemosa and their cytotoxic activities. Chem. Pharm. Bull. 2002, 50, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, S.; Aburatani, M.; Ohta, T. Isolation of CYP3A4 inhibitors from the black cohosh (Cimicifuga racemosa). Evid. Based Complement. Altern. Med. 2005, 2, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Cicek, S.S.; Schwaiger, S.; Ellmerer, E.P.; Stuppner, H. Development of a fast and convenient method for the isolation of triterpene saponins from Actaea racemosa by high-speed countercurrent chromatography coupled with evaporative light scattering detection. Planta Med. 2010, 76, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Jamróz, M.K.; Jamróz, M.H.; Dobrowolski, J.C.; Gliński, J.A.; Davey, M.H.; Wawer, I. Novel and unusual triterpene from black cohosh. Determination of structure of 9,10-seco-9,19-cyclolanostane xyloside (cimipodocarpaside) by NMR, IR and Raman spectroscopy and DFT calculations. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2011, 78, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Jamróz, M.K.; Paradowska, K.; Gliński, J.A.; Wawer, I. 13C CPMAS NMR studies and DFT calculations of triterpene xylosides isolated from Actaea racemosa. J. Mol. Struct. 2011, 994, 248–255. [Google Scholar] [CrossRef]
- Jamróz, M.K.; Jamróz, M.H.; Dobrowolski, J.C.; Gliński, J.A.; Gleńsk, M. One new and six known triterpene xylosides from Cimicifuga racemosa: FT-IR, Raman and NMR studies and DFT calculations. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2012, 93, 10–18. [Google Scholar] [CrossRef] [PubMed]
- He, C.-C.; Dai, Y.-Q.; Hui, R.-R.; Hua, J.; Chen, H.-J.; Luo, Q.-Y.; Li, J.-X. NMR-based metabonomic approach on the toxicological effects of a Cimicifuga triterpenoid. J. Appl. Toxicol. 2012, 32, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Kruse, S.O.; Löhning, A.; Pauli, G.F.; Winterhoff, H.; Nahrstedt, A. Fukiic and piscidic acid esters from the rhizome of Cimicifuga racemosa and the in vitro estrogenic activity of fukinolic acid. Planta Med. 1999, 65, 763–764. [Google Scholar] [CrossRef] [PubMed]
- Stromeier, S.; Petereit, F.; Nahrstedt, A. Phenolic esters from the rhizomes of Cimicifuga racemosa do not cause proliferation effects in MCF-7 cells. Planta Med. 2005, 71, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-N.; Fabricant, D.S.; Lu, Z.-Z.; Zhang, H.; Fong, H.H.S.; Farnsworth, N.R. Cimiracemates A-D, phenylpropanoid esters from the rhizomes of Cimicifuga racemosa. Phytochemistry 2002, 61, 409–413. [Google Scholar] [CrossRef]
- Li, W.; Chen, S.; Fabricant, D.; Angerhofer, C.K.; Fong, H.S.; Farnsworth, N.R.; Fitzloff, J.F. High-performance liquid chromatographic analysis of black cohosh (Cimicifuga racemosa) constituents with in-line evaporative light scattering and photodiode array detection. Anal. Chim. Acta 2002, 471, 61–75. [Google Scholar] [CrossRef]
- Nuntanakorn, P.; Jiang, B.; Einbond, L.S.; Yang, H.; Kronenberg, F.; Weinstein, I.B.; Kennelly, E.J. Polyphenolic constituents of Actaea racemosa. Nournal Nat. Prod. 2006, 69, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Gödecke, T.; Lankin, D.C.; Nikolic, D.; Chen, S.-N.; van Breemen, R.B.; Farnsworth, N.R.; Pauli, G.F. Guanidine alkaloids and Pictet-Spengler adducts from black cohosh (Cimicifuga racemosa). J. Nat. Prod. 2009, 72, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Azimova, S.S.; Gluchenkova, A.I. (Eds.) Collinsonia canadensis L. In Lipids, Lipophilic Components and Essential Oils from Plant Sources; Springer: London, UK, 2012; p. 401. [Google Scholar]
- Joshi, B.S.; Moore, K.M.; Pelletier, S.W.; Puar, M.S.; Pramanik, B.N. Saponins from Collinsonia canadensis. J. Nat. Prod. 1992, 55, 1468–1474. [Google Scholar] [CrossRef]
- Stevens, J.F.; Ivancic, M.; Deinzer, M.L.; Wollenweber, E. A novel 2-hydroxyflavanone from Collinsonia canadensis. J. Nat. Prod. 1999, 62, 392–394. [Google Scholar] [CrossRef] [PubMed]
- Hutton, K. A Comparative Study of the Plants Used for Medicinal Purposes by the Creek and Seminole Tribes. Master’s Thesis, University of South Florida, Tampa, FL, USA, 2010. [Google Scholar]
- Mukhtar, N.; Iqbal, K.; Anis, I.; Malik, A. Sphingolipids from Conyza canadensis. Phytochemistry 2002, 61, 1005–1008. [Google Scholar] [CrossRef]
- Mukhtar, N.; Iqbal, K.; Malik, A. Sphingolipids from Conyza canadensis. Chem. Pharm. Bull. 2002, 50, 1558–1560. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.M.; Li, T.Y.; Zhao, D.Q.; Shao, S.; Bi, S.N. A new derivative of triterpene with anti-melanoma B16 activity from Conyza canadensis. Chin. Chem. Lett. 2010, 21, 834–837. [Google Scholar] [CrossRef]
- Shakirullah, M.; Ahmad, H.; Shah, M.R.; Imtiaz, A.; Ishaq, M.; Khan, N.; Badshah, A.; Khan, I. Antimicrobial activities of conyzolide and conyzoflavone from Conyza canadensis. J. Enzyme Inhib. Med. Chem. 2011, 26, 468–471. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.D.; Gao, X.; Jia, Z.J. A new C-10 acetylene and a new triterpenoid from Conyza canadensis. Arch. Pharm. Res. 2007, 30, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Su, Y.; Guo, H.; Yang, F.; Mao, H.; Gao, X.; Zhu, Z.; Tu, G. Phenylpropanoyl esters from horseweed (Conyza canadensis) and their inhibitory effects on catecholamine secretion. J. Nat. Prod. 2010, 73, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, S.C.N.; Cantrell, C.L.; Duke, S.O.; Nandula, V.; Moraes, R.M.; Cerdeira, A.L. Bioassay-directed isolation and identification of phytotoxic terpenoids from horseweed (Conyza canadensis). Planta Med. 2012, 78, P48. [Google Scholar] [CrossRef]
- Porto, R.S.; Rath, S.; Queiroz, S.C.N. Conyza canadensis: Green extraction method of bioactive compounds and evaluation of their antifungal activity. J. Braz. Chem. Soc. 2017, 28, 913–919. [Google Scholar] [CrossRef]
- Pawlaczyk, I.; Czerchawski, L.; Kuliczkowski, W.; Karolko, B.; Pilecki, W.; Witkiewicz, W.; Gancarz, R. Anticoagulant and anti-platelet activity of polyphenolic-polysaccharide preparation isolated from the medicinal plant Erigeron canadensis L. Thromb. Res. 2011, 127, 328–340. [Google Scholar] [CrossRef] [PubMed]
- Csupor-Löffler, B.; Hajdú, Z.; Zupkó, I.; Molnár, J.; Forgo, P.; Kele, Z.; Hohmann, J. New dihydropyrone derivatives and further antitumor compounds from Conyza canadensis. Planta Med. 2010, 76, P258. [Google Scholar] [CrossRef]
- Csupor-Löffler, B.; Hajdú, Z.; Zupkó, I.; Molnár, J.; Forgo, P.; Vasas, A.; Kele, Z.; Hohmann, J. Antiproliferative constituents of the roots of Conyza canadensis. Planta Med. 2011, 77, 1183–1188. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Qin, Y.-H.; Yu, J.-Y.; Ma, H.; Song, X.-L. 3-β-Erythrodiol isolated from Conyza canadensis inhibits MKN-45 human gastric cancer cell proliferation by inducing apoptosis, cell cycle arrest, DNA fragmentation, ROS generation and reduces tumor weight and volume in mouse xenograft model. Oncol. Rep. 2016, 35, 2328–2338. [Google Scholar] [CrossRef] [PubMed]
- Banday, J.A.; Mir, F.A.; Farooq, S.; Qurishi, M.A.; Koul, S.; Razdan, T.K. Salicylic acid and methyl gallate from the roots of Conyza canedensis. Int. J. Chem. Anal. Sci. 2012, 3, 2–5. [Google Scholar]
- Banday, J.A.; Farooq, S.; Qurishi, M.A.; Koul, S.; Razdan, T.K. Conyzagenin-A and B, two new epimeric lanostane triterpenoids from Conyza canadensis. Nat. Prod. Res. 2013, 27, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Curini, M.; Bianchi, A.; Epifano, F.; Bruni, R.; Torta, L.; Zambonelli, A. Compsotion and in vitro antifungal activity of essential oils of Erigeron canadensis and Myrtus communis from France. Chem. Nat. Compd. 2003, 39, 191–194. [Google Scholar] [CrossRef]
- Lis, A.; Piggott, J.R.; Góra, J. Chemical composition variability of the essential oil of Conyza canadensis Cronq. Flavour Fragr. J. 2003, 18, 364–367. [Google Scholar] [CrossRef]
- Tzakou, O.; Vagias, C.; Gani, A.; Yannitsaros, A. Volatile constituents of essential oils isolated at different growth stages from three Conyza species growing in Greece. Flavour Fragr. J. 2005, 20, 425–428. [Google Scholar] [CrossRef]
- Lis, A.; Góra, J. Essential oil of Conyza canadensis (L.) Cronq. J. Essent. Oil Res. 2000, 12, 781–783. [Google Scholar] [CrossRef]
- Stoyanova, A.; Georgiev, E.; Kermedchieva, D.; Lis, A.; Gora, J. Changes in the essential oil of Conyza canadensis (L.) Cronquist. during its vegetation. J. Essent. Oil Res. 2003, 15, 44–45. [Google Scholar] [CrossRef]
- Rustaiyan, A.; Azar, P.A.; Moradalizadeh, M.; Masoudi, S.; Ameri, N. Volatile constituents of three Compositae herbs: Anthemis altissima L. var altissima, Conyza canadensis (L.) Cronq. and Grantina aucheri Boiss. growing wild in Iran. J. Essent. Oil Res. 2004, 16, 579–581. [Google Scholar] [CrossRef]
- Miyazawa, M.; Yamamoto, K.; Kameoka, H. The essential oil of Erigeron canadensis L. J. Essent. Oil Res. 1992, 4, 227–230. [Google Scholar] [CrossRef]
- Choi, H.-J.; Want, H.-Y.; Kim, Y.-N.; Heo, S.-J.; Kim, N.-K.; Jeong, M.-S.; Park, Y.-H.; Kim, S. Composition and cytotoxicity of essential oil extracted by steam distillation from horseweed (Erigeron canadensis L.) in Korea. J. Korean Soc. Appl. Biol. Chem. 2008, 51, 55–59. [Google Scholar]
- Veres, K.; Csupor-Löffler, B.; Lázár, A.; Hohmann, J. Antifungal activity and composition of essential oils of Conyza canadensis herbs and roots. Sci. World J. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Du, D.; Liang, Y.; Xin, G.; Huang, B.-Z.; Huang, W. Novel polyacetylenes from Coreopsis tinctoria Nutt. J. Asian Nat. Prod. Res. 2015, 17, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Lam, S.-C.; Lam, S.-F.; Zhao, J.; Li, S.-P. Rapid identification and comparison of compounds with antioxidant activity in Coreopsis tinctoria herbal tea by high-performance thin-layer chromatography coupled with DPPH bioautography and densitometry. J. Food Sci. 2016, 81, C2218–C2223. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shi, S.; Zhao, M.; Chai, X.; Tu, P. Coreosides A-D, C14-polyacetylene glycosides from the capitula of Coreopsis tinctoria and its anti-inflammatory activity against COX-2. Fitoterapia 2013, 87, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, A.; Yang, K.; Ding, H.; Hu, Y.; Yang, Y.; Huang, S.; Xu, J.; Liu, T.; Yang, H.; et al. Isolation, characterization and antimicrobial activities of polyacetylene glycosides from Coreopsis tinctoria Nutt. Phytochemistry 2017, 136, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Du, D.; Jin, T.; Xing, Z.-H.; Hu, L.-Q.; Long, D.; Li, S.-F.; Gong, M. One new linear C14 polyacetylene glucoside with antiadipogenic activities on 3T3-L1 cells from the capitula of Coreopsis tinctoria. J. Asian Nat. Prod. Res. 2016, 18, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Dias, T.; Liu, B.; Jones, P.; Houghton, P.J.; Mota-Filipe, H.; Paulo, A. Cytoprotective effect of Coreopsis tinctoria extracts and flavonoids on tBHP and cytokine-induced cell injury in pancreatic MIN6 cells. J. Ethnopharmacol. 2012, 139, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shi, S.; Zhao, M.; Jiang, Y.; Tu, P. A novel chalcone from Coreopsis tinctoria Nutt. Biochem. Syst. Ecol. 2006, 34, 766–769. [Google Scholar] [CrossRef]
- Dias, T.; Bronze, M.R.; Houghton, P.J.; Mota-Filipe, H.; Paulo, A. The flavonoid-rich fraction of Coreopsis tinctoria promotes glucose tolerance regain through pancreatic function recovery in streptozotocin-induced glucose-intolerant rats. J. Ethnopharmacol. 2010, 132, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Abdureyim, A.; Abliz, M.; Sultan, A.; Eshbakova, K.A. Phenolic compounds from the flowers of Coreopsis tinctoria. Chem. Nat. Compd. 2013, 48, 1085–1086. [Google Scholar] [CrossRef]
- Ma, Z.; Zheng, S.; Han, H.; Meng, J.; Yang, X.; Zeng, S.; Zhou, H.; Jiang, H. The bioactive components of Coreopsis tinctoria (Asteraceae) capitula: Antioxidant activity in vitro and profile in rat plasma. J. Funct. Foods 2016, 20, 575–586. [Google Scholar] [CrossRef]
- Chen, L.X.; Hu, D.J.; Lam, S.C.; Ge, L.; Wu, D.; Zhao, J.; Long, Z.R.; Yang, W.J.; Fan, B.; Li, S.P. Comparison of antioxidant activities of different parts from snow chrysanthemum (Coreopsis tinctoria Nutt.) and identification of their natural antioxidants using high performance liquid chromatography coupled with diode array detection and mass spectrometry and 2,2′-azinobis(3-ethylbenzthiazoline-sulfonic acid)diammonium salt-based assay. J. Chromatogr. A 2016, 1428, 134–142. [Google Scholar] [PubMed]
- Deng, Y.; Lam, S.-C.; Zhao, J.; Li, S.-P. Quantitative analysis of flavonoids and phenolic acid in Coreopsis tinctoria Nutt. by capillary zone electrophoresis. Electrophoresis 2017, 38, 2654–2661. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Sun, X.; Liu, J.; Kang, L.; Chen, S.; Ma, B.; Guo, B. Quantitative and qualitative analysis of flavonoids and phenolic acids in snow chrysanthemum (Coreopsis tinctoria Nutt.) by HPLC-DAD and UPLC-ESI-QTOF-MS. Molecules 2016, 21, 1307. [Google Scholar] [CrossRef] [PubMed]
- Zǎlaru, C.; Crişan, C.C.; Cǎlinescu, I.; Moldovan, Z.; Ţârcomnicu, I.; Litescu, S.C.; Tatia, R.; Moldovan, L.; Boda, D.; Iovu, M. Polyphenols in Coreopsis tinctoria Nutt. fruits and the plant extracts antioxidant capacity evaluation. Cent. Eur. J. Chem. 2014, 12, 858–867. [Google Scholar] [CrossRef]
- Wang, T.; Xi, M.; Guo, Q.; Wang, L.; Shen, Z. Chemical components and antioxidant activity of volatile oil of a Compositae tea (Coreopsis tinctoria Nutt.) from Mt. Kunlun. Ind. Crops Prod. 2015, 67, 318–323. [Google Scholar] [CrossRef]
- Hostettmann, K.; Hostettmann-Kaldas, M.; Nakanishi, K. Molluscicidal saponins from Cornus florida L. Helv. Chim. Acta 1978, 61, 1990–1995. [Google Scholar] [CrossRef]
- Robins, R.J.; Abraham, T.W.; Parr, A.J.; Eagles, J.; Walton, N.J. The biosynthesis of tropane alkaloids in Datura stramonium: The identity of the intermediates between N-methylpyrrolinium salt and tropinone. J. Am. Chem. Soc. 1997, 119, 10929–10934. [Google Scholar] [CrossRef]
- Monforte-González, M.; Ayora-Talavera, T.; Maldonado-Mendoza, E.; Loyola-Vargas, V.M. Quantitative analysis of serpentine and ajmalicine in plant tissues of Catharanthus roseus and hyoscyamine and scopolamine in root tissues of Datura stramonium by thin layer chromatography-densitometry. Phytochem. Anal. 1992, 3, 117–121. [Google Scholar] [CrossRef]
- Lanfranchi, D.A.; Tomi, F.; Casanova, J. Enantiomeric differentiation of atropine/hyoscyamine by 13C NMR spectroscopy and its application to Datura stramonium extract. Phytochem. Anal. 2010, 21, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Mroczek, T.; Głowniak, K.; Kowalska, J. Solid-liquid extraction and cation-exchange solid-phase extraction using a mixed-mode polymeric sorbent of Datura and related alkaloids. J. Chromatogr. A 2006, 1107, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Fallas, A.L.; Thomson, R.H. Ebenaceae extractives. Part III. Binaphthaquinones from Diospyros species. J. Chem. Soc. C Org. 1968, 1968, 2279–2282. [Google Scholar] [CrossRef]
- Rashed, K.; Ćirić, A.; Glamočlija, J.; Soković, M. Antibacterial and antifungal activities of methanol extract and phenolic compounds from Diospyros virginiana L. Ind. Crops Prod. 2014, 59, 210–215. [Google Scholar] [CrossRef]
- Wang, X.; Habib, E.; León, F.; Radwan, M.M.; Tabanca, N.; Gao, J.; Wedge, D.E.; Cutler, S.J. Antifungal metabolites from the roots of Diospyros virginiana by overpressure layer chromatography. Chem. Biodivers. 2011, 8, 2331–2340. [Google Scholar] [CrossRef] [PubMed]
- Kiss, A.; Kowalski, J.; Melzig, M.F. Compounds from Epilobium angustifolium inhibit the specific metallopeptidases ACE, NEP and APN. Planta Med. 2004, 70, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Kiss, A.; Kowalski, J.; Melzig, M.F. Effect of Epilobium angustifolium L. extracts and polyphenols on cell proliferation and neutral endopeptidase activity in selected cell lines. Pharmazie 2006, 61, 66–69. [Google Scholar] [PubMed]
- Ramstead, A.G.; Schepetkin, I.A.; Quinn, M.T.; Jutila, M.A. Oenothein B, a cyclic dimeric ellagitannin isolated from Epilobium angustifolium, enhances IFNγ production by lymphocytes. PLoS ONE 2012, 7, e50546. [Google Scholar] [CrossRef] [PubMed]
- Baert, N.; Karonen, M.; Salminen, J.P. Isolation, characterisation and quantification of the main oligomeric macrocyclic ellagitannins in Epilobium angustifolium by ultra-high performance chromatography with diode array detection and electrospray tandem mass spectrometry. J. Chromatogr. A 2015, 1419, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Baert, N.; Kim, J.; Karonen, M.; Salminen, J.P. Inter-population and inter-organ distribution of the main polyphenolic compounds of Epilobium angustifolium. Phytochemistry 2017, 134, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Park, B.-J.; Tomohiko, M. Feruloyl, caffeoyl, and flavonol glucosides from Equisetum hyemale. Chem. Nat. Compd. 2011, 47, 363–365. [Google Scholar] [CrossRef]
- Jin, M.; Zhang, C.; Zheng, T.; Yao, D.; Shen, L.; Luo, J.; Jiang, Z.; Ma, J.; Jin, X.-J.; Cui, J.; et al. A new phenyl glycoside from the aerial parts of Equisetum hyemale. Nat. Prod. Res. 2014, 28, 1813–1818. [Google Scholar] [CrossRef] [PubMed]
- Price, J.I. An in vitro evaluation of the Native American ethnomedicinal plant Eryngium yuccifolium as a treatment for snakebite envenomation. J. Intercult. Ethnopharmacol. 2016, 5, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Yarnell, E.; Abascal, K. Natural approaches to treating chronic prostatitis and chronic pelvic pain syndromes. Altern. Complement. Ther. 2005, 11, 246–251. [Google Scholar] [CrossRef]
- Ayoub, N.; Al-Azizi, M.; König, W.; Kubeczka, K.H. Essential oils and a novel polyacetylene from Eryngium yuccifolium Michaux. (Apiaceae). Flavour Fragr. J. 2006, 21, 864–868. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, S.; Ownby, S.; Wang, P.; Yuan, W.; Zhang, W.; Beasley, R.S. Phenolic compounds and rare polyhydroxylated triterpenoid saponins from Eryngium yuccifolium. Phytochemistry 2008, 69, 2070–2080. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Yuan, W.; Deng, G.; Su, Z.; Li, S. Triterpenoid saponins from Eryngium yuccifolium “Kershaw Blue”. Phytochem. Lett. 2013, 6, 306–309. [Google Scholar] [CrossRef]
- Wang, P.; Su, Z.; Yuan, W.; Deng, G.; Li, S. Phytochemical constituents and pharmacological activities of Eryngium L. (Apiaceae). Pharm. Crop. 2012, 3, 99–120. [Google Scholar] [CrossRef]
- Cavallito, C.J.; Haskell, T.H. α-Methylene butyrolactone from Erythronium americanum. J. Am. Chem. Soc. 1946, 68, 2332–2334. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, Y.; Marion, L. The alkaloids of Eupatorium maculatum L. Can. J. Chem. 1963, 41, 1919–1924. [Google Scholar] [CrossRef]
- Wiedenfeld, H.; Hösch, G.; Roeder, E.; Dingermann, T. Lycopsamine and cumambrin B from Eupatorium maculatum. Pharmazie 2009, 64, 415–416. [Google Scholar] [PubMed]
- Maas, M.; Hensel, A.; Da Costa, F.B.; Brun, R.; Kaiser, M.; Schmidt, T.J. An unusual dimeric guaianolide with antiprotozoal activity and further sesquiterpene lactones from Eupatorium perfoliatum. Phytochemistry 2011, 72, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Herz, W.; Kalyanaraman, P.S.; Ramakrishnan, G.; Blount, J.F. Sesquiterpene lactones of Eupatorium perfoliatum. J. Org. Chem. 1977, 42, 2264–2271. [Google Scholar] [CrossRef] [PubMed]
- Habtemariam, S. Activity-guided isolation and identification of free radical-scavenging components from ethanolic extract of boneset (leaves of Eupatorium perfoliatum). Nat. Prod. Commun. 2008, 3, 1317–1320. [Google Scholar]
- Maas, M.; Deters, A.M.; Hensel, A. Anti-inflammatory activity of Eupatorium perfoliatum L. extracts, eupafolin, and dimeric guaianolide via iNOS inhibitory activity and modulation of inflammation-related cytokines and chemokines. J. Ethnopharmacol. 2011, 137, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Maas, M.; Petereit, F.; Hensel, A. Caffeic acid derivatives from Eupatorium perfoliatum L. Molecules 2009, 14, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Herz, W. Chemistry of the Eupatoriinae. Biochem. Syst. Ecol. 2001, 29, 1115–1137. [Google Scholar] [CrossRef]
- Hensel, A.; Maas, M.; Sendker, J.; Lechtenberg, M.; Petereit, F.; Deters, A.; Schmidt, T.; Stark, T. Eupatorium perfoliatum L.: Phytochemistry, traditional use and current applications. J. Ethnopharmacol. 2011, 138, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Lewis, N.G.; Inciong, M.E.J.; Ohashi, H.; Towers, G.H.N.; Yamamoto, E. Exclusive accumulation of Z-isomers of monolignols and their glucosides in bark of Fagus grandifolia. Phytochemistry 1988, 27, 2119–2121. [Google Scholar] [CrossRef]
- Stout, G.H.; Balkenhol, W.J. Xanthones of the Gentianaceae-I: Frasera caroliniensis. Tetrahedron 1969, 25, 1947–1960. [Google Scholar] [CrossRef]
- Aberham, A.; Pieri, V.; Croom, E.M.; Ellmerer, E.; Stuppner, H. Analysis of iridoids, secoiridoids and xanthones in Centaurium erythraea, Frasera caroliniensis and Gentiana lutea using LC-MS and RP-HPLC. J. Pharm. Biomed. Anal. 2011, 54, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Eyles, A.; Jones, W.; Riedl, K.; Cipollini, D.; Schwartz, S.; Chan, K.; Herms, D.A.; Bonello, P. Comparative phloem chemistry of Manchurian (Fraxinus mandshurica) and two North American ash species (Fraxinus americana and Fraxinus pennsylvanica). J. Chem. Ecol. 2007, 33, 1430–1448. [Google Scholar] [CrossRef] [PubMed]
- Takenaka, Y.; Tanahashi, T.; Shintaku, M.; Sakai, T.; Nagakura, N. Parida Secoiridoid glucosides from Fraxinus americana. Phytochemistry 2000, 55, 275–284. [Google Scholar] [CrossRef]
- Aybek, A.; Zhou, J.; Malik, A.; Umar, S.; Xiao, Z. Catechins and proanthocyanidins from seeds of Fraxinus americana. Chem. Nat. Compd. 2015, 51, 565–567. [Google Scholar] [CrossRef]
- Gallardo, A.; Picollo, M.I.; González-Audino, P.; Mougabure-Cueto, G. Insecticidal activity of individual and mixed monoterpenoids of Geranium essential oil against Pediculus humanus capitis (Phthiraptera: Pediculidae). J. Med. Entomol. 2012, 49, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Tena, S.; Fernández-Cachón, M.L.; Carreras, A.; Mateos-Martín, M.L.; Costoya, N.; Moyer, M.P.; Nuñez, M.J.; Torres, J.L.; Cascante, M. Hamamelitannin from witch hazel (Hamamelis virginiana) displays specific cytotoxic activity against colon cancer cells. J. Nat. Prod. 2012, 75, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Duckstein, S.M.; Stintzing, F.C. Investigation on the phenolic constituents in Hamamelis virginiana leaves by HPLC-DAD and LC-MS/MS. Anal. Bioanal. Chem. 2011, 401, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Dauer, A.; Rimpler, H.; Hensel, A. Polymeric proanthocyanidins from the bark of Hamamelis virginiana. Planta Med. 2003, 69, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Touriño, S.; Lizárraga, D.; Carreras, A.; Lorenzo, S.; Ugartondo, V.; Mitjans, M.; Vinardell, M.P.; Julía, L.; Cascante, M.; Torres, J.L. Highly galloylated tannin fractions from witch hazel (Hamamelis virginiana) bark: Electron transfer capacity, in vitro antioxidant activity, and effects on skin-related cells. Chem. Res. Toxicol. 2008, 21, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Hartisch, C.; Kolodziej, H. Galloylhamameloses and proanthocyanidins from Hamamelis virginiana. Phytochemistry 1996, 42, 191–198. [Google Scholar] [CrossRef]
- Lucas, R.A.; Smith, R.G.; Dorfman, L. The isolation of dihydromexicanin E from Helenium autumnale L. J. Org. Chem. 1964, 29, 2101. [Google Scholar] [CrossRef]
- Herz, W.; Subramaniam, P.S.; Dennis, N. Constituents of Helenium species. XXIII. Stereochemistry of flexuosin A and related compounds. J. Org. Chem. 1969, 34, 2915–2917. [Google Scholar] [CrossRef]
- Herz, W.; de Vivar, A.R.; Romo, J.; Viswanathan, N. Constituents of Helenium species. XIII. The structure of helenalin and mexicanin A. J. Am. Chem. Soc. 1963, 85, 19–26. [Google Scholar] [CrossRef]
- Herz, W.; Subramaniam, P.S. Pseudoguianolides in Helenium autumnale from Pennsylvania. Phytochemistry 1972, 11, 1101–1103. [Google Scholar] [CrossRef]
- Lee, K.-H.; Meck, R.; Piantadosi, C.; Huang, E.-S. Antitumor agents. 4. Cytotoxicity and in vivo activity of helenalin esters and related derivatives. J. Med. Chem. 1973, 16, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, H.; Lee, K.-H.; Shingu, T.; Meck, R.; Piantadosi, C. Carolenin and carolenalin, two new guaianolides in Helenium autumnale L. from North Carolina. J. Org. Chem. 1973, 38, 1722–1725. [Google Scholar] [CrossRef] [PubMed]
- Pettit, G.R.; Budzinski, J.C.; Cragg, G.M.; Brown, P.; Johnston, L.D. Antineoplastic agents. 34. Helenium autumnale L. J. Med. Chem. 1974, 17, 1013–1016. [Google Scholar] [CrossRef] [PubMed]
- Kozuka, M.; Lee, K.-H.; McPhail, A.T.; Onan, K.D. Structure and absolute stereochemistry of dihydroflorilenalin, a new sesquiterpene lactone from Florida Helenium autumnale L. Chem. Pharm. Bull. 1975, 23, 1895–1897. [Google Scholar] [CrossRef]
- Furukawa, H.; Itoigawa, M.; Kumagai, N.; Ito, K.; McPhail, A.T.; Onan, K.D. Isolation and structure determination of 4-O-tigloyl-11,13-dihydroautumnolide, a new sesquiterpene lactone from North Carolina Helenium autumnale L. Chem. Pharm. Bull. 1978, 25, 1335–1337. [Google Scholar] [CrossRef]
- Gentry, E.J.; Jampani, H.B.; Keshavarz-Shokri, A.; Morton, M.D.; Vander Velde, D.; Telikepalli, H.; Mitscher, L.A.; Shawar, R.; Humble, D.; Baker, W. Antitubercular natural products: Berberine from the roots of commercial Hydrastis canadensis powder. Isolation of inactive 8-oxotetrahydrothalifendine, canadine, β-hydrastine, and two new quinic acid esters, hycandinic acid esters-1 and -2. J. Nat. Prod. 1998, 61, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Scazzocchio, F.; Cometa, M.F.; Tomassini, L.; Palmery, M. Antibacterial activity of Hydrastis canadensis extract and its major isolated alkaloids. Planta Med. 2001, 67, 561–564. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, L.R.; Wu, C.D.; Kinghorn, A.D. Isolation of alkaloids from goldenseal (Hydrastis canadensis rhizomes) using pH-zone refining countercurrent chromatography. J. Liq. Chromatogr. Relat. Technol. 2001, 24, 2445–2453. [Google Scholar] [CrossRef]
- Le, P.M.; McCooeye, M.; Windust, A. Characterization of the alkaloids in goldenseal (Hydrastis canadensis) root by high resolution Orbitrap LC-MSn. Anal. Bioanal. Chem. 2013, 405, 4487–4498. [Google Scholar] [CrossRef] [PubMed]
- Leyte-Lugo, M.; Britton, E.R.; Foil, D.H.; Brown, A.R.; Todd, D.A.; Rivera-Chávez, J.; Oberlies, N.H.; Cech, N.B. Secondary metabolites from the leaves of the medicinal plant goldenseal (Hydrastis canadensis). Phytochem. Lett. 2017, 20, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Junio, H.A.; Sy-Cordero, A.A.; Ettefagh, K.A.; Burns, J.T.; Micko, K.T.; Graf, T.N.; Richter, S.J.; Cannon, R.E.; Oberlies, N.H.; Cech, N.B. Synergy-directed fractionation of botanical medicines: A case study with goldenseal (Hydrastis canadensis). J. Nat. Prod. 2011, 74, 1621–1629. [Google Scholar] [CrossRef] [PubMed]
- Babka, H.L.; Hillwig, M.L.; Price, J.; Maury, W.; Harslan, H.; Wu, L.; Wurtele, E.S. Hypericum gentianoides produces bioactive compounds in schizogenously formed glands. Microsc. Microanal. 2010, 16, 1160–1161. [Google Scholar]
- Crispin, M.C.; Hur, M.; Park, T.; Kim, Y.H.; Wurtele, E.S. Identification and biosynthesis of acylphloroglucinols in Hypericum gentianoides. Physiol. Plant. 2013, 148, 354–370. [Google Scholar] [CrossRef] [PubMed]
- Hillwig, M.L.; Hammer, K.D.P.; Birt, D.F.; Wurtele, E.S. Characterizing the metabolic fingerprint and anti-inflammatory activity of Hypericum gentianoides. J. Agric. Food Chem. 2008, 56, 4359–4366. [Google Scholar] [CrossRef] [PubMed]
- Christian, O.E.; McLean, S.; Reynolds, W.F.; Jacobs, H. Prenylated benzophenones from Hypericum hypericoides. Nat. Prod. Commun. 2008, 3, 1781–1786. [Google Scholar]
- Dictionary of Natural Products Dictionary of Natural Products on DVD. J. Antibiot. 1994, 48, 261–266.
- Gupta, S.R.; Ravindranath, B.; Seshadri, T.R. Polyphenols of Juglans nigra. Phytochemistry 1972, 11, 2634–2636. [Google Scholar] [CrossRef]
- Binder, R.G.; Benson, M.E.; Flath, R.A. Eight 1,4-naphthoquinones from Juglans. Phytochemistry 1989, 28, 2799–2801. [Google Scholar] [CrossRef]
- Lal, C.; Raja, A.S.M.; Pareek, P.K.; Shakyawar, D.B.; Sharma, K.K.; Sharma, M.C. Juglans nigra: Chemical constitution and its application on Pashmina (Cashmere) fabric as a dye. J. Nat. Prod. Plant Resour. 2011, 1, 13–19. [Google Scholar]
- Paudel, P.; Satyal, P.; Dosoky, N.S.; Maharjan, S.; Setzer, W.N. Juglans regia and J. nigra, two trees important in traditional medicine: A comparison of leaf essential oil compositions and biological activities. Nat. Prod. Commun. 2013, 8, 1481–1486. [Google Scholar] [PubMed]
- Jin, D.-Z.; Min, Z.-D.; Chiou, G.C.Y.; Iinuma, M.; Tanaka, T. Two p-coumaroyl glycerides from Juncus effusus. Phytochemistry 1996, 41, 545–547. [Google Scholar]
- Dellagreca, M.; Fiorentino, A.; Monaco, P.; Previtera, L.; Sorrentino, M. Antialgal phenylpropane glycerides from Juncus effusus. Nat. Prod. Lett. 1998, 12, 263–270. [Google Scholar] [CrossRef]
- Della Greca, M.; Fiorentino, A.; Molinaro, A.; Monaco, P.; Previtera, L. A bioactive dihydrodibenzoxepin from Juncus effusus. Phytochemistry 1993, 34, 1182–1184. [Google Scholar] [CrossRef]
- Corsaro, M.M.; della Greca, M.; Fiorentino, A.; Monaco, P.; Previtera, L. Cycloartane glucosides from Juncus effusus. Phytochemistry 1994, 37, 515–519. [Google Scholar] [CrossRef]
- Della Greca, M.; Fiorentino, A.; Monaco, P.; Previtera, L. Cycloartane triterpenes from Juncus effusus. Phytochemistry 1994, 35, 1017–1022. [Google Scholar] [CrossRef]
- Della Greca, M.; Fiorentino, A.; Monaco, P.; Previtera, L. Juncoside I, a new cycloartanelactone glucoside from Juncus effusus. Nat. Prod. Lett. 1994, 4, 183–188. [Google Scholar] [CrossRef]
- Su, X.-H.; Yuan, Z.-P.; Li, C.-Y.; Zhong, Y.-J.; Du, H.-J.; Wen, Y.-Y.; Li, Y.-F.; Liang, B. Phenanthrenes from Juncus effusus. Planta Med. 2013, 79, 1447–1452. [Google Scholar] [CrossRef] [PubMed]
- Hanawa, F.; Okamoto, M.; Towers, G.H. Antimicrobial DNA-binding photosensitizers from the common rush, Juncus effusus. Photochem. Photobiol. 2002, 76, 51–56. [Google Scholar] [CrossRef]
- della Greca, M.; Fiorentino, A.; Mangoni, L.; Molinaro, A.; Monaco, P.; Previtera, L. 9,10-Dihydrophenanthrene metabolites from Juncus effusus L. Tetrahedron Lett. 1992, 33, 5257–5260. [Google Scholar] [CrossRef]
- Della Greca, M.; Fiorentino, A.; Mangoni, L.; Molinaro, A.; Monaco, P.; Previtera, L. Cytotoxic 9,10-dihydrophenanthrenes from Juncus effusus L. Tetrahedron 1993, 49, 3425–3432. [Google Scholar] [CrossRef]
- DellaGreca, M.; Monaco, P.; Previtera, L.; Zarrelli, A.; Pollio, A.; Pinto, G.; Fiorentino, A. Minor bioactive dihydrophenanthrenes from Juncus effusus. J. Nat. Prod. 1997, 60, 1265–1268. [Google Scholar] [CrossRef]
- Della Greca, M.; Fiorentino, A.; Previtera, L.; Zarrelli, A. Effusides I–V: 9,10-Dihydrophenanthrene glucosides from Juncus effusus. Phytochemistry 1995, 40, 533–535. [Google Scholar] [CrossRef]
- Wang, Y.-G.; Wang, Y.-L.; Zhai, H.-F.; Liao, Y.-J.; Zhang, B.; Huang, J.-M. Phenanthrenes from Juncus effusus with anxiolytic and sedative activities. Nat. Prod. Res. 2012, 26, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.Z.; Li, H.X.; Song, F.J.; Chen, Y. Diterpenoid and phenolic compounds from Juncus effusus L. Helv. Chim. Acta 2007, 90, 1289–1295. [Google Scholar] [CrossRef]
- Shima, K.; Toyota, M.; Asakawa, Y. Phenanthrene derivatives from the medullae of Juncus effusus. Phytochemistry 1991, 30, 3149–3151. [Google Scholar] [CrossRef]
- Ishiuchi, K.; Kosuge, Y.; Hamagami, H.; Ozaki, M.; Ishige, K.; Ito, Y.; Kitanaka, S. Chemical constituents isolated from Juncus effusus induce cytotoxicity in HT22 cells. J. Nat. Med. 2015, 69, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Della Greca, M.; Fiorentino, A.; Monaco, P.; Previtera, L.; Zarrelli, A. Tetrahydropyrene glucosides from Juncus effusus. Nat. Prod. Lett. 1995, 7, 85–92. [Google Scholar] [CrossRef]
- Ma, W.; Liu, F.; Ding, Y.Y.; Zhang, Y.; Li, N. Four new phenanthrenoid dimers from Juncus effusus L. with cytotoxic and anti-inflammatory activities. Fitoterapia 2015, 105, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Zhang, Y.; Ding, Y.Y.; Liu, F.; Li, N. Cytotoxic and anti-inflammatory activities of phenanthrenes from the medullae of Juncus effusus L. Arch. Pharm. Res. 2016, 39, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.J.; Zhai, H.F.; Zhang, B.; Duan, T.X.; Huang, J.M. Anxiolytic and sedative effects of dehydroeffusol from Juncus effusus in mice. Planta Med. 2011, 77, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Singhuber, J.; Baburin, I.; Khom, S.; Zehl, M.; Urban, E.; Hering, S.; Kopp, B. GABAA Receptor modulators from the Chinese herbal drug junci medulla—The pith of Juncus effusus. Planta Med. 2012, 78, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.D.; Jones, C.D.; Setzer, W.N. Essential oil compositions of Juniperus virginiana and Pinus virginiana, two important trees in Cherokee traditional medicine. Am. J. Essent. Oils Nat. Prod. 2014, 2, 17–24. [Google Scholar]
- Adams, R.P. Cedar wood oil—Analyses and properties. In Essential Oils and Waxes; Linskens, H.F., Jackson, J.F., Eds.; Springer: Berlin, Germany, 1991; pp. 159–173. [Google Scholar]
- Tumen, I.; Süntar, I.; Eller, F.J.; Keleş, H.; Akkol, E.K. Topical wound-healing effects and phytochemical composition of heartwood essential oils of Juniperus virginiana L., Juniperus occidentalis Hook., and Juniperus ashei J. Buchholz. J. Med. Food 2013, 16, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Renouard, S.; Lopez, T.; Hendrawati, O.; Dupre, P.; Doussot, J.; Falguieres, A.; Ferroud, C.; Hagege, D.; Lamblin, F.; Laine, E.; et al. Podophyllotoxin and deoxypodophyllotoxin in Juniperus bermudiana and 12 other Juniperus species: Optimization of extraction, method validation, and quantification. J. Agric. Food Chem. 2011, 59, 8101–8107. [Google Scholar] [CrossRef] [PubMed]
- Michalska, K.; Szneler, E.; Kisiel, W. Sesquiterpene lactones from Lactuca canadensis and their chemotaxonomic significance. Phytochemistry 2013, 90, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Kagan, J. The flavonoid pigments of Liatris spicata. Phytochemistry 1968, 7, 1205–1207. [Google Scholar] [CrossRef]
- Karlsson, K.; Wahlberg, I.; Enzell, C.R. Volatile constituents of the Liatris species, L. spicata, L. elegans and L. gracilis. Acta Chem. Scand. 1973, 27, 1613–1621. [Google Scholar] [CrossRef] [PubMed]
- Herz, W.; Poplawski, J.; Sharma, R.P. New guaianolides from Liatris species. J. Org. Chem. 1975, 40, 199–206. [Google Scholar] [CrossRef]
- Ezzat, M.I.; Ezzat, S.M.; El Deeb, K.S.; El Fishawy, M. In vitro cytotoxic activity of the ethanol extract and isolated compounds from the corms of Liatris spicata (L.) Willd on HepG2. Nat. Prod. Res. 2017, 31, 1325–1328. [Google Scholar] [CrossRef] [PubMed]
- Setzer, W.N. Chemical composition of the leaf essential oil of Lindera benzoin growing in North Alabama. Am. J. Essent. Oils Nat. Prod. 2016, 4, 1–3. [Google Scholar]
- Tucker, A.O.; Maciarello, M.J.; Burbage, P.W.; Sturtz, G. Spicebush [Lindera benzoin (L.) Blume var. benzoin, Lauraceae]: A tea, spice, and medicine. Econ. Bot. 1994, 48, 333–336. [Google Scholar]
- Anderson, J.E.; Ma, W.; Smith, D.L.; Chang, C.-J.; McLaughlin, J.L. Biologically active γ-lactones and methylketoalkenes from Lindera benzoin. J. Nat. Prod. 1992, 55, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Duke, J.; Pelkki, M.; Clausen, E.C.; Carrier, D.J. Sweetgum (Liquidambar styraciflua L.): Extraction of shikimic acid coupled to dilute acid pretreatment. Appl. Biochem. Biotechnol. 2010, 162, 1660–1668. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Fukuda, Y.; Matsunaga, S.; Tanaka, R.; Yamori, T. New cytotoxic oleanane-type triterpenoids from the cones of Liquidamber styraciflua. J. Nat. Prod. 2004, 67, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Rajan, K.; Nelson, A.; Adams, J.P.; Carrier, D.J. Phytochemical recovery for valorization of loblolly pine and sweetgum bark residues. ACS Sustain. Chem. Eng. 2017, 5, 4258–4266. [Google Scholar] [CrossRef]
- Fukuda, Y.; Yamada, T.; Wada, S.I.; Sakai, K.; Matsunaga, S.; Tanaka, R. Lupane and oleanane triterpenoids from the cones of Liquidamber styraciflua. J. Nat. Prod. 2006, 69, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Eid, H.H.; Labib, R.M.; Hamid, N.S.A.; Hamed, M.A.; Ross, S.A. Hepatoprotective and antioxidant polyphenols from a standardized methanolic extract of the leaves of Liquidambar styraciflua L. Bull. Fac. Pharm. Cairo Univ. 2015, 53, 117–127. [Google Scholar] [CrossRef]
- Rashed, K.N.Z.; Sucupira, A.C.C.; Ferreira, P.M.P.; Feitosa, C.M. Phytoconstituents and evaluation of acetylcholinesterase inhibition by methanol extract of Liquidambar styraciflua (L.) aerial parts. J. Appl. Pharm. 2014, 6, 143–152. [Google Scholar] [CrossRef]
- El-Readi, M.Z.; Eid, H.H.; Ashour, M.L.; Eid, S.Y.; Labib, R.M.; Sporer, F.; Wink, M. Variations of the chemical composition and bioactivity of essential oils from leaves and stems of Liquidambar styraciflua (Altingiaceae). J. Pharm. Pharmacol. 2013, 65, 1653–1663. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-L.; Chang, H.-M. Lignans and aporphine alkaloids in bark of Liriodendron tulipifera. Phytochemistry 1978, 17, 779–782. [Google Scholar] [CrossRef]
- Graziose, R.; Rathinasabapathy, T.; Lategan, C.; Poulev, A.; Smith, P.J.; Grace, M.; Lila, M.A.; Raskin, I. Antiplasmodial activity of aporphine alkaloids and sesquiterpene lactones from Liriodendron tulipifera L. J. Ethnopharmacol. 2011, 133, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.-F.; Liu, C.-M.; Kao, C.-L.; Chen, C.-Y. Antioxidant and anticancer constituents from the leaves of Liriodendron tulipifera. Molecules 2014, 19, 4235–4245. [Google Scholar] [CrossRef] [PubMed]
- Doskotch, R.W.; Wilton, J.H.; Harraz, F.M.; Fairchild, E.H.; Huang, C.T.; El-Feraly, F.S. Six additional sesquiterpene lactones from Liriodendron tulipifera. J. Nat. Prod. 1983, 46, 923–929. [Google Scholar] [CrossRef]
- Jeong, E.J.; Kim, N.-H.; Heo, J.-D.; Lee, K.Y.; Rho, J.-R.; Kim, Y.C.; Sung, S.H. Antifibrotic compounds from Liriodendron tulipifera attenuating HSC-T6 proliferation and TNF-α production in RAW264.7 cells. Biol. Pharm. Bull. 2015, 38, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Doskotch, R.W.; El-Feraly, F.S. The structure of tulipinolide and epitulipinolide. Cytotoxic sesquiterpenes from Liriodendron tulipifera L. J. Org. Chem. 1970, 35, 1928–1936. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.L.; Villanueva, H.E.; Palazzo, M.C.; Wright, B.S.; Setzer, W.N. Seasonal variation and bioactivity in the leaf oil of Liriodendron tulipifera growing in Huntsville, Alabama. Nat. Prod. Commun. 2009, 4, 839–843. [Google Scholar] [PubMed]
- Smith, A.L.; Campbell, C.L.; Walker, D.B.; Hanover, J.W.; Miller, R.O. Geographic variation in the essential oil monoterpenes of Liriodendron tulipifera L. Biochem. Syst. Ecol. 1988, 16, 627–630. [Google Scholar] [CrossRef]
- Brown, D.P.; Rogers, D.T.; Pomerleau, F.; Siripurapu, K.B.; Kulshrestha, M.; Gerhardt, G.A.; Littleton, J.M. Novel multifunctional pharmacology of lobinaline, the major alkaloid from Lobelia cardinalis. Fitoterapia 2016, 111, 109–123. [Google Scholar] [CrossRef] [PubMed]
- Yamanaka, M.; Ishibashi, K.; Shimomura, K.; Ishimaru, K. Polyacetylene glucosides in hairy root cultures of Lobelia cardinalis. Phytochemistry 1996, 41, 183–185. [Google Scholar] [CrossRef]
- Vodopivec, B.M.; Wang, J.; Møller, A.L.; Krake, J.; Lund, T.; Hansen, P.E.; Nielsen, S.L. Differences in the structure of anthocyanins from the two amphibious plants, Lobelia cardinalis and Nesaea crassicaulis. Nat. Prod. Res. 2013, 27, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Bálványos, I.; Kursinszki, L.; Bányai, P.; Szöke, É. Analysis of polyacetylenes by HPLC in hairy root cultures of Lobelia inflata cultivated in bioreactor. Chromatographia 2004, 60, S235–S238. [Google Scholar] [CrossRef]
- Kursinszki, L.; Ludányi, K.; Szöke, É. LC-DAD and LC-MS-MS analysis of piperidine alkaloids of Lobelia inflata L. (in vitro and in vivo). Chromatographia 2008, 68, S27–S33. [Google Scholar] [CrossRef]
- Kursinszki, L.; Szöke, É. HPLC-ESI-MS/MS of brain neurotransmitter modulator lobeline and related piperidine alkaloids in Lobelia inflata L. J. Mass Spectrom. 2015, 50, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Resting, J.R.; Tolderlund, I.-L.; Pedersen, A.F.; Witt, M.; Jaroszewski, J.W.; Staerk, D. Piperidine and tetrahydropyridine alkaloids from Lobelia siphilitica and Hippobroma longiflora. J. Nat. Prod. 2009, 72, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Bucar, F.; Kartnig, T. Flavone glucuronides of Lycopus virginicus. Planta Med. 1995, 61, 378–380. [Google Scholar] [CrossRef] [PubMed]
- Doskotch, R.W.; Flom, M.S. Acuminatin, a new bis-phenylpropide from Magnolia acuminata L. Tetrahedron 1972, 28, 4711–4717. [Google Scholar] [CrossRef]
- Flom, M.S. Part I. The Isolation and Characterization of Alkaloids of Caulophyllum thalictroides (L.) Michx. Part II. The Isolation and Characterization of Alkaloid and Neutral Principles of Magnolia acuminata L. Ph.D. Thesis, The Ohio State University, Columbus, OH, USA, 1971. [Google Scholar]
- Furmanowa, M.; Jozefowicz, J. Alkaloids as taxonomic markers in some species of Magnolia L. and Liriodendron L. Acta Soc. Bot. Pol. 1980, 49, 527–535. [Google Scholar] [CrossRef]
- Manske, R.H.F. An alkaloid from Menispermum canadense L. Can. J. Res. 1943, 21b, 17–20. [Google Scholar] [CrossRef]
- Knapp, J.E. The Isolation and Chemical Characterization of Alkaloids from Menispermum canadense L. Ph.D. Thesis, The Ohio State University, Columbus, OH, USA, 1969. [Google Scholar]
- Carnat, A.P.; Lamaison, J.L.; Rémery, A. Composition of leaf and flower essential oil from Monarda didyma L. cultivated in France. Flavour Fragr. J. 1991, 6, 79–80. [Google Scholar] [CrossRef]
- Tognolini, M.; Barocelli, E.; Ballabeni, V.; Bruni, R.; Bianchi, A.; Chiavarini, M.; Impicciatore, M. Comparative screening of plant essential oils: Phenylpropanoid moiety as basic core for antiplatelet activity. Life Sci. 2006, 78, 1419–1432. [Google Scholar] [CrossRef] [PubMed]
- Fraternale, D.; Giamperi, L.; Bucchini, A.; Ricci, D.; Epifano, F.; Burini, G.; Curini, M. Chemical composition, antifungal and in vitro antioxidant properties of Monarda didyma L. essential oil. J. Essent. Oil Res. 2006, 18, 581–585. [Google Scholar] [CrossRef]
- Gwinn, K.D.; Ownley, B.H.; Greene, S.E.; Clark, M.M.; Taylor, C.L.; Springfield, T.N.; Trently, D.J.; Green, J.F.; Reed, A.; Hamilton, S.L. Role of essential oils in control of Rhizoctonia damping-off in tomato with bioactive Monarda herbage. Phytopathology 2010, 100, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Adebayo, O.; Bélanger, A.; Khanizadeh, S. Variable inhibitory activities of essential oils of three Monarda species on the growth of Botrytis cinerea. Can. J. Plant Sci. 2013, 93, 987–995. [Google Scholar] [CrossRef]
- Mattarelli, P.; Epifano, F.; Minardi, P.; Di Vito, M.; Modesto, M.; Barbanti, L.; Bellardi, M.G. Chemical composition and antimicrobial activity of essential oils from aerial parts of Monarda didyma and Monarda fistulosa cultivated in Italy. J. Essent. Oil-Bear. Plants 2017, 20, 76–86. [Google Scholar] [CrossRef]
- Ricci, D.; Epifano, F.; Fraternale, D. The essential oil of Monarda didyma L. (Lamiaceae) exerts phytotoxic activity in vitro against various weed seeds. Molecules 2017, 22, 222. [Google Scholar] [CrossRef] [PubMed]
- Savickienė, N.; Dagilytė, A.; Barsteigienė, Z.; Kazlauskas, S.; Vaičiūnienė, J. Flavonoidų analizė raudonosios monardos (Monarda didyma L.) žieduose ir lapuose. Medicina 2002, 38, 1119–1122. [Google Scholar] [PubMed]
- Mazza, G.; Chubey, B.B.; Kiehn, F. Essential oil of Monarda fistulosa L. var. menthaefolia, a potential source of geraniol. Flavour Fragr. J. 1987, 2, 129–132. [Google Scholar] [CrossRef]
- Contaldo, N.; Bellardi, M.G.; Cavicchi, L.; Epifano, F.; Genovese, S.; Curini, M.; Bertaccini, A. Phytochemical effects of phytoplasma infections on essential oil of Monarda fistulosa L. Bull. Insectol. 2011, 64, S177–S178. [Google Scholar]
- Tabanca, N.; Bernier, U.R.; Ali, A.; Wang, M.; Demirci, B.; Blythe, E.K.; Khan, S.I.; Baser, K.H.C.; Khan, I.A. Bioassay-guided investigation of two Monarda essential oils as repellents of yellow fever mosquito Aedes aegypti. J. Agric. Food Chem. 2013, 61, 8573–8580. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Ali, M.; Tandon, S. New oenotheralanosterol A and B: Constituents from the Oenothera biennis roots. Chin. J. Chem. 2010, 28, 2474–2478. [Google Scholar] [CrossRef]
- Singh, R.; Trivedi, P.; Bawankule, D.U.; Ahmad, A.; Shanker, K. HILIC quantification of oenotheralanosterol A and B from Oenothera biennis and their suppression of IL-6 and TNF-α expression in mouse macrophages. J. Ethnopharmacol. 2012, 141, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Shukla, Y.N.; Srivastava, A.; Kumar, S.; Kumar, S. Phytotoxic and antimicrobial constituents of Argyreia speciosa and Oenothera biennis. J. Ethnopharmacol. 1999, 67, 241–245. [Google Scholar] [CrossRef]
- Ahmad, A.; Singh, D.K.; Fatima, K.; Tandon, S.; Luqman, S. New constituents from the roots of Oenothera biennis and their free radical scavenging and ferric reducing activity. Ind. Crops Prod. 2014, 58, 125–132. [Google Scholar] [CrossRef]
- Shukla, Y.N.; Srivastava, A.; Kumar, S. Aryl, lipid and triterpenoid constituents from Oenothera biennis. Indian J. Chem. 1999, 38, 705–708. [Google Scholar]
- Montserrat-de la Paz, S.; Fernández-Arche, M.A.; Ángel-Martín, M.; García-Giménez, M.D. Phytochemical characterization of potential nutraceutical ingredients from evening primrose oil (Oenothera biennis L.). Phytochem. Lett. 2014, 8, 158–162. [Google Scholar] [CrossRef]
- Wettasinghe, M.; Shahidi, F.; Amarowicz, R. Identification and quantification of low molecular weight phenolic antioxidants in seeds of evening primrose (Oenothera biennis L.). J. Agric. Food Chem. 2002, 50, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Zadernowski, R.; Naczk, M.; Nowak-Polakowska, H. Phenolic acids of borage (Borago officinalis L.) and evening primrose (Oenothera biennis L.). J. Am. Oil Chem. Soc. 2002, 79, 335–338. [Google Scholar] [CrossRef]
- Granica, S.; Czerwińska, M.E.; Piwowarski, J.P.; Ziaja, M.; Kiss, A.K. Chemical composition, antioxidative and anti-inflammatory activity of extracts prepared from aerial parts of Oenothera biennis L. and Oenothera paradoxa Hudziok obtained after seeds cultivation. J. Agric. Food Chem. 2013, 61, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Assinewe, V.A.; Baum, B.R.; Gagnon, D.; Arnason, J.T. Phytochemistry of wild populations of Panax quinquefolius L. (North American ginseng). J. Agric. Food Chem. 2003, 51, 4549–4553. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Wang, C.Z.; Wu, J.A.; Osinski, J.; Yuan, C.S. Determination of major ginsenosides in Panax quinquefolius (American ginseng) using high-performance liquid chromatography. Phytochem. Anal. 2005, 16, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Corbit, R.M.; Ferreira, J.F.S.; Ebbs, S.D.; Murphy, L.L. Simplified extraction of ginsenosides from American ginseng (Panax quinquefolius L.) for high-performance liquid chromatography-ultraviolet analysis. J. Agric. Food Chem. 2005, 53, 9867–9873. [Google Scholar] [CrossRef] [PubMed]
- Qu, C.; Bai, Y.; Jin, X.; Wang, Y.; Zhang, K.; You, J.; Zhang, H. Study on ginsenosides in different parts and ages of Panax quinquefolius L. Food Chem. 2009, 115, 340–346. [Google Scholar] [CrossRef]
- Christensen, L.P.; Jensen, M.; Kidmose, U. Simultaneous determination of ginsenosides and polyacetylenes in American ginseng root (Panax quinquefolium L.) by high-performance liquid chromatography. J. Agric. Food Chem. 2006, 54, 8995–9003. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-Z.; Aung, H.H.; Ni, M.; Wu, J.-A.; Tong, R.; Wicks, S.; He, T.-C.; Yuan, C.-S. Red American ginseng: Ginsenoside constituents and antiproliferative activities of heat-processed Panax quinquefolius roots. Planta Med. 2007, 73, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Choi, H.-K.; Brinckmann, J.A.; Jiang, X.; Huang, L. Chemical analysis of Panax quinquefolius (North American ginseng): A review. J. Chromatogr. A 2015, 1426, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, C.; Santangelo, R. Panax ginseng and Panax quinquefolius: From pharmacology to toxicology. Food Chem. Toxicol. 2017, 107, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.-Z.; Hu, Y.; Wu, W.-Y.; Ye, M.; Guo, D.-A. Saponins in the genus Panax L. (Araliaceae): A systematic review of their chemical diversity. Phytochemistry 2014, 106, 7–24. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.-S.; Wang, C.-Z.; Wicks, S.M.; Qi, L.-W. Chemical and pharmacological studies of saponins with a focus on American ginseng. J. Ginseng Res. 2010, 34, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.M.; Der Marderosian, A.H. Studies on the constituents of dwarf ginseng. Phyther. Res. 1988, 2, 165–169. [Google Scholar] [CrossRef]
- Lui, J.H.-C.; Staba, E.J. The ginsenosides of various ginseng plants and selected products. J. Nat. Prod. 1980, 43, 340–346. [Google Scholar] [CrossRef]
- Tanaka, T.; Iinuma, M.; Murata, H. Stilbene derivatives in the stem of Parthenocissus quinquefolia. Phytochemistry 1998, 48, 1045–1049. [Google Scholar] [CrossRef]
- Yang, J.B.; Wang, A.G.; Ji, T.F.; Su, Y.L. Two new oligostilbenes from the stem of Parthenocissus quinquefolia. J. Asian Nat. Prod. Res. 2014, 16, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Chistokhodova, N.A.; Zhiviriga, I.; Nguen, C.; Miles, G.D.; Uzhegova, N.A.; Solodnikov, S.Y. β-Amyrylhexadecanoate from Parthenocissus quinquefolia as a thrombin inhibitor. Pharm. Chem. J. 2002, 36, 245–247. [Google Scholar] [CrossRef]
- Li, Q.; van den Heuvel, H.; Delorenzo, O.; Corthout, J.; Pieters, L.A.C.; Vlietinck, A.J.; Claeys, M. Mass spectral characterization of C-glycosidic flavonoids isolated from a medicinal plant (Passiflora incarnata). J. Chromatogr. B 1991, 562, 435–446. [Google Scholar]
- Raffaelli, A.; Moneti, G.; Mercati, V.; Toja, E. Mass spectrometric characterization of flavonoids in extracts from Passiflora incarnata. J. Chromatogr. A 1997, 777, 223–231. [Google Scholar] [CrossRef]
- Rahman, K.; Krenn, L.; Kopp, B.; Schubert-Zsilavecz, M.; Mayer, K.K.; Kubelka, W. Isoscoparin-2″-O-glucoside from Passiflora incarnata. Phytochemistry 1997, 45, 1093–1094. [Google Scholar] [CrossRef]
- Chimichi, S.; Mercati, V.; Moneti, G.; Raffaelli, A.; Toja, E. Isolation and characterization of an unknown flavonoid in dry extracts from Passiflora incarnata. Nat. Prod. Lett. 1998, 11, 225–232. [Google Scholar] [CrossRef]
- Dhawan, K.; Dhawan, S.; Sharma, A. Passiflora: A review update. J. Ethnopharmacol. 2004, 94, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Woo, W.S.; Kang, S.S.; Wagner, H.; Seligmann, O.; Chari, V.M. Triterpenoid saponins from the roots of Phytolacca americana. Planta Med. 1978, 34, 87–92. [Google Scholar] [CrossRef]
- Woo, W.S.; Kang, S.S. Phytolaccoside B: Triterpene glucoside from Phytolacca americana. Phytochemistry 1976, 15, 1315–1317. [Google Scholar] [CrossRef]
- Suga, Y.; Maruyama, Y.; Kawanishi, S.; Shoji, J. Studies on the constituents of phytolaccaceous plants. I. On the structures of phytolaccasaponin B, E and G from the roots of Phytolacca americana L. Chem. Pharm. Bull. 1978, 25, 520–525. [Google Scholar] [CrossRef]
- Wang, L.; Bai, L.; Nagasawa, T.; Hasegawa, T.; Yang, X.; Sakai, J.-I.; Bai, Y.; Kataoka, T.; Oka, S.; Hirose, K.; et al. Bioactive triterpene saponins from the roots of Phytolacca americana. J. Nat. Prod. 2008, 71, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Seung, I.J.; Kang, J.K.; Min, K.C.; Kyung, S.K.; Lee, S.; Seon, H.A.; Seung, H.B.; Ju, H.S.; Young, S.J.; Bong, K.C.; et al. α-Spinasterol isolated from the root of Phytolacca americana and its pharmacological property on diabetic nephropathy. Planta Med. 2004, 70, 736–739. [Google Scholar]
- Fleer, H.; Verspohl, E.J. Antispasmodic activity of an extract from Plantago lanceolata L. and some isolated compounds. Phytomedicine 2007, 14, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Beara, I.N.; Lesjak, M.M.; Orčić, D.Z.; Simin, N.D.; Četojević-Simin, D.D.; Božin, B.N.; Mimica-Dukić, N.M. Comparative analysis of phenolic profile, antioxidant, anti-inflammatory and cytotoxic activity of two closely-related plantain species: Plantago altissima L. and Plantago lanceolata L. LWT Food Sci. Technol. 2012, 47, 64–70. [Google Scholar] [CrossRef]
- Darrow, K.; Bowers, M.D. Phenological and population variation in iridoid glycosides of Plantago lanceolata (Plantaginaceae). Biochem. Syst. Ecol. 1997, 25, 1–11. [Google Scholar] [CrossRef]
- Marak, H.B.; Biere, A.; Van Damme, J.M.M. Direct and correlated responses to selection on iridoid glycosides in Plantago lanceolata L. J. Evol. Biol. 2000, 13, 985–996. [Google Scholar] [CrossRef]
- Gonda, S.; Tóth, L.; Gyémánt, G.; Braun, M.; Emri, T.; Vasas, G. Effect of high relative humidity on dried Plantago lanceolata L. leaves during long-term storage: Effects on chemical composition, colour and microbiological quality. Phytochem. Anal. 2012, 23, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Gonda, S.; Kiss, A.; Emri, T.; Batta, G.; Vasas, G. Filamentous fungi from Plantago lanceolata L. leaves: Contribution to the pattern and stability of bioactive metabolites. Phytochemistry 2013, 86, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Rønsted, N.; Göbel, E.; Franzyk, H.; Jensen, S.R.; Olsen, C.E. Chemotaxonomy of Plantago. Iridoid glucosides and caffeoyl phenylethanoid glycosides. Phytochemistry 2000, 55, 337–348. [Google Scholar] [CrossRef]
- Samuelsen, A.B. The traditional uses, chemical constituents and biological activities of Plantago major L. A review. J. Ethnopharmacol. 2000, 71, 1–21. [Google Scholar] [CrossRef]
- Chiang, L.C.; Chiang, W.; Chang, M.Y.; Ng, L.T.; Lin, C.C. Antiviral activity of Plantago major extracts and related compounds in vitro. Antiv. Res. 2002, 55, 53–62. [Google Scholar] [CrossRef]
- Zacchigna, M.; Cateni, F.; Faudale, M.; Sosa, S.; Della Loggia, R. Rapid HPLC analysis for quantitative determination of the two isomeric triterpenic acids, oleanolic acid and ursolic acid, in Plantago major. Sci. Pharm. 2009, 77, 79–86. [Google Scholar] [CrossRef]
- Tarvainen, M.; Suomela, J.-P.; Kallio, H.; Yang, B. Triterpene acids in Plantago major: Identification, quantification and comparison of different extraction methods. Chromatographia 2010, 71, 279–284. [Google Scholar] [CrossRef]
- Kolak, U.; Boǧa, M.; Uruşak, E.A.; Ulubelen, A. Constituents of Plantago major subsp. intermedia with antioxidant and anticholinesterase capacities. Turk. J. Chem. 2011, 35, 637–645. [Google Scholar]
- Kartini, P.S.; Siripong, P.; Vallisuta, O. HPTLC simultaneous quantification of triterpene acids for quality control of Plantago major L. and evaluation of their cytotoxic and antioxidant activities. Ind. Crops Prod. 2014, 60, 239–246. [Google Scholar] [CrossRef]
- Stenholm, Å.; Göransson, U.; Bohlin, L. Bioassay-guided supercritical fluid extraction of cyclooxygenase-2 inhibiting substances in Plantago major L. Phytochem. Anal. 2013, 24, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.A.; Mansoor, A.A.; Gross, A.; Ashfaq, M.K.; Jacob, M.; Khan, S.I.; Hamann, M.T. Methicillin-resistant Staphylococcus aureus (MRSA)-active metabolites from Platanus occidentalis (American sycamore). J. Nat. Prod. 2009, 72, 2141–2144. [Google Scholar] [CrossRef] [PubMed]
- Bedows, E.; Hatfield, G.M. An investigation of the antiviral activity of Podophyllum peltatum. J. Nat. Prod. 1982, 45, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.E.; Dewick, P.M. Aryltetralin lignans from Podophyllum hexandrum and Podophyllum peltatum. Phytochemistry 1984, 23, 1147–1152. [Google Scholar] [CrossRef]
- Bastos, J.K.; Burandt, C.L.; Nanayakkara, N.P.D.; Bryant, L.; McChesney, J.D. Quantitation of aryltetralin lignans in plant parts and among different populations of Podophyllum peltatum by reversed-phase high-performance liquid chromatography. J. Nat. Prod. 1996, 59, 406–408. [Google Scholar] [CrossRef]
- Tsukitani, Y.; Kawanishi, S.; Shoji, J. Studies on the constituents of Senegae Radix. II. The structure of senegin-II, a saponin from Polygala senega latifolia Torry et Gray. Chem. Pharm. Bull. 1973, 21, 791–799. [Google Scholar] [CrossRef]
- Tsukitani, Y.; Shoji, J. Studies on the constituents of Senegae Radix. III. The structures of senegin-III and -IV, saponins from Polygala senega Linne var. latifolia Torry et Gray. Chem. Pharm. Bull. 1973, 21, 1564–1574. [Google Scholar] [CrossRef]
- Saitoh, H.; Miyase, T.; Ueno, A. Senegoses A-E, oligosaccharide multi-esters from Polygala senega var. latifolia Torr. et Gray. Chem. Pharm. Bull. 1993, 41, 1127–1131. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, H.; Miyase, T.; Ueno, A. Senegoses F-I, oligosaccharide multi-esters from the roots of Polygala senega var. latifolia Torr. et Gray. Chem. Pharm. Bull. 1993, 41, 2125–2128. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, H.; Miyase, T.; Ueno, A.; Atarashi, K.; Saiki, Y. Senegoses J-O, oligosaccharide multi-esters from the roots of Polygala senega L. Chem. Pharm. Bull. 1994, 43, 641–645. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Murakami, T.; Ueno, T.; Kadoya, M.; Matsuda, H.; Yamahara, J.; Murakami, N. E-Senegasaponins A and B, Z-senegasaponins A and B, Z-senegins II and III, new type inhibitors of ethanol absorption in rats from Senegae Radix, the roots of Polygala senega L. var latifolia Torrey et Gray. Chem. Pharm. Bull. 1995, 43, 350–352. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Kameoka, H. Volatile compounds of Polygala senega L. var. latifolia Torrey et Gray. Flavour Fragr. J. 1995, 10, 273–280. [Google Scholar] [CrossRef]
- Arai, M.; Hayashi, A.; Sobou, M.; Ishida, S.; Kawachi, T.; Kotoku, N.; Kobayashi, M. Anti-angiogenic effect of triterpenoidal saponins from Polygala senega. J. Nat. Med. 2011, 65, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Woo, E.-R.; Park, H. A novel lignan and flavonoids from Polygonum aviculare. J. Nat. Prod. 1994, 57, 581–586. [Google Scholar] [CrossRef]
- Al-Hazimi, H.M.A.; Haque, S.N. A new naphthoquinone from Polygonum aviculare. Nat. Prod. Lett. 2002, 16, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Yunuskhodzhaeva, N.A.; Eshbakova, K.A.; Abdullabekova, V.N. Flavonoid composition of the herb Polygonum aviculare. Chem. Nat. Compd. 2010, 46, 803–804. [Google Scholar] [CrossRef]
- Granica, S.; Czerwińska, M.E.; Zyzyńska-Granica, B.; Kiss, A.K. Antioxidant and anti-inflammatory flavonol glucuronides from Polygonum aviculare L. Fitoterapia 2013, 91, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Nugroho, A.; Kim, E.J.; Choi, J.S.; Park, H.-J. Simultaneous quantification and peroxynitrite-scavenging activities of flavonoids in Polygonum aviculare L. herb. J. Pharm. Biomed. Anal. 2014, 89, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.H.; Hwangbo, K.; Zheng, M.S.; Cho, J.H.; Son, J.-K.; Kim, H.Y.; Baek, S.H.; Choi, H.C.; Park, S.Y.; Kim, J.-R. Quercetin-3-O-β-d-glucuronide isolated from Polygonum aviculare inhibits cellular senescence in human primary cells. Arch. Pharm. Res. 2014, 37, 1219–1233. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.S.; Loder, J.W. The structure of polygodial: A new sesquiterpene dialdehyde from Polygonum hydropiper L. Aust. J. Chem. 1962, 15, 322–327. [Google Scholar] [CrossRef]
- Fukuyama, Y.; Sato, T.; Asakawa, Y.; Takemoto, T. A potent cytotoxic warburganal and related drimane-type sesquiterpenoids from Polygonum hydropiper. Phytochemistry 1980, 21, 2895–2898. [Google Scholar] [CrossRef]
- Yang, X.; Wang, B.-C.; Zhang, X.; Yang, S.-P.; Li, W.; Tang, Q.; Singh, G.K. Simultaneous determination of nine flavonoids in Polygonum hydropiper L. samples using nanomagnetic powder three-phase hollow fibre-based liquid-phase microextraction combined with ultrahigh performance liquid chromatography-mass spectrometry. J. Pharm. Biomed. Anal. 2011, 54, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Fukuyama, Y.; Sato, T.; Miura, I.; Asakawa, Y. Drimane-type sesqui- and norsesquiterpenoids from Polygonum hydropiper. Phytochemistry 1985, 24, 1521–1524. [Google Scholar] [CrossRef]
- Haraguchi, H.; Hashimoto, K.; Yagi, A. Antioxidative substances in leaves of Polygonum hydropiper. J. Agric. Food Chem. 1992, 40, 1349–1351. [Google Scholar] [CrossRef]
- Yagi, A.; Uemura, T.; Okamura, N.; Haraguchi, H.; Imoto, T.; Hashimoto, K. Antioxidative sulphated flavonoids in leaves of Polygonum hydropiper. Phytochemistry 1994, 35, 885–887. [Google Scholar] [CrossRef]
- Peng, Z.F.; Strack, D.; Baumert, A.; Subramaniam, R.; Goh, N.K.; Chia, T.F.; Tan, S.N.; Chia, L.S. Antioxidant flavonoids from leaves of Polygonum hydropiper L. Phytochemistry 2003, 62, 219–228. [Google Scholar] [CrossRef]
- Haraguchi, H.; Matsuda, R.; Hashimoto, K. High-performance liquid chromatographic determination of sesquiterpene dialdehydes and antifungal activity from Polygonum hydropiper. J. Agric. Food Chem. 1993, 41, 5–7. [Google Scholar] [CrossRef]
- Miyazawa, M.; Tamura, N. Inhibitory compound of tyrosinase activity from the sprout of Polygonum hydropiper L. (Benitade). Biol. Pharm. Bull. 2007, 30, 595–597. [Google Scholar] [CrossRef] [PubMed]
- Van Kiem, P.; Nhiem, N.X.; Cuong, N.X.; Hoa, T.Q.; Huong, H.T.; Huong, L.M.; Van Minh, C.; Kim, Y.H. New phenylpropanoid esters of sucrose from Polygonum hydropiper and their antioxidant activity. Arch. Pharm. Res. 2008, 31, 1477–1482. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, M.; Tamura, N. Components of the essential oil from sprouts of Polygonum hydropiper L. (‘Benitade’). Flavour Fragr. J. 2007, 22, 188–190. [Google Scholar] [CrossRef]
- Maheswaran, R.; Ignacimuthu, S. Bioefficacy of essential oil from Polygonum hydropiper L. against mosquitoes, Anopheles stephensi and Culex quinquefasciatus. Ecotoxicol. Environ. Saf. 2013, 97, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Morteza-Semnani, K.; Saeedi, M.; Akbarzadeh, M. The essential oil composition of Prunella vulgaris L. J. Essent. Oil Bear. Plants 2006, 9, 257–260. [Google Scholar] [CrossRef]
- Chen, Y.; Guo, Q.; Zhu, Z.; Zhang, L.; Dai, X. Comparative analysis of the essential oil of flowers, leaves and stems of Prunella vulgaris L. J. Essent. Oil Bear. Plants 2012, 15, 662–666. [Google Scholar] [CrossRef]
- Chen, Y.; Zhu, Z.; Guo, Q.; Zhang, L.; Zhang, X. Variation in concentrations of major bioactive compounds in Prunella vulgaris L. related to plant parts and phenological stages. Biol. Res. 2012, 45, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yu, M.; Zhu, Z.; Zhang, L.; Guo, Q. Optimisation of potassium chloride nutrition for proper growth, physiological development and bioactive component production in Prunella vulgaris L. PLoS ONE 2013, 8, e66259. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.Y.; Oak, M.-H.; Yoon, S.-K.; Cho, D.-I.; Yoo, G.-S.; Kim, T.-S.; Kim, K.-M. Anti-allergic and anti-inflammatory triterpenes from the herb of Prunella vulgaris. Planta Med. 2000, 66, 358–360. [Google Scholar] [CrossRef] [PubMed]
- Yoon, M.Y.; Choi, G.J.; Choi, Y.H.; Jang, K.S.; Park, M.S.; Cha, B.; Kim, J.C. Effect of polyacetylenic acids from Prunella vulgaris on various plant pathogens. Lett. Appl. Microbiol. 2010, 51, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.-J.; Li, Y.-B.; Li, P.; Qian, S.-H.; Zhang, J.-F. Triterpenoid saponins from the spikes of Prunella vulgaris. Helv. Chim. Acta 2007, 90, 72–78. [Google Scholar] [CrossRef]
- Lee, I.K.; Kim, D.H.; Lee, S.Y.; Kim, K.R.; Choi, S.U.; Hong, J.K.; Lee, J.H.; Park, Y.H.; Lee, K.R. Triterpenoic acids of Prunella vulgaris var. lilacina and their cytotoxic activities in vitro. Arch. Pharm. Res. 2008, 31, 1578–1583. [Google Scholar] [PubMed]
- Wang, Z.J.; Zhao, Y.Y.; Wang, B.; Ai, T.M.; Chen, Y.Y. Depsides from Prunella vulgaris. Chin. Chem. Lett. 2000, 11, 997–1001. [Google Scholar]
- Şahin, S.; Demir, C.; Malyer, H. Determination of phenolic compounds in Prunella L. by liquid chromatography-diode array detection. J. Pharm. Biomed. Anal. 2011, 55, 1227–1230. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Li, Y.; Mu, J.; Zhang, Y. Chemical constituents of Prunella vulgaris. J. Environ. Sci. 2013, 25, S161–S163. [Google Scholar] [CrossRef]
- Olszewska, M. Flavonoids from Prunus serotina Ehrh. Acta Pol. Pharm. Drug Res. 2005, 62, 127–133. [Google Scholar]
- Olszewska, M. Quantitative HPLC analysis of flavonoids and chlorogenic acid in the leaves and inflorescences of Prunus serotina Ehrh. Acta Chromatogr. 2007, 19, 253–269. [Google Scholar]
- Olszewska, M. Optimization and validation of an HPLC-UV method for analysis of corosolic, oleanolic, and ursolic acids in plant material: Application to Prunus serotina Ehrh. Acta Chromatogr. 2008, 20, 643–659. [Google Scholar] [CrossRef]
- Ibarra-Alvarado, C.; Rojas, A.; Luna, F.; Rojas, J.I.; Rivero-Cruz, B.; Rivero-Cruz, J.F. Vasorelaxant constituents of the leaves of Prunus serotina “capulín”. Rev. Latinoam. Quim. 2009, 37, 164–173. [Google Scholar]
- Rivero-Cruz, B. Simultaneous quantification by HPLC of the phenolic compounds for the crude drug of Prunus serotina subsp. capuli. Pharm. Biol. 2014, 52, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Biessels, H.W.A.; van der Kerk-van Hoof, A.C.; Kettenes-van den Bosch, J.J.; Salemink, C.A. Triterpenes of Prunus serotina and P. lusitanica. Phytochemistry 1974, 13, 203–207. [Google Scholar] [CrossRef]
- Omar, S.; Lalonde, M.; Marcotte, M.; Cook, M.; Proulx, J.; Goel, K.; Durst, T.; Philogène, B.J.R.; Arnason, J.T. Insect growth-reducing and antifeedant activity in eastern North America hardwood species and bioassay-guided isolation of active principles from Prunus serotina. Agric. For. Entomol. 2000, 2, 253–257. [Google Scholar] [CrossRef]
- Hänsel, R.; Ohlendorf, D.; Pelter, A. Obtusifolin, ein Flavanon mit einem biogenetisch unüblichen C9-Baustein. Z. Naturforsch. B 1970, 25, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.; Maurer, G.; Farkas, L.; Hänsel, R.; Ohlendorf, D. Zur Struktur und Synthese von Gnaphaliin, Methyl-gnaphaliin aus Gnaphalium obtusifolium L. und Isognaphaliin aus Achrocline satureoides. Chem. Ber. 1971, 104, 1281–1288. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Schwarz, R.; Hänsel, R. 3,5,7-Trihydroxy-6,8-dimethoxyflavon aus Gnaphalium obtusifolium. Arch. Pharm. 1971, 304, 213–215. [Google Scholar] [CrossRef]
- Murata, T.; Nakano, M.; Miyase, T.; Yoshizaki, F. Chemical constituents of aerial parts and roots of Pycnanthemum flexuosum. Chem. Pharm. Bull. 2014, 62, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Beebe, C.W.; Luvisi, F.P.; Happich, M.L. Tennessee Valley oak bark as a source of tannin. J. Am. Leather Chem. Assoc. 1953, 48, 32–41. [Google Scholar]
- Bai, Y.; Benn, M.H.; Majak, W.; McDiarmid, R. Extraction and HPLC determination of ranunculin in species of the buttercup family. J. Agric. Food Chem. 1996, 44, 2235–2238. [Google Scholar] [CrossRef]
- Mekala, A.B.; Satyal, P.; Setzer, W.N. Phytochemicals from the bark of Rhamnus caroliniana. Nat. Prod. Commun. 2017, 12, 403–406. [Google Scholar]
- Saxena, G.; McCutcheon, A.R.; Farmer, S.; Towers, G.H.N.; Hancock, R.E.W. Antimicrobial constituents of Rhus glabra. J. Ethnopharmacol. 1994, 42, 95–99. [Google Scholar] [CrossRef]
- Heckman, R.A. The Isolation and Identification of Organic Compounds from Rhus glabra. Ph.D. Thesis, Georgia Institute of Technology, Atlanta, GA, USA, 1965. [Google Scholar]
- Wu, T.; McCallum, J.L.; Wang, S.; Liu, R.; Zhu, H.; Tsao, R. Evaluation of antioxidant activities and chemical characterisation of staghorn sumac fruit (Rhus hirta L.). Food Chem. 2013, 138, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Zhang, H.; Liu, R.; Mine, Y.; McCallum, J.; Kirby, C.; Tsao, R. Antioxidant and anti-inflammatory activities of pyranoanthocyanins and other polyphenols from staghorn sumac (Rhus hirta L.) in Caco-2 cell models. J. Funct. Foods 2016, 20, 139–147. [Google Scholar] [CrossRef]
- Van Damme, E.J.M.; Barre, A.; Smeets, K.; Torrekens, S.; Van Leuven, F.; Rougé, P.; Peumans, W.J. The bark of Robinia pseudoacacia contains a complex mixture of lectins. Characterization of the proteins and the cDNA clones. Plant Physiol. 1995, 107, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Rabijns, A.; Verboven, C.; Rougé, P.; Barre, A.; Van Damme, E.J.M.; Peumans, W.J.; De Ranter, C.J. Structure of a legume lectin from the bark of Robinia pseudoacacia and its complex with N-acetylgalactosamine. Proteins Struct. Funct. Genet. 2001, 44, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; McLaughlin, J.L. Bioactive flavonoids from the black locust tree, Robinia pseudoacacia. Pharm. Biol. 2000, 38, 229–234. [Google Scholar] [CrossRef]
- Veitch, N.C.; Elliott, P.C.; Kite, G.C.; Lewis, G.P. Flavonoid glycosides of the black locust tree, Robinia pseudoacacia (Leguminosae). Phytochemistry 2010, 71, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Duverger, E.; Delmotte, F.M. Purification of lectins from Robinia pseudoacacia L. root-tips. Plant Sci. 1997, 123, 9–18. [Google Scholar] [CrossRef]
- Ono, M.; Yasuda, S.; Komatsu, H.; Fujiwara, Y.; Takeya, M.; Nohara, T. Triterpenoids from the fruits and leaves of the blackberry (Rubus allegheniensis) and their inhibitory activities on foam cell formation in human monocyte-derived macrophage. Nat. Prod. Res. 2014, 28, 2347–2350. [Google Scholar] [CrossRef] [PubMed]
- Dvaranauskaite, A.; Venskutonis, P.R.; Labokas, J. Comparison of quercetin derivatives in ethanolic extracts of red raspberry (Rubus idaeus L.) leaves. Acta Aliment. 2008, 37, 449–461. [Google Scholar] [CrossRef]
- Vera, J.R.; Dacke, C.G.; Blunden, G.; Patel, A.V. Smooth muscle relaxant triterpenoid glycosides from Rubus idaeus (raspberry) leaves. Nat. Prod. Commun. 2006, 1, 705–710. [Google Scholar]
- Ferlemi, A.-V.; Lamari, F.N. Berry leaves: An alternative source of bioactive natural products of nutritional and medicinal value. Antioxidants 2016, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.D.; Jones, C.D.; Setzer, W.N. Leaf essential oil compositions of Rudbeckia fulgida Aiton, Rudbeckia hirta L., and Symphyotrichum novae-angliae (L.) G.L. Nesom (Asteraceae). Am. J. Essent. Oils Nat. Prod. 2014, 2, 36–38. [Google Scholar]
- Lee, S.Y.; Woo, K.W.; Kim, C.S.; Lee, D.U.; Lee, K.R. New lignans from the aerial parts of Rudbeckia laciniata. Helv. Chim. Acta 2013, 96, 320–325. [Google Scholar] [CrossRef]
- Lee, S.Y.; Shin, Y.J.; Choi, S.U.; Lee, K.R. A new flavonol glycoside from the aerial part of Rudbeckia laciniata. Arch. Pharm. Res. 2014, 37, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Bohlmann, F.; Jakupovic, J.; Zdero, C. Neue Norsesquiterpene aus Rudbeckia laciniata und Senecio paludaffinis. Phytochemistry 1978, 17, 2034–2036. [Google Scholar] [CrossRef]
- Jakupovic, J.; Jia, Y.; King, R.M.; Bohlmann, F. Rudbeckiolid, ein dimeres Sesquiterpenlacton aus Rudbeckia laciniata. Justus Liebigs Ann. Chem. 1986, 8, 1474–1477. [Google Scholar] [CrossRef]
- Fukushi, Y.; Yajima, C.; Mizutani, J.; Tahara, S. Tricyclic sesquiterpenes from Rudbeckia laciniata. Phytochemistry 1998, 49, 593–600. [Google Scholar] [CrossRef]
- Sando, C.E.; Lloyd, J.U. The isolation and identification of rutin from the flowers of elder (Sambucus canadensis L.). J. Biol. Chem. 1924, 58, 737–745. [Google Scholar]
- Inami, O.; Tamura, I.; Kikuzaki, H.; Nakatani, N. Stability of anthocyanins of Sambucus canadensis and Sambucus nigra. J. Agric. Food Chem. 1996, 44, 3090–3096. [Google Scholar] [CrossRef]
- Lee, J.; Finn, C.E. Anthocyanins and other polyphenolics in American elderberry (Sambucus canadensis) and European elderberry (S. nigra) cultivars. J. Sci. Food Agric. 2007, 87, 2665–2675. [Google Scholar] [CrossRef] [PubMed]
- Nakatani, N.; Kikuzaki, H.; Hikida, J.; Ohba, M.; Inami, O.; Tamura, I. Acylated anthocyanins from fruits of Sambucus canadensis. Phytochemistry 2013, 38, 755–757. [Google Scholar] [CrossRef]
- Greathouse, G.A. Alkaloids from Sanguinaria canadensis and their influence on growth of Phymatotrichum omnivorum. Plant Physiol. 1939, 14, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Salmore, A.K.; Hunter, M.D. Environmental and genotypic influences on isoquinoline alkaloid content in Sanguinaria canadensis. J. Chem. Ecol. 2001, 27, 1729–1747. [Google Scholar] [CrossRef] [PubMed]
- Newton, S.M.; Lau, C.; Gurcha, S.S.; Besra, G.S.; Wright, C.W. The evaluation of forty-three plant species for in vitro antimycobacterial activities; isolation of active constituents from Psoralea corylifolia and Sanguinaria canadensis. J. Ethnopharmacol. 2002, 79, 57–67. [Google Scholar] [CrossRef]
- Mahady, G.B.; Pendland, S.L.; Stoia, A.; Chadwick, L.R. In vitro susceptibility of Helicobacter pylori to isoquinoline alkaloids from Sanguinaria canadensis and Hydrastis canadensis. Phyther. Res. 2003, 17, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.N.; Levine, K.E.; Andrews, M.E.; Perlmutter, J.M.; Nielsen, S.J.; Davis, J.M.; Wani, M.C.; Oberlies, N.H. Variability in the yield of benzophenanthridine alkaloids in wildcrafted vs. cultivated bloodroot (Sanguinaria canadensis L.). J. Agric. Food Chem. 2007, 55, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Croaker, A.; King, G.J.; Pyne, J.H.; Anoopkumar-Dukie, S.; Liu, L. Sanguinaria canadensis: Traditional medicine, phytochemical composition, biological activities and current uses. Int. J. Mol. Sci. 2016, 17, 1414. [Google Scholar] [CrossRef] [PubMed]
- Kaler, K.M.; Setzer, W.N. Seasonal variation in the leaf essential oil composition of Sassafras albidum. Nat. Prod. Commun. 2008, 3, 829–832. [Google Scholar]
- Kamdem, D.P.; Gage, D.A. Chemical composition of essential oil from the root bark of Sassafras albidum. Planta Med. 1995, 61, 574–575. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.E.; Davé, P.C.; Harbin, L.N.; Setzer, W.N. Allelopathic potential of Sassafras albidum and Pinus taeda essential oils. Allelopath. J. 2011, 27, 111–122. [Google Scholar]
- Pulivarthi, D.; Steinberg, K.M.; Monzote, L.; Piñón, A.; Setzer, W.N. Antileishmanial activity of compounds isolated from Sassafras albidum. Nat. Prod. Commun. 2015, 10, 1229–1230. [Google Scholar] [PubMed]
- Rao, K.V.; Alvarez, F.M. Chemistry of Saururus cernuus. I. Saucernetin, a new neolignan. J. Nat. Prod. 1982, 45, 393–397. [Google Scholar] [CrossRef]
- Rao, K.V.; Alvarez, F.M. Manassantins A/B and saucerneol: Novel biologically active lignoids from Saururus cernuus. Tetrahedron Lett. 1983, 24, 4947–4950. [Google Scholar] [CrossRef]
- Rao, K.V.; Reddy, G.C.S. Chemistry of Saururus cernuus, V. Sauristolactam and other nitrogenous constituents. J. Nat. Prod. 1990, 53, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.V.; Prakasa Rao, N.S. Chemistry of Saururus cernuus, VI: Three new neolignans. J. Nat. Prod. 1990, 53, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Kubanek, J.; Fenical, W.; Hay, M.E.; Brown, P.J.; Lindquist, N. Two antifeedant lignans from the freshwater macrophyte Saururus cernuus. Phytochemistry 2000, 54, 281–287. [Google Scholar] [CrossRef]
- Kubanek, J.; Hay, M.E.; Brown, P.J.; Lindquist, N.; Fenical, W. Lignoid chemical defenses in the freshwater macrophyte Saururus cernuus. Chemoecology 2001, 11, 1–8. [Google Scholar] [CrossRef]
- Rajbhandari, I.; Takamatsu, S.; Nagle, D.G. A new dehydrogeranylgeraniol antioxidant from Saururus cernuus that inhibits intracellular reactive oxygen species (ROS)-catalyzed oxidation within HL-60 cells. J. Nat. Prod. 2001, 64, 693–695. [Google Scholar] [CrossRef] [PubMed]
- Hodges, T.W.; Hossain, C.F.; Kim, Y.-P.; Zhou, Y.-D.; Nagle, D.G. Molecular-targeted antitumor agents: The Saururus cernuus dineolignans manassantin B and 4-O-demethylmanassantin B are potent inhibitors of hypoxia-activated HIF-1. J. Nat. Prod. 2004, 67, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Hossain, C.F.; Kim, Y.-P.; Baerson, S.R.; Zhang, L.; Bruick, R.K.; Mohammed, K.A.; Agarwal, A.K.; Nagle, D.G.; Zhou, Y.D. Saururus cernuus lignans—Potent small molecule inhibitors of hypoxia-inducible factor-1. Biochem. Biophys. Res. Commun. 2005, 333, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Upton, R.; DAyu, R.H. Skullcap Scutellaria lateriflora L.: An American nervine. J. Herb. Med. 2012, 2, 76–96. [Google Scholar] [CrossRef]
- Yaghmai, M.S. Volatile constituents of Scutellaria lateriflora L. Flavour Fragr. J. 1988, 3, 27–31. [Google Scholar] [CrossRef]
- Bruno, M.; Cruciata, M.; Bondi, M.L.; Piozzi, F.; de la Torre, M.; Rodgriguez, B.; Servettaz, O. Neo-clerodane diterpenoids from Scutellaria lateriflora. Phytochemistry 1998, 48, 687–691. [Google Scholar] [CrossRef]
- Awad, R.; Arnason, J.T.; Trudeau, V.; Bergeron, C.; Budzinski, J.W.; Foster, B.C.; Merali, Z. Phytochemical and biological analysis of skullcap (Scutellaria lateriflora L.): A medicinal plant with anxiolytic properties. Phytomedicine 2003, 10, 640–649. [Google Scholar] [CrossRef] [PubMed]
- Cole, I.B.; Cao, J.; Alan, A.R.; Saxena, P.K.; Murch, S.J. Comparisons of Scutellaria baicalensis, Scutellaria lateriflora and Scutellaria racemosa: Genome size, antioxidant potential and phytochemistry. Planta Med. 2008, 74, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Lian, X.Y.; Li, S.; Stringer, J.L. Characterization of chemical ingredients and anticonvulsant activity of American skullcap (Scutellaria lateriflora). Phytomedicine 2009, 16, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ding, Y.; Li, X.; Ferreira, D.; Khan, S.; Smillie, T.; Khan, I.A. Scuteflorins A and B, dihydropyranocoumarins from Scutellaria lateriflora. J. Nat. Prod. 2009, 72, 983–987. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.N.; Downey, F.; Ng, C.K.Y. Comparative analysis of bioactive phytochemicals from Scutellaria baicalensis, Scutellaria lateriflora, Scutellaria racemosa, Scutellaria tomentosa and Scutellaria wrightii by LC-DAD-MS. Metabolomics 2011, 7, 446–453. [Google Scholar] [CrossRef]
- Kuroda, M.; Iwabuchi, K.; Mimaki, Y. Chemical constituents of the aerial parts of Scutellaria lateriflora and their α-glucosidase inhibitory activities. Nat. Prod. Commun. 2012, 7, 471–474. [Google Scholar] [PubMed]
- Li, J.; Wang, Y.H.; Smillie, T.J.; Khan, I.A. Identification of phenolic compounds from Scutellaria lateriflora by liquid chromatography with ultraviolet photodiode array and electrospray ionization tandem mass spectrometry. J. Pharm. Biomed. Anal. 2012, 63, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Zalkow, L.H.; Gelbaum, L.T.; Van Derveer, D. Eremophilane sesquiterpenes from Senecio aureus. J. Chem. Soc. Perkin Trans. 1979, 1542–1546. [Google Scholar] [CrossRef]
- Williams, J.D. The Flavonoids and Phenolic Acids of the Genus Silphium and Their Chemosystematic and Medicinal Value. Ph.D. Thesis, University of Texas, Austin, TX, USA, 2006. [Google Scholar]
- Thacker, J.D.; Bordner, J.; Bumgardner, C. Carolinoside: A phytosteroidal glycoside from Solanum carolinense. Phytochemistry 1990, 29, 2965–2970. [Google Scholar] [CrossRef]
- Evans, W.C.; Somanabandhu, A. Bases from roots of Solanum carolinense. Phytochemistry 1977, 16, 1859–1860. [Google Scholar] [CrossRef]
- Tucker, A.O.; Maciarello, M.J.; Clancy, K. Sweet goldenrod (Solidago odora, Asteraceae): A medicine, tea, and state herb. Econ. Bot. 1999, 53, 281–284. [Google Scholar] [CrossRef]
- Adolf, W.; Hecker, E. New irritant diterpene-esters from roots of Stillingia sylvatica L. (Euphorbiaceae). Tetrahedron Lett. 1980, 21, 2887–2890. [Google Scholar] [CrossRef]
- Shamma, M.; Rothenberg, A.S. The alkaloids of Thalictrum dioicum. Lloydia 1978, 41, 169–178. [Google Scholar]
- Shamma, M.; Rothenberg, A.S.; Salgar, S.S.; Jayatilake, G.S. Thalidine, a new isopavine alkaloid from Thalictrum dioicum. Lloydia 1976, 39, 395–398. [Google Scholar] [PubMed]
- Shamma, M.; Salgar, S.S. Pallidine and corydine from Thalictrum dioicum. Phytochemistry 1973, 12, 1505–1506. [Google Scholar] [CrossRef]
- Pérez-Ortega, G.; Guevara-Fefer, P.; Chávez, M.; Herrera, J.; Martínez, A.; Martínez, A.L.; González-Trujano, M.E. Sedative and anxiolytic efficacy of Tilia americana var. mexicana inflorescences used traditionally by communities of State of Michoacan, Mexico. J. Ethnopharmacol. 2008, 116, 461–468. [Google Scholar]
- Herrera-Ruiz, M.; Román-Ramos, R.; Zamilpa, A.; Tortoriello, J.; Jiménez-Ferrer, J.E. Flavonoids from Tilia americana with anxiolytic activity in plus-maze test. J. Ethnopharmacol. 2008, 118, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Martínez, A.L.; González-Trujano, M.E.; Aguirre-Hernández, E.; Moreno, J.; Soto-Hernández, M.; López-Muñoz, F.J. Antinociceptive activity of Tilia americana var. mexicana inflorescences and quercetin in the formalin test and in an arthritic pain model in rats. Neuropharmacology 2009, 56, 564–571. [Google Scholar]
- Aguirre-Hernández, E.; González-Trujano, M.E.; Martínez, A.L.; Moreno, J.; Kite, G.; Terrazas, T.; Soto-Hernández, M. HPLC/MS analysis and anxiolytic-like effect of quercetin and kaempferol flavonoids from Tilia americana var. mexicana. J. Ethnopharmacol. 2010, 127, 91–97. [Google Scholar]
- Cardenas-Rodriguez, N.; Gonzalez-Trujano, M.E.; Aguirre-Hernandez, E.; Ruiz-Garcia, M.; Sampieri, A.; Coballase-Urrutia, E.; Carmona-Aparicio, L. Anticonvulsant and antioxidant effects of Tilia americana var. mexicana and flavonoids constituents in the pentylenetetrazole-induced seizures. Oxid. Med. Cell. Longev. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.C. The essential oil of Tsuga canadensis (L.) Carr. J. Am. Chem. Soc. 1951, 73, 2859–2861. [Google Scholar] [CrossRef]
- Lagalante, A.F.; Montgomery, M.E. Analysis of terpenoids from hemlock (Tsuga) species by solid-phase microextraction/gas chromatography/ion-trap mass spectrometry. J. Agric. Food Chem. 2003, 51, 2115–2120. [Google Scholar] [CrossRef] [PubMed]
- Lagalante, A.F.; Lewis, N.; Montgomery, M.E.; Shields, K.S. Temporal and spatial variation of terpenoids in eastern hemlock (Tsuga canadensis) in relation to feeding by Adelges tsugae. J. Chem. Ecol. 2006, 32, 2389–2403. [Google Scholar] [CrossRef] [PubMed]
- Lagalante, A.F.; Montgomery, M.E.; Calvosa, F.C.; Mirzabeigi, M.N. Characterization of terpenoid volatiles from cultivars of eastern hemlock (Tsuga canadensis). J. Agric. Food Chem. 2007, 55, 10850–10856. [Google Scholar] [CrossRef] [PubMed]
- Craft, J.D.; Setzer, W.N. Leaf essential oil composition of Tsuga canadensis growing wild in North Alabama and Northwest Georgia. Am. J. Essent. Oils Nat. Prod. 2017, 5, 26–29. [Google Scholar]
- Horhammer, L.; Wagner, H.; Reinhardt, H. Isoleuring des Bis-(5,7,4 -trihydroxy-)-flavons, Amentoflavon aus der Rinde von Viburnum prunifolium L. (Amerikan Schneeball). Naturwissenschaften 1965, 7, 161–162. [Google Scholar] [CrossRef]
- Cometa, M.F.; Parisi, L.; Palmery, M.; Meneguz, A.; Tomassini, L. In vitro relaxant and spasmolytic effects of constituents from Viburnum prunifolium and HPLC quantification of the bioactive isolated iridoids. J. Ethnopharmacol. 2009, 123, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Jarboe, C.H.; Zirvi, K.A.; Schmidt, C.M.; McLafferty, F.W.; Haddon, W.F. 1-Methyl 2,3-dibutyl hemimellitate, a novel component of Viburnum prunifolium. J. Org. Chem. 1969, 34, 4202–4203. [Google Scholar] [CrossRef] [PubMed]
- Lopez, E.M.; Craft, J.D.; Setzer, W.N. Volatile composition of Vicia caroliniana growing in Huntsville, Alabama. Am. J. Essent. Oils Nat. Prod. 2017, 5, 8–10. [Google Scholar]
- Hussein, F.T. An Investigation of the Alkaloids of Xanthorhiza simplicissima Marsh. Ph.D. Thesis, The Ohio State University, Columbus, OH, USA, 1963. [Google Scholar]
- Okunade, A.L.; Hufford, C.D.; Richardson, M.D.; Peterson, J.R.; Clark, A.M. Antimicrobial properties of alkaloids from Xanthorhiza simplicissima. J. Pharm. Sci. 1994, 83, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Knapp, J.E.; Hussein, F.T.; Beal, J.L.; Doskotch, R.W.; Tomimatsu, T. Isolation of two bisbenzylisoquinoline alkaloids from the rhizomes and roots of Xanthorhiza simplicissima. J. Pharm. Sci. 1967, 56, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.; Still, C.C.; Sacalis, J.N.; Li, J.; Ho, C.T. Cytotoxic coumarins and lignans from extracts of the northern prickly ash (Zanthoxylum americanum). Phyther. Res. 2001, 15, 441–443. [Google Scholar] [CrossRef] [PubMed]
- Eiter, L.C.; Fadamiro, H.; Setzer, W.N. Seasonal variation in the leaf essential oil composition of Zanthoxylum clava-herculis growing in Huntsville, Alabama. Nat. Prod. Commun. 2010, 5, 457–460. [Google Scholar] [PubMed]
- Steinberg, K.M.; Satyal, P.; Setzer, W.N. Bark essential oils of Zanthoxylum clava-herculis and Ptelea trifoliata: Enantiomeric distribution of monoterpenoids. Nat. Prod. Commun. 2017, 12, 961–963. [Google Scholar]
- Rao, K.V.; Davies, R. The ichthyotoxic principles of Zanthoxylum clava-herculis. J. Nat. Prod. 1986, 49, 340–342. [Google Scholar] [CrossRef]
- Gibbons, S.; Leimkugel, J.; Oluwatuyi, M.; Heinrich, M. Activity of Zanthoxylum clava-herculis extracts against multi-drug resistant methicillin-resistant Staphylococcus aureus (mdr-MRSA). Phyther. Res. 2003, 17, 274–275. [Google Scholar] [CrossRef] [PubMed]
- Chandler, R.F.; Hooper, S.N.; Harvey, M.J. Ethnobotany and phytochemistry of yarrow, Achillea millefolium, Compositae. Econ. Bot. 1982, 36, 203–223. [Google Scholar] [CrossRef]
- Bruneton, J. Pharmacognosy, 2nd ed.; Intercept Ltd.: London, UK, 1999. [Google Scholar]
- Ali, S.I.; Gopalakrishnan, B.; Venkatesalu, V. Pharmacognosy, phytochemistry and pharmacological properties of Achillea millefolium L.: A review. Phyther. Res. 2017, 31, 1140–1161. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, F.; Romano, B.; Fasolino, I.; Tagliatatela-Scafati, O.; Aprea, G.; Capasso, R.; Capasso, F.; Coppola Bottazzi, E.; Izzo, A.A. Prokinetic effect of a standardized yarrow (Achillea millefolium) extract and its constituent choline: Studies in the mouse and human stomach. Neurogastroenterol. Motil. 2012, 24, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Hajhashemi, M.; Ghanbari, Z.; Movahedi, M.; Rafieian, M.; Keivani, A.; Haghollahi, F. The effect of Achillea millefolium and Hypericum perforatum ointments on episiotomy wound healing in primiparous women. J. Matern. Neonatal Med. 2018, 31, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.-C.; Liou, S.-S.; Tzeng, T.-F.; Lee, S.-L.; Liu, I.-M. Effect of topical application of chlorogenic acid on excision wound healing in rats. Planta Med. 2013, 79, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Bagdas, D.; Etoz, B.C.; Gul, Z.; Ziyanok, S.; Inan, S.; Turacozen, O.; Gul, N.Y.; Topal, A.; Cinkilic, N.; Tas, S.; et al. In vivo systemic chlorogenic acid therapy under diabetic conditions: Wound healing effects and cytotoxicity/genotoxicity profile. Food Chem. Toxicol. 2015, 81, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Süntar, I.; Akkol, E.K.; Keles, H.; Yesilada, E.; Sarker, S.D. Exploration of the wound healing potential of Helichrysum graveolens (Bieb.) Sweet: Isolation of apigenin as an active component. J. Ethnopharmacol. 2013, 149, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Jornet, P.; Camacho-Alonso, F.; Gómez-Garcia, F.; Molina Miñano, F.; Cañas, X.; Serafín, A.; Castillo, J.; Vicente-Ortega, V. Effects of potassium apigenin and Verbena extract on the wound healing process of SKH-1 mouse skin. Int. Wound J. 2014, 11, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Manivannan, R. Isolation of apigenin-7-O-(6″-O-E-caffeoyl)-β-d-glucopyranoside from Leucas aspera L. with anti-inflammatory and wound healing activities. J. Pharm. Pharmacogn. Res. 2016, 4, 54–61. [Google Scholar]
- Lodhi, S.; Singhai, A.K. Wound healing effect of flavonoid rich fraction and luteolin isolated from Martynia annua Linn. on streptozotocin induced diabetic rats. Asian Pac. J. Trop. Med. 2013, 6, 253–259. [Google Scholar] [CrossRef]
- Bayrami, Z.; Khalighi-Sigaroodi, F.; Rahimi, R.; Farzaei, M.H.; Hodjat, M.; Baeeri, M.; Rahimifard, M.; Navaei-Nigjeh, M.; Abdollahi, M.; Hajiaghaee, R. In vitro wound healing activity of luteolin. Res. J. Pharmacogn. 2017, 4, 7. [Google Scholar]
- Ozay, Y.; Guzel, S.; Erdogdu, I.H.; Yildirim, Z.; Pehlivanoglu, B.; Turk, B.A.; Darcan, S. Evaluation of the wound healing properties of luteolin ointments on excision and incision wound models in diabetic and non-diabetic rats. Rec. Nat. Prod. 2018, 12, 350–366. [Google Scholar] [CrossRef]
- Süntar, I.; Akkol, E.K.; Keles, H.; Yesilada, E.; Sarker, S.D.; Arroo, R.; Baykal, T. Efficacy of Daphne oleoides subsp. kurdica used for wound healing: Identification of active compounds through bioassay guided isolation technique. J. Ethnopharmacol. 2012, 141, 1058–1070. [Google Scholar]
- Gopalakrishnan, A.; Ram, M.; Kumawat, S.; Tandan, S.; Kumar, D. Quercetin accelerated cutaneous wound healing in rats by increasing levels of VEGF and TGF-β1. Indian J. Exp. Biol. 2016, 54, 187–195. [Google Scholar] [PubMed]
- Ahmad, M.; Sultana, M.; Raina, R.; Pankaj, N.K.; Verma, P.K.; Prawez, S. Hypoglycemic, hypolipidemic, and wound healing potential of quercetin in streptozotocin-induced diabetic rats. Pharmacogn. Mag. 2017, 13, S633–S639. [Google Scholar] [PubMed]
- Doersch, K.M.; Newll-Rogers, M.K. The impact of quercetin on wound healing relates to changes in αV and β1 integrin expression. Exp. Biol. Med. 2017, 242, 1424–1431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Süntar, I.P.; Akkol, E.K.; Yalçin, F.N.; Koca, U.; Keleş, H.; Yesilada, E. Wound healing potential of Sambucus ebulus L. leaves and isolation of an active component, quercetin 3-O-glucoside. J. Ethnopharmacol. 2010, 129, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Clericuzio, M.; Tinello, S.; Burlando, B.; Ranzato, E.; Martinotti, S.; Cornara, L.; La Rocca, A. Flavonoid oligoglycosides from Ophioglossum vulgatum L. Having wound healing properties. Planta Med. 2012, 78, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Rajamanickam, M.; Kalaivanan, P.; Sivagnanam, I. Antibacterial and wound healing activities of quercetin-3-O-α-l-rhamnopyranosyl-(1-->6)-β-d-glucopyranoside isolated from Salvia leucantha. Int. J. Pharm. Sci. Res. 2013, 22, 264–268. [Google Scholar]
- Manivannan, R.; Prabakaran, K.; Ilayaraja, S. Isolation, identification and antibacterial and wound healing studies of quercetin-3-O-α-l-rhamnopyranoside-2″-gallate. Int. J. Appl. Sci. Eng. 2014, 12, 99–106. [Google Scholar]
- Seo, S.H.; Lee, S.-H.; Cha, P.-H.; Kim, M.-Y.; Min, D.S.; Choi, K.-Y. Polygonum aviculare L. and its active compounds, quercitrin hydrate, caffeic acid, and rutin, activate the Wnt/β-catenin pathway and induce cutaneous wound healing. Phytotherapy 2016, 30, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Scott, C.C.; Chen, K.K. The pharmacological action of N-methylcytisine. J. Pharmacol. Exp. Ther. 1943, 79, 334–339. [Google Scholar]
- Anonymous. Lupin Alkaloids in Food: A Toxicological Review and Risk Assessment; Australia New Zealand Food Authority: Canberra, Australia, 2001.
- Keeler, R.F. Lupin alkaloids from teratogenic and nonteratogenic lupins. III. Identification of anagyrine as the probable teratogen by feeding trials. J. Toxicol. Environ. Health 1976, 1, 887–898. [Google Scholar] [CrossRef] [PubMed]
- de la Peña, J.B.I.; Lee, H.L.; Yoon, S.Y.; Kim, G.H.; Lee, Y.S.; Cheong, J.H. The involvement of magnoflorine in the sedative and anxiolytic effects of Sinomeni Caulis et Rhizoma in mice. J. Nat. Med. 2013, 67, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Predny, M.L.; De Angelis, P.; Chamberlain, J.L. Black Cohosh, Actaea Racemosa: An Annotated Bibliography; U.S. Department of Agriculture Forest Service, Southern Research Station: Asheville, NC, USA, 2006.
- Gruenwald, J.; Brendler, T.; Jaenicke, C. PDR for Herbal Medicines, 4th ed.; Thompson Healthcare, Inc.: Montvale, NJ, USA, 2007. [Google Scholar]
- Liu, Z.; Yang, Z.; Zhu, M.; Huo, J. [Estrogenicity of black cohosh (Cimicifuga racemosa) and its effect on estrogen receptor level in human breast cancer MCF-7 cells]. Wei Sheng Yan Jiu 2001, 30, 77–80. [Google Scholar] [PubMed]
- Seidlová-Wuttke, D.; Hesse, O.; Jarry, H.; Christoffel, V.; Spengler, B.; Becker, T.; Wuttke, W. Evidence for selective estrogen receptor modulator activity in a black cohosh (Cimicifuga racemosa) extract: Comparison with estradiol-17β. Eur. J. Endocrinol. 2003, 149, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Lupu, R.; Mehmi, I.; Atlas, E.; Tsai, M.-S.; Pisha, E.; Oketch-Rabah, H.A.; Nuntanakorn, P.; Kennelly, E.J.; Kronenberg, F. Black cohosh, a menopausal remedy, does not have estrogenic activity and does not promote breast cancer cell growth. Int. J. Oncol. 2003, 23, 1407–1412. [Google Scholar] [CrossRef] [PubMed]
- Mahady, G.B. Is black cohosh estrogenic? Nutr. Rev. 2003, 61, 183–186. [Google Scholar] [PubMed]
- Gaube, F.; Wolfl, S.; Pusch, L.; Kroll, T.C.; Hamburger, M. Gene expression profiling reveals effects of Cimicifuga racemosa (L.) NUTT. (black cohosh) on the estrogen receptor positive human breast cancer cell line MCF-7. BMC Pharmacol. 2007, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Kennelly, E.J.; Baggett, S.; Nuntanakorn, P.; Ososki, A.L.; Mori, S.A.; Duke, J.; Coleton, M.; Kronenberg, F. Analysis of thirteen populations of black cohosh for formononetin. Phytomedicine 2002, 9, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Powers, C.N.; Setzer, W.N. A molecular docking study of phytochemical estrogen mimics from dietary herbal supplements. Silico Pharmacol. 2015, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Burdette, J.E.; Liu, J.; Chen, S.-N.; Fabricant, D.S.; Piersen, C.E.; Barker, E.L.; Pezzuto, J.M.; Mesecar, A.; van Breemen, R.B.; Farnsworth, N.R.; et al. Black cohosh acts as a mixed competitive ligand and partial agonist of the serotonin receptor. J. Agric. Food Chem. 2003, 51, 5661–5670. [Google Scholar] [CrossRef] [PubMed]
- Rhyu, M.-R.; Lu, J.; Webster, D.E.; Fabricant, D.S.; Farnsworth, N.R.; Wang, Z.J. Black cohosh (Actaea racemosa, Cimicifuga racemosa) behaves as a mixed competitive ligand and partial agonist at the human μ opiate receptor. J. Agric. Food Chem. 2006, 54, 9852–9857. [Google Scholar] [CrossRef] [PubMed]
- Reame, N.E.; Lukacs, J.L.; Padmanabhan, V.; Eyvazzadeh, A.D.; Smith, Y.R.; Zubieta, J.-K. Black cohosh has central opioid activity in postmenopausal women: Evidence from naloxone blockade and PET neuroimaging studies. Menopause 2008, 15, 832–849. [Google Scholar] [CrossRef] [PubMed]
- Cicek, S.S.; Khom, S.; Taferner, B.; Hering, S.; Stuppner, H. Bioactivity-guided isolation of GABAA receptor modulating constituents from the rhizomes of Actaea racemosa. J. Nat. Prod. 2010, 73, 2024–2028. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, F.; Ernst, E. Cimicifuga racemosa: A systematic review of its clinical efficacy. Eur. J. Clin. Pharmacol. 2002, 58, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, F.; Ernst, E. Black cohosh (Cimicifuga racemosa) for menopausal symptoms: A systematic review of its efficacy. Pharmacol. Res. 2008, 58, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Frei-Kleiner, S.; Schaffner, W.; Rahlfs, V.W.; Bodmer, C.; Birkhäuser, M. Cimicifuga racemosa dried ethanolic extract in menopausal disorders: A double-blind placebo-controlled clinical trial. Maturitas 2005, 51, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, F.; Ernst, E. Black cohosh (Cimicifuga racemosa): A systematic review of adverse events. Am. J. Obstet. Gynecol. 2008, 199, 455–466. [Google Scholar] [CrossRef] [PubMed]
- Schmid, D.; Woehs, F.; Svoboda, M.; Thalhammer, T.; Chiba, P.; Moeslinger, T. Aqueous extracts of Cimicifuga racemosa and phenolcarboxylic constituents inhibit production of proinflammatory cytokines in LPS-stimulated human whole blood. Can. J. Physiol. Pharmacol. 2009, 87, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.L.H.; Chik, S.C.C.; Li, J.C.B.; Cheung, B.K.W.; Lau, A.S.Y. Identification of the bioactive constituent and its mechanisms of action in mediating the anti-inflammatory effects of black cohosh and related Cimicifuga species on human primary blood macrophages. J. Med. Chem. 2009, 52, 6707–6715. [Google Scholar] [CrossRef] [PubMed]
- Schmid, D.; Gruber, M.; Woehs, F.; Prinz, S.; Etzlstorfer, B.; Prucker, C.; Fuzzati, N.; Kopp, B.; Moeslinger, T. Inhibition of inducible nitric oxide synthesis by Cimicifuga racemosa (Actaea racemosa, black cohosh) extracts in LPS-stimulated RAW 264.7 macrophages. J. Pharm. Pharmacol. 2009, 61, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Erdelmeier, C.A.J.; Cinatl, J.; Rabenau, H.; Doerr, H.W.; Biber, A.; Koch, E. Antiviral and antiphlogistic activities of Hamamelis virginiana bark. Planta Med. 1996, 62, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Duwiejua, M.; Zeitlin, I.J.; Waterman, P.G.; Gray, A.I. Anti-inflammatory activity of Polygonum bistorta, Guaiacum officinale and Hamamelis virginiana in rats. J. Pharm. Pharmacol. 1994, 46, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Hartisch, C.; Kolodziej, H.; von Bruchhousen, F. Dual inhibitory activities of tannins from Hamamelis virginiana and related polyphenols on 5-lipoxygenase and lyso-PAF: Acetyl-CoA acetyltransferase. Planta Med. 1997, 63, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Deters, A.; Dauer, A.; Schnetz, E.; Fartasch, M.; Hensel, A. High molecular compounds (polysaccharides and proanthocyanidins) from Hamamelis virginiana bark: Influence on human skin keratinocyte proliferation and differentiation and influence on irritated skin. Phytochemistry 2001, 58, 949–958. [Google Scholar] [CrossRef]
- Theisen, L.L.; Erdelmeier, C.A.J.; Spoden, G.A.; Boukhallouk, F.; Sausy, A.; Florin, L.; Muller, C.P. Tannins from Hamamelis virginiana bark extract: Characterization and improvement of the antiviral efficacy against influenza A virus and human papillomavirus. PLoS ONE 2014, 9, e88062. [Google Scholar] [CrossRef] [PubMed]
- Hughes-Formella, B.J.; Bohnsack, K.; Rippke, F.; Benner, G.; Rudolph, M.; Tausch, I.; Gassmueller, J. Anti-inflammatory effect of Hamamelis lotion in a UVB erythema test. Dermatology 1998, 196, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Dawid-Pać, R. Medicinal plants used in treatment of inflammatory skin diseases. Postęp. Dermatol. Alergol. 2013, 30, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Missouri Botanical Garden Tropicos. Available online: www.tropicos.org (accessed on 27 July 2018).
- Memorial Sloan Kettering Cancer Center Goldenseal. Available online: www.mskcc.org (accessed on 16 October 2018).
- Orfila, L.; Rodríguez, M.; Colman, T.; Hasegawa, M.; Merentes, E.; Arvelo, F. Structural modification of berberine alkaloids in relation to cytotoxic activity in vitro. J. Ethnopharmacol. 2000, 71, 449–456. [Google Scholar] [CrossRef]
- Cordero, C.P.; Gómez-González, S.; León-Acosta, C.J.; Morantes-Medina, S.J.; Aristizabal, F.A. Cytotoxic activity of five compounds isolated from Colombian plants. Fitoterapia 2004, 75, 225–227. [Google Scholar] [CrossRef] [PubMed]
- Correché, E.R.; Andujar, S.A.; Kurdelas, R.R.; Lechón, M.J.G.; Freile, M.L.; Enriz, R.D. Antioxidant and cytotoxic activities of canadine: Biological effects and structural aspects. Bioorganic Med. Chem. 2008, 16, 3641–3651. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.B.; Yu, J.-H.; Ko, E.; Lee, K.-W.; Song, A.K.; Park, S.Y.; Shin, I.; Han, W.; Noh, D.Y. The alkaloid berberine inhibits the growth of Anoikis-resistant MCF-7 and MDA-MB-231 breast cancer cell lines by inducing cell cycle arrest. Phytomedicine 2010, 17, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Mazzini, S.; Bellucci, M.C.; Mondelli, R. Mode of binding of the cytotoxic alkaloid berberine with the double helix oligonucleotide d(AAGAATTCTT)2. Bioorganic Med. Chem. 2002, 11, 505–514. [Google Scholar] [CrossRef]
- Kumar, G.S.; Das, S.; Bhadra, K.; Maiti, M. Protonated forms of poly[d(G-C)] and poly(dG).poly(dC) and their interaction with berberine. Bioorganic Med. Chem. 2003, 11, 4861–4870. [Google Scholar] [CrossRef]
- Ferraroni, M.; Bazzicalupi, C.; Bilia, A.R.; Gratteri, P. X-ray diffraction analyses of the natural isoquinoline alkaloids berberine and sanguinarine complexed with double helix DNA d(CGTACG). Chem. Commun. 2011, 47, 4917–4919. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-P.; Chuang, T.-C.; Yeh, M.-H.; Hsu, S.-C.; Way, T.-D.; Chen, P.-Y.; Wang, S.S.; Chang, Y.-H.; Kao, M.-C.; Liu, J.-Y. Growth suppression of HER2-overexpressing breast cancer cells by berberine via modulation of the HER2/PI3K/Akt signaling pathway. J. Agric. Food Chem. 2011, 59, 8216–8224. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-P.; Chuang, T.-C.; Tsai, S.-C.; Tseng, H.-H.; Hsu, S.-C.; Chen, Y.-C.; Kuo, C.-L.; Kuo, Y.-H.; Liu, J.-Y.; Kao, M.-C. Berberine, an isoquinoline alkaloid, inhibits the metastatic potential of breast cancer cells via Akt pathway modulation. J. Agric. Food Chem. 2012, 60, 9649–9658. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, K.; Kamigauchi, M.; Ueki, M.; Taniguchi, M. Antibacterial activity and structure-activity relationships of berberine analogs. Eur. J. Med. Chem. 1996, 31, 469–478. [Google Scholar] [CrossRef]
- Kaneda, Y.; Torii, M.; Tanaka, T.; Aikawa, M. In vitro effects of berberine sulphate on the growth and structure of Entamoeba histolytica, Giardia lamblia and Trichomonas vaginalis. Ann. Trop. Med. Parasitol. 1991, 85, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Merschjohann, K.; Sporer, F.; Steverding, D.; Wink, M. In vitro effect of alkaloids on bloodstream forms of Trypanosoma brucei and T. congolense. Planta Med. 2001, 67, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Vennerstrom, J.L.; Lovelace, J.K.; Waits, V.B.; Hanson, W.L.; Klayman, D.L. Berberine derivatives as antileishmanial drugs. Antimicrob. Agents Chemother. 1990, 34, 918–921. [Google Scholar] [CrossRef] [PubMed]
- Ropivia, J.; Derbré, S.; Rouger, C.; Pagniez, F.; Le Pape, P.; Richomme, P. Isoquinolines from the roots of Thalictrum flavum L. and their evaluation as antiparasitic compounds. Molecules 2010, 15, 6476–6484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Küpeli, E.; Koşar, M.; Yeşilada, E.; Başer, K.H.C.; Başer, C. A comparative study on the anti-inflammatory, antinociceptive and antipyretic effects of isoquinoline alkaloids from the roots of Turkish Berberis species. Life Sci. 2002, 72, 645–657. [Google Scholar] [CrossRef]
- Mahady, G.B.; Chadwick, L.R. Goldenseal (Hydrastis canadensis): Is there enough scientific evidence to support safety and efficacy? Nutr. Clin. Care 2001, 4, 243–249. [Google Scholar] [CrossRef]
- Cicero, A.F.; Ertek, S. Metabolic and cardiovascular effects of berberine: From preclinical evidences to clinical trial results. Clin. Lipidol. 2009, 4, 553–563. [Google Scholar] [CrossRef]
- Hämet-Ahti, L. The Juncus effusus aggregate in eastern North America. Ann. Bot. Fenn. 1980, 17, 183–191. [Google Scholar]
- Della Greca, M.; Fiorentino, A.; Molinaro, A.; Monaco, P.; Previtera, L. 9,10-Dihydrophenanthrene glucosides from Juncus effusus. Nat. Prod. Lett. 1995, 6, 111–117. [Google Scholar] [CrossRef]
- Park, S.N.; Won, D.H.; Hwang, J.P.; Han, S.B. Cellular protective effects of dehydroeffusol isolated from Juncus effusus L. and the mechanisms underlying these effects. J. Ind. Eng. Chem. 2014, 20, 3046–3052. [Google Scholar] [CrossRef]
- Krochmal, A.; Walters, R.S.; Doughty, R.M. A Guide to Medicinal Plants of Appalachia; United States Department of Agriculture: Upper Darby, PA, USA, 1969.
- Nolan, J.M. The roots of tradition: Social ecology, cultural geography, and medicinal plant knowledge in the Ozark-Ouachita Highlands. J. Ethnobiol. 1998, 18, 249–269. [Google Scholar]
- Scholey, A.; Ossoukhova, A.; Owen, L.; Ibarra, A.; Pipingas, A.; He, K.; Roller, M.; Stough, C. Effects of American ginseng (Panax quinquefolius) on neurocognitive function: An acute, randomised, double-blind, placebo-controlled, crossover study. Psychopharmacology 2010, 212, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Barton, D.L.; Liu, H.; Dakhil, S.R.; Linquist, B.; Sloan, J.A.; Nichols, C.R.; McGinn, T.W.; Stella, P.J.; Seeger, G.R.; Sood, A.; et al. Wisconsin ginseng (Panax quinquefolius) to improve cancer-related fatigue: A randomized, double-blind trial, N07C2. J. Natl. Cancer Inst. 2013, 105, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- McElhaney, J.E.; Goel, V.; Toane, B.; Hooten, J.; Shan, J.J. Efficacy of COLD-fX in the prevention of respiratory symptoms in community-dwelling adults: A randomized, double-blinded, placebo controlled trial. J. Altern. Complement. Med. 2006, 12, 153–157. [Google Scholar] [CrossRef] [PubMed]
- McElhaney, J.E.; Simor, A.E.; McNeil, S.; Predy, G.N. Efficacy and safety of CVT-E002, a proprietary extract of Panax quinquefolius in the prevention of respiratory infections in influenza-vaccinated community-dwelling adults: A multicenter, randomized, double-blind, and placebo-controlled trial. Influenza Res. Treat. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- Predny, M.L.; Chamberlain, J.L. Bloodroot (Sanguinaria canadensis) an Annotated Bibliography; U.S. Department of Agriculture, Forest Service, Southern Research Station: Asheville, NC, USA, 2005.
- Qing, Z.-X.; Yang, P.; Tang, Q.; Cheng, P.; Liu, X.-B.; Zheng, Y.; Liu, Y.-S.; Zeng, J.-G. Isoquinoline alkaloids and their antiviral, antibacterial, and antifungal activities and structure-activity relationship. Curr. Org. Chem. 2017, 21, 1920–1934. [Google Scholar] [CrossRef]
- Obiang-Obounou, B.W.; Kang, O.-H.; Choi, J.-G.; Keum, J.-H.; Kim, S.-B.; Mun, S.-H.; Shin, D.-W.; Kim, K.W.; Park, C.-B.; Kim, Y.-G.; et al. The mechanism of action of sanguinarine against methicillin-resistant Staphylococcus aureus. J. Toxicol. Sci. 2011, 36, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Watamoto, T.; Egusa, H.; Sawase, T.; Yatani, H. Screening of pharmacologically active small molecule compounds identifies antifungal agents against Candida biofilms. Front. Microbiol. 2015, 6, 1453. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.; Duke, J.A. A Field Guide to Medicinal Plants; Houghton Mifflin: Boston, MA, USA, 1990. [Google Scholar]
- Brock, C.; Whitehouse, J.; Tewfik, I.; Towell, T. The use of Scutellaria lateriflora: A pilot survey amongst herbal medicine practitioners. J. Herb. Med. 2012, 2, 34–41. [Google Scholar] [CrossRef]
- Zhu, J.T.T.; Choi, R.C.Y.; Li, J.; Xie, H.Q.H.; Bi, C.W.C.; Cheung, A.W.H.; Dong, T.T.X.; Jiang, Z.Y.; Chen, J.J.; Tsim, K.W.K. Estrogenic and neuroprotective properties of scutellarin from Erigeron breviscapus: A drug against postmenopausal symptoms and Alzheimer’s disease. Planta Med. 2009, 75, 1489–1493. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Ma, H.; Tang, Y.; Chen, W.; Lu, Y.; Guo, J.; Duan, J.A. Discovery of estrogen receptor α modulators from natural compounds in Si-Wu-Tang series decoctions using estrogen-responsive MCF-7 breast cancer cells. Bioorganic Med. Chem. Lett. 2012, 22, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.F.; Gao, F.; Li, X.W.; Jia, R.H.; Meng, X.D.; Zhao, R.; Jing, Y.Y.; Wang, Y.; Jiang, W. The anticonvulsant and neuroprotective effects of baicalin on pilocarpine-induced epileptic model in rats. Neurochem. Res. 2012, 37, 1670–1680. [Google Scholar] [CrossRef] [PubMed]
- Park, H.G.; Yoon, S.Y.; Choi, J.Y.; Lee, G.S.; Choi, J.H.; Shin, C.Y.; Son, K.H.; Lee, Y.S.; Kim, W.K.; Ryu, J.H.; et al. Anticonvulsant effect of wogonin isolated from Scutellaria baicalensis. Eur. J. Pharmacol. 2007, 574, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Feng, T.; Shan, L.; Cai, B.; Chu, W.; Niu, H.; Lu, Y.; Yang, B. Scutellarin-induced endothelium-independent relaxation in rat aorta. Phyther. Res. 2008, 22, 1428–1433. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Lust, R.M.; Bofferding, A.B.S.; Wingard, C.J. Nitric oxide and catalase-sensitive relaxation by scutellarin in the mouse thoracic aorta. J. Cardiovasc. Pharmacol. 2009, 53, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.T.; Zhang, D.X.; Liu, F.; Mao, H.P.; Ma, Y.K.; Yang, Y.; Li, C.X.; Qiu, L.Z.; Geng, X.; Zhang, J.M.; et al. Vasodilatory effect of wogonin on the rat aorta and its mechanism study. Biol. Pharm. Bull. 2015, 38, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Shih, H.C.; Yang, L.L. Relaxant effect induced by wogonin from Scutellaria baicalensis on rat isolated uterine smooth muscle. Pharm. Biol. 2012, 50, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wong, C.M.; Lau, C.W.; Yao, X.; Tsang, S.Y.; Su, Y.L.; Chen, Z.Y. Inhibition of nitric oxide/cyclic GMP-mediated relaxation by purified flavonoids, baicalin and baicalein, in rat aortic rings. Biochem. Pharmacol. 2004, 67, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.F.; Hung, W.Y.; Chen, C.F. Anxiolytic-like effects of baicalein and baicalin in the Vogel conflict test in mice. Eur. J. Pharmacol. 2003, 464, 141–146. [Google Scholar] [CrossRef]
- Hui, K.M.; Huen, M.S.Y.; Wang, H.Y.; Zheng, H.; Sigel, E.; Baur, R.; Ren, H.; Li, Z.W.; Wong, J.T.-F.; Xue, H. Anxiolytic effect of wogonin, a benzodiazepine receptor ligand isolated from Scutellaria baicalensis Georgi. Biochem. Pharmacol. 2002, 64, 1415–1424. [Google Scholar] [CrossRef]
- Wang, F.; Xu, Z.; Ren, L.; Tsang, S.Y.; Xue, H. GABAA receptor subtype selectivity underlying selective anxiolytic effect of baicalin. Neuropharmacology 2008, 55, 1231–1237. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, R.S.M.; Duarte, F.S.; de Lima, T.C.M. Involvement of GABAergic non-benzodiazepine sites in the anxiolytic-like and sedative effects of the flavonoid baicalein in mice. Behav. Brain Res. 2011, 221, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, P.; Hoffmann, D.L. An investigation into the efficacy of Scutellaria lateriflora in healthy volunteers. Altern. Ther. Health Med. 2003, 9, 74–78. [Google Scholar] [PubMed]
- Brock, C.A.; Whitehouse, J.; Tewfik, I.; Towell, T. American skullcap (Scutellaria lateriflora L.): A randomised, double-blind placebo-controlled crossover study of its effects on mood in healthy volunteers. Phyther. Res. 2012, 28, 692–698. [Google Scholar] [CrossRef] [PubMed]


| Scientific Name | Family | Common Name | Cherokee Use | Part Used | Chemical Constituents and Activities | Ref. |
|---|---|---|---|---|---|---|
| Acer rubrum L. | Sapindaceae | Red maple | analgesic (cramps), eye soreness | bark | [15] | |
| Leaves: 1-O-galloyl-α-l-rhamnose, 1-O-galloyl-β-d-glucose, gallic acid, methyl gallate, ethyl gallate, m-digallate, ethyl digallate | [27] | |||||
| Leaves: gallic acid, methyl gallate, ethyl gallate, m-digallate, ethyl m-digallate, 1-O-galloyl-β-d-glucose, 1-O-galloyl-α-l-rhamnose, kaempferol 3-O-β-d-glucoside, kaempferol 3-O-β-d-galactoside, kaempferol 3-O-β-l-rhamnoside, kaempferol-3-O-rhamnoglucoside, quercetin 3-O-β-d-glucoside, quercetin 3-O-β-l-rhamnoside and quercetin | [28] | |||||
| Leaves: major gallotannins: maplexin B, ginnalin B, ginnalin C, ginnalin A, maplexin F and a pair of isomers, 6-O-digalloyl-2-O-galloyl-1,5-anhydro-d-glucitol and 2-O-digalloyl-6-O-galloyl-1,5-anhydro-d-glucitol; ginnalin A was the predominant gallotannin | [29] | |||||
| Bark: catechin, epicatechin, epicatechin gallate, procyanidin A6, procyanidin A2, quercetin-3-O-α-l-rhamnopyranoside, quercetin-3-O-(3′′-O-galloyl)-α-l-rhamnopyranoside, quercetin-3-O-(2′′-O-galloyl)-α-l-rhamnopyranoside, nortrachelogenin-8′-O-β-d-glucopyranoside, 7,8-dihydroxy-6-ethoxycoumarin, phloridzin, methyl vanillate, 3,5-dihydroxy-4-methoxybenzoic acid, and 3-methoxy-4-hydroxyphenol-1-O-β-d-(6′-O-galloyl)- glucopyranoside | [30] | |||||
| Bark: gallotannins, named maplexins A–E; showed α-glucosidase inhibitory activity | [31] | |||||
| Bark: gallotannins, maplexins F–I; phenolic glycosides, rubrumosides A–B. The maplexins showed α-glucosidase inhibitory activity | [32] | |||||
| Bark: Maplexins C and D showed cytotoxic activity on HCT-116 and MCF-7 cells | [33] | |||||
| Leaves and flowers: 2-methoxyl-1-O-galloyl-myo-inositol, 1-O-(3′-methoxyl-galloyl)-β-d-glucose | [34] | |||||
| Acer saccharinum L. | Sapindaceae | Silver maple | analgesic (cramps), eye soreness | bark | [15] | |
| Leaves: methyl gallate; cytotoxic to B16 melanoma in mice | [35] | |||||
| Leaves: glucitol-core containing gallotannins (GCGs), ginnalins A–C, maplexins B, D, and F; phenolics, methyl syringate, methyl gallate, and 3-methoxy-4-hydroxyphenol-1-β-d-(6-galloyl)-glucopyranoside; sesquiterpenoid pubineroid A | [36] | |||||
| Achillea millefolium L. | Asteraceae | Yarrow | hemorrhages (leaves), fever (infusion) | leaves | [15] | |
| Herb: 5-hydroxy-3,6,7,4′-tetramethoxyflavone, artemetin, casticin | [37] | |||||
| Herb: chlorogenic acid, vicenin-2, luteolin-7-O-glucoside, rutin, apigenin-7-O-glucoside, luteolin, and apigenin | [38] | |||||
| Herb: apigenin, luteolin, centaureidin, β-sitosterol, 3β-hydroxy-11α,13-dihydro-costunolide, desacetylmatricarin, leucodin, achillin, 8α-angeloxy-leucodin and 8α-angeloxy-achillin | [39] | |||||
| Herb: chlorogenic acid, rutin, luteolin 7-O-glucoside, 1,3-dicaffeoylquinic acid, 1,4-dicaffeoylquinic acid, 3,4-dicaffeoylquinic acid, apigenin 4′-O-glucoside, apigenin 7-O-glucoside, luteolin 4′-O-glucoside, 3,5-dicaffeoylquinic acid; luteolin and apigenin 7-O-glucoside showed notable antiplasmodial activity | [40] | |||||
| Herb: 5-O-caffeoylquinic acid, quercetin O-hexoside, 3,4-O-dicaffeoylquinic acid, quercetin O-acetylhexoside, cis-3,5-O-dicaffeoylquinic acid, trans-3,5-O-dicaffeoylquinic acid, 4,5-O-dicaffeoylquinic acid, apigenin 7-O-glucoside, luteolin O-acetylhexoside, apigenin O-acetylhexoside | [41] | |||||
| Herb: chlorogenic acid, 3,5-dicaffeoyl quinic acid, 4,5-dicaffeoyl quinic acid, apigenin 7-O-glucoside, luteolin | [42] | |||||
| Flowers: methyl achimillate A, methyl achimillate B, methyl achimillate C; all three compounds active against P-388 leukemia in vivo (mouse) | [43] | |||||
| Herb: dihydrodehydrodiconiferyl alcohol 9-O-β-d-glucopyranoside, apigenin, apigenin-7-O-β-d-glucopyranoside, luteolin, luteolin-7-O-β-d-glucopyranoside, luteolin-4′-O-β-d-glucopyranoside, rutin, 3,5-dicaffeoylquinic acid, and chlorogenic acid; apigenin and luteolin showed in vitro estrogenic activity | [44] | |||||
| Herb: hydroalcoholic extract showed antinociceptive activity | [45] | |||||
| Herb: rutin, schaftoside, isoschaftoside, luteolin-7-O-glucoside (major), apigenin-7-O-glucoside (major), luteolin-7-malonylglucoside, apigenin-7-malonylglucoside, luteolin, apigenin | [46] | |||||
| Herb: five flavonoids (apigenin, luteolin, centaureidin, casticin and artemetin) and five sesquiterpenoids (paulitin, isopaulitin, psilostachyin C, desacetylmatricarin and sintenin); centaureidin, casticin, and paulitin showed good in vitro cytotoxic activity on HeLa, MCF-7, and A-431 cells | [47] | |||||
| Herb EO: 1,8-cineole (24.6%), camphor (16.7%), α-terpineol (10.2%); weak antimicrobial activity on Streptococcus pneumoniae, Clostridium perfringens, and Candida albicans | [48] | |||||
| Herb EO: germacrene D (6.1%), chamazulene (48.3%); shows antitrypanosomal activity (Trypanosoma cruzi) | [49] | |||||
| Herb EO: α-pinene (0.6–10.0%), camphene (0.4–15.4%), β-pinene (1.9–38.7%), limonene (1.4–3.8%), γ-terpinene (3.5–13.1%), β-caryophyllene (4.4–13.8%), germacrene D (1.7–10.7%), cadinene (0.7–32.2%) | [50] | |||||
| Herb supercritical CO2 extract: myrcene (4.9%), p-cymene (5.4%), 1,8-cineole (16.2%), γ-terpinene (9.4%), camphor (38.4%), bornyl acetate (4.3%) | [51] | |||||
| Herb EO: β-pinene (4.3%), 1,8-cineole (15.2%), β-cubebene (4.0%), germacrene D (14.1%), τ-cadinol (4.4%) | [52] | |||||
| Herb EO: sabinene (5.4%), 1,8-cineole (24.5%), trans-sabinene hydrate (10.2%), cis-sabinene hydrate (4.6%), camphor (4.9%), terpinen-4-ol (5.6%), bornyl acetate (4.0%), germacrene D (7.2%) | [53] | |||||
| Aesculus pavia L. | Sapindaceae | Red buckeye | tumors, infections (poultice of nuts) | nuts | [15] | |
| Fruits: polyhydroxyoleanene triterpenoid saponins (aesuliosides Ia–Ie, IIa–IId, and IVa–IVc) | [54] | |||||
| Fruits: 13 polyhydroxyoleanene pentacyclic triterpenoid saponins, aesculiosides IIe–IIk, and IIIa–IIIf, together with 18 known compounds: aesculiosides Ia–Ie, IIa–IId, IVa–IVc, 3-O-[β-d-galactopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,15α,16α,21β,22α,28-hexahydroxyolean-12-ene, 3-O-[β-d-glucopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,16α,21β,22α,24β,28-hexahydroxyolean-12-ene, 3-O-[β-d-galactopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,16α,21β,22α,28-pentahydroxyolean-12-ene, R1-barrigenol, scopolin, and 5-methoxyscopolin. Aesculioside IIc, 3-O-[β-d-galactopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,15α,16α,21β,22α,28-hexahydroxyolean-12-ene, 3-O-[β-d-glucopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,16α,21β,22α,24β,28-hexahydroxyolean-12-ene, 3-O-[β-d-galactopyranosyl(1→2)]-α-l-arabinofuranosyl(1→3)-β-d-glucuronopyranosyl-21,22-O-diangeloyl-3β,16α,21β,22α,28-pentahydroxyolean-12-ene, showed broad cytotoxic activity | [55] | |||||
| Fruits: oleane saponins (vaccaroside A, vaccaroside B); showed in vitro cytotoxic activity on FL normal human amniotic cells and A-549 human lung carcinoma cells | [56] | |||||
| Leaves: prenylated coumarin pavietin; flavonol glycosides quercetin 3-O-α-rhamnoside (quercitrin), quercetin 3-O-α-arabinoside, and isorhamnetin 3-O-α-arabinoside (distichin). Pavietin showed antifungal activity on Guignardia aesculi | [57] | |||||
| Leaves: oleane saponins (escins Ia, Ib, IIa, IIb, IIIa) | [58] | |||||
| Leaves: oleane saponins (paviosides A–H); all show in vitro cytotoxic activity on J-774 murine macrophage and WEHI-164 murine fibrosarcoma | [59] | |||||
| Ageratina altissima (L.) R.M. King and H. Rob. (syn. Eupatorium rugosum Houtt.) | Asteraceae | White snakeroot | fever, tonic, urinary diseases | root | [15] | |
| Aerial parts: tremetone, 6-hydroxytremetone, dehydrotremetone; tremetone cytotoxic on murine melanoma (B16F1) cells | [60] | |||||
| Aerial parts: tremetone, dehydrotremetone | [61] | |||||
| Aerial parts: tremetone, 6-hydroxytremetone, dehydrotremetone, dehydrotremetone, 2-senecioyl-4-acetylphenol, 2-senecioyl-4-(1-methoxyethyl)phenol, 6-acetyl-2,2-dimethylchroman-4-one, 6-acetyl-7-methoxy-2,2-dimethylchromene, 6-acetyl-8-methoxy-2,2-dimethylchromene, 6-acetyl-5-hydroxy-8-methoxy-2,2-dimethylchromene, 6,7-dimethoxy-2,2-dimethylchromene, and 6-(1-hydroxyethyl)-7-methoxy-2,2-dimethylchromene. Tremetone, hydroxygremetone, dehydrotremetone toxic in goldfish assay | [62] | |||||
| Allium canadense L. | Amarylli-daceae | Meadow garlic | cathartic, diuretic | entire plant | [15] | |
| Herb: cysteine sulfoxides: methiin, alliin, propiin | [63] | |||||
| Allium cernuum Roth | Amarylli-daceae | Nodding onion | fever | entire plant | [15] | |
| Herb: diosgenin | [64] | |||||
| Herb: cysteine sulfoxides: methiin, alliin, isoalliin | [63] | |||||
| Allium tricoccum Aiton | Amarylli-daceae | Wild leek | tonic (entire plant) | entire plant | [15] | |
| Herb: methanesulfinothioic acid S-methyl ester, methanesulfinothioic acid S-2-propenyl ester, 2-propene-1-sulfinothioic acid S-methyl ester, methanesulfinothioic acid S-(E)-1-propenyl ester, methanesulfinothioic acid S-(Z)-1-propenyl ester, (E)-1-propenesulfinothioic acid S-methyl ester, 2-propene-1-sulfinothioic acid S-2-propenyl ester (allicin), 1-propanesulfinothioic acid S-2-propenyl ester, 2-propene-1-sulfinothioic acid S-(E)-1-propenyl ester, 2-propene-1-sulfinothioic acid S-(Z)-1-propenyl ester, (E)-1-propenesulfinothioic acid S-2-propenyl ester, 1-propanesulfinothioic acid S-(E)-1-propenyl ester, (E)-1-propenesulfinothioic acid S-n-propyl ester, methyl 1-(methylsulfinyl)propyl disulfide, methyl (E)-1-(1-propenylsulfinyl)propyl disulfide, 1-(methylsulfinyl)propyl (E,Z)-1-propenyl disulfide, methyl 1-(2-propenylsulfinyl)propyl disulfide, 1-(methylsulfinyl) propyl 2-propenyl disulfide, 1-(methylsulfinyl)propyl propyl disulfide, (E)-1-propenyl 1-(1-propenylsulfinyl)propyl disulfide, 2-propenyl 1-(2-propenylsulfinyl) propyl disulfide, (E)-1-(1-propenylsulfinyl)propyl propyl disulfide, (E)-1-propenyl 1-(propylsulfinyl)propyl disulfide, propyl 1-(propylsulfinyl)propyl disulfide | [65] | |||||
| Allium vineale L. a | Amarylli-daceae | Wild garlic | carminative, cathartic, diuretic | entire plant | [15] | |
| Herb: molluscicidal saponins (nuatigenin 3-O-[α-rhamnosyl-(1→2)-β-glucoside, isonuatigenin 3-O-[α-rhamnosyl-(1→2)-β-glucoside | [66] | |||||
| Herb: diosgenin saponins: diosgenin 3-O-α-rhamnosyl-(1→2)-β-glucoside (ophiopogonin C′), diosgenin 3-O-β-glucosyl-(1→4)-α-rhamnosyl-(1→4)-β-glucoside, diosgenin 3-O-α-rhamnosyl-(1→2)-β-glucosyl-(1→4)-β-glucoside (deltonin), diosgenin 3-O-β-glucosyl-(1→4)-α-rhamnosyl-(1→4)-α-rhamnosyl-(1→2)-β-glucoside, diosgenin 3-O-β-glucosyl-(1→4)-β-glucosyl-(1→6)-α-rhamnosyl-(1→4)-α-rhamnosyl-(1→2)-β-glucoside, diosgenin 3-O-β-glucosyl-(1→3)-β-glucosyl-(1→6)-α-rhamnosyl-(1→4)-α-rhamnosyl-(1→2)-β-glucoside, diosgenin 3-O-β-glucosyl-(1→6)-β-glucosyl-(1→4)-α-rhamnosyl-(1→4)-α-rhamnosyl-(1→2)-β-glucoside. Several of these saponins showed molluscicidal activity | [67] | |||||
| Herb: flavones: chrysoeriol-7-O[2′′-O-E-feruloyl]-β-d-glucoside, chrysoeriol, isorhamnetin-3-β-d-glucoside, and quercetin | [68] | |||||
| Herb EO: methyl (E)-1-propenyl disulfide (2.6–12.5%), benzaldehyde (up to 16.4%), dimethyl trisulfide (3.8–17.4%), allyl (E)-1-propenyl disulfide (7.9–12.5%), allyl methyl trisulfide (7.9–13.2%), diallyl trisulfide (2.8–10.5%), p-vinylguaiacol (5.2–6.5%), 5-methyl-1,2,3,4-tetrathiane (up to 6.1%) | [69] | |||||
| Aralia nudicaulis L. | Araliaceae | Wild sarsaparilla | root infusion taken as a blood tonic | root | [15] | |
| Rhizome: diacetylenes falcarinol and panaxydol; showed antimycobacterial activity | [70] | |||||
| Aralia spinosa L. | Araliaceae | Devil′s walking stick | root (poisonous) used for emetic, venereal diseases | root | [15] | |
| Leaf EO: (2E)-hexenal (13.8–29.8%), myrcene (13.9–15.1%), β-caryophyllene (8.2–15.7%), α-humulene (1.9–4.9%), germacrene D (28.0–37.3%), (E)-nerolidol (1.2–10.4%) | [71] | |||||
| Arnica cordifolia Hook. | Asteraceae | Arnica | pain reliever, anti-inflammatory | flowers | [18] | |
| Aerial parts: flavonoids: hispidulin, genkwanin, quercetin 3-methyl ether, quercetin 3-gentiobioside, quercetin 3-diglucoside, 6-methoxykaempferol 3-glucoside, isoquercitrin, astragalin, nepitrin, and glucoluteolin | [72] | |||||
| Leaves: pseudoguaianolide sesquiterpenoids carabrone, 2,3-dihydroaromaticin, 2,3-dihydroaromatin | [73] | |||||
| Artemisia biennis Willd. | Asteraceae | Biennial wormwood | poultice used on sores and wounds | plant | [15] | |
| Aerial parts EO: camphor (24.6%), artemisia ketone (11.4%), α-pinene (10.2%), 1,8-cineole (10.1%), germacrene D (5.3%) | [74] | |||||
| Aerial parts EO: (Z)-β-ocimene (34.7%), (E)-β-farnesene (40.0%); EO shows antimicrobial activity | [75] | |||||
| Aruncus dioicus (Walter) Fernald | Rosaceae | Goatsbeard | beaten root applied to bee stings | root | Phytochemistry of Eurasian varieties studied, but not North American varieties | [15] |
| Aruncus dioicus var. kamtschaticus (Maxim.) H. Hara a | Aerial parts: aruncin A, aruncin B, aruncide A, aruncide B, aruncide C; aruncin B showed cytotoxic activity on Jurkat T cells | [76] | ||||
| A. dioicus var. kamtschaticus a | Aerial parts: aruncin B; cytotoxic to Jurkat T cells (apoptosis, microtubule damage) | [77] | ||||
| A. dioicus var. kamtschaticus a | Aerial parts: palmitic acid, 10-nonacosanol, pentacosan-1-ol, phytol, β-sitosterol, β-sitosterol-3-O-β-d-glucopyranoside, 2,4-dihydroxycinnamic acid, hyperoside, uridine, and adenosine; β-sitosterol-3-O-β-d-glucopyranoside cytotoxic to HL-60 cells; 2,4-dihydroxycinnamic acid and hyperoside showed antioxidant (DPPH radical-scavenging) activity | [78] | ||||
| A. dioicus var. kamtschaticus a | Aerial parts: sambunigrin, prunasin, aruncide A, aruncide C, 1-O-caffeoyl-β-d-glucopyranose, and caffeic acid; aruncide C cytotoxic to HeLa cells; aruncide A cytotoxic to HL-60 cells; 1-O-caffeoyl-β-d-glucopyranose cytotoxic to MCF-7 cells | [79] | ||||
| A. dioicus (Italy) | Young shoots: 4-O-caffeoylglucose, chlorogenic acid, dicaffeoylglucose isomer I, dicaffeoylglucose isomer II, 3,5-dicaffeoylquinic acid, prunasin | [80] | ||||
| Asarum canadense L. | Aristolochi-aceae | Wild ginger | vermifuge (root), wounds (poultice of leaves) | root, leaves | [15] | |
| Leaves: chalcone glycosides (chalcononaringenin 2′,4′-di-O-glucoside and chalcononaringenin 2′-O-glucoside-4′-O-gentiobioside) and flavonol glycosides (quercetin 3-O-galactoside, quercetin 3-O-robinobioside, quercetin 3-O-β-d-galactopyranoside-7-O-α-l-rhamnopyranoside, kaempferol 3-O-galactoside, kaempferol 3-O-glucoside, kaempferol 3-O-galactoside-7-O-rhamnoside and iso-rhamnetin 3-O-rhamnosylgalactoside) | [81] | |||||
| Rhizome EO: methyleugenol (44.5%), linalyl acetate (41.1%), geraniol (7.4%), linalool (5.3%) | [82] | |||||
| Rhizome EO: linalool (5.0%), linalyl acetate (28.0%), methyleugenol (36.1%) | [83] | |||||
| Rhizome EO: methyleugenol (53.6%), linalool (12.5%), α-terpineol (6.6%) | [84] | |||||
| Rhizome EO: Linalool (19.4%), α-terpineol (5.9%), methyleugenol (38.5%) | [85] | |||||
| Asclepias tuberosa L. | Apocyn-aceae | Butterfly weed | cough | root | [22] | |
| Roots: steroids (ascandroside, Δ5-calotropin, Δ5-calotropin 3′-O-β-d-glucoside, Δ5-calotropin (3′S)-3′-thiazolidinone, Δ5-calotropin (3′R)-3′-thiazolidinone-S-oxide) | [86] | |||||
| Roots: Pregnane steroid (ikemagenin, lineolon, pleurogenin) glycosides | [87] | |||||
| Aerial parts: Pregnane steroid glycosides (tuberosides A1–L5) | [88] | |||||
| Aerial parts: Pregnane steroid glycosides (tuberosides B7 and B8) | [89] | |||||
| Roots: Pregnane steroid glycosides (tuberosides A2, B1, B2, C2, D1, D2, E2, F2, G1, H1, H2, I2, I3, J3, K3, M1, N1, O1, P1, and Q1) | [90] | |||||
| Baptisia australis (L.) R. Br. | Fabaceae | Wild indigo | cold infusion purgative/emetic | plant | [15] | |
| Flavonoids: afrormosin 7-O-β-d-glucoside, apigenin 7-O-β-d-glucoside, luteolin 7-O-β-d-glucoside, formononetin 7-O-β-d-glucoside, formononetin, and afrormosin; coumarin trifolirhizin | [91] | |||||
| Isoflavonoid: texasin 7-O-β-d-glucoside | [92] | |||||
| Alkaloids: (+)-sparteine and (–)-N-methylcytisine | [93] | |||||
| Berberis canadensis Mill. | Berberi-daceae | American barberry | bark infusion for diarrhea | bark | [15] | |
| Callus culture: isoquinoline alkaloid jatrorrhizine | [94] | |||||
| Betula nigra L. | Betulaceae | River birch | dysentery, colds | leaves | [15] | |
| Bud EO: benzyl alcohol (2.4–5.0%), nonanal (0.7–6.6%), eugenol (28.7–55.7%), tricosane (1.6–8.0%), pentacosane (1.3–8.8%), heptacosane (6.2–39.1%) | [95] | |||||
| Leaf EO: linalool (9.8–19.2%), eugenol (6.7–13.5%) | [95] | |||||
| Bark EO: hexanal (0.8–5.8%), (3Z)-hexenol (0–7.8%), o-methylanisole (0.3–5.3%), octanoic acid (0.2–7.4%), eugenol (trace-8.8%), decanoic acid (0.6–24.4%), dodecanoic acid (0.7–29.2%), palmitic acid (8.8–43.7%), heptacosane (2.5–24.3%) | [95] | |||||
| Bark: betulonaldehyde, lupeol, betulin, betulinic acid, betulin caffeate | [96] | |||||
| Buds: combretol, 5-hydroxy-3,4′,7-trimethoxyflavone | [97] | |||||
| Buds: 3,5-dihydroxy-4′,7-dimethoxyflavone | [98] | |||||
| Callicarpa americana L. | Lamiaceae | American beautyberry | Alabama tribe of Native Americans (not Cherokee) used a decoction of roots/branches sweat bath for rheumatism, fever | roots, branches | [15] | |
| Callicarpa americana | Leaf EO: 1-octen-3-ol (8.5%), β-pinene (8.8%), α-humulene (10.1%), humulene epoxide II (13.9%), intermediol (9.5%), callicarpenal (4.3%); the EO was selectively toxic toward the cyanobacterium Oscillatoria perornata | [99] | ||||
| Leaf EO: α-humulene, humulene epoxide II, intermediol, callicarpenal; intermediol and callicarpenal showed mosquito repellent activity (Aedes aegypti, Anopheles stephensi) | [100] | |||||
| Leaves: callicarpenal and intermediol; both showed tick repellent activity | [101] | |||||
| Fruiting branches: clerodane diterpenoids: 12(S),16ξ-dihydroxycleroda-3,13-dien-15,16-olide, 12(S)-hydroxy-16ξ-methoxycleroda-3,13-dien-15,16-olide, 12(S)-hydroxycleroda-3,13-dien-15,16-olide, 16ξ-hydroxycleroda-3,11(E),13-trien-15,16-olide, 3β,12(S)-dihydroxycleroda-4(18),13-dien-15,16-olide, and 12(S)-hydroxycleroda-3,13-dien-16,15-olide, 16ξ-hydroxycleroda-3,13-dien-15,16-olide, 2-formyl-16ξ-hydroxy-3-A-norcleroda-2,13-dien-15,16-olide. 12(S),16ξ-dihydroxycleroda-3,13-dien-15,16-olide, 16ξ-hydroxycleroda-3,11(E),13-trien-15,16-olide, 12(S)-hydroxycleroda-3,13-dien-16,15-olide, 16ξ-hydroxycleroda-3,13-dien-15,16-olide, 2-formyl-16ξ-hydroxy-3-A-norcleroda-2,13-dien-15,16-olide showed broad-spectrum cytotoxic activity | [102] | |||||
| Calycanthus floridus L. | Calycanth-aceae | Eastern sweetshrub | bark sap used on sores; bark infusion used on hives. Root strong emetic. | bark/root | [15] | |
| Flowers: anthocyanin pigments: cyanidin-3-glucoside, cyanidin-3-rutinoside | [103] | |||||
| Herb EO: α-pinene, 1,8-cineole (major), borneol, bornyl acetate | [104] | |||||
| Herb EO: (E)-β-ocimene (13.8%) | [105] | |||||
| C. floridus var. oblongifolius (Nutt.) Boufford and Spongberg (Iran) a | Floral EO: α-pinene (10.2%), β-pinene (8.6%), 1,8-cineole (33.1%), bornyl acetate (14.1%), α-terpinyl acetate (5.8%), elemol (8.2%) | [106] | ||||
| C. floridus var. oblongifolius (Iran) a | Stem EO: α-pinene (10.0%), β-pinene (7.2%), 1,8-cineole (31.7%), bornyl acetate (12.6%), α-terpinyl acetate (6.8%), elemol (9.0%) | [107] | ||||
| Caulophyllum thalictroides (L.) Michx. | Berberi-daceae | Blue cohosh | root decoction given as sedative and anticonvulsive; root taken internally to treat rheumatism | root | [15] | |
| Roots: alkaloids: N-methylcytisine, baptifoline, anagyrine, magnoflorine (major) | [108] | |||||
| Roots: quinolizidine alkaloids: N-methylcytisine, baptifoline (major), anagyrine | [109] | |||||
| Roots: alkaloids: thalictroidine, taspine, magnoflorine, anagyrine, baptifoline, 5,6-dehydro-α-isolupanine, α-isolupanine, lupanine, N-methylcytisine, and sparteine; N-methylcytisine showed teratogenic activity | [110] | |||||
| Roots: piperidine alkaloids (caulophyllumine A, caulophyllumine B), quinolizidine alkaloids (anagyrine, lupanine, O-acetylbaptifolin, N-methylcytisine), oleanane saponins (caulosides A, B, C, D, G, H, leonticin D, ciwujianoside A, saponin PE) | [111] | |||||
| Roots: alkaloids, O-acetylbaptifolin, anagyrine, caulophyllumine B, lupanine showed cytochrome-P450 inhibitory activity | [112] | |||||
| Roots: oleanane saponins: caulosides A, B, C, D, G; leonticin D, and 3-O-β-d-glucopyranosyl-(1→2)-α-l-arabinopyranosyl-echinocystic acid 28-O-α-l-rhamnopyranosyl-(1→4)-β-d-glucopyranosyl(1→6)-β-d-glucopyranoside | [113] | |||||
| Roots: 22 oleanane saponins; several showed cytotoxicity on HL-60 cells | [114] | |||||
| Roots: oleanane saponins caulosides A–D exert anti-inflammatory effects by inhibiting expression of iNOS and proinflammatory cytokines | [115] | |||||
| Ceanothus americanus L. | Rhamnaceae | New Jersey tea | root infusion taken for ′′bowel complaints′′ | root | [15] | |
| Root bark: peptide alkaloids (ceanothine A, B, C; ceanothamine A, B) | [116] | |||||
| Root bark: peptide alkaloid americine | [117] | |||||
| Root bark: peptide alkaloids (ceanothine D, E; frangulanine, adouetine-X, adouetine-Y) | [118] | |||||
| Cercis canadensis L. | Fabaceae | Redbud | bark infusion used for severe coughs | inner bark | [15] | |
| Bark EO: 1-hexanol (23.3%), hexanoic acid (18.2%), (2E)-hexenoic acid (3.4%) | [119] | |||||
| Chelone glabra L. | Plantagin-aceae | Balmony | herb used to treat skin problems; herb infusion taken as a digestive tonic | herb | [22] | |
| Leaves: iridoid glycoside catalpol | [120] | |||||
| Cichorium intybus L. a | Asteraceae | Chickory | infusion of root as tonic | root | [15] | |
| Sesquiterpene lactones (8-deoxylactucin, lactucin, lactupicrin) | [121] | |||||
| Leaves and roots: sesquiterpene lactones (lactucin, 11β,13-dihydrolactucin, jacquinelin, 8-desoxylactucin, lactucopicrin, crepidiaside B, loliolide), p-hydroxyphenylacetic acid methy and ethyl esters, cichoriside B, sonchuside A, ixerisoside D, magnolialide | [122] | |||||
| Root: sesquiterpene lactones (lactucin, lactucopicrin) | [123] | |||||
| Leaves and roots: sesquiterpene lactones (guaianolides, lactucin, lactucopicrin, 11β,13-dihydrolactucin) | [124] | |||||
| Flowers: anthocyanin pigments: delphinidin 3,5-di-O-(6-O-malonyl-β-d-glucoside) and delphinidin 3-O-(6-O-malonyl-β-d-glucoside)-5-O-β-d-glucoside; delphinidin 3-O-β-d-glucoside-5-O-(6-O-malonyl-β-d-glucoside) and delphinidin 3,5-di-O-β-d-glucoside | [125] | |||||
| Cimicifuga racemosa (L.) Nutt. (syn. Actaea racemosa L.) | Ranuncu-laceae | Black cohosh | root used to stimulate menstruation; root infusion used for rheumatism, coughs, colds | root | [15] | |
| Rhizome: triterpene glycosides (actein, 27-deoxyactein, cimicfugoside M, and cimicifugoside) | [126] | |||||
| Rhizome: triterpene glycosides (cimiaceroside A, 25-O-methylcimigenol-3-O-β-d-xylopyranoside, 27-deoxyactein, 23-O-acetylshengmanol-3-O-β-d-xylopyranoside, 16β,23;22β,25-diepoxy-12β-acetoxy-3β,23,24β-trihydroxy-9,19,cyclolanost-7-ene-3-O-β-d-xylopyranoside) | [127] | |||||
| Rhizome: triterpene glycosides (12β-acetoxycimigenol-3-O-β-d-xylopranoside, 25-acetylcimigenol xyloside, cimigenol-3-O-β-d-xylopyranoside, acetin, 27-deoxyacetin, cimicifugoside H-1, 23-O-acetylshengmanol 3-O-β-d-xylopranoside, foetidinol-3-O-β-xyloside, cimicifugoside H-2, 25-O-methylcimigenol xyloside, 21-hydroxycimigenol-3-O-β-d-xylopyranoside, 24-epi-7,8-didehydrocimigenol-3-xyloside, cimidahurinine, cimidahurine, and cimifugin) | [128] | |||||
| Rhizome: triterpene glycosides (cimiracemosides A–H, 27-deoxyactein, 26-deoxycimicifugoside, actein, acetyl shengmanol xyloside, cimicifugoside (cimigenol-3-O-β-d-xylopyranoside), cimiaceroside A, 12β-hydroxycimigenol-3-O-β-d-xylopyranoside, and 12β-hydroxycimigenol-3-O-α-l-arabinopyranoside) | [129] | |||||
| Rhizome: triterpene glycosides (cimigenol 3-O-α-l-arabinopyranoside, 25-O-methoxycimigenol 3-O-α-l-arabinopyranoside, 12β-hydroxycimigenol 3-O-α-l-arabinopyranoside, 27-deoxyactein, actein, cimiracemoside F, cimiracemoside G, cimiracemoside H, 25-O-acetyl-12β-hydroxycimigenol 3-O-α-l-arabinopyranoside, 12β,21-dihydroxycimigenol 3-O-α-l-arabinopyranoside, 23-O-acetylshengmanol 3-O-α-l-arabinopyranoside, (22R,23R,24R)-12β-acetyloxy-16β,23:22,25-diepoxy-23,24-dihydroxy-9,19-cyclolanostan-3β-yl α-l-arabinopyranoside) | [130] | |||||
| Rhizome: triterpene glycosides (cimiracemoside H, 26-deoxyactein, 23-O-acetylshengmanol 3-O-β-d-xylopyranoside, actaeaepoxide 3-O-β-d-xylopyranoside, 25-O-acetylcimigenol 3-O-α-l-arabinopyranoside, 25-O-acetylcimigenol 3-O-β-d-xylopyranoside) | [131] | |||||
| Rhizome: triterpene glycosides (actein, 23-epi-26-deoxyactein, 23-O-acetylshengmanol-3-O-β-d-xylopyranoside, cimiracemoside D, 25-O-acetylcimigenol-3-O-β-d-xylopyranoside, and cimigenol) | [132] | |||||
| Rhizome: triterpene xyloside, 9,10-seco-9,19-cyclolanostane xyloside (cimipodocarpaside) | [133] | |||||
| Rhizome: triterpene xylosides (cimigenol xyloside, 26-deoxyactein, cimicifugoside H-1, and 24-acethylhydroshengmanol xyloside) | [134] | |||||
| Rhizome: triterpene xylosides (isocimipodocarpaside, 23-epi-26-deoxycimicifugoside, 23-epi-26-deoxyactein, 25-anhydrocimigenol xyloside, 23-O-acetylshengmanol xyloside, 25-O-acetylcimigenol xyloside, 3′-O-acetylcimicifugoside H-1) | [135] | |||||
| Rhizome: Cimicidol-3-O-β-d-xyloside (slightly hepatotoxic) | [136] | |||||
| Rhizome: fukiic and piscidic acid esters: (2-E-caffeoylfukiic acid (fukinolic acid), 2-E-feruloylfukiic acid (cimicifugic acid A), 2-E-isoferuloylfukiic acid (cimicifugic acid B), 2-E-feruloylpiscidic acid (cimicifugic acid E) and 2-E-isoferuloylpiscidic acid (cimicifugic acid F), free caffeic, ferulic and isoferulic acids) | [137] | |||||
| Rhizome: phenylpropanoid esters (cimicifugic acid D, petasiphenone, cimiciphenol, cimiciphenone | [138] | |||||
| Rhizome: phenylpropanoid esters (cimiracemates A–D) | [139] | |||||
| Rhizome: phenylpropanoids (caffeic acid, isoferulic acid, ferulic acid), triterpene xylosides (cimicifugoside H-1, cimiracemoside A, cimicifugoside H-2, (26R)-actein, 26-deoxycimicifugoside, (26S)-actein, 23-epi-26-deoxyactein, 23-acetoxy-shengmanol-3-O-β-d-xyloside, 26-deoxyactein, 25-acetoxy-cimigenol-3-O-α-l-arabinoside, 25-acetoxy-cimigenol-3-O-β-d-xyloside, cimigenol-3-O-α-l-arabinoside, cimigenol-3-O-β-d-xyloside) | [140] | |||||
| Rhizome: polyphenolics (actaealactone, cimicifugic acid G, protocatechuic acid, protocatechualdehyde, p-coumaric acid, caffeic acid, methyl caffeate, ferulic acid, ferulate-1-methyl ester, isoferulic acid, 1-isoferuloyl-â-d-glucopyranoside, fukinolic acid, and cimicifugic acids A, B, and D–F) | [141] | |||||
| Rhizome: alkaloids (cyclocimipronidine, cimipronidine methyl ester, cimipronidine, dopargine, salsolinol, 3-hydroxytyrosol 3-O-glucoside) | [142] | |||||
| Collinsonia canadensis L. | Lamiaceae | Heal-all | decoction taken as emetic | leaves | [15] | |
| Leaf EO: germacrene D (46.0%), β-caryophyllene (5.3%), elemicin (3.6%), β-elemene (3.3%) | [143] | |||||
| Roots: triterpene glycosides, hederagenin-3-O-α-l-arabinopyranoside (leontoside A), 3-O-α-l-arabinopyranosylcollinsogenin (collinsonin), 3-O-β-d-glucopyranosyl-(1′′→3′)-α-l-arabinopyranosylhederagenin (collinsonidin) | [144] | |||||
| Leaf and stem exudates: flavonoids, 2,5-dihydroxy-6,7-dimethoxyflavanone, baicalein-6,7-dimethyl ether, norwogenin-7,8-dimethyl ether, and tectochrysin (5-hydroxy-7-methoxyflavone) | [145] | |||||
| Conyza canadensis (L.) Cronquist (syn. Erigeron canadensis L.) | Asteraceae | Horseweed | leaves used for toothache | leaves | [21] | |
| decoction of herb used to treat diarrhea | herb | [23] | ||||
| Mikasuki and Seminole Native Americans used the plant to treat sore throats and respiratory complaints | [146] | |||||
| Whole plant: β-sitosterol, stigmasterol, β-sitosterol 3-O-β-d-glucoside, harmine, and sphingolipid | [147] | |||||
| Whole plant: sphingolipids, 1,3,5-trihydroxy-2-hexadecanoylamino-(6E,9E)-heptacosdiene, 1,3,5-trihydroxy-2-hexadecanoylamino-(6E,9E)-heptacosdiene-1-O-glucopyranoside, 1,3-dihydroxy-2-hexanoylamino-(4E)-heptadecene; p-hydroxybenzoic acid, 3,5-dihydroxybenzoic acid, 3,5-dimethoxybenzoic acid, 3β-hydroxyolean-12-en-28-oic acid, and 3β-erythrodiol | [148] | |||||
| Aerial parts: triterpenoid erigeronol (showed potent anti-melanoma cytotoxicity) | [149] | |||||
| Whole plant: conyzolide, conyzoflavone (both showed antimicrobial activities) | [150] | |||||
| Whole plant: 8R,9R-dihydroxymatricarine methyl ester, matricarine methyl ester, matricarine lactone, 3β,16β,20β–tritrihydroxytaraxast-3-O-palmitoyl ester, friedelin, friedelinol, β-sitosterol, α-spinasterol, 3-isopropenyl-6-oxoheptanoic acid, 9-hydroxy-10Z,12E-octadecenoic acid, (+)-hydroxydihydroneocarvenol, 3′,4′,5,7-tetrohydroxydihydroflavone, 9,12,13-trihydroxy-10(Z)-octadecenoic acid | [151] | |||||
| Whole plants: phenylprobanoyl esters (rel-(1S,2R,3R,5S,7R)-methyl 7-caffeoyloxymethyl-2-hydroxy-3-feruloyloxy-6,8-dioxabicyclo[3.2.1]octane-5-carboxylate, rel-(1S,2R,3R,5S,7R)-methyl 7-feruloyloxymethyl-2-hydroxy-3-feruloyloxy-6,8-dioxabicyclo[3.2.1]octane-5-carboxylate, and rel-(1R,2R,3R,5S,7R)-methyl 7-feruloyloxymethyl-2-feruloyloxy-3-hydroxy-6,8-dioxabicyclo[3.2.1]octane-5-carboxylate) | [152] | |||||
| Aerial parts: enyne derivatives, (2Z,8Z)-matricaria acid methyl ester, (4Z,8Z)-matricaria lactone, and (4Z)-lachnophyllum lactone | [153] | |||||
| Aerial parts: (4Z)-lachnophyllum lactone, (4Z,8Z)-matricaria lactone, (2Z,8Z)-matricaria acid methyl ester; (4Z)-lachnophyllum lactone and (4Z,8Z)-matricaria lactone showed antifungal activity against Aspergillus niger, Cladosporium sp., and Penicillium digitatum | [154] | |||||
| Flowering parts: polyphenolic-polysaccharide (anticoagulant, antiplatelet activity) | [155] | |||||
| Roots: dihydropyranones conyzapyranone A and B; 4Z,8Z-matricaria-γ-lactone, 4E,8Z-matricaria-γ-lactone, 9,12,13-trihydroxy-10(E)-octadecenoic acid, epifriedelanol, friedelin, taraxerol, simiarenol, spinasterol, stigmasterol, β-sitosterol, and apigenin; conyzapyranone B, 4E,8Z-matricaria-γ-lactone, and spinasterol showed cytotoxic activity | [156,157] | |||||
| Roots: triterpenoid 3β-erythrodiol (inhibits MKN-45 gastric cell proliferation) | [158] | |||||
| Roots: salicylic acid, methyl gallate | [159] | |||||
| Roots: lanostane triterpenoids conyzagenin-A, conyzagenin-B | [160] | |||||
| Aerial parts EO: limonene (76.0%), α-santalene (5.8%), δ-3-carene (3.9%), myrcene (3.6%) | [161] | |||||
| Aerial parts EO: limonene (57.9–81.1%), (E)-β-ocimene (0.7–9.1%), trans-α-bergamotene (5.6–8.9%), (Z)-β-farnesene (tr-11.1%). | [162] | |||||
| Aerial parts EO: limonene (50.0–70.3%) and (E)-β-ocimene (4.0–7.5%) | [163] | |||||
| Aerial parts EO: limonene (70.0%), trans-α-bergamotene (7.0%) | [164] | |||||
| Aerial parts EO: limonene (77.7–89.4%), trans-α-bergamotene (1.5–3.8%), β-pinene (0.8–6.6%), carvone (0.5–1.8%) | [165] | |||||
| Aerial parts EO: (E)-β-Farnesene (14.6%), spathulenol (14.1%) and limonene (12.3%) | [166] | |||||
| Aerial parts EO: limonene (31.2%), camphene (14.2%) and germacrene D (11.3%) | [167] | |||||
| Aerial parts EO: limonene (68.3%), δ-3-carene (15.9%) | [168] | |||||
| Root EO: (2Z,8Z)-matricaria ester (88.2–93.9%) | [169] | |||||
| Coreopsis tinctoria Nutt. | Asteraceae | Tickseed | root tea for diarrhea | root | [15] | |
| Plant: polyacetylenes, (2S)-(3Z,11E)-decadiene-5,7,9-triyne-1,2-diol and (2R)-(3E,11Z)-decadiene-5,7,9-triyne-1,2-diol | [170] | |||||
| Plant: seven compounds made up the major contributions of antioxidant activity in C. tinctoria, including okanin, isookanin, marein, flavanomarein, 5,7,3′,5′-tetrahydroxyflavanone-7-O-glucoside, 3,5-dicaffeoylquinic acid, and chlorogenic acid | [171] | |||||
| Flowers: C14 polyacetylene glycosides coreosides A–D | [172] | |||||
| Buds: C14 polyacetylene glycosides coreosides E and F | [173] | |||||
| Flowers: C14 polyacetylene glycosides coreosides A, B, D, and E | [174] | |||||
| Flowers: chalcone marein, flavanone flavanomarein | [175] | |||||
| Flowers: chalcone okanin-4′-O-β-(6′′-O-malonyl)glucopyranoside; flavonoids flavanomarein okanin-4′-O-β-d-glucopyranoside, quercetagitin 7-O-β-d-glucopyranoside, (2R,3R)-dihydroquercetin 7-O-β-d-glucopyranoside, okanin, quercetin, butein, 2S-3′,4′,7,8-tetrahydroxyflavanone, (2R,3R)-3,3′,5,5′,7-pentahydroxyflavanone, (2R,3R)-3,4′,5,6,7-penta-hydroxyflavanone, and 2S-3′,5,5′,7-tetrahydroxy-flavanone | [176] | |||||
| Flowers: flavonoids (flavanomarein, flavanokanin, quercetagitin-7-O-glucoside, marein) | [177] | |||||
| Flowers: flavonoids ((+)-catechin, kaempferol-3-O-d-glycoside, quercetin-3-O-glycoside, quercetin-3-O-rutinoside | [178] | |||||
| Flowers: flavonoids (taxifolin, taxifolin-7-O-β-d-glucopyranoside, isookanin, flavanomarein, quercetagetin-7-O-β-d-glucopyranoside, 5,7,3′,5′-tetrahydroxyflavanone-7-O-β-d-glucopyranoside), chalcones (okanin, marein), and phenolic acids (chlorogenic acid, 3,5-di-O-caffeoylquinic acid, 4,5-di-O-caffeoylquinic acid) | [179] | |||||
| Flowers: quercetagitin-7-O-glucoside, marein (major), 1,3-dicaffeoylquinic acid, okanin, acetylmarein | [180] | |||||
| Flowers: taxifolin-7-O-glucoside, flavanomarein, quercetagetin-7-O-glucoside, okanin 4′-O-glucoside, okanin, chlorogenic acid | [181] | |||||
| Flowers: chlorogenic acid, (R/S)-flavanomarein, butin-7-O-β-d-glucopyranoside, isookanin, taxifolin, 5,7,3′,5′-tetrahydroxyflavanone-7-O-β-d-glucopyranoside, marein, and okanin | [182] | |||||
| Fruits: flavonoids (marein, flavanomarein, quercetagetin-7-O-glucoside, okanin aurone, leptosidin, luteolin, apigenin) and phenolic acids (chlorogenic acid, caffeic acid) | [183] | |||||
| Floral EO: limonene (11.3%), α-bergamotene (7.3%) | [184] | |||||
| Cornus florida L. | Cornaceae | Dogwood | bark chewed for headache | bark | [15] | |
| bark decoction used for fevers, body aches; bark poultice used on sores/ulcers | bark | [22] | ||||
| Bark: saponins (sarsapogenin-O-β-d-xylopyranosyl-(1→2)-β-d-galactopyranoside and sarsapogenin-O-β-d-glucopyranosyl-(1→2)-β-d-galactopyranoside) | [185] | |||||
| Datura stramonium L. | Solanaceae | Jimson weed | leaf poultice applied to boils; leaves smoked for asthma | leaves | [15] | |
| Root culture: tropane alkaloid (−)-hyoscyamine | [186] | |||||
| Root culture: tropane alkaloids (hyoscyamine and scopolamine) | [187] | |||||
| Seeds: tropane alkaloid (−)-hyoscyamine | [188] | |||||
| Leaves: tropane alkaloids (hyoscyamine and scopolamine) | [189] | |||||
| Diospyros virginiana L. | Ebenaceae | Persimmon | bark infusion for venereal diseases, sore throat and mouth; syrup for oral thrush, bloody discharge from bowels | bark | [17] | |
| Bark: binaphthoquinone isodiospyrin | [190] | |||||
| Fruits: polyphenolics (methyl gallate, gallic acid, luteolin, quercetin, myricetin, yricetin 3-O-α-rhamnoside, myricetin 3-O-β-glucoside, myricetin 3-O-β-glucuronide) | [191] | |||||
| Roots: 4-hydroxy-5,6-dimethoxynaphthalene-2-carbaldehyde, 12,13-didehydro-20,29-dihydrobetulin, 7-methyljuglone, diospyrin, isodiospyrin, shinanolone, lupeol, betulin, betulinic acid, betulinaldehyde, and ursolic acid | [192] | |||||
| Epilobium angustifolium L. | Onagraceae | Fireweed | eye conditions due to asthma, allergies | herb | [18] | |
| Herb: quercetin 3-O-(6′′-galloyl)-galactoside, kaempferol 3-O-(6′-p-coumaroyl)-glucoside, quercetin 3-O-glucuronide, oenothein B; oenothein B inhibited the endopeptidases neutral endopeptidase (NEP) and angiotensin converting enzyme (ACE) | [193] | |||||
| Herb: oenothein B (a dimeric macrocyclic ellagitannin) inhibits proliferation of SK-N-SK and PC-3 cells | [194] | |||||
| Herb: oenothein B enhances IFNγ production by lymphocytes | [195] | |||||
| Herb: ellagitannins (oenothein B, oenothein A, tetramer, pentamer, hexamer, heptamer) | [196] | |||||
| Flowers and leaves: ellagitannins (oenothein B, oenothein A, tetramer, pentamer, hexamer, heptamer) | [197] | |||||
| Equisetum hyemale L. | Equiset-aceae | Horsetail | infusion taken for kidneys | plant | [15] | |
| Stems: (E)-feruloyl-4-β-glucoside, (Z)-feruloyl-4-β-glucoside, (E)-caffeoyl-3-β-glucoside, kaempferol-3-sophoroside, Kaempferol-3-sophoroside-7-β-glucoside, herbacetin-3-sophoroside-8-β-glucoside | [198] | |||||
| Aerial parts: 2-(sophorosyl)-1-(4-hydroxyphenyl)ethenone | [199] | |||||
| Eryngium yuccifolium Michx. | Apiaceae | Baneberry, Rattlesnake master | remedy for snakebites | root | [15,17] | |
| remedy for snakebites | Plant extracts showed inhibition of Crotalus proteases | [200] | ||||
| urinary-tract inflammation modulator | root | [201] | ||||
| Aerial parts EO: polyacetylenes (falcarinone, falcarinol, yuccifolol, 1,8-heptadecadiene-4,6-diyne-3,9-diol) | [202] | |||||
| Leaf EO: α-pinene (7.6%), terpinolene (17.8%), β-caryophyllene (6.2%), germacrene D (18.3%), bicyclogermacrene (8.8%), falcarinol (9.6%) | [202] | |||||
| Root EO: α-pinene (4.7%), terpinolene (25.8%), 2,3,6-trimethylbenzaldehyde (13.9%), trans-β-bergamotene (18.6%) | [202] | |||||
| Whole plant: triterpenoid saponins (eryngiosides A–L, saniculasaponin III); flavonoid (kaempferol) glycosides; polyphenolics (caffeates) | [203] | |||||
| Root: Triterpenoid saponins | [204] | |||||
| The phytochemistry of E. yuccifolium has been reviewed | [205] | |||||
| Erythronium americanum Ker Gawl. | Liliaceae | Troutlily | leaves crushed and juice poured over wounds | leaves | [15] | |
| α-Methylenebutyrolactone | [206] | |||||
| Eupatorium maculatum L. | Asteraceae | Joe-Pye weed | root infusion for kidney, dropsy | root | [15] | |
| Roots: pyrrolyzidine alkaloids (echinatine, trachelanthamidine) | [207] | |||||
| Leaves: pyrrolizidine alkaloid (lycopsamine) and guaianolide sesquiterpene lactone (cumambrin B) | [208] | |||||
| Eupatorium perfoliatum L. | Asteraceae | Boneset | infusion of the plant taken as a tonic, for colds, sore throat, and influenza | plant | [15] | |
| Aerial parts: guianolide and germacranolide sesquiterpene lactones; flavonoids (eupafolin, hispidulin, patuletin, and kaempferol) | [209] | |||||
| Aerial parts: guianolide and germacranolide sesquiterpene lactones | [210] | |||||
| Leaves: polyphenolics (protocatechuic acid, hyperoside, quercetin, rutin) | [211] | |||||
| Aerial parts: extracts show anti-inflammatory activity, but not immunostimulatory activity | [212] | |||||
| Aerial parts: caffeic acid derivatives (5-caffeoylquinic acid (chlorogenic acid), 3-caffeoylquinic acid (neochlorogenic acid) and 3,5-dicaffeoylquinic acid, 2,5-dicaffeoylglucaric acid, 3,4-dicaffeoylglucaric acid, and 2,4- or 3,5-dicaffeoylglucaric acid) | [213] | |||||
| Aerial parts: glycosides of kaempferol and quercetin; quaianolides | [214] | |||||
| Aerial parts EO: (E)-Anethole (16.5%), carvone (7.6%), selin-11-en-4α-ol (5.5%) | [215] | |||||
| Fagus grandifolia Ehrh. | Fagaceae | American beech | nuts chewed for worms | nuts | [15] | |
| Bark: monolignols [(Z)-coniferyl alcohol, (Z)-sinapyl alcohol, (Z) coniferin, (Z)-isoconiferin, (Z)-syringin] | [216] | |||||
| Frasera caroliniensis Walter | Gentian- aceae | American Columbo | root used to treat dysentery | root | [15] | |
| Root: xanthones (1-hydroxy-2,3,4,7-tetramethoxyanthone, 1-hydroxy-2,3,4,5-tetramethoxyxanthone, 1-hydroxy-2,3,7-trimethoxyxanthone, 1-hydroxy-2,3,5-trimethoxyxanthone, swerchirin, 1,3-dihydroxy-4,5-dimethoxyxanthone) | [217] | |||||
| Plant: iridoid (loganic acid), secoiridoid (gentiopicroside), and xanthones [1,3-diOH-4,5-diMeO-xanthone, 1-OH-2,3,5-triMeO-xanthone, 1-OH-2,3,4,5-tetraMeO-xanthone, 1-OH-2,3,4,7-tetraMeO-xanthone, 1,8-diOH-3,5-diMeO-xanthone (swerchirin)] | [218] | |||||
| Fraxinus americana L. | Oleaceae | American ash | tonic of inner bark taken for liver and stomach problems | bark | [15] | |
| Bark: oleoside, syringin, hydroxypinoresinol glycoside, verbascoside, ligustroside | [219] | |||||
| Leaves: secoiridoid glucosides (demethylligstroside, (2″R)-2″-hydroxyoleuropein, (2″S)-2″-hydroxyoleuropein, fraxamoside, frameroside, oleoside dimethyl ester, oleuropein, ligstroside, nuezhenide, (2″R)-2″-methoxyoleuropein, (2″S)-2″-methoxyoleuropein) | [220] | |||||
| Seeds: catechins (epicatechin, catechin-3-O-gallate, epigallocatechin, epigallocatechin-3-O-gallate, epigallocatechin-(4β-8)-epicatechin, epicatechin-3-O-gallate-(4β-8)-epigallocatechin-3-O-gallate), procyanidins (procyanidin B-1, procyanidin B-3) | [221] | |||||
| Geranium maculatum L. | Geraniaceae | Wild geranium | cuts, sores, oral thrush | plant | ||
| Plant EO: citronellol (38%), geraniol (16%), citronellyl formate (10.4%), and linalool (6.45%) | [222] | |||||
| Hamamelis virginiana L. | Hamameli-daceae | Witch hazel | bark infusion used on sores | bark | [15] | |
| Bark: hamamelitannin cytotoxic to HT-29 colon tumor cells | [223] | |||||
| Leaves: gallotannins (hydrolyzable tannins: monogalloyl, heptagalloyl, octagalloyl, and nonagalloyl hexoses), caffeoylquinic acids (3-, and 5-), kaempferol glycoside | [224] | |||||
| Bark: polymeric proanthocyanidins (condensed tannins). | [225] | |||||
| Bark: tannins, antioxidant, cytotoxic to SK-Mel-28 melanoma cells | [226] | |||||
| Bark: condensed (proanthocyanidins) and hydrolyzable (galloylhamameloses) tannins | [227] | |||||
| Helenium autumnale L. | Asteraceae | Sneezeweed | root infusion used to prevent menstruation after childbirth; dried leaves used to induce sneezing | roots, leaves | Apparently the root extract has not been examined | [15] |
| Aerial parts: dihydromexicanin E | [228] | |||||
| Aerial parts: flexuosin A | [229] | |||||
| Aerial parts: helenalin | [230] | |||||
| Aerial parts: tenulin | [231] | |||||
| Helenalin is cytotoxic (human epithelial type 2, HEp-2, cells) | [232] | |||||
| Whole plant: carolenin and carolenalin | [233] | |||||
| Flowers: helenalin, autumnolide, mexicanin I; helenalin is cytotoxic | [234] | |||||
| Plant: dihydroflorilenalin | [235] | |||||
| Plant: 4-O-tigloyl-11,13-dihydroautumnolide | [236] | |||||
| Hydrastis canadensis L. | Ranuncu-laceae | Goldenseal | sedative, anti-inflammatory; sores, wounds, cancer | root | [15] | |
| Rhizomes: alkaloids (berberine, 8-oxotetrahydrothalifendine, canadine, and β-hydrastine); berberine shows antitubercular activity | [237] | |||||
| Rhizomes: berberine alkaloids (berberine, β-hydrastine, canadine and canadaline); berberine is antibacterial. | [238] | |||||
| Rhizomes: alkaloids (berberine, canadaline, canadine, β-hydrastine, and isocorypalmine) | [239] | |||||
| Rhizomes: alkaloids (hydrastinine, hydrastine, canadaline, berberine, canadine) | [240] | |||||
| Leaves: 3,4-dimethoxy-2-(methoxycarbonyl)benzoic acid, 3,5,3′-trihydroxy-7,4′-dimethoxy-6,8-C-dimethyl-flavone, (±)-chilenine, (2R)-5,4′-dihydroxy-6-C-methyl-7-methoxy-flavanone, 5,4′-dihydroxy-6,8-di-C-methyl-7-methoxy-flavanone, noroxyhydrastinine, oxyhydrastinine, 4′,5′-dimethoxy-4-methyl-3′-oxo-(1,2,5,6-tetrahydro-4H-1,3-dioxolo-[4′,5′:4,5]-benzo[1–e]-1,2-oxazocin)-2-spiro-10-phtalan | [241] | |||||
| Leaves: flavonoids (sideroxylin, 8-desmethyl-sideroxylin, and 6-desmethyl-sideroxylin); inhibit N or A multidrug resistance pump; synergistic antibacterial activity with berberine | [242] | |||||
| Hypericum gentianoides (L.) Britton, Sterns and Poggenb. | Hyperic-aceae | St. John′s wort | root poultice used for stakebite | root | [15] | |
| Aerial parts: acyl-phloroglucinols (saroaspidin A, uliginosin A, hyperbrasilol C) | [243] | |||||
| Aerial parts: acyl-phloroglucinols (3′-prenyl-phlorisobutyrophenone, saroaspidin A, uliginosin A, hyperbrasilol C) | [244] | |||||
| Aerial parts: chlorogenic acid, hyperoside, isoquercitrin, quercitrin, quercetin, at least 9 acyl-phloroglucinols (not identified). The acyl-phloroglucinols fraction reduced prostaglandin E2 synthesis in mammalian macrophages | [245] | |||||
| Hypericum hypericoides (L.) Crantz | Hypericaceae | St. John′s wort | root poultice used for stakebite | root | [15] | |
| Roots: prenylated benzophenones (clusianone, 7-epi-clusianone, 18-hydroxy-7-epi-clusianone, 18-hydroxyclusianone, and 18-hydroxyhyperibone K) | [246] | |||||
| Iris versicolor L. | Iridaceae | Blue flag, Snake lily | eyewash | root | [18] | |
| powerful cathartic | rhizome | [24] | ||||
| root poultice used to treat sores | rhizome | [23] | ||||
| Rhizomes: iridals (17,26-dihydroxyiridal, 16-hydroxyiridal, 17-hydroxyiridal, 26-hydroxyiridal, 10-deoxy-17-hydroxyiridal, iriversical) | [247] | |||||
| Juglans nigra L. | Jugland-aceae | Black walnut | bark infusion used on sores | bark | [15] | |
| Bark: juglone, α-hydroxyjuglone-4-glucoside, myricetin, myricitrin, sakuranetin, sakuranin, and neosakuranin | [248] | |||||
| Unripe fruit: naphthoquinones (dihydroplumbagin, 3-methylplumbagin, isoplumbagin) | [249] | |||||
| Husk: naphthoquinones (juglone, plumbagin, regiolone), sterols (stigmasterol, β-sitosterol), flavonoids (taxifolin, kaempferol, quercetin, myricetin) | [250] | |||||
| Leaf EO: α-Pinene (6.3–11.4%), β-caryophyllene (17.3–20.4%), germacrene D (7.1–22.5%), juglone (1.0–8.8%) | [251] | |||||
| Juncus effusus L. | Juncaceae | Common rush | plant decoction used as emetic | plant | [15] | |
| Medullae: p-Coumaroyl glycerides (juncusyl esters A and B) | [252] | |||||
| Plant: cinnamoylglycerols (1-O-coumaroylglycerol, 1-O-feruloylglycerol, 1-O-coumaroylglycerol, juncusyl ester A, 1-O-(4-methoxycinnamoyl)glycerol, 1-O-(4-methoxycinnamoyl)-2,3-O-isoppropylidene-sn-glycerol, 2-O-coumaroylglycerol, 2-O-(4-methoxycinnamoyl)glycerol, 1,2-di-O-feruloylglycerol, 1,3-di-p-coumaroylglycerol) | [253] | |||||
| Plant: 8-dihydroxy-1,7-dimethyl-6-vinyl-10,11-dihydro-dibenz[b,f] oxepin (showed brine shrimp lethality) | [254] | |||||
| Stems: cycloartane glucosides (juncosides II–V) | [255] | |||||
| Plant: cycloartane triterpenoids (lagerenol, cycloartane-3β,24,25-triol, cycloart-22Z-ene-3β,25-diol, sterculin A, cycloart-25-ene-3β,24-diol, 3-hydroxycycloart-25-ene-24-one, 24,25-epoxycycloartan-3β-ol) | [256] | |||||
| Plant: cycloartane glucoside juncoside I | [257] | |||||
| Medullae: phenanthrenes (junceunins E–G, dehydrojuncuenins D–E); junceunin E cytotoxic to MCF-7 and HeLa cells | [258] | |||||
| Underground parts: phenanthrenes (dehydroeffusol, juncusol); compounds showed UVA light-enhanced antimicrobial activities due to DNA binding | [259] | |||||
| Plant: phenanthrenes (4-ethenyl-9,10-dihydro-1,8-dimethyl-2,7-phenanthrenediol, 4-ethenyl-9,10-dihydro-7-methoxy-1,8-dimethyl-2-phenanthrenol, 4-ethenyl-9,10-dihydro-3,8-dimethyl-1,7-phenanthrenediol, 4-ethenyl-9,10-dihydro-7-methoxy-3,8-dimethyl-1-phenanthrenol, 4-ethenyl-9,10-dihydro-7-hydroxy-8-methyl-2-phenanthrenecarboxylic acid) | [260] | |||||
| Plant: phenanthrenes (junceunin F 2-methyl ether, 4-formyl-9,10-dihydro-3,7-dihydroxy-2,8-dimethylphenanthrene, 5-ethenyl-9,10-dihydro-1,7-dimethyl-2,3-phenanthrenediol, 9,10-dihydro-1,7-dihydroxy-4-(1-hydroxyethyl)-2,8-dimethylphenanthrene, 9,10-dihydro-6,6-dihydroxy-5-(1-hydroxyethyl)-1,7-dimethylphenanthrene, 9,10-dihydro-2,6-dihydroxy-5-(1-methoxyethyl)-1,7-dimethylphenanthrene, 4-ethenyl-9,10-dihydro-7-hydroxy-8-methyl-1-phenanthrenecarboxylic acid) | [261] | |||||
| Plant: phenanthrenes (2-hydroxy-7-(hydroxymethyl)-1-methyl-5-vinyl-9,10-dihydrophenanthrene, 2-hydroxy-6-(hydroxymethyl)-1-methyl-5-vinyl-9,10-dihydrophenanthrene, 2-hydroxy-5-(hydroxymethyl)-1,7-dimethyl-9,10-dihydrophenanthrene, 2,7-dihydroxy-5-(hydroxymethyl)-1,8-dimethyl-9,10-dihydrophenanthrene, 2-hydroxy-5-(hydroxymethyl)-7-methoxy-1,8-dimethyl-9,10-dihydrophenanthrene, 5-(1-ethoxy)-2,7-dihydroxy-1,8-dimethyl-9,10-dihydrophenanthrene, 2-hydroxy-1,7-dimethyl-9,10-dihydrophenanthro-[5,6-b]-4′,5′-dihydro-4′,5′-dihydroxyfuran) | [262] | |||||
| Plant: phenanthrene glucosides (Effusides I–V) | [263] | |||||
| Aerial parts: phenanthrenes (7-carboxy-2-hydroxy-1-methyl-5-vinyl-phenanthrene, 2,7-dihydroxy-1-methyl-5-aldehyde-9,10-dihydrophenanthrene, dehydroeffusol, dehydrojuncusol, 7-carboxy-2-hydroxy-1-methyl-5-vinyl-9,10-dihydrophenanthrene, 8-carboxy-2-hydroxy-1-methyl-5-vinyl-9,10-dihydrophenanthrene, effusol, and juncusol; effusol and juncusol showed anxiolytic and sedative activities) | [264] | |||||
| Medullae: diterpenoid effusenone A, phenanthrene 5-(hydroxymethyl)-1-methylphenanthrene-2,7-diol, pyrenes 1-methylpyrene-2,7-diol and 7-methoxy-8-methylpyren-2-ol | [265] | |||||
| Medullae: phenanthrenes (effusol, dehydroeffusol, dehydroeffusal) | [266] | |||||
| Medullae: phenanthrenes (effusol, dehydroeffusol, juncusol, dehydrojuncusol, juncuenin B, dehydrojuncuenin B, juncuenin D, and effususol A), flavonoids (luteolin and luteolin 5-methyl ether), and 4-hydroxy-2,3-dimethyl-2-nonen-4-olide | [267] | |||||
| Plant: tetrahydropyrene glucosides (4,5,9,10-tetrahydro-2,7-dihydroxy-1,6-dimethylpyrene monoglucoside and diglucoside) | [268] | |||||
| Medullae: phenanthrene dimers (effususins A–D); effususins A and B showed cytotoxic activity against several tumor cell lines; effususin B showed inflammatory activity (inhibition of NO production in LPS-stimulated RAW 264.7 cells) | [269] | |||||
| Phenanthrenes from medullae of Juncus effusus show cytotoxic activity against several tumor cell lines; some also show inhibition of NO production indicating anti-inflammatory potential | [270] | |||||
| The phenanthrene dehydroeffusol shows anxiolytic and sedative effects (mouse model) | [271] | |||||
| The phenanthrenes effusol and dehydroeffusol activate GABAA receptors, explaining the traditional Chinese use of the plant as a sedative and anxiolytic agent | [272] | |||||
| Juniperus virginiana L. | Cupress-aceae | Eastern red cedar | decoction of berries given for worms; infusion of some part taken for colds; ointment used on skin diseases | various | [15] | |
| Bark EO: α-pinene (77.5%) | [273] | |||||
| Leaf EO: α-pinene (2.3–6.5%), sabinene (2.8–8.7%), limonene (4.1–5.0%), safrole (18.8–22.3%), methyl eugenol (11.9–13.8%), elemol (10.6–13.6%), elemicin (6.8–7.1%) | [273] | |||||
| Berry EO: limonene (63.1%), elemol (18.4%) | [273] | |||||
| Wood EO: α-cedrene (27.2–35.0%), β-cedrene (7.7%), thujopsene (27.6–30.0%), cuparene (2.0–6.3%), cedrol (4.0–15.8%), widdrol (1.0–2.0%) | [274] | |||||
| Wood EO: α-cedrene (4.0%), β-cedrene (2.0%), thujopsene (30.1%), cedrol (38.8%), widdrol (5.6%) | [275] | |||||
| Wood EO: α-cedrene (41.4%), β-cedrene (7.5%), cis-thujopsene (20.0%), cedrol (13.4%) | dT b | |||||
| Leaves: podophyllotoxin | [276] | |||||
| Lactuca canadensis L. | Asteraceae | Canada lettuce | infusion taken for pain and calming nerves | plant | [15] | |
| Roots: sesquiterpene lactones (3-epizaluzanin C glucoside, 9-hydroxydehydroleucodin glucoside, zaluzanin C, 11β,13-dihydrozaluzanin C, 3-epizaluzanin C, 11β,13-dihydro 3-epizaluzanin C, vernoflexuoside, 11β,13-dihydro vernoflexuoside, macrocliniside A, ixerin F, picriside B, santamarin, 11β,13-dihydro santamarin, armexifolin, 1-epidehydroisoerivanin, armefolin, 1-epiisoerivanin, 3α-hydroxyreynosin and 1-epierivanin) | [277] | |||||
| Liatris spicata (L.) Willd. | Asteraceae | Blazing star | tonic, tincture used on pains | root | [15] | |
| Flavonoid glycosides: quercetin 3-glucoside, quercetin 3-rutinoside, and quercetin 3-glucoside-7-rhamnoside | [278] | |||||
| Leaf: major volatiles: α-pinene, mesityl oxide, β-pinene, myrcene, 2,4-heptadienal, β-caryophyllene, germacrene D, caryophyllene oxide | [279] | |||||
| Aerial parts: guaianolide sesquiterpenoid spicatin | [280] | |||||
| Corms (underground stems): sterols (stigmasterol and its 3-O-glucoside), triterpene (obtusifoliyl acetate), benzofurans: (euparin and 6-hydroxy-3-methoxytremetone), phenolic acids (protocatechuic, vanillic and ferulic acid) and a sesquiterpene lactone igalan. Iglan showed cytotoxic activity on Hep-G2 cells | [281] | |||||
| Lindera benzoin (L.) Blume | Lauraceae | Spicebush | infusion taken for measles, cough | bark | [15] | |
| infusion of leaves taken for coughs, colds, flu | leaves | [22] | ||||
| Leaf EO: 6-methyl-5-hepten-2-one (42.9%), β-caryophyllene (7.7%), bicyclogermacrene (5.1%), δ-cadinene (4.9%), and (E)-nerolidol (4.8%) | [282] | |||||
| Twigs EO: α-pinene (5.9%), sabinene (6.8%), α-phellandrene (4.2%), 1,8-cineole (45.4%), α-terpineol (6.8%) | [283] | |||||
| Fruit EO: myrcene (4.7%), α-phellandrene (64.6%), β-phellandrene (11.2%) | [283] | |||||
| Fruit: (6Z,9Z)-pentadecadien-2-one, (6Z,9Z,12Z)-pentadecatrien-2-one, (Z)-nerolidol, isolinderanolide, isolinderenolide, isoobtusilactone A, obtusilactone A, isoobtusilactone, obtusilactone, and linderanolide | [284] | |||||
| Liquidambar styraciflua L. | Altingiaceae | Sweet gum | inner bark for diarrhea, externally for wounds, sores, ulcers | bark | [15] | |
| Bark: shikimic acid | [285] | |||||
| Bark: pentacyclic triterpenoids (25-acetoxy-3α-hydroxyolean-12-en-28-oic acid, 3α,25-dihydroxyolean-12-en-28-oic acid, 6β-hydroxy-3-oxolup-20(29)-en-28-oic acid, and 3,11-dioxoolean-12-en-28-oic acid); 25-acetoxy-3α-hydroxyolean-12-en-28-oic acid showed broad cytotoxic activity against a panel of human tumor cell lines | [286] | |||||
| Bark: polyphenolics (shikimic acid, gallic acid, vanillic acid) | [287] | |||||
| Cones: pentacyclic triterpenoids (6β,30-dihydroxy-3-oxolup-20(29)-en-28-oic acid, 3α-hydroxy-11-oxoolean-12-en-28-oic acid, and massagenic acid G) | [288] | |||||
| Leaves: polyphenolics (gallic acid, isorugosin, casuarictin, quercetin-3-O-glucoside, myricetrin, quercetin, myricetin); extract showed hepatoprotective activity | [289] | |||||
| Aerial parts: β-sitosterol, lupeol, oleanolic acid, ursolic acid, luteolin, orientin, isoorientin, kaempferol 3-O-α-rhamnoside, and kaempferol 3-O-β-glucoside. Extract showed acetylcholinesterase inhibitory activity | [290] | |||||
| Leaf EO: α-Pinene (26.2–28.0%), β-pinene (10.1–11.3%), Limonene (20.7–22.3%) | [291] | |||||
| Stem EO: α-Pinene (11.1–16.0%), β-pinene (4.4–8.6%), Limonene (11.2–12.9%), β-caryophyllene (5.4–6.9%), germacrene D (6.7–10.9%) | [291] | |||||
| Liriodendron tulipifera L. | Magnoli-aceae | Tulip tree | bark infusion taken for pinworms, cholera, coughs, rheumatism | bark | [15] | |
| Bark: lignans (lirionol, syringic acid methyl ester, pinoresinol, syringaresinol), aporphine alkaloids (O-methyl-N-noraporphine, N-(2-hydroxy-2-phenylethyl)-benzamide) | [292] | |||||
| Bark: aporphine alkaloids (asimilobine, norushinsunine, norglacine, liriodenine, anonaine, oxoglaucine); the aporphine alkaloids showed antiplasmodial activity | [293] | |||||
| Leaves: germacranolide sesquiterpenoids (peroxyferolide, lipiferolide); showed antiplasmodial and cytotoxic activities | [293] | |||||
| Leaves: aporphine alkaloids (anonaine, norstephalagine, liridinine, nornuciferine, caaverine, lirinidine, lysicamine), a coumarin (scopoletin), a germacranolide (epitulipinolide diepoxide), polyphenolics (β-orcinol carboxylate, syringaldehyde, syringic acid, vanillic acid), sterols (β-sitosterol, stigmasterol); anonaine, liridinine, lysicamine, and epitulipinolide diepoxide significantly inhibited prolifertion of A375 melanoma cells | [294] | |||||
| Leaves: germacranolide (dihydrochrysanolide, 11,13-dehydrolanuginolide, laurenbiolide) and guaianolide (β-cyclolipiferolide) sesquiterpenoids | [295] | |||||
| Aerial parts: lignans (sesamin, syringaresinol, dihydrodehydrodiconiferyl alcohol, salvinal, guaicylglycerol-8-O-4′-dihydroconiferyl ether, guaiacylglycerol-8-O-4′-sinapyl alcohol ether, tanegool, 5,5′-dimethoxy-7-oxolariciresinol), phenolics (3-hydroxy-4-methoxyacetophenone, 4-acetoxymethylphenol), germacranolide (paramicholide), and blumenol A | [296] | |||||
| Roots: germacranolides (tulipinolide, epitulipinolide) | [297] | |||||
| Leaf EO: (Z)-β-Ocimene (6.1–59.4%), (E)-β-ocimene (4.4–24.0%), β-elemene (8.2–23.5%), germacrene D (4.8–43.5%), bicyclogermacrene (3.0–21.5%); β-ocimenes cytotoxic to MDA-MB-231 and Hs578T cells | [298] | |||||
| Bark EO: α-Pinene (6.7–11.3%), camphene (1.1–5.0%), β-pinene (6.9–19.1%), myrcene (2.4–11.7%), limonene (4.5–12.0%), β-phellandrene (up to 13.7%), (Z)-β-ocimene (30.6–53.9%), bornyl acetate (2.6–13.3%) | [299] | |||||
| Lobelia cardinalis L. | Campanu-laceae | Cardinal flower | root infusion for worms, rheumatism; leaf infusion for colds, fever; root poultice for sores | root, leaves | [15] | |
| Aerial parts: alkaloid lobinaline | [300] | |||||
| Hairy root culture: diacetylene triol lobetyol + glucosides lobetyolin and lobetyolinin | [301] | |||||
| Leaves: anthocyanin cyanidin-3-O-[6-O-(4-O-E-p-coumaroyl-O-α-rhamnopyranosyl)-β-glucopyrano]-5-O-β-glucopyranoside | [302] | |||||
| Lobelia inflata L. | Campanu-laceae | Indian tobacco | root poultice used on pains; root/leaf poultice used on ringworm, insect bites | root, leaves | [15] | |
| Hairy root culture: diacetylene triol lobetyol + glucosides lobetyolin and lobetyolinin | [303] | |||||
| Aerial parts: piperidine alkaloids (lobeline, lobelanine, norlobeline, norlobelanine, lobelanidine, norallosedamine, 8-ethyl-10-phenylnorlobelionol, 8-ethyl-10-phenyllobelionol) | [304] | |||||
| Aerial parts: piperidine alkaloids (8,10-diethyllobelidione, 8,10-diethyllobelidione, 8-ethyl-10-phenyl-norlobelionol, 8-ethyl-10-phenyl-dehydrolobelionol, 8-ethyl-10-phenyl-dehydrolobelionol, lobeline, lobelidine, lobelanine) | [305] | |||||
| Lobelia siphilitica L. | Campanu-laceae | Great blue lobelia | root infusion for worms; leaf infusion for colds, fever | root, leaves | [15] | |
| Aerial parts: piperidine alkaloids (lobeline, cis-8,10-diphenyllobelidiol, (S)-2-[(2S,6R)-1-methyl-6-(2-oxo-2-phenylethyl)piperidin-2-yl]-1-phenylethyl acetate, 6-[(E)-2-(3-methoxyphenyl)ethenyl]-2,3,4,5-tetrahydropyridine) and the diacetylene lobetyolin | [306] | |||||
| Lycopus virginicus L. | Lamiaceae | Virginia bugleweed | tea; root applied to snakebite | plant, root | [15] | |
| Aerial parts: flavone glucuronides (7-O-β-d-glucuronides of apigenin, acacetin, and luteolin as well as the methyl ester of apigenin 7-O-β-d-glucuronide) | [307] | |||||
| Magnolia acuminata (L.) | Magnoli-aceae | Cucumber magnolia | bark infusion for toothache | bark | [15] | |
| Root bark: lignans (calopiptin, galgravin, veraguensin, and acuminatin) | [308] | |||||
| Root bark: alkaloids (anolobine, N-methyllidcarpine methiodide, N,N′-dimethyl-2,11,-dihydro-1,10-dimethoxyaporphine iodide), lignans (calopiptin, galgravin, veraguensin, acuminatin), sesquiterpene lactone (costunolide), sterol (β-sitosterol) | [309] | |||||
| Leaves: alkaloids (asimilobine, liriodenine, norarmepavine, roemerine, armepavine, magnocurarine, magnoflorine) | [310] | |||||
| Menispermum canadense L. | Menisperm-aceae | Common moonseed | root used for skin diseases | root | [15] | |
| Roots: alkaloid dauricine | [311] | |||||
| Aerial parts: alkaloid acutumine | [312] | |||||
| Roots: alkaloids (acutumine, acutumidine, dauricine, daurinoline, N′-desmethyldauricine, magnoflorine, N,N-dimethyllindcarpine, dehydrocheilanthifoline) | [312] | |||||
| Monarda didyma L. | Lamiaceae | Scarlet beebalm | infusion abortifacient; poultice for colds, headache | leaves | Several essential oil chemotypes are known | [15] |
| Floral EO: sabinene (5.0%), γ-terpinene (5.3%), p-cymene (11.0%), linalool (64.5%) | [313] | |||||
| Leaf EO: linalool (74.2%), bornyl acetate (5.7%), germacrene D (5.3%) | [313] | |||||
| Commercial EO (Pam′innov, Le Chaffaut-Saint-Jurson, Provence, France): geraniol (89.5%) | [314] | |||||
| Leaf EO: δ-3-carene (4.5%), p-cymene (10.5%), γ-terpinene (9.3%), thymol (57.3%); EO showed antifungal and DPPH radical inhibitory activities | [315] | |||||
| Leaf EO: γ-terpinene (7.0%), α-terpinene (7.0%), p-cymene (20.1%), borneol (11.7%), 1-octen-3-ol (21.7%), thymol (12.3%), thymoquinone (10.1%) | [316] | |||||
| Leaf EO: γ-terpinene (6.6%), p-cymene (33.9%), thymol (38.0%), thymoquinone (12.8%) | [316] | |||||
| Leaf EO: p-cymene (17.0%), carvacrol (69.7%) | [316] | |||||
| Leaf EO: p-cymene (17.0%), linalool (29.3%), 1-octen-3-ol (9.8%), thymol (5.5%), thymoquinone (22.3%) | [316] | |||||
| Leaf EO: p-cymene (21.2%), 1-octen-3-ol (7.1%), carvacrol (46.8%), thymoquinone (21.3%) | [316] | |||||
| Aerial parts EO (M. didyma var 80-1A): p-cymene (8.2%), linalool (55.4%), geraniol (20.7%); EO inhibited mycelial growth spore germination of Botrytis cinerea | [317] | |||||
| Aerial parts EO: p-cymene (12.6%), γ-terpinene (15.9%), thymol (41.2%), carvacrol (15.2%); EO inhibited mycelial growth spore germination of Botrytis cinerea | [317] | |||||
| Aerial parts EO: δ-3-carene (4.1–4.5%), p-cymene (10.2–10.3%), γ-terpinolene (9.2%), thymol (59.4–64.3%); EO showed anticandidal and antibacterial activity. | [318] | |||||
| Aerial parts EO: p-cymene (10.3%), terpinolene (9.2%), thymol (59.3%); EO showed anti-germination activity against several ′′weed′′ seeds | [319] | |||||
| Leaves and flowers: flavonoids (rutin, hyperoside, quercitrin, luteolin, quercetin) | [320] | |||||
| Monarda fistulosa L. | Lamiaceae | Wild bergamot | fevers, colds | plant | Several subspecies are known | [15] |
| Aerial parts EO: geraniol (86.8%) | [321] | |||||
| Leaf EO: p-cymene (9.2%), thymol (72.9%), carvacrol (6.8%), thymoquinone (5.9%) | [316] | |||||
| Aerial parts EO: myrcene (8.1%), α-phellandrene (13.7%), β-phellandrene (17.0%), p-cymene (13.5%), thymol (26.5%) | [322] | |||||
| Aerial parts EO: p-cymene (35.4%), 1-octen-3-ol (10.3%), carvacrol (39.1%); the EO and carvacrol showed good mosquito (Aedes aegypti) repellent activity | [323] | |||||
| Aerial parts EO: myrcene (8.6–8.7%), α-phellandrene (13.7–14.0%), p-cymene (13.2–13.3%), thymol (28.4–33.4%); EO showed anticandidal and antibacterial activity | [318] | |||||
| Leaf EO: α-terpineol (35.9%, 99% l-enantiomer), thymol methyl ether (14.0%), linalool (5.0%, 100% l-enantiomer) | WNS c | |||||
| Oenothera biennis L. | Onagraceae | Evening primrose | eye conditions due to asthma, allergies; poultice on boils | root | [15] | |
| poultice used on hemorrhoids | leaves | [21] | ||||
| Roots: oenotheralanosterol A, oenotheralanosterol B | [324] | |||||
| Roots: oenotheralanosterol A, oenotheralanosterol B | [325] | |||||
| Roots: gallic acid (antifungal) | [326] | |||||
| Roots: 6-(13,14-ciacetyloxyprenyl)-1,3,7-trimethoxyxanthone, eicos-9-enoyl-α-d-glucopyranosyl-(6→1′′)-α-d-glucopyranoside | [327] | |||||
| Roots: oleanolic acid, maslinic acid, β-sitolsterol, gallic acid, 2,7,8-trimethylellagic acid, tetramethylellagic acid, 2-methyl-7-oxotritetracont-1,5,dien-21ol, 18-hydroxypentacos-21-enoic acid, 5-methyl-27-oxotriacont-4-en-24-ol, and 3,5-dihydroxy-4-pent-4′-enoyl-1′-oxymethylbenzoic acid | [328] | |||||
| Seed oil: linoleic acid, sterols (campesterol, β-sitosterol, Δ5-avenasterol) | [329] | |||||
| Seeds: catechin, epicatechin, gallic acid | [330] | |||||
| Seeds: protocatechuic acid | [331] | |||||
| Aerial parts: phenolics (galloylglucose, gallic acid, oenothein B, quercetin 3-O-glucuronide, kaempferol 3-O-glucuronide) | [332] | |||||
| Panax quinquefolius L. | Araliaceae | American ginseng | root used as tonic | root | [15] | |
| Root (wild): ginsenosides [Rb1 (2.81%), Rb2 (0.09%), Rc (0.42%), Rd (0.29%), Re (1.42%), and Rg1 (0.94%)] | [333] | |||||
| Root: ginsenosides (Rb1, Rb2, Rc, Rd, Re, Rf and Rg1) | [334] | |||||
| Root (cultivated): ginsenosides [Rb1 (3.70%), Rb2 (0.05%), Rc (0.41%), Rd (0.42%), Re (0.50%), and Rg1 (0.13%)] | [335] | |||||
| Root (cultivated): ginsenosides [Rb1 (1.85%), Rb2 (0.04%), Rb3 (0.04%), Rc (0.29%), Rd (0.29%), Re (2.05%), Rg1 (0.25%), and F11 (0.20%)] | [336] | |||||
| Root (cultivated): polyacetylenes (falcarinol, panaxydol) | [337] | |||||
| Root (cultivated): ginsenosides [Rb1 (4.94%), Rb2 (0.04%), Rc (0.39%), Rd (0.60%), Re (1.75%), and Rg1 (0.13%)] | [338] | |||||
| Leaves (wild): ginsenosides [Rb1 (0.17%), Rb2 (1.04%), Rc (0.18%), Rd (1.08%), Re (0.93%), and Rg1 (0.14%)] | [333] | |||||
| Leaves (cultivated): ginsenosides [Rb1 (0.28%), Rb2 (1.82%), Rb3 (4.64%), Rc (0.56%), Rd (2.82%), Re (3.42%), Rg1 (0.96%), and F11 (1.94%)] | [336] | |||||
| Review of chemical analysis of P. quinquefolius | [339] | |||||
| Review of pharmacology and toxicology of P. quinquefolius | [340] | |||||
| Review of ginsenosides in P. quinquefolius | [341] | |||||
| Review of pharmacology of P. quinquefolius | [342] | |||||
| Panax trifolius L. | Araliaceae | Dwarf ginseng | root used as tonic | root | [22] | |
| Leaves: flavonoids (kaempferol-3,7-dirhamnoside and kaempferol-3-gluco-7-rhamnoside), ginsenosides (ginsenoside-Rd, -Rc, -Rb3 and notoginsenoside-Fe) | [343] | |||||
| Leaves: ginsenosides (Ro, Rb1, Rb2, Rc) | [344] | |||||
| Parthenocissus quinquefolia (L.) Planch. | Vitaceae | Virginia creeper | infusion taken for jaundice | [15] | ||
| Stem: resveratrol oligomers, parthenocissins A and B, were isolated in addition to three known stilbenes (resveratrol, piceatannol, resveratrol 3-glucoside) | [345] | |||||
| Stem: oligostilbenes, parthenocissins M and N, together with two known compounds, miyabenol C and ϵ-viniferin | [346] | |||||
| Leaves: β-amyryl palmitate; shows thrombin inhibitory activity | [347] | |||||
| Passiflora incarnata L. | Passiflor- aceae | Passion flower | root infusion used for boils, earache, to wean babies; poultice for wounds | root | [15] | |
| Plant: C-Glycosidic flavonoids (schaftoside, isoschaftoside, isovetexin-2″-O-glucopyranoside and isoorientin-2″-O-glucopyranoside) | [348] | |||||
| Plant: flavonoid glycosides (vicenin-2. schaftoside, isoschaftoside isoorientin-2′′-O-glucoside, isoorientin, isovitexin-2′′-O-glucoside, swertisin, orientin isovitexin, vitexin | [349] | |||||
| Plant: flavonoid glycoside (isoscoparin-2′′-O-glucoside) | [350] | |||||
| Plant: C-glycosidic flavonoid (6-β-D-glucopyranosyl-8-β-d-ribopyranosyl apigenin) | [351] | |||||
| The phytochemistry of P. incarnata has been reviewed | [352] | |||||
| Phytolacca americana L. | Phytolac-caceae | Pokeweed | poultice used for ulcers; root infusion used for eczema | root | [15] | |
| Roots: triterpenoid saponins (phytolaccosides A, D, E) | [353] | |||||
| Roots: triterpenoid saponin (phytolaccoside B) | [354] | |||||
| Roots: triterpenoid saponins (phytolaccasaponins B, E, G) | [355] | |||||
| Roots: triterpenoid saponins (phytolaccasaponins N1–N5; esculentoside H, esculentoside A = phytolaccoside E, esculentoside M, esculentoside B = phytolaccoside B, esculentoside S, esculentoside R-28-O-glucoside, esculentoside L) | [356] | |||||
| Roots: phytosterol α-spinasterol | [357] | |||||
| Pinus virginiana Mill. | Pinaceae | Pine | wash for skin ulcers/sores; sap used on stubborn sores; syrup from inner bark for coughs/congestion; inner bark used for intestinal worms and parasites. | bark | [18] | |
| Bark EO: α-pinene (43.1%), β-pinene (24.8%), β-phellandrene (13.9%) | [273] | |||||
| Leaf EO: α-pinene (22.8%), β-pinene (25.1%), β-phellandrene (14.3%), α-terpineol (8.7%) | [273] | |||||
| Plantago lanceolata L. a | Plantagin-aceae | Narrowleaf plantain | infusion or poultice used for bites and stings | plant | [15] | |
| Herb: purpureaside A, lavandulifolioside B, acteoside, luteolin-3′,7-diglucuronide, isoacteoside, luteolin-7-glucuronide, and luteolin | [358] | |||||
| Herb: phenolic acids: p-hydroxybenzoic acid, vanillic acid, gallic acid, cinnamic acid, chlorogenic acid (major); flavonoids: apigenin, luteolin, luteolin-7-O-glucoside. Extract shows antioxidant, COX-1-inhibitory, 12-LOX-inhibitory, and weak cytotoxic activity | [359] | |||||
| Herb: iridoid glycosides: aucubin and catapol | [360] | |||||
| Herb: iridoid glycosides: aucubin and catapol | [361] | |||||
| Herb: acteoside, aucubin, catalpol | [362] | |||||
| Herb: acteoside, aucubin, catalpol | [363] | |||||
| Plantago major L. a | Plantagin-aceae | Common plantain | infusion or poultice used for bites and stings | plant | [15] | |
| Review, Herb: aucubin, melittoside, asperuloside, melampyroside, plantarenaloside, ixoroside, majoroside, 10-hydroxymajoroside, 10-acetoxymajoroside, acteoside, plantamajoside | [364] | |||||
| Review, Herb: caffeic acid derivatives (caffeic acid, chlorogenic acid, plantamajoside, acteoside), flavonoids (apigenin 7-glucoside, baicalein, hispidulin, hispidulin 7-glucuronide, homoplantaginin, luteolin 7-glucoside, luteolin 7-diglucoside, luteolin 6-hydroxy-4′-methoxy-7-galactoside, nepetin 7-glucoside, plantaginin, scutellarein), iridoid glycosides (asperuloside, aucubin, catapol, gardoside, geniposidic acid, majoroside, 10-acetoxymajoroside, 10-hydroxymajoroside, melittoside), triterpenoids (oleanolic acid, ursolic acid, 18β-glycyrrhetinic acid). Bioactivities of extracts includes wound healing activity, anti-inflammatory, analgesic, antioxidant, weak antibiotic, immuno modulating and antiulcerogenic activity | [365] | |||||
| P. major compounds showed antiviral activity: caffeic acid on herpesvirus (HSV-1) and adenovirus (ADV-3); chlorogenic acid on ADV-11 | [366] | |||||
| Herb: ursolic acid, oleanolic acid | [367] | |||||
| Herb: ursolic acid, oleanolic acid | [368] | |||||
| Herb: isomarynoside, 10-hydroxymajoroside, β-sitosterol, ursolic acid | [369] | |||||
| Herb: ursolic acid, oleanolic acid | [370] | |||||
| Herb: α-linolenic acid, ursolic acid, oleanolic acid; SFE extract showed COX-2 inhibitory activity | [371] | |||||
| Platanus occidentalis L. | Platanaceae | American sycamore | infusion of inner bark for cough, measles, urinary infection | bark | [15] | |
| Bark: anti-MRSA flavonoids (kaempferol 3-O-α-l-(2′′,3′′-di-E-p-coumaroyl)rhamnoside, kaempferol 3-O-α-l-(2′′-E-p-coumaroyl-3′′-Z-p-coumaroyl)rhamnoside, kaempferol 3-O-α-l-(2′′-Z-p-coumaroyl-3′′-E-p-coumaroyl)rhamnoside, and kaempferol 3-O-α-l-(2′′,3′′-di-Z-p-coumaroyl)rhamnoside) | [372] | |||||
| Podophyllum peltatum L. | Berberi-daceae | Mayapple | anthelmintic, sores | root | [15] | |
| warts | resin | [15] | ||||
| Roots: aryltetralin lignans (podophyllotoxin, picropodophyllotoxin, α-peltatin, β-peltatin, desoxypodophyllotoxin) | [373] | |||||
| Roots: aryltetralin lignans (podophyllotoxin, 4′-demethylpodophyllotoxin, α-peltatin, β-peltatin, desoxypodophyllotoxin, podophyllotoxone, isopicropodophyllone, 4′-demethyldesoxypodophyllotoxin, 4′-demethylpodophyllotoxone and 4′-demethylisopicropodophyllone | [374] | |||||
| Plants: aryltetralin lignans (podophyllotoxin 4-O-β-d-glucopyranoside, epipodophyllotoxin 4-O-β-d-glucopyranoside, 4¢-demethylpodophyllotoxin, α-peltatin, epipodophyllotoxin, podophyllotoxin, β-peltatin, 1,2,3,4-dehydrodesoxypodophyllotoxin) | [375] | |||||
| Polygala senega L. | Polygalaceae | Seneca snakeroot | snakebite | root | [15] | |
| Root: triterpenoid saponin senegin-II | [376] | |||||
| Root: triterpenoid saponins (senegin III, senegin IV) | [377] | |||||
| Root: oligosaccharide esters (senegose A, senegose B, senegose C, senegose D, senegose E) | [378] | |||||
| Root: oligosaccharide esters (senegose F, senegose G, senegose H, senegose I) | [379] | |||||
| Root: oligosaccharide esters (senegose J, senegose K, senegose L, senegoseM, senegose N, senegose O) | [380] | |||||
| Root: triterpenoid saponins (senegin II, senegin III, E-senegasaponin A, E-senegasaponin B, Z-senegasaponin A, Z-senegasaponin B, Z-senegin II, Z-senegen III) | [381] | |||||
| Root: essential oil [hexanoic acid (33.6%), methyl salicylate (26.5%), n-hexanal (5.3%) and o-cresol (3.5%)] | [382] | |||||
| Root: triterpenoid saponins (senegin II, senegin III, senegin IV, senegasaponin A, senegasaponin B) | [383] | |||||
| Polygonum aviculare L. | Polygon-aceae | Prostrate knotweed | fish poison | plant | [15] | |
| Plant: lignan aviculin; flavonoids (juglanin, avicularin, astragalin, and betmidin) | [384] | |||||
| Plant: naphthoquinone 6-methoxyplumbagin, also β-sitosterol, oleanolic acid, and 5,6,7,4′-tetramethoxyflavanone | [385] | |||||
| Aerial parts: flavonoids (avicularin, liquiritin, cinaroside) | [386] | |||||
| Plant: flavonol glucuronides [myricetin 3-O-β-d-glucuronide, mearsetin 3-O-β-d-glucuronide, quercetin 3-O-β-d-glucuronide, isorhamnetin 3-O-β-d-glucuronide, kaempferide 3-O-β-d-glucuronide, kaempferol 3-O-β-d-glucuronide, kaempferol 3-O-β-(2″-O-acetyl-β-d-glucuronide), isorhamnetin 3-O-β-(2″-O-acetyl-β-d-glucuronide), quercetin 3-O-β-(2″-O-acetyl-β-d-glucuronide), quercetin 3-O-β-(3″-O-acetyl-β-d-glucuronide), and kaempferol 3-O-β-(3″-O-acetyl-β-d-glucuronide)] | [387] | |||||
| Leaves: flavonoids (myricetin, quercetin, kaempferol, myricitrin, desmanthin-1, isoquercitrin, quercitrin, avicularin, juglanin) and gallic acid | [388] | |||||
| Aerial parts: flavonoids (avicularin, juglanin, myricitrin, isoastragalin, isoquercitrin, kaempferol-5,7-di-O-β-d-glucopyranoside, and kaempferol 5-O-α-l-rhamnopyranoside 5-O-β-d-glucopyranoside), lignan aviculin, and loliolide and 1,6-digalloylglucose | [389] | |||||
| Polygonum hydropiper L. | Polygon-aceae | Marshpepper knotweed | fish poison | plant | [15] | |
| Plant: polygodial | [390] | |||||
| Plant: drimane sesquiterpenoids (warburanal, polygodial, isopolygodial, polygonal, isodrimeninol, drimenol, confertifolin) | [391] | |||||
| Plant: flavonoids [rutin (0.58–0.93%), hyperin (0.37–0.63%), isoquercitrin (0.08–0.38%), quercitrin (0.55–0.95%), catechin (0.06–0.09%), epicatechin (0.05–0.08%), quercetin (0.28–0.65%), kaempferol (0.28–0.53%), isorhamnetin (0.03–0.04%)] | [392] | |||||
| Leaves: drimane sesquiterpenoids (polygonic acid, 11-ethoxycinnamolide, polygodial acetal, valdiviolide, and fuegin), drimane norsesquiterpenoids (isopolygonal and polygonone) | [393] | |||||
| Leaves: flavonoids (7,4′-dimethylquercetin, 3′-methylquercetin, quercetin, isoquercitrin) | [394] | |||||
| Leaves: flavonoid sulfates (quercetin 3-sulfate, isorhamnetin 3,7-disulfate, and tamarixetin 3-glucoside-7-sulfate) | [395] | |||||
| Leaves: flavonoids [3-O-α-l-rhamnopyranosyloxy-3′,4′,5,7-tetrahydroxyflavone; 3-O-β-d-glucopyranosyloxy-4′,5,7-trihydroxyflavone; 6-hydroxyapigenin; 6″-O-(3,4,5-trihydroxybenzoyl) 3-O-β-d-glucopyranosyloxy-3′,4′,5,7-tetrahydroxyflavone; scutillarein; 6-hydroxyluteolin;3′,4′,5,6,7-pentahydroxyflavone; 6-hydroxyluteolin-7-O-β-d-glucopyranoside; quercetin 3-O-β-d-glucuronide; 2″-O-(3,4,5-trihydroxybenzoyl)quercitrin; quercetin) | [396] | |||||
| Sprout: drimane sesquiterpenoids (polygodial, warburganal) | [397] | |||||
| Sprout: flavonoid (2R,3R)-(+)-taxifolin (showed tyrosinase inhibition) | [398] | |||||
| Aerial parts: sucrose cinnamyl esters (hydropiperoside A, hydropiperoside B, vanicoside A, vanicoside B, vanicoside E) | [399] | |||||
| Sprout: essential oil [β-caryophyllene (9.3%), α-humulene (6.0%), (E)-β-farnesene (44.1%), (E)-nerolidol (6.9%), phytol (10.8%)] | [400] | |||||
| Leaves: essential oil (confertifolin, 22.9%) | [401] | |||||
| Polymnia canadensis L. | Asteraceae | Whiteflower leafcup | Houma Native American use (not Cherokee) applied a leaf poultice to swellings | leaves | [15] | |
| Leaf EO: germacrene D (44.5–63.7%), β-caryophyllene (14.8–15.9%), α-humulene (3.9–5.1%) | WNSc | |||||
| Polymnia uvedalia (L.) (syn. Smallanthus uvedalia (L.) Mack.) | Asteraceae | Leafcup, Bear′s foot | bruised root used on cuts, burns | root | [15] | |
| Germacranolide sesquiterpenoids (uvedalin, isouvedalin, 2′,3′-dehydromelnerin A, 9-hydroxy-2′,3′-dehydromelnerin A), ent-kaurane diterpenoids (ent-12-hydroxy-16-kauren-19-oic acid, ent-18-hydroxy-16-kauren-19-oic acid derivatives, ent-16-kauren-3,19-diol derivatives, ent-12,18-dihydroxy-16-kauren-19-oic acid derivatives | [247] | |||||
| Leaf EO: caryophyllane sesquiterpenoids: β-caryophyllene (16.5–24.5%), caryophyllene oxide (14.2–19.8%), caryophylla-4(12), 8(13)-dien-5β-ol (2.3–5.5%), 14-hydroxy-9-epi-(Z)-caryophyllene (4.3–8.2%), 14-hydroxy-9-epi-(E)-caryophyllene (6.2–8.9%) | WNSc | |||||
| Prunella vulgaris L. | Lamiaceae | Heal-all | sore throat, cuts, burns | plant | [15] | |
| Leaf EO: selin-1 1-en-4α-ol (14.9%), cis-eudesma-6,11-diene (9.4%), 1,10-di-epi-cubenol (8.0%), spathulenol (5.8%) and germacrene D (5.1%) | [402] | |||||
| Leaf EO: aromadendrene (55.4%), cucumber alcohol (8.5%) and phytol (5.1%) | [403] | |||||
| Aerial parts: rosmarinic acid, ursolic acid, oleanolic acid | [404] | |||||
| Aerial parts: rosmarinic acid, ursolic acid, oleanolic acid | [405] | |||||
| Aerial parts: four triterpenes, i.e., betulinic acid, ursolic acid, 2α,3α-dihydroxyurs-12-en-28-oic acid, and 2α-hydroxyursolic acid | [406] | |||||
| Aerial parts: polyacetylenic acids (octadeca-9,11,13-triynoic acid and trans-octadec-13-ene-9,11-diynoic acid | [407] | |||||
| oleanane-skeleton triterpenoid saponins, 3β,4β,16α-17-carboxy-16,24-dihydroxy-28-norolean-12-en-3-yl 4-O-β-d-xylopyranosyl-β-d-glucopyranosiduronic acid, (3β,4β,16α)-17-carboxy-16,24-dihydroxy-28-norolean-12-en-3-yl β-d-glucopyranosiduronic acid methyl ester, and (3β,4β)-24-hydroxy-16-oxo-28-norolean-12-en-3-yl 4-O-β-d-xylopyranosyl-β-d-glucopyranosiduronic acid | [408] | |||||
| Aerial parts: 15 triterpene acids (oleanic acid, ursolic acid, 2α,3α,19α-trihydroxyurs-12-en-28-oic acid, 2α,3α-dihydroxyurs-12-en-28-oic acid, maslinic acid, 2α,3α,19α,23-tetrahydroxyurs-12-en-28-oic acid, 2α,3α,23-trihydroxyurs-12-en-28-oic acid, 2α,3β-dihydroxyurs-12-en-28-oic acid, 2α,3β,24-trihydroxyolea-12-en-28-oic acid, (12R,13S)-2α,3α,24,trihydroxy-12,13-cyclotaraxer-14-en-28-oic acid, 2α,3α,24-trihydroxyurs-12,20(30)-dien-28-oic acid, 2α,3α,24-trihydroxyolea-12-en-28-oic acid, 2α,3β,19α,24-tetrahydroxyurs-12-en-28-oic acid 28-O-d-glucopyranoside, 2α,3α,19α,24-tetrahydroxyurs-12-en-28-oic acid 28-O-d-glucopyranoside, prunvuloside A); four flavonoids (quercertin 3-O-β-d-glucopyranoside, kaempferol 3-O-α-l-rhamnopyranosyl(1→6)-β-d-glucopranoside, kaempferol 3-O-β-d-glucopyranoside, quercertin 3-O-α-l-rhamnopyranosyl(1→6)-β-d-glucopyranoside); four phenolics (caffeic acid, p-hydroxycinnamic acid, rosmarinic acid, and 2-hydroxy-3-(3′,4′-dihydroxyphenly)propanoic acid); and a diterpene (trans-phytol) | [409] | |||||
| Aerial parts: polyphenolics (butyl rosmarinate, ethyl rosmarinate, methyl rosmarinate, rosmarinic acid, 3,4,α-trihydroxy-methyl phenylpropionate, and p-coumaric acid) | [410] | |||||
| Aerial parts: phenolics (quercetin, rutin, rosmarinic acid, caffeic acid, chlorogenic acid ferulic acid, protocatechuic acid) | [411] | |||||
| Aerial parts: polygalacerebroside, ursolic acid, β-amyrin, quercetin, quercetin-3-O-β-d-galactoside, α-spinasterol, stigmasterol, β-sitosterol, daucosterol | [412] | |||||
| Prunus serotina Ehrh. | Prunaceae | Black cherry | bark infusion for colds | bark | [15] | |
| Leaves: flavonoids (avicularin, noutrin, hyperoside, narcissin, rutin, quercetin 3-O-neohesperidoside, 3-O-(2″-O-α-l-rhamnopyranosyl)-β-d-galactopyranoside) | [413] | |||||
| Leaves: chlorogenic acid (1.08–2.30%), rutin (0.10–0.35%), hyperoside (1.20–2.23%), reynoutrin (0.26–0.44%), guajiverin (0.07–0.22%), avicularin (0.98–1.82%), juglanin (0.04–0.20%) | [414] | |||||
| Leaves: triterpenoids [corosolic acid (0.137%), olanolic acid (0.129%), ursolic acid (0.884%)] | [415] | |||||
| Leaves: hyperoside, prunin, ursolic acid | [416] | |||||
| Leaves: chlorogenic acid, hyperoside, benzaldehyde | [417] | |||||
| Leaf EO: benzyl alcohol (20.3%), benzaldehyde (12.1%), cinnamyl alcohol (4.7%), cinnamaldehyde (1.1%) | [416] | |||||
| Flowers: chlorogenic acid (0.63–1.90%), rutin (0.17–0.31%), hyperoside (0.80–1.59%), reynoutrin (0.08–0.21%), guajiverin (0.10–0.28%), avicularin (0.20–0.95%), juglanin (0.08–0.16%) | [414] | |||||
| Bark: triterpenoids (ursolic acid, ursolic aldehyde, 2α,3α-dihydroxyurs-12-en-28-oic acid) | [418] | |||||
| Bark: flavonoids (4′-methoxynaringenin, naringenin, dihydrokaempferol, eriodictyol) | [419] | |||||
| Pseudognaphalium obtusifolium (L.) Hilliard and B.L. Burtt (syn. Gnaphalium obtusifolium L.) | Asteraceae | Rabbit tobacco | infusion of herb for coughs, colds, flu | herb | [22] | |
| Plant: flavonoid obtusifolin | [420] | |||||
| Plant: flavonoids (gnaphaliin A, methylgnaphaliin) | [421] | |||||
| Plant: flavonoid 3,5,7-trihydroxy-6,8-dimethoxyflavone | [422] | |||||
| Pycnanthemum flexuosum (Walter) Britton, Sterns and Poggenb. | Lamiaceae | Mountain mint | leaf infusion for headache, colds, fevers | leaves | [15] | |
| Whole plant: vanillic acid 1-O-[(5-O-syringoyl)-β-Dapiofuranosyl]-(1→2)-β-d-glucopyranoside, (4S,5R)-4-hydroxy-5-phenyl-tetrahydrofuran-2-one, luteoline 7-O-[(6-O-acetyl)-β-d-allopyranosyl-(1→2)-β-d-glucopyranoside], 4′-O-methylhypolaetin 7-O-[6-O-acetyl-β-d-allopyranosyl-(1→2)-β-d-glucopyranoside], apigenin 7-O-[6-O-acetyl-β-d-allopyranosyl-(1→2)-β-d-glucopyranoside], isoscutellarein 4-O-methylether 7-O-[(6-O-acetyl)-β-d-allopyranosyl-(1→2)-β-d-glucopyranoside], apigenin 7-O-[6-O-(p-E-coumaroyl)-β-d-glucopyranoside], 3′-hydroxy-4-O-methylisoscutellarein 7-O-[(6-O-acetyl)-β-d-allopyranosyl-(1→2)-(6-O-acetyl)-β-d-glucopyranoside], acteoside, leucosceptoside A, martynoside, artselaeroside A, stachysoside B, and chlorogenic acid | [423] | |||||
| Quercus alba L. | Fagaceae | White oak | bark infusion for dysentery, antiseptic, fever | bark | [15] | |
| Bark: tannins | [424] | |||||
| Ranunculus acris L. a | Ranuncu- laceae | Tall buttercup | leaf poultice for abcesses; leaf infusion for sore throat | leaves | [15] | |
| Aerial parts: ranunculin | [425] | |||||
| Rhamnus caroliniana Walter | Rhamnaceae | Buckthorn | itching skin, sores | berries, bark | ||
| Bark: chrysophanol, physcion, ararobinol, orachrysone, 1-docosanol | [426] | |||||
| Bark EO: chrysarobin (24.2%), piperine (15.4%), and pacharin (7.5%) | [426] | |||||
| Rhus glabra L. | Anacardi-aceae | Smooth sumac | bark decoction to wash blisters | bark | [15] | |
| Branches: methyl gallate, 3,5-dihydroxy-4-methoxybenzoic acid, gallic acid; methyl gallate and 3,5-dihydroxy-4-methoxybenzoic acid showed antibacterial activity | [427] | |||||
| Leaves: myo-inositol, 1-docosanol, β-sitosterol, β-sitosterol glucoside, mixture of homologous alkanes (C14–C33, major heptacosane) | [428] | |||||
| Rhus hirta Harv. ex Engl. | Anacardi-aceae | Staghorn sumac | bark decoction to wash blisters | bark | [15] | |
| Fruits: major components: sumadin B-3-O-(2″-galloyl)-galactoside-3′′′-O-glucoside, 7-O-methyl-cyanidin-3-O-(2″-galloyl)-galactoside; shows anti-oxidant activity | [429] | |||||
| Fruits: major components: sumadin B-3-O-(2″-galloyl)-galactoside-3′′′-O-glucoside, 7-O-methyl-cyanidin-3-O-(2″-galloyl)-galactoside; shows anti-inflammatory activity | [430] | |||||
| Rhus spp. (as above) | Anacardi-aceae | infusion of berries for urinary tract infections, thrush | berries | [22] | ||
| Robinia pseudoacacia L. | Fabaceae | Black locust | bark chewed as emetic | bark | [15] | |
| Bark: lectins (RPbAI and RPbAII) | [431] | |||||
| Bark: lectin RPbAI (xtal structure) | [432] | |||||
| Saplings: flavonoids (acacetin, secundiflorol I, mucronulatol, isomucronulatol, isovestitol) | [433] | |||||
| Leaves: flavonoid glycosides (7-O-β-d-glucuronopyranosyl-(1→2)[α-l-rhamnopyranosyl-(1→6)]-β-d-glucopyranosides of acacetin, apigenin, diosmetin, and luteolin) | [434] | |||||
| Roots: lectins (RPrAI and RPrAII) | [435] | |||||
| Rubus allegheniensis Porter | Rosaceae | Allegheny blackberry | leaf infusion for diarrhea | leaves | [15] | |
| Leaf extract: triterpenoids (tormentic acid, euscaphic acid, myrianthic acid, ziyu glycoside II, sericic acid, and 19-hydroxy-2,3-secours-12-ene-2,3,28-trioic acid 3-methyl ester) | [436] | |||||
| Rubus idaeus L. a | Rosaceae | Red raspberry | leaf infusion for pain; root infusion cathartic | roots, leaves | [15] | |
| Leaf extract: quercetin glucuronide, quercetin-3-glucoside and quercetin glucosylrhamnoside (rutin) | [437] | |||||
| Leaf extract: triterpenoid glycosides (3β-(O-β-d-glucopyranosyl)-olean-12-ene-1α,2α,3β-triol, 28-(O-β-d-glucopyranosyl)-urs-12-ene-2α,3β,19α-trihydroxy-28-oic acid, and 3β-(O-β-d-glucopyranosyl)-olean-12-ene-1α,2α,3β-trihydroxy-28-oic acid) | [438] | |||||
| Leaf extracts: tannins (ellagic acids, ellagitannins, sanguiin H-6 and H-10, and the trimers lambertianin D and lambertianin C, as well as methyl gallate), phenolic acids (chlorogenic acid, p-coumaric, ferulic, protocatechuic, gentisic, caffeoyltartaric, feruloyltartaric, and p-coumaroyl-glucoside acids, as well as p-hydroxybenzoic and vanillic acids), terpenoids (terpinolene, 3-oxo-α-ionol, α- and β-amyrin, squalene and cycloartenol) | [439] | |||||
| Rudbeckia fulgida Aiton | Asteraceae | Orange coneflower | root used for ear medicine | root | [15] | |
| Leaf EO: β-caryophyllene (10.0%), γ-muurolene (8.9%), germacrene D (30.1%), δ-cadinene (17.8%) | [440] | |||||
| Rudbeckia hirta L. | Asteraceae | Black-eyed Susan | root infusion taked for sexually transmitted diseases (STDs) | root | [15] | |
| Leaf EO: (2E)-hexenal (20.2%), (E)-β-ocimene (15.2%), γ-muurolene (8.1%), germacrene D (23.6%), δ-cadinene (16.2%) | [440] | |||||
| Rudbeckia laciniata L. | Asteraceae | Souchan, Green-headed coneflower | tonic, skin wash | leaves | [15] | |
| Aerial parts: lignans ((+)-4,4′-O-diangeloylpinoresinol, (+)-4,4′-O-diangeloylmedioresinol, (+)-4,4′-O-diangeloylsyringaresinol, and (+)-syringaresinol) | [441] | |||||
| Aerial parts: flavonoid glycosides (quercetin 3-O-α-l-arabinofuranosyl-(1″→6″)-β-d-galactopyranoside, quercetin 3-O-α-l-arabinopyranosyl-(1″→6″)-β-d-galactopyranoside, quercetin-3-O-β-d-xylopyranosyl-(1″→2″)-β-d-glucopyranoside, and quercetin 3-O-β-d-glucopyranoside, isorhamnetin 3-O-β-d-glucopyranoside), quinic acid derivatives (3,5-O-trans-dicaffeoylquinic acid methyl ester, 3,5-O-trans-dicaffeoylquinic acid, 4,5-O-trans-dicaffeoylquinic acid methyl ester, 3,4-O-trans-caffeoylquinic acid methyl ester, 3,4-O-trans-caffeoylquinic acid, 5-O-trans-caffeoylquinic acid methyl ester, 3-O-trans-caffeoylquinic acid, and 3,5-O-trans-dicaffeoylepiquinic acid) | [442] | |||||
| Roots: sesquiterpene rudbeckianone | [443] | |||||
| Roots: sesquiterpene lactone rudbeckiolide | [444] | |||||
| Root extract: sesquiterpenoids (sesquithuriferol, igalan, lacinan-8-ol) | [445] | |||||
| Sambucus canadensis L. | Adoxaceae | American elder | berry infusion for rheumatism; infusion of flowers taken for fever; leaves used to wash sores | plant | [15] | |
| Flowers: rutin | [446] | |||||
| Fruits: anthocyanins (cyanidin 3-sambubioside-5-glucoside, cyanidin 3,5-diglucoside, cyanidin 3-sambubioside, cyanidin 3-glucoside, cyanidin 3-O-(6-O-Z-p-coumaroyl-2-O-β-d-xylopyranosyl)-β-d-glucopyranoside-5-O-β-d-glucopyranoside, cyanidin 3-O-(6-O-E-p-coumaroyl-2-O-β-d-xylopyranosyl)-β-d-glucopyranoside-5-O-β-d-glucopyranoside (major), cyanidin 3-O-(6-O-E-p-coumaroyl-2-O-β-d-xylopyranosyl)-β-d-glucopyranoside) | [447] | |||||
| Fruits: anthocyanins [cyanidin 3-sambubioside-5-glucoside (0.0.11–0.19%), cyanidin 3,5-diglucoside (0.03–0.06%), cyanidin 3-sambubioside (0.03–0.04%), cyanidin 3-glucoside (0.04–0.06%), cyanidin 3-(E)-p-coumaroyl-sambubioside-5-glucoside (0.32–0.59%), cyanidin 3-p-coumaroyl-sambubioside (0.01–0.02%)] | [448] | |||||
| Fruits: anthocyanins (cyanidin 3-O-(6-O-Z-p-coumaroyl-2-O-β-d-xylopyranosyl)-β-d-glucopyranoside-5-O-β-d-glucopyranoside and cyanidin 3-O-(6-O-E-p-coumaroyl-2-O-β-d-xylopyranosyl)-β-d-glucopyranoside-5-O-β-d-glucopyranoside) | [449] | |||||
| Sanguinaria canadensis L. | Papaver-aceae | Bloodroot | root decoction for cough | root | [15] | |
| Rhizome: alkaloids (sanguinarine, chelerythrine, protopine) | [450] | |||||
| Rhizome: alkaloids [protopine (0.32–0.74%), allocryptopine (0.34–0.77%), sanguinarine (1.38–4.45%), chelerythrine (0.99–2.57%), chelirubine (0.37–0.87%), chelilutine (0.78–1.83%), sanguilutine (0.49–1.03%)] | [451] | |||||
| Rhizome: alkaloids (sanguinarine and chelerythrine-antimycobacterial) | [452] | |||||
| Rhizome: alkaloids (sanguinarine, chelerythrine, protopine - anti-Helicobacter pylori) | [453] | |||||
| Rhizome: alkaloids [sanguinarine (2.81–3.96%), chelerythrine (1.38–2.08%)] | [454] | |||||
| Rhizome: alkaloids (sanguinarine, chelerythrine, sanguilutine, chelilutine, sanguirubine, chelirubine, protopine, and allocryptopine) | [455] | |||||
| Sassafras albidum (Nutt.) Nees | Lauraceae | Sassafras | bark decoction for skin diseases, sexually-transmitted diseases; poultice for wounds and sores | bark | [17] | |
| Leaf EO: (3Z)-hexenol (2.5–9.9%), α-pinene (3.2–12.2%), camphene (0.3–5.4%), limonene (5.7–16.4%), linalool (3.5–6.7%), neral (9.9–18.1%), geranial (10.7–26.5%), β-caryophyllene (5.1–12.5%), caryophyllene oxide (0.4–19.0%) | [456] | |||||
| Root EO: safrole (85%), camphor (3.25%), and methyleugenol (1.10%) | [457] | |||||
| Bark EO: α-pinene (37.9–61.5%), camphene (2.9–5.1%), β-pinene (10.0–13.0%), 1,8-cineole (7.3–10.0%), camphor (1.7–4.6%), and α-terpineol (4.2–11.6%) | [458] | |||||
| Bark: sesamin, spinescin, β-sitosterol, hexatriacontanal, and 1-triacontanol; sesamin and spinescin showed antileishmanial activity | [459] | |||||
| Saururus cernuus L. | Saururaceae | Lizard′s tail | mashed roots poultice for wounds | root | [15] | |
| Aerial parts: lignans (austrobailignan-5, veraguensin, guaiacin, saucernetin) | [460] | |||||
| Plant: lignans (manassantin A, manassantin B, saucerneol) | [461] | |||||
| Aerial parts: indole alkaloids (sauristolactam, cepharanone B) | [462] | |||||
| Aerial parts: lignans (saururin, saururenin, saururinone, austrobailignan 6, calopiptin, galbacin, zuonin A) | [463] | |||||
| Aerial parts: lignans (sauriol A, sauriol B) | [464] | |||||
| Aerial parts: lignans (licarin A, saucernetin, dihydroguaiaretic acid, sauriol A, sauriol B, saucerneol, and saucerneol methyl ether) | [465] | |||||
| Aerial parts: diterpenoid 12,13-dehydrogeranylgeraniol | [466] | |||||
| Aerial parts: lignans (manassantin B, 4-O-demethylmanassantin B) | [467] | |||||
| Stems and leaves: lignans (manassantin A, manassantin B, manassantin B1, 4-O-methylsaucerneol, verrucosin, austrobailignan-5) | [468] | |||||
| Scutellaria lateriflora L. | Lamiaceae | Blue skullcap | root infusion for monthly period, diarrhea; root decoction to expel afterbirth; for breast pains, and for nerves | root | [15] | |
| Review | [469] | |||||
| Aerial parts EO: δ-cadinene (27%), calamenene (15.2%), β-elemene (9.2%), α-cubenene (4.2%), α-humulene (4.2%), and α-bergamotene (2.8%) | [470] | |||||
| Aerial parts: neo-clerodane diterpenoids (scutelaterin A, scutelaterin B, scutelaterin C, ajugapitin, and scutecyprol A) | [471] | |||||
| Herb: flavonoids baicalin and baicalein (aglycone) | [472] | |||||
| Aerial parts: indole alkaloids (melatonin, serotonin); flavonoids (baicalin, baicalein, wogonin, scutellarin) | [473] | |||||
| Herb: flavonoids (viscidulin III, chrysin, baicalein, oroxylin A, wogonin); phenolics (trans-verbascoside, trans-martynoside) | [474] | |||||
| Aerial parts: coumarins (scuteflorin A, scuteflorin B, decursin) | [475] | |||||
| Stem: flavonoids [scutellarin (0.08%)]; phenolic [acteoside (0.05%)] | [476] | |||||
| Root: flavonoids [baicalin (0.05%), baicalein (0.06%), wogonin (0.20%), oroxylin A (0.02%)] | [476] | |||||
| Leaf: flavonoids [scutellarin (0.92%), baicalin (0.05%)] | [476] | |||||
| Aerial parts: flavonoids (apigenin, luteolin, baicalein, wogonin, 6-methoxyluteolin 4′-methyl ether, isoscutellarin 8-O-β-d-glucuronide, apigenin 7-O-β-glucuronide, luteolin 7-O-β-glucuronide, baicalin, wogonin 7-O-β-glucuronide, wogonin 7-O-β-glucuronide methyl ester, eriodictyol, naringenin, naringenin 7-O-β-glucuronide); phenolics (acteoside, nonoside D, leucosceptoside A, martynoside, isoacteoside); lignan (syringaresinol 4′-O-β-d-glucopyranoside) | [477] | |||||
| Aerial parts: flavonoids (norwogonin-7-O-glucuronide, baicalin, dihydrobaicalin, galangin-7-O-glucuronide, dihydrooroxylin A-7-O-glucuronide, oroxylin A-7-O-glucuronide, wogonin-7-O-glucouronide, 5,7-dihydroxy-6,8-dimethoxyflavone-7-O-glucuronide, dihydrowogonin-7-O-glucuronide, baicalein, wogonin, oroxylin A, chrysin); phenolic (5-(β-d-glucosyloxy)-3-hydroxy-trans-stilbene-2-carboxylic acid) | [478] | |||||
| Senecio aureus L. | Asteraceae | Golden ragwort | infusion of plant taken to prevent pregnancy/induce abortions | plant | [15] | |
| Eremophilane sesquiterpenoids (trans-9-oxofuranoeremophilane, 8α-ethoxy-10αH-eremophilenolide, 3α-angeloyloxy-9-oxo-10αH-furanoeremophilane) | [479] | |||||
| Silphium compositum Michx. | Asteraceae | Rosin weed | tonic | plant | [15] | |
| Leaves: flavonoid glycosides (isorhamnetin 3-O-α-l-rhamnosyl (1′′′→6″)-O-β-d-galactopyranoside 7-O-β-l-apiofuranoside, quercetin 3-O-α-l-rhamnosyl(1′′′→6″)-O-β-d-galactopyranoside 7-O-β-l-apiofuranoside, quercetin 3-O-α-l-rhamnosyl (1′′′→6″)-O-β-d-galactopyranoside, quercetin 3-O-α-l-rhamnosyl (1′′′→6″)-O-β-d-glucopyranoside, isorhamnetin 3-O-α-l-rhamnosyl(1′′′→6″)-O-β-d-galactopyranoside, and quercetin 3-O-β-d-galactopyranoside) | [480] | |||||
| Solanum carolinense L. | Solanaceae | Carolina horsenettle | leaf infusion for worms | leaves | [15] | |
| Leaves: steroidal glycoside (carolinoside) is shown to be O-(α-pentulopyranosyl)-(1→4)-O-(α-l-arabinopyranosyl)-(1→1)-d-glucopyranose | [481] | |||||
| Roots: ethyl N,N-bis(4-dimethylaminobutyl) carbamate (solaurethine). Other compounds reported for the first time in this species include solamine (principal base), cuscohygrine and anabasine | [482] | |||||
| Solidago odora Aiton | Asteraceae | Goldenrod | bee stings, sore throat | flowers | [15] | |
| S. odora Aiton fo. odora | Flowering parts EO: methyl chavicol (70.8%), myrcene (12.5%), methyl eugenol (5.8%), limonene (4.5%) | [483] | ||||
| S. odora fo. inodora (A. Gray) Britton | Flowering parts EO: myrcene (31.3%), limonene (27.1%), (E)-methyl isoeugenol (12.9%), β-pinene (6.5%), α-pinene (5.4%), methyl eugenol (4.4%) | [483] | ||||
| Stillingia sylvatica L. | Euphorbi-aceae | Queen′s delight | root tincture for STDs | root | [15] | |
| Roots: stillingia factors S1–S6 (2-hydroxydaphnetoxin diterpenoids) | [484] | |||||
| Symphyotrichum novae-angliae (L.) G.L. Nesom (syn. Aster novae-angliae L.) | Asteraceae | New England aster | root poultice for pain | root | [15] | |
| Leaf EO: (2E)-hexenal (31.0%), α-pinene (16.4%), germacrene D (25.5%), δ-cadinene (14.3%) | [440] | |||||
| Thalictrum dioicum L. | Ranuncu-laceae | Early meadowrue | root infusion for diarrhea | root | [15] | |
| Bis-benzylisoquinoline alkaloids (thalictropine, thalidoxine, pennsylvanine, thalmelatine, thalictrogamine | [485] | |||||
| Thalictrum dioicum | Isopavine alkaloid thalidine | [486] | ||||
| Pallidine and corydine alkaloids | [487] | |||||
| Tilia americana L. | Tiliaceae | American basswood | inner bark decoction for diarrhea, coughs, boils. | bark | [15] | |
| T. americana var. mexicana (Schltdl.) Hardin | Flowers: quercetin and kaempferol derivatives; showed sedative and anxiolytic activity | [488] | ||||
| T. americana var. mexicana | Flowers: tiliroside, quercetin, quercitrin, kaempherol; showed anxiolytic activity | [489] | ||||
| T. americana var. mexicana | Flowers: quercetin; showed analgesic activity | [490] | ||||
| T. americana var. mexicana | Flowers: quercetin, kaempferol; showed anxiolytic activity | [491] | ||||
| T. americana var. mexicana | Flowers and leaves: flavonoids quercetin, rutin, isoquercetin); extract showed anticonvusant activity | [492] | ||||
| Tsuga canadensis (L.) Carrière | Pinaceae | Eastern hemlock | bark poultice for itching skin; stem tips for kidneys | bark, leaves | [15] | |
| Foliar EO: α-pinene (17.6%), camphene (11.5%), isobornyl acetate (43.4%) | [493] | |||||
| Foliar EO: α-pinene (13.2%), camphene (7.8%), isobornyl acetate (42.9%) | [494] | |||||
| Foliar EO: tricyclene (1.6–5.1%), α-pinene (4.1–15.1%), camphene (3.0–11.1%), myrcene (0.5–21.1%), isobornyl acetate (22.0–55.8%), α-humulene (3.6–9.8%), germacrene D (1.4–21.3%) | [495] | |||||
| Foliar EO: tricyclene (3.1–7.8%), α-pinene (11.6–22.7%), camphene (7.8–15.9%), isobornyl acetate (32.8–50.7%), α-humulene (up to 9.2%), germacrene D (up to 6.4%) | [496] | |||||
| Foliar EO: α-pinene (13.9, 5.4%), camphene (13.3, 3.4%), limonene (6.0, 7.0%), piperitone (4.3, 7.7%), isobornyl acetate (38.6, 37.0%) | [497] | |||||
| Viburnum prunifolium L. | Adoxaceae | Black haw shrub | bark infusion as tonic for female bleeding | bark | [15] | |
| Bark: biflavonoid amentoflavone | [498] | |||||
| Bark: iridoid glycosides (2-O-acetyldihydropenstemide, 2-O-trans-p-coumaroyldihydropenstemide, 2-O-acetylpatrinoside, and patrinoside) | [499] | |||||
| Bark: 1-methyl-2,3-dibutyl hemimellitate | [500] | |||||
| Vicia caroliniana Walter | Fabaceae | Vetch | pains, rheumatism | plant | [15] | |
| Aerial parts EO: phytone (2.2–21.5%), methyl roughanate (1.9–29.5%), palmitic acid (9.9–28.1%), (E)-phytol (15.8–36.1%) | [501] | |||||
| Xanthorhiza simplicissima Marshall | Ranuncu-laceae | Yellow root | root infusion for cramps, as tonic | root | [15] | |
| Root: alkaloids (berberine, jatrorrhizine, magnoflorine) | [502] | |||||
| Whole plant: alkaloids berberine and puntarenine | [503] | |||||
| Roots: bisbenzylisoquinoline alkaloids (obamegine and oxyacanthine) | [504] | |||||
| Zanthoxylum americanum Mill. | Rutaceae | Common prickly ash | bark infusion for swollen joints | bark | [15] | |
| Bark: pyranocoumarins (dipetaline, alloxanthoxyletin, xanthoxyletin, xanthyletin) and lignans (sesamin, asarinin) | [505] | |||||
| Zanthoxylum clava-herculis L. | Rutaceae | Hercules′s club | Houma tribe of Native Americans (not Cherokee) used the bark for toothache | bark | [15] | |
| Leaf EO: α-thujene (0.2–5.6%), limonene (43.6–73.0%), 1,8-cineole (12.9–43.3%), linalool (up to 11.3%) | [506] | |||||
| Bark EO: sabinene (47.0%), limonene (18.7%), terpinen-4-ol (12.9%) | [507] | |||||
| Bark: asarinin, sesamin, neoherculin, xanthoxylol-γ,γ-dimethylallyl ether, piperitol-γ,γ-dimethylallyl ether, pluviatol-γ,γ-dimethylallyl ether | [508] | |||||
| Bark: chelerythrine | [509] | |||||
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Setzer, W.N. The Phytochemistry of Cherokee Aromatic Medicinal Plants. Medicines 2018, 5, 121. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines5040121
Setzer WN. The Phytochemistry of Cherokee Aromatic Medicinal Plants. Medicines. 2018; 5(4):121. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines5040121
Chicago/Turabian StyleSetzer, William N. 2018. "The Phytochemistry of Cherokee Aromatic Medicinal Plants" Medicines 5, no. 4: 121. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines5040121