Neurogenic Erectile Dysfunction. Where Do We Stand?
Abstract
:1. Introduction
2. Physiology of Erection
3. Etiology of Neurogenic ED
3.1. Central Nervous System (CNS) Conditions
3.1.1. Spinal Cord Injury (SCI)
3.1.2. Multiple Sclerosis (MS)
3.1.3. Parkinson’s Disease (PD)
3.1.4. Multiple System Atrophy (MSA)
3.1.5. Cerebrovascular Accident (CVA/Stroke)
3.2. Peripheral Neurological Impairment
4. Diagnostic Evaluation
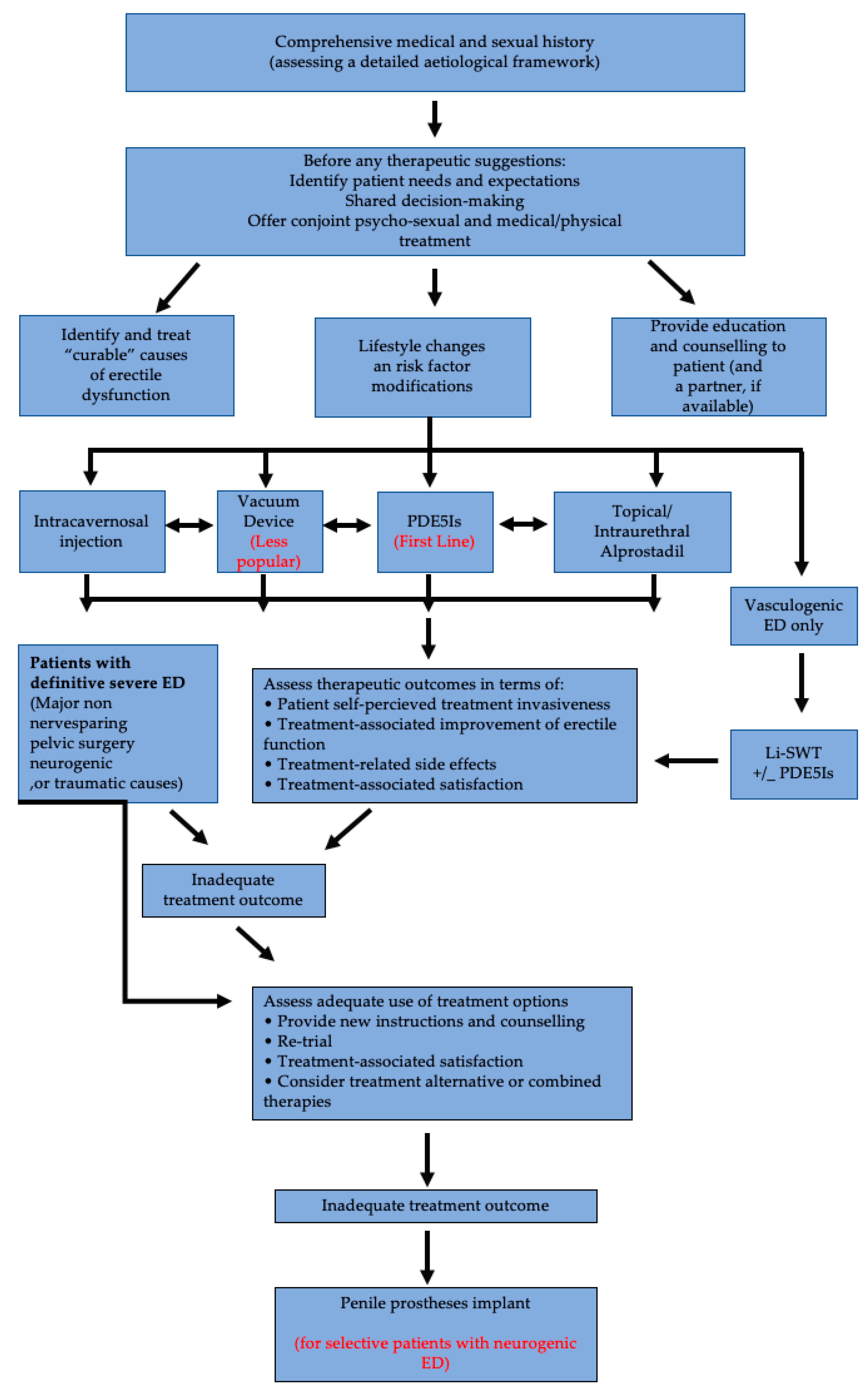
5. Management of Neurogenic Erectile Dysfunction
5.1. Oral Pharmacotherapy
5.1.1. Phosphodiesterase Type 5 Inhibitors (PDE5Is)
5.1.2. Fampridine
5.1.3. Apomorphine
5.2. Local Therapies
5.2.1. Topical/Intraurethral Alprostadil
5.2.2. Vacuum Devices
5.2.3. Intra-Cavernous Injections
5.2.4. Low-Intensity Extra-Corporeal Shock Waves Treatment (LI-ESWT)
5.3. Regenerative Therapeutic Strategies
5.4. Penile Prostheses
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Salonia, A.; Bettocchi, C.; Carvalho, J.; Corona, G.; Jones, T.H.; Kadioglu, A. EAU Guidelines on Sexual and Reproductive Health 2020. In European Association of Urology Guidelines, 2020 ed.; Presented at the EAU Annual Congress Amsterdam 2020; European Association of Urology Guidelines Office: Arnhem, The Netherlands, 2020. [Google Scholar]
- Fisher, W.A.; Eardley, I.; McCabe, M.P.; Sand, M. Erectile Dysfunction (ED) is a Shared Sexual Concern of Couples II: Association of Female Partner Characteristics with Male Partner ED Treatment Seeking and Phosphodiesterase Type 5 Inhibitor Utilization. J. Sex. Med. 2009, 6, 3111–3124. [Google Scholar] [CrossRef] [PubMed]
- Shridharani, A.; Brant, W.O. The treatment of erectile dysfunction in patients with neurogenic disease. Transl. Androl. Urol. 2016, 5, 88–101. [Google Scholar] [PubMed]
- Giuliano, F. Neurophysiology of Erection and Ejaculation. J. Sex. Med. 2011, 8 (Suppl. 4), 310–315. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, F.; Clement, P. Neuroanatomy and physiology of ejaculation. Annu. Rev. Sex Res. 2005, 16, 190–216. [Google Scholar]
- De Tejada, I.S.; Angulo, J.; Cellek, S.; Gonzalez-Cadavid, N.; Heaton, J.; Pickard, R.; Simonsen, U. Physiology of Erectile Function. J. Sex. Med. 2004, 1, 254–265. [Google Scholar] [CrossRef]
- National Spinal Cord Injury Statistical Center. Facts and Figures at a Glance; University of Alabama at Birmingham: Birmingham, AL, USA, 2020; Available online: https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%202020.pdf (accessed on 7 January 2021).
- Anderson, K.D.; Borisoff, J.F.; Johnson, R.D.; Stiens, S.A.; Elliott, S.L. The impact of spinal cord injury on sexual function: Concerns of the general population. Spinal Cord 2007, 45, 328–337. [Google Scholar] [CrossRef]
- Alexander, M.S.; Aisen, C.M.; Alexander, S.M.; Aisen, M.L. Sexual concerns after Spinal Cord Injury: An update on management. NeuroRehabilitation 2017, 41, 343–357. [Google Scholar] [CrossRef]
- Chapelle, P.A.; Durand, J.; Lacert, P. Penile Erection Following Complete Spinal Cord Injury in Man. Br. J. Urol. 1980, 52, 216–219. [Google Scholar] [CrossRef]
- Anderson, K.D.; Borisoff, J.F.; Johnson, R.D.; Stiens, S.A.; Elliott, S.L. Long-term effects of spinal cord injury on sexual function in men: Implications for neuroplasticity. Spinal Cord 2007, 45, 338–348. [Google Scholar] [CrossRef] [Green Version]
- Biering-Sørensen, F.; Sønksen, J. Penile Erection in Men with Spinal Cord or Cauda Equina Lesions. Semin. Neurol. 1992, 12, 98–105. [Google Scholar] [CrossRef]
- Biering-Sørensen, F.; Sønksen, J. Sexual function in spinal cord lesioned men. Spinal Cord 2001, 39, 455–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konstantinidis, C. Erectile Dysfunction in Paraplegic Males, Erectile Dysfunction—Disease-Associated Mechanisms and Novel Insights into Therapy, Kenia Pedrosa Nunes; IntechOpen: London, UK, 2012; Available online: https://www.intechopen.com/books/erectile-dysfunction-disease-associated-mechanisms-and-novel-insights-into-therapy/erectile-dysfunction-in-paraplegic-males (accessed on 7 January 2021). [CrossRef] [Green Version]
- Suh, D.D.; Yang, C.C.; Clowers, D.E. Nocturnal penile tumescence and effects of complete spinal cord injury: Possible physiologic mechanisms. Urology 2003, 61, 184–189. [Google Scholar] [CrossRef]
- Calabrò, R.S.; De Luca, R.; Conti-Nibali, V.; Reitano, S.; Leo, A.; Bramanti, P. Sexual dysfunction in male patients with multiple sclerosis: A need for counseling! Int. J. Neurosci. 2014, 124, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Foley, F.W.; Zemon, V.; Campagnolo, D.; Marrie, R.A.; Cutter, G.; Tyry, T.; Beier, M.; Farrell, E.; Vollmer, T.; Schairer, L. The Multiple Sclerosis Intimacy and Sexuality Questionnaire—Re-validation and development of a 15-item version with a large US sample. Mult. Scler. J. 2013, 19, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.R.; Healy, D.G.; Schapira, A.H.; National Institute for Clinical Excellence. Non-motor symptoms of Parkinson’s disease: Diagnosis and management. Lancet Neurol. 2006, 5, 235–245. [Google Scholar] [CrossRef]
- Bronner, G.; Royter, V.; Korczyn, A.D.; Giladi, N. Sexual Dysfunction in Parkinson’s Disease. J. Sex Marital. Ther. 2004, 30, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, K.B.; Rosa-Grilo, M. Sexual Dysfunctions in Parkinson’s Disease: An Underrated Problem in a Much Discussed Disorder. In International Review of Neurobiology; Elsevier: Amsterdam, The Netherlands, 2017; Volume 134, pp. 859–876. [Google Scholar] [CrossRef]
- Kirchhof, K.; Apostolidis, A.N.; Mathias, C.J.; Fowler, C.J. Erectile and urinary dysfunction may be the presenting features in patients with multiple system atrophy: A retrospective study. Int. J. Impot. Res. 2003, 15, 293–298. [Google Scholar] [CrossRef] [Green Version]
- Papatsoris, A.; Papapetropoulos, S.; Singer, C.; Deliveliotis, C. Urinary and erectile dysfunction in multiple system atrophy (MSA). Neurourol. Urodyn. 2008, 27, 22–27. [Google Scholar] [CrossRef]
- Bener, A.; Al-Hamaq, A.O.; Kamran, S.; Al-Ansari, A. Prevalence of erectile dysfunction in male stroke patients, and associated co-morbidities and risk factors. Int. Urol. Nephrol. 2008, 40, 701–708. [Google Scholar] [CrossRef]
- Koehn, J.; Crodel, C.; Deutsch, M.; Kolominsky-Rabas, P.L.; Hösl, K.M.; Köhrmann, M.; Schwab, S.; Hilz, M.J. Erectile dysfunction (ED) after ischemic stroke: Association between prevalence and site of lesion. Clin. Auton. Res. 2015, 25, 357–365. [Google Scholar] [CrossRef]
- Yuan, J.; Zhang, R.; Yang, Z.; Lee, J.; Liu, Y.; Tian, J.; Qin, X.; Ren, Z.; Ding, H.; Chen, Q.; et al. Comparative Effectiveness and Safety of Oral Phosphodiesterase Type 5 Inhibitors for Erectile Dysfunction: A Systematic Review and Network Meta-analysis. Eur. Urol. 2013, 63, 902–912. [Google Scholar] [CrossRef] [PubMed]
- Schmid, D.M.; Schurch, B.; Hauri, D. Sildenafil in the treatment of sexual dysfunction in spinal cord-injured male patients. Eur. Urol. 2000, 38, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Safarinejad, M.R. Evaluation of the Safety and Efficacy of Sildenafil Citrate for Erectile Dysfunction in Men with Multiple Sclerosis: A Double-Blind, Placebo Controlled, Randomized Study. J. Urol. 2009, 181, 252–258. [Google Scholar] [CrossRef]
- Lombardi, G.; Nelli, F.; Celso, M.; Mencarini, M.; Del Popolo, G. Treating Erectile Dysfunction and Central Neurological Diseases with Oral Phosphodiesterase Type 5 Inhibitors. Review of the Literature. J. Sex. Med. 2012, 9, 970–985. [Google Scholar] [CrossRef] [PubMed]
- Bronner, G.; Vodušek, D.B. Management of sexual dysfunction in Parkinson’s disease. Ther. Adv. Neurol. Disord. 2011, 4, 375–383. [Google Scholar] [CrossRef] [Green Version]
- Cardenas, D.D.; Ditunno, J.F.; Graziani, V.; McLain, A.B.; Lammertse, D.P.; Potter, P.J.; Alexander, M.S.; Cohen, R.; Blight, A.R. Two phase 3, multicenter, randomized, placebo-controlled clinical trials of fampridine-SR for treatment of spasticity in chronic spinal cord injury. Spinal Cord 2014, 52, 70–76. [Google Scholar] [CrossRef] [Green Version]
- Strebel, R.; Reitz, A.; Tenti, G.; Curt, A.; Hauri, D.; Schurch, B. Apomorphine sublingual as primary or secondary treatment for erectile dysfunction in patients with spinal cord injury. BJU Int. 2004, 93, 100–104. [Google Scholar] [CrossRef]
- Padma-Nathan, H.; Hellstrom, W.J.G.; Kaiser, F.E.; Labasky, R.F.; Lue, T.F.; Nolten, W.E.; Norwood, P.C.; Peterson, C.A.; Shabsigh, R.; Tam, P.Y.; et al. Treatment of Men with Erectile Dysfunction with Transurethral Alprostadil. N. Engl. J. Med. 1997, 336, 1–7. [Google Scholar] [CrossRef]
- Moncada, I.; Cuzin, B. Clinical Efficacy and Safety of Vitaros©/Virirec©(Alprostadil Cream) for the Treatment of Erectile Dysfunction. Urol. J. 2015, 82, 84–92. [Google Scholar] [CrossRef]
- Bodner, D.R.; Haas, C.A.; Krueger, B.; Seftel, A.D. Intraurethral alprostadil for treatment of erectile dysfunction in patients with spinal cord injury. Urology 1999, 53, 199–202. [Google Scholar] [CrossRef]
- Zasler, N.D.; Katz, P.G. Synergist erection system in the management of impotence secondary to spinal cord injury. Arch. Phys. Med. Rehabil. 1989, 70, 712–716. [Google Scholar] [PubMed]
- Heller, L.; Keren, O.; Aloni, R.; Davidoff, G. An open trial of vacuum penile tumescence: Constriction therapy for neurological impotence. Spinal Cord 1992, 30, 550–553. [Google Scholar] [CrossRef] [PubMed]
- Denil, J.; Ohl, D.A.; Smythe, C. Vacuum erection device in spinal cord injured men: Patient and partner satisfaction. Arch. Phys. Med. Rehabil. 1996, 77, 750–753. [Google Scholar] [CrossRef]
- Rivas, D.A.; Chancellor, M.B. Complications Associated with the Use of Vacuum Constriction Devices for Erectile Dysfunction in the Spinal Cord Injured Population. J. Am. Paraplegia Soc. 1994, 17, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Chochina, L.; Naudet, F.; Chéhensse, C.; Manunta, A.; Damphousse, M.; Bonan, I.; Giuliano, F. Intracavernous Injections in Spinal Cord Injured Men with Erectile Dysfunction, a Systematic Review and Meta-Analysis. Sex. Med. Rev. 2016, 4, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Vardi, Y.; Appel, B.; Jacob, G.; Massarwi, O.; Gruenwald, I. Can Low-Intensity Extracorporeal Shockwave Therapy Improve Erectile Function? A 6-Month Follow-up Pilot Study in Patients with Organic Erectile Dysfunction. Eur. Urol. 2010, 58, 243–248. [Google Scholar] [CrossRef]
- Hatzichristou, D. Low-Intensity Extracorporeal Shock Waves Therapy (LI-ESWT) for the treatment of erectile dysfunction: Where do we stand? Eur. Urol. 2017, 71, 234–236. [Google Scholar] [CrossRef]
- Frey, A.; Sønksen, J.; Fode, M. Low-intensity extracorporeal shockwave therapy in the treatment of postprostatectomy erectile dysfunction: A pilot study. Scand. J. Urol. 2016, 50, 123–127. [Google Scholar] [CrossRef]
- Usta, M.F.; Gabrielson, A.T.; Bivalacqua, T.J. Low-intensity extracorporeal shockwave therapy in the treatment of erectile dysfunction following radical prostatectomy: A critical review. Int. J. Impot. Res. 2019, 31, 231–238. [Google Scholar] [CrossRef]
- Zewin, T.S.; El-Assmy, A.; Harraz, A.M.; Bazeed, M.; Shokeir, A.A.; Sheir, K.; Mosbah, A. Efficacy and safety of low-intensity shock wave therapy in penile rehabilitation post nerve-sparing radical cystoprostatectomy: A randomized controlled trial. Int. Urol. Nephrol. 2018, 50, 2007–2014. [Google Scholar] [CrossRef]
- Yahata, K.; Kanno, H.; Ozawa, H.; Yamaya, S.; Tateda, S.; Ito, K.; Shimokawa, H.; Itoi, E. Low-energy extracorporeal shock wave therapy for promotion of vascular endothelial growth factor expression and angiogenesis and improvement of locomotor and sensory functions after spinal cord injury. J. Neurosurg. Spine 2016, 25, 745–755. [Google Scholar] [CrossRef] [Green Version]
- Bochinski, D.; Lin, G.T.; Nunes, L.; Carrion, R.; Rahman, N.; Lin, C.-S.; Lue, T.F. The effect of neural embryonic stem cell therapy in a rat model of cavernosal nerve injury. BJU Int. 2004, 94, 904–909. [Google Scholar] [CrossRef] [PubMed]
- Albersen, M.; Fandel, T.M.; Lin, G.; Wang, G.; Banie, L.; Lin, C.-S.; Lue, T.F. Injections of Adipose Tissue-Derived Stem Cells and Stem Cell Lysate Improve Recovery of Erectile Function in a Rat Model of Cavernous Nerve Injury. J. Sex. Med. 2010, 7, 3331–3340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Protogerou, V.; Michalopoulos, E.; Mallis, P.; Gontika, I.; Dimou, Z.; Liakouras, C.; Stavropoulos-Giokas, C.; Kostakopoulos, N.; Chrisofos, M.; Deliveliotis, C. Administration of Adipose Derived Mesenchymal Stem Cells and Platelet Lysate in Erectile Dysfunction: A Single Center Pilot Study. Bioengineering 2019, 6, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achilleos, A.; Trainor, P.A. Neural crest stem cells: Discovery, properties and potential for therapy. Cell Res. 2012, 22, 288–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Y.S.; Lee, H.J.; Park, I.H.; Lim, I.S.; Ku, J.H.; Kim, S.U. Human neural crest stem cells transplanted in rat penile corpus cavernosum to repair erectile dysfunction. BJU Int. 2008, 102, 220–224. [Google Scholar] [CrossRef]
- Gou, X.; He, W.-Y.; Xiao, M.-Z.; Qiu, M.; Wang, M.; Deng, Y.-Z.; Liu, C.-D.; Tang, Z.-B.; Li, J.; Chen, Y. Transplantation of endothelial progenitor cells transfected with VEGF165 to restore erectile function in diabetic rats. Asian J. Androl. 2011, 13, 332–338. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.S.; Lee, S.R.; Woo, Y.K.; Lee, H.J. Stem Cell Therapies for Neurogenic Erectile Dysfunction. Austin J. Urol. 2014, 1, 1015. [Google Scholar]
- Kim, Y.-D.; Yang, S.O.; Lee, J.K.; Jung, T.Y.; Shim, H.B. Usefulness of a malleable penile prosthesis in patients with a spinal cord injury: Penile prosthesis and spinal cord injury. Int. J. Urol. 2008, 15, 919–923. [Google Scholar] [CrossRef]
- Zermann, D.-H.; Kutzenberger, J.; Sauerwein, D.; Schubert, J.; Loeffler, U. Penile Prosthetic Surgery in Neurologically Impaired Patients: Long-Term Followup. J. Urol. 2006, 175, 1041–1044. [Google Scholar] [CrossRef]
- Chung, E. Penile prosthesis implant in the special populations: Diabetics, neurogenic conditions, fibrotic cases, concurrent urinary continence surgery, and salvage implants. Asian J. Androl. 2020, 22, 39–44. [Google Scholar] [CrossRef] [PubMed]
| Neurogenic |
|---|
| CentralCauses |
| Degenerative disorders (e.g., multiple sclerosis, Parkinson’s disease, multiple atrophy, etc.) |
| Spinal cord trauma or diseases |
| Stroke |
| Central nervous system tumours |
| Peripheral Causes |
| Type 1 and 2 diabetes mellitus |
| Chronic renal failure; chronic liver failure |
| Polyneuropathy |
| Surgery (major surgery of pelvis/retroperitoneum) or radiotherapy (pelvis or retroperitoneum) |
| Surgery of the urethra (urethral stricture, urethroplasty, etc.) |
| Patient with ED (Self-Reported) | |||||
| Medical and Psychosexual History (Use of Validated Instruments, e.g., IIEF) History of Neurological Condition | |||||
| Identify other sexual problems, (not ED) | Identify common causes of ED (neurological conditions should be recognized here) | Identify reversible risk factors for ED | Assess psychosocial status | ||
| Focused Physical Examination | |||||
| Penile deformities | Prostatic disease | Signs of hypogonadism | Cardiovascular and neurological status | ||
| Check sensation of perinatal area and integrity of reflective arc sacral parasympathetic centre (S2–S4) (Bulbocavernosus and anal reflexes) | |||||
| Laboratory Tests | |||||
| Glucose-lipid profile (if not assessed in the last 12 months) | Total testosterone (morning sample) if indicated, bio-available or free testosterone | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomas, C.; Konstantinidis, C. Neurogenic Erectile Dysfunction. Where Do We Stand? Medicines 2021, 8, 3. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8010003
Thomas C, Konstantinidis C. Neurogenic Erectile Dysfunction. Where Do We Stand? Medicines. 2021; 8(1):3. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8010003
Chicago/Turabian StyleThomas, Charalampos, and Charalampos Konstantinidis. 2021. "Neurogenic Erectile Dysfunction. Where Do We Stand?" Medicines 8, no. 1: 3. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8010003





