The Role of Poly-Herbal Extract in Sodium Chloride-Induced Oxidative Stress and Hyperlipidemia in Male Wistar Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Source and Extraction
2.2. Preparation of Poly-Herbal Extracts (PHE)
2.3. Acute Toxicity and Determination of LD50
2.4. Animal Grouping and Experimental Design
2.5. Collection of Blood Serum and Tissue Preparation from Treated Rats
2.6. Antioxidant Assays
2.7. Determination of Superoxide Dismutase Activity
2.8. Determination of Glutathione Concentration
2.9. Determination of Glutathione Peroxidase Activity
2.10. Determination of Catalase Activity
2.11. Determination of Malondialdehyde Concentration
2.12. Determination of Nitric Oxide Concentration
2.13. Serum Lipid Assay
2.14. Statistical Analysis
3. Results
3.1. Acute Toxicity Studies of PHE Extracts
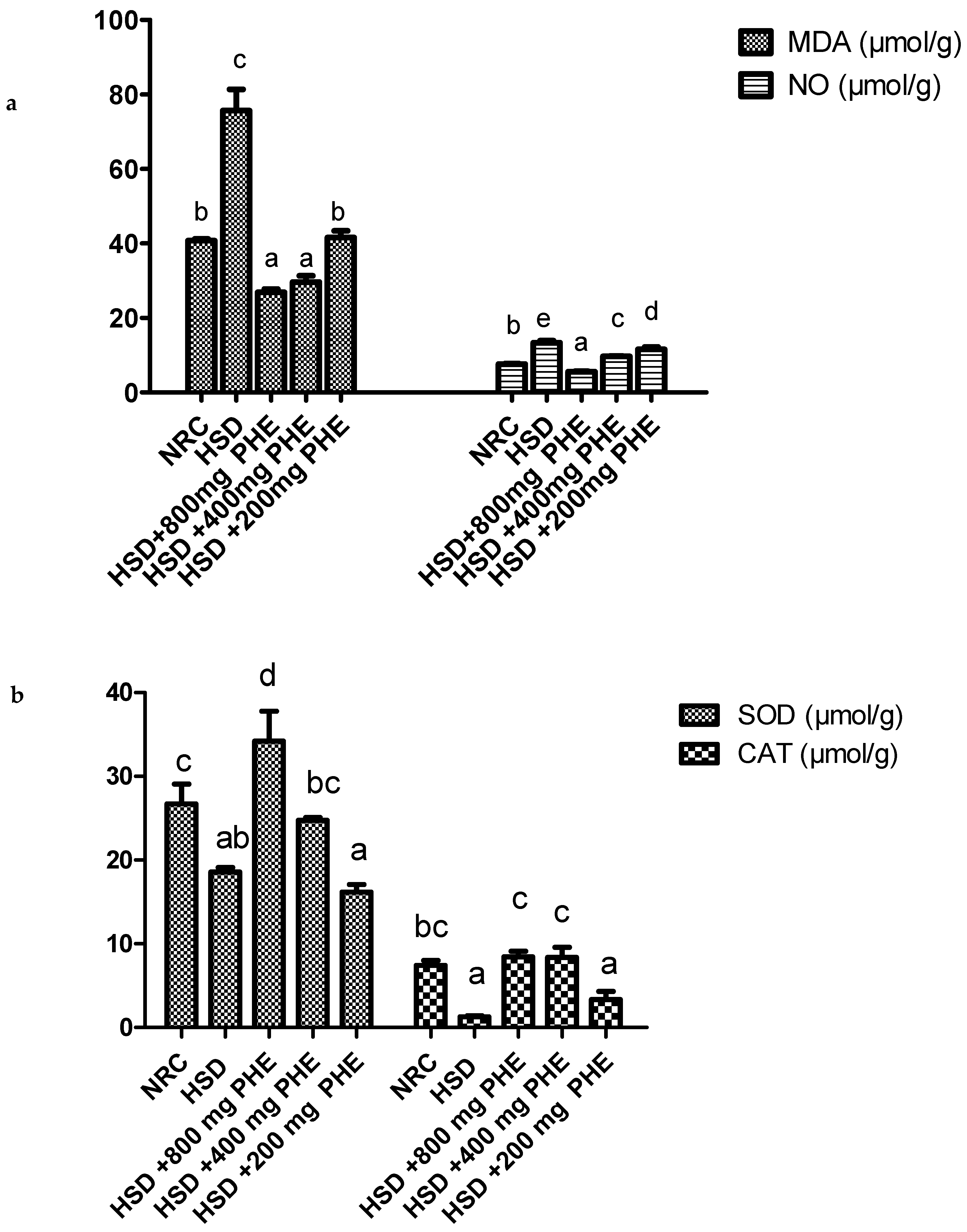
3.2. Antioxidant Status of the Liver
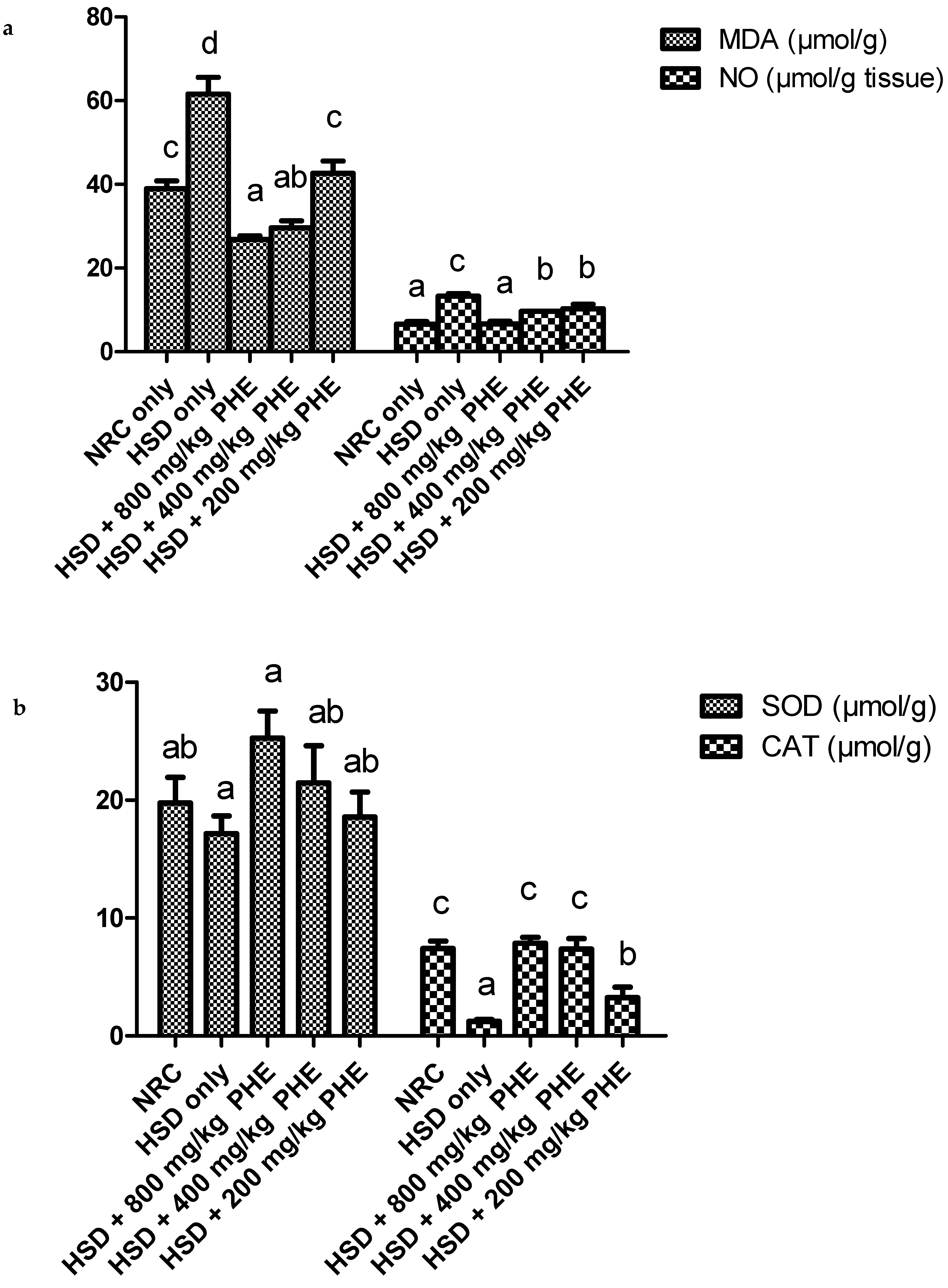
3.3. Antioxidant Status of the Kidney
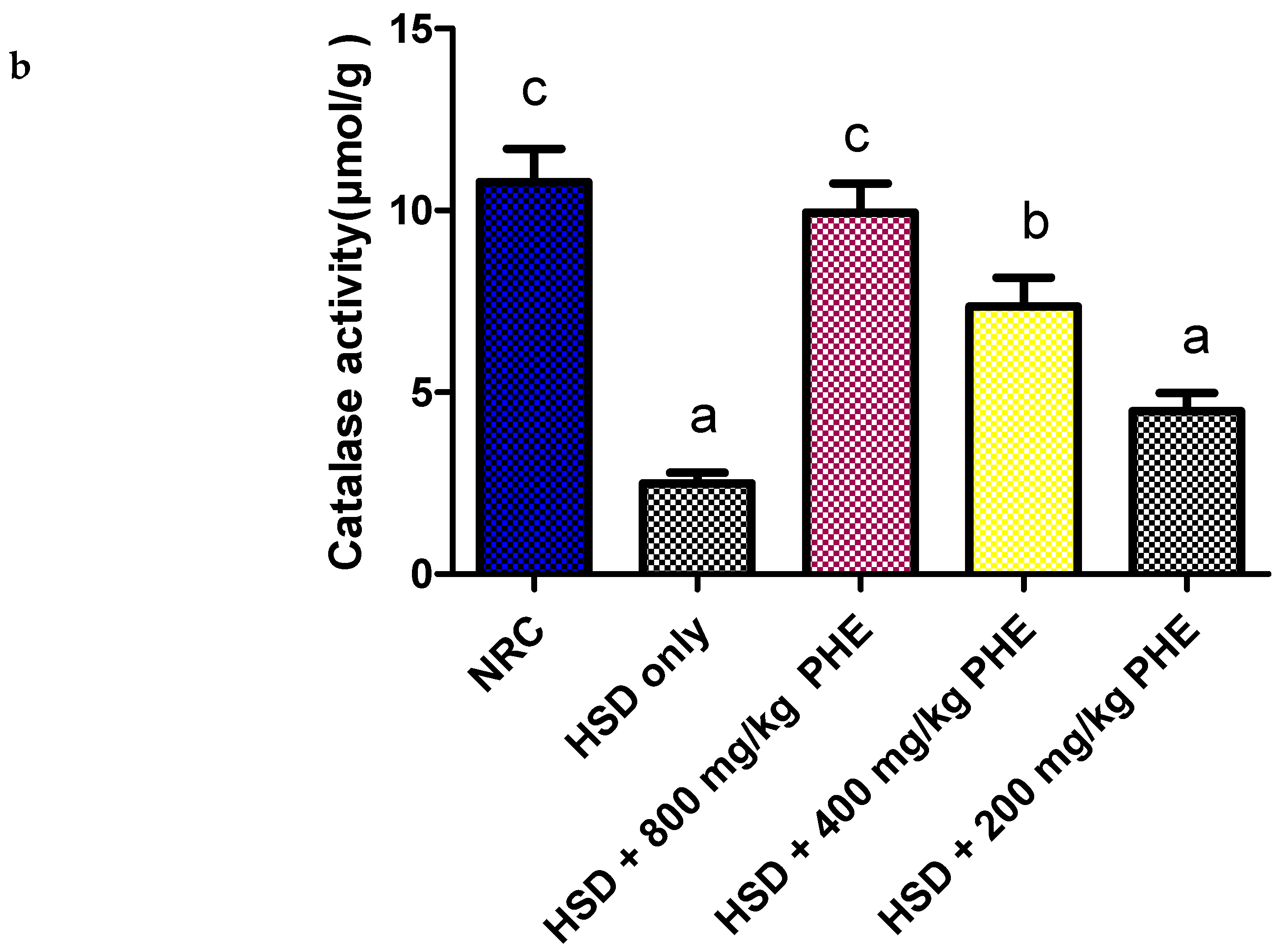
3.4. Antioxidant Status of the Aorta
3.5. Serum Lipid Profile of Treated Rats
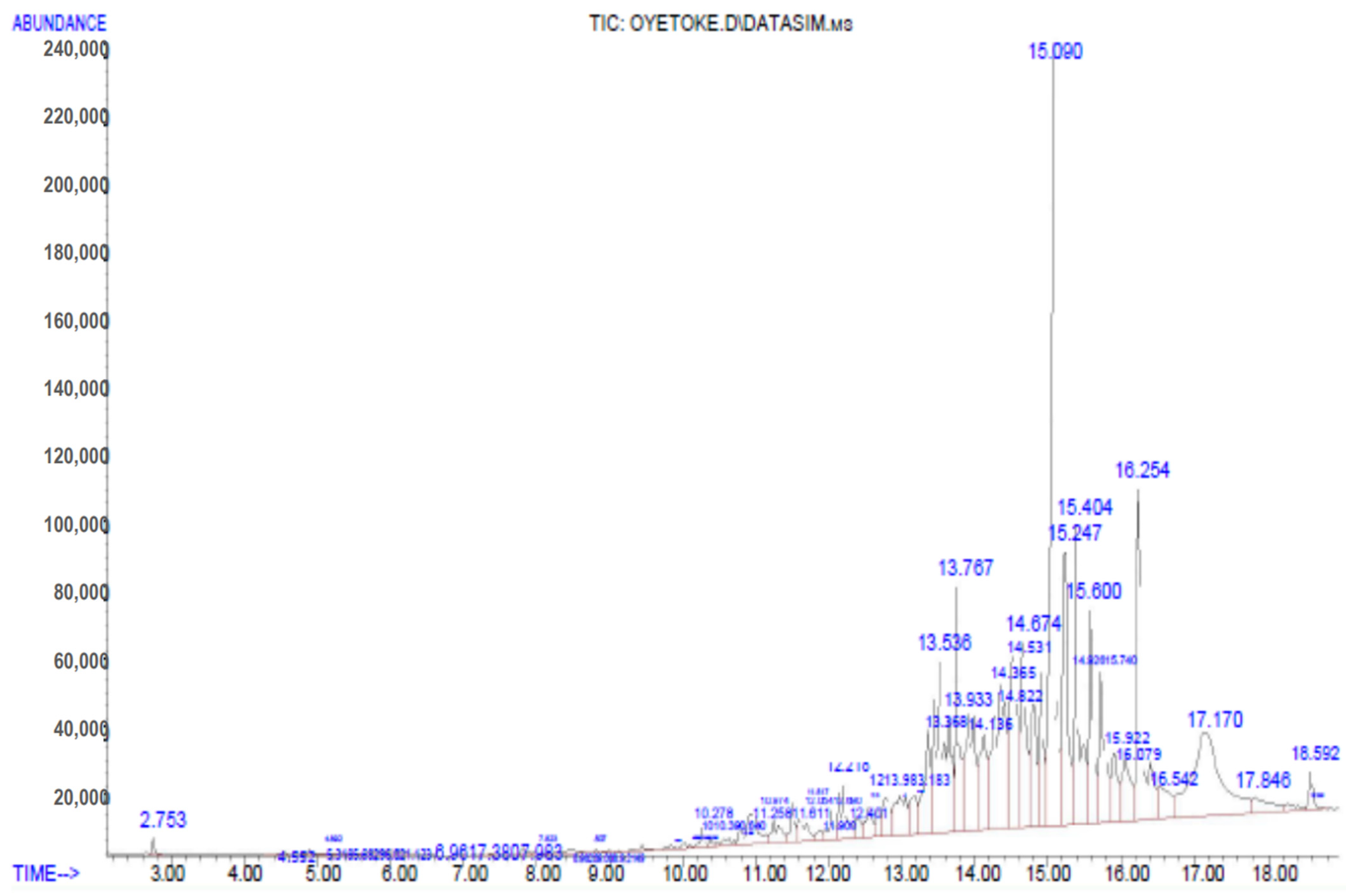
3.6. Gas Chromatography Mass Spectrophotometry (GC-MS) Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent statement
Data Availability Statement
Conflicts of Interest
References
- Jacka, F.N.; Mykletun, A.; Berk, M. Moving towards a population health approach to the primary prevention of common mental disorders. BMC Med. 2012, 10, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, X.-Y.; Yin, X.-X.; Guan, Q.-W.; Xia, Q.-X.; Yang, N.; Zhou, H.-H.; Liu, Z.-Q.; Jin, W.-L. Dietary nutrition for neurological disease therapy: Current status and future directions. Pharmacol. Ther. 2021, 226, 107861. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Casal, M.N.; Mowson, R.; Rogers, L.; Grajeda, R.; Groups, C.W. Risk of excessive intake of vitamins and minerals delivered through public health interventions: Objectives, results, conclusions of the meeting, and the way forward. Ann. N. Y. Acad. Sci. 2019, 1446, 5–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soto-Escageda, J.A.; Vidal, E.B.; Victoria, V.; Chávez, A.V.; Beltran, M.A.; Rodríguez, H.B. Does salt addiction exist. Salud Ment. 2016, 39, 175–181. [Google Scholar] [CrossRef] [Green Version]
- Korosec, Z.; Pravst, I. Assessing the Average Sodium Content of Prepacked Foods with Nutrition Declarations: The Importance of Sales Data. Nutrients 2014, 6, 3501–3515. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Capelin, C.; Dunford, E.K.; Webster, J.L.; Neal, B.C.; Jebb, S.A. Sodium content of processed foods in the United Kingdom: Analysis of 44,000 foods purchased by 21,000 households. Am. J. Clin. Nutr. 2011, 93, 594–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brouillard, A.M.; Deych, E.; Canter, C.; Rich, M.W. Trends in Sodium Intake in Children and Adolescents in the US and the Impact of US Department of Agriculture Guidelines: NHANES 2003–2016. J. Pediatr. 2020, 225, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.R.C.; Rodriguez-Fernandez, R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt Reduction Initiatives around the World—A Systematic Review of Progress towards the Global Target. PLoS ONE 2015, 10, e0130247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyseni, L.; Elliot-Green, A.; Lloyd-Williams, F.; Kypridemos, C.; O’Flaherty, M.; McGill, R. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS ONE 2017, 12, e0177535. [Google Scholar] [CrossRef] [Green Version]
- Umemura, S.; Arima, H.; Arima, S.; Asayama, K.; Dohi, Y.; Hirooka, Y.; Horio, T.; Hoshide, S.; Ikeda, S.; Ishimitsu, T.; et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens. Res. 2019, 42, 1235–1481. [Google Scholar] [CrossRef]
- WHO. Recommendations for Salt Reduction. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 15 September 2020).
- Anderson, C.A.; Appel, L.J.; Okuda, N.; Brown, I.J.; Chan, Q.; Zhao, L.; Ueshima, H.; Kesteloot, H.; Miura, K.; Curb, J.D.; et al. Dietary Sources of Sodium in China, Japan, the United Kingdom, and the United States, Women and Men Aged 40 to 59 Years: The INTERMAP Study. J. Am. Diet. Assoc. 2010, 110, 736–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kloss, L.; Meyer, J.D.; Graeve, L.; Vetter, W. Sodium intake and its reduction by food reformulation in the European Union—A review. NFS J. 2015, 1, 9–19. [Google Scholar] [CrossRef] [Green Version]
- Grau, R.; Andrés, A.M.; Barat, J.M. Principles of Drying. In Handbook of Fermented Meat and Poultry; Wiley: Hoboken, NJ, USA, 2014; pp. 31–38. [Google Scholar]
- Ayed, C.; Lim, M.; Nawaz, K.A.; Macnaughtan, W.; Sturrock, C.J.; Hill, S.E.; Linforth, R.; Fisk, I.D. The role of sodium chloride in the sensory and physico-chemical properties of sweet biscuits. Food Chem. 2021, 9, 100115. [Google Scholar]
- Wang, G.; Yeung, C.-K.; Zhang, J.-L.; Hu, X.-W.; Ye, Y.-X.; Yang, Y.-X.; Li, J.-C.; Lee, K.; Yang, X.; Wang, L.-J. High salt intake negatively impacts ovarian follicle development. Ann. Anat. Anat. Anz. 2015, 200, 79–87. [Google Scholar] [CrossRef]
- Han, S.; Cheng, D.; Liu, N.; Kuang, H. The relationship between diabetic risk factors, diabetic complications and salt intake. J. Diabetes Complicat. 2018, 32, 531–537. [Google Scholar] [CrossRef]
- He, F.J.; Tan, M.; Ma, Y.; MacGregor, M. Salt Reduction to Prevent Hypertension and Cardiovascular Disease JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 632–647. [Google Scholar] [CrossRef]
- Shimosawa, T. Salt, the renin–angiotensin–aldosterone system and resistant hypertension. Hypertens. Res. 2013, 36, 657–660. [Google Scholar] [CrossRef] [Green Version]
- Mattson, D.L. Infiltrating immune cells in the kidney in salt-sensitive hypertension and renal injury. Am. J. Physiol. Physiol. 2014, 307, F499–F508. [Google Scholar] [CrossRef] [Green Version]
- Fehrenbach, D.J.; Abais-Battad, J.M.; Dasinger, J.H.; Lund, H.; Mattson, D.L. Salt-sensitive increase in macrophages in the kidneys of Dahl SS rats. Am. J. Physiol. Physiol. 2019, 317, F361–F374. [Google Scholar] [CrossRef] [PubMed]
- Harvey, A.L.; Edrada-Ebel, R.; Quinn, R.J. The re-emergence of natural products for drug discovery in the genomics era. Nat. Rev. Drug Discov. 2015, 14, 111–129. [Google Scholar] [CrossRef] [Green Version]
- Ruhsam, M.; Hollingsworth, P.M. Authentication of Eleutherococcus and Rhodiola herbal supplement products in the United Kingdom. J. Pharm. Biomed. Anal. 2018, 149, 403–409. [Google Scholar] [CrossRef]
- Zhao, C.; Li, S.; Zhang, J.; Huang, Y.; Zhang, L.; Zhao, F.; Du, X.; Hou, J.; Zhang, T.; Shi, C.; et al. Current state and future perspective of cardiovascular medicines derived from natural products. Pharmacol. Ther. 2020, 216, 107698. [Google Scholar] [CrossRef] [PubMed]
- Elkordy, A.A.; Haj-Ahmad, R.R.; Awaad, A.S.; Zaki, R.M. An overview on natural product drug formulations from conventional medicines to nanomedicines: Past, present and future. J. Drug Deliv. Sci. Technol. 2021, 63, 102459. [Google Scholar] [CrossRef]
- Ji, S.; Fattahi, A.; Raffel, N.; Hoffmann, I.; Beckmann, M.W.; Dittrich, R.; Schrauder, M. Antioxidant effect of aqueous extract of four plants with therapeutic potential on gynecological diseases; semen persicae, Leonurus cardiaca, Hedyotis diffusa, and Curcuma zedoaria. Eur. J. Med. Res. 2017, 22, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pole, S. Ayurvedic Medicine: The Principles of Traditional Practice; Jessica Kingsley Publishers: London, UK, 2013. [Google Scholar]
- Parasuraman, S.; Thing, G.S.; Dhanaraj, S.A. Poly-herbal formulation: Concept of ayurveda. Pharmacogn. Rev. 2014, 8, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Van Wyk, B.E. A review of commercially important African medicinal plants. J. Ethnopharmacol. 2015, 24, 118–134. [Google Scholar] [CrossRef]
- Walid, R.; Hafidaa, M.; Abdelhamid, E.H.; Redae, B.; Rachidf, A.; Mohamed, B. Beneficial effects of Aloe vera gel on lipid profile, lipase activities and oxidant/antioxidant status in obese rats. J. Funct. Foods 2018, 48, 525–532. [Google Scholar]
- Taukoorah, U.; Mahomoodally, M.F. Crude Aloe vera gel shows antioxidant propensities and inhibits pancreatic lipase and glucose movement in vitro. Adv. Pharmacol. Sci. 2016, 2016, 3720850. [Google Scholar]
- Padayachee, B.; Baijnath, H. An updated comprehensive review of the medicinal, phytochemical and pharmacological properties of Moringa oleifera. S. Afr. J. Bot. 2020, 129, 304–316. [Google Scholar] [CrossRef]
- Lorke, D. A new approach to practical acute toxicity testing. Arch. Toxicol. 1983, 54, 275–287. [Google Scholar] [CrossRef]
- Misra, H.P.; Fridovich, I. The role of superoxide anion in the autooxidation of epinephrine and simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [CrossRef]
- Ellman, G.L. Tissue sulfhydryl groups. Arch. Biochem. Biophys. 1959, 82, 70–77. [Google Scholar] [CrossRef]
- Reddy, K.P.; Subhani, S.M.; Khan, P.A.; Kumar, K.B. Effect of light and benzyladenine and desk treated growing leaves, Changes in the peroxidase activity. Cell Physiol. 1995, 26, 984. [Google Scholar]
- Clairborne, A. Catalase Activity. In Handbook of Methods for Oxygen Radical Research; Greenwald, R.A., Ed.; CRC Press: Boca Raton, FL, USA, 1985; pp. 283–284. [Google Scholar]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef]
- Tsikas, D. ReviewMethods of quantitative analysis of the nitric oxide metabolites nitrite and nitrate in human biological fluids. Free. Radic. Res. 2005, 39, 797–815. [Google Scholar] [CrossRef] [PubMed]
- Parakh, A.C.; Jank, A.H. Free and Total Cholesterol in Clinical Laboratory Methods; Mosby: Toronto, ON, Canada, 1982; pp. 546–549. [Google Scholar]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, Without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Dmitrieva, N.I.; Park, J.-H.; Levine, R.L.; Burg, M.B. From the Cover: High urea and NaCl carbonylate proteins in renal cells in culture and in vivo, and high urea causes 8-oxoguanine lesions in their DNA. Proc. Natl. Acad. Sci. USA 2004, 101, 9491–9496. [Google Scholar] [CrossRef] [Green Version]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.D.; Mazur, M.; Telser, J. Free radicals and antioxidants in normal physiological functions and human disease. Int. J. Biochem. Cell Biol. 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, Y.-L.; He, S.-W.; Chen, M.-H.; Zhang, Z.; Fu, X.-P.; Fu, B.-B.; Liao, B.-Q.; Lin, Y.-H.; Qi, Z.-Q.; et al. Protective effects of resveratrol against mancozeb induced apoptosis damage in mouse oocytes. Oncotarget 2016, 8, 6233–6245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pham-Huy, L.A.; He, H.; Pham-Huy, C. Free Radicals, Antioxidants in Disease and Health. Int. J. Biomed. Sci. IJBS 2008, 4, 89–96. [Google Scholar] [PubMed]
- Singh, Z.; Karthigesu, I.; Singh, P.; Kaur, R. Use of Malondialdehyde as a biomarker for assessing oxidative Stress in Different Disease Pathologies: A Review. Iran. J. Publ. Health 2014, 43, 7–16. [Google Scholar]
- Esterbauer, H.; Schaur, R.J.; Zollner, H. Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and related aldehydes. Free. Radic. Biol. Med. 1991, 11, 81–128. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, S.Y.; Hsu, T.; Santella, R.M. Immuno histochemical detection of malondialdehyde-DNA adducts in human oral mucosa cells. Carcinogenesis 2002, 23, 207–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luis, J.M.; Morales, A.; Blasco, C. Critical role of mitochondrial glutathione in the survival of hepatocytes during hypoxia. J. Biol. Chem. 2005, 280, 3224–3232. [Google Scholar] [CrossRef] [Green Version]
- Nahrevanian, H.; Dascombe, M.J. Oxide and its up/downstream molecules in malaria: Cytotoxic or preventive? Southeast Asian J. Trop. Med. Public Health 2003, 34, 4–50. [Google Scholar]
- Bian, K.; Doursout, M.-F.; Murad, F. Vascular System: Role of Nitric Oxide in Cardiovascular Diseases. J. Clin. Hypertens. 2008, 10, 304–310. [Google Scholar] [CrossRef]
- Nahrevanian, H.; Amini, M. The role of nitric1. Nitric Oxide Functions; an Emphasis on its Diversity in Infectious Diseases. Iran. J. Basic Med. Sci. 2009, 11, 197–204. [Google Scholar]
- Khazan, M.; Hdayati, M. The Role of Nitric Oxide in Health and Diseases. Scimetr 2014, 3, 20987. [Google Scholar] [CrossRef]
- Ighodaro, O.M.; Akinloye, O.A. First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alex. J. Med. 2018, 54, 287–293. [Google Scholar] [CrossRef] [Green Version]
- Franco, R.; Schoneveld, O.J.; Pappa, A.; Panayiotidis, M.I. The central role of glutathione in the pathophysiology of human diseases. Arch. Physiol. Biochem. 2007, 113, 234–258. [Google Scholar] [CrossRef]
- Liu, M.; Deng, M.; Luo, Q.; Dou, X.; Jia, Z. High-Salt Loading Downregulates Nrf2 Expression in a Sodium-Dependent Manner in Renal Collecting Duct Cells. Front. Physiol. 2020, 10, 1565. [Google Scholar] [CrossRef]
- Bayorh, M.A.; Ganafa, A.A.; Socci, R.R.; Silvestrov, N.; Abukhalaf, I.K. The role of oxidative stress in salt-induced hypertension. Am. J. Hypertens. 2004, 17, 31–36. [Google Scholar] [CrossRef] [Green Version]
- Saidu, Y.; Bilbis, L.; Muhammad, S.A.; Nasir, M.K. Serum Lipid Profile and Antioxidant Status of Salt- induced Hypertensive Rats Treated with an Antioxidants Rich Nutraceutical. Cameroon J. Exp. Biol. 2012, 8, 47–54. [Google Scholar]
- Lee, E.Y.; Cho, K.H. High-dose consumption of NaCl resulted in severe degradation of lipoproteins associated with hyperlipidemia, hyperglycemia, and infertility via impairment of testicular spermatogenesis. Toxicol. Res. 2016, 5, 557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omage, K.; Azeke, M.A.; Omage, S.O. Evaluation of the efficacy of Acalypha wilkesiana leaves in managing cardiovascular disease risk factors in rabbits exposed to salt-loaded diets. Clin. Phytoscience 2018, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Uche, O.K.; Osakpolor, F.A. Kolaviron Attenuates Elevation in Blood Pressure and Ameliorates Dyslipidemia in Salt-Induced Hypertensive Sprague-Dawley Rats. Afr. J. Biomed. Res. 2018, 21, 219–224. [Google Scholar]
- Ginsberg, H.N.; Goldberg, I.J. Disorders of Lipoprotein Metabolism. In Harrison’s Principles of Internal Medicine, 15th ed.; McGraw Hill: New York, NY, USA, 2001; pp. 2245–2256. [Google Scholar]
- NCEP. Summary of the Second Report of the National Cholesterol, Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Cholesterol in Adults (Adult Treatment Panel II). JAMA 1993, 269, 3015–3023. [Google Scholar] [CrossRef]
- George, V.C.; Kumar, D.R.N.; Suresh, P.K.; Kumar, R.A. Antioxidant, DNA protective efficacy and HPLC analysis of Annona muricata (soursop) extracts. J. Food Sci. Technol. 2015, 52, 2328–2335. [Google Scholar] [CrossRef]
- Justino, A.B.; Miranda, N.C.; Franco, R.R.; Martins, M.M.; da Silva, N.M.; Espindola, F.S. Annona muricata Linn. leaf as a source of antioxidant compounds with in vitro antidiabetic and inhibitory potential against α-amylase, α-glucosidase, lipase, non-enzymatic glycation and lipid peroxidation. Biomed. Pharmacother. 2018, 100, 83–92. [Google Scholar] [CrossRef]
- Oyedepo, T.; Babarinde, S.O.; Ajayeoba, T.A. Evaluation of Anti-hyperlipidemic Effect of Aqueous Leaves Extract of Moringa oleifera in Alloxan Induced Diabetic Rats. Int. J. Biochem. Res. Rev. 2013, 3, 162–170. [Google Scholar] [CrossRef] [Green Version]
- Venkateswaran, V.; Rassak, R.A.; Sudaram, R.S.; Sambathkumar, R. Evaluation of Antihyperlipidemic Activity of Ethanolic Root Extract of Carica Papaya in Poloxamer—407 Induced Hyperlipidemia in Wistar Rats. Am. J. PharmTech Res. 2017, 7, 36–43. [Google Scholar]
- Ukpabi, C.F.; Chukwu, M.; Onyemaechi, J.N.; Ibe, P.; Onuh, E.F. Antidiabetic and Antihyperlipidemic Effects of Aqueous Extract of Carica papaya Leaf on the Experimental Model against Single Alloxan Toxicity. World Sci. Res. 2019, 6, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Shin, E.; Shin, S.; Kong, H.; Lee, S.; Do, S.; Lee, C. Dietary aloe reduces adipogenesisvia the activation of AMPK and suppresses obesity-related inflammation in obese mice. Immune Netw. 2011, 11, 107–113. [Google Scholar] [CrossRef] [Green Version]
- Dhingra, D.; Lamba, D.; Kumar, R.; Nath, P.; Gauttam, S. Anti-hyperlipidemic activity of Aloe succotrina in rats: Possibly mediated by inhibition of HMG-CoA reductase. ISRN Pharmacol. 2014, 24357. [Google Scholar] [CrossRef] [Green Version]
- Nomaguchia, K.; Tanakaa, M.; Misawaa, E.; Yamadaa, M.; Toidaa, T.; Iwatsukia, K.; Gotob, T.; Kawadab, T. Aloe vera phytosterols act as ligands for PPAR and improve the expression levels of PPAR target genes in the livers of mice with diet-induced obesity. Obes. Res. Clin. Pract. 2011, 5, e190–e201. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.P.; Son, T.G.; Camandola, S. Viewpoint: Mechanisms of Action and Therapeutic Potential of Neurohormetic Phytochemicals. Dose Response 2007, 5, 174–186. [Google Scholar] [CrossRef]
- Calabrese, E.J. Neuroscience and Hormesis: Overview and General Findings. Crit. Rev. Toxicol. 2008, 38, 249–252. [Google Scholar] [CrossRef]
- Scapagnini, G.; Sonya, V.; Nader, A.G.; Calogero, C.; Zella, D.; Fabio, G. Modulation of Nrf2/ARE Pathway by Food Polyphenols: A Nutritional Neuroprotective Strategy for Cognitive and Neurodegenerative Disorders. Mol. Neurobiol. 2011, 44, 192–201. [Google Scholar] [CrossRef] [Green Version]
- Barrajon-Catalan, E.; Herranz-Lopez, M.; Joven, J. Molecular promiscuity of plant polyphenols in the management of age-related diseases: Far beyond their antioxidant properties. Adv. Exp. Med. Biol. 2014, 824, 141–159. [Google Scholar]
- Santos-Sánchez, N.F.; Salas-Coronado, R.; Villanueva-Cañongo, C.; Hernández-Carlos, B. Antioxidant Compounds and Their Antioxidant Mechanism. In Antioxidants; IntechOpen: London, UK, 2019. [Google Scholar]
- Silva, G.; Neto, A.; Moura, A.; Sousa, H.; Lavor, E.; Vasconcelos, P.; Macêdo, D.S.; Sousa, D.; Vasconcelos, S.; Sousa, F. Effects of isopulegol on pentylenetetrazol-induced convulsions in mice: Possible involvement of GABAergic system and antioxidant activity. Fitoterapia 2008, 80, 506–513. [Google Scholar] [CrossRef]
- Roussaki, M.; Kontogiorgis, C.A.; Litina, H.D.; Hamilakis, S.; Detsi, A. A novel synthesis of 3- aryl coumarins and evaluation of their antioxidant and lipoxygenase inhibitory activity. Bioorg. Med. Chem. Lett. 2010, 20, 3889–3892. [Google Scholar] [CrossRef]
- Veselinović, J.B.; Veselinović, A.M.; Vitnik, Z.; Vitnik, V.; Nikolić, G. Antioxidant properties of selected 4-phenyl hydroxycoumarins: Integrated in vitro and computational studies. Chem. Interact. 2014, 214, 49–56. [Google Scholar] [CrossRef]
- Sreekanth, T.; Kavitha, N.; Anusha, S.; Rajeshwar, Y. Design, synthesis, characterization, antioxidant and in vitro cytotoxic activities of novel coumarin thiazole derivatives. Med. Chem. Res. 2015, 24, 1162–1169. [Google Scholar]
- Veselinović, J.B.; Veselinović, A.M.; Nikolić, G.; Pesic, S.; Stojanovic, D.; Matejić, J.S.; Mihajilov-Krstev, T.M. Antibacterial potential of selected 4-phenyl hydroxycoumarins: Integrated in vitro and molecular docking studies. Med. Chem. Res. 2015, 24, 1626–1634. [Google Scholar] [CrossRef]
- Locatelli, M.; Epifano, F.; Genovese, S.; Carlucci, S.; Končić, M.Z.; Kosalec, I.; Kremer, D. Anthraquinone Profile, Antioxidant and Antimicrobial Properties of Bark Extracts of Rhamnus catharticus and R. orbiculatus. Nat. Prod. Commun. 2011, 6, 1276–1280. [Google Scholar] [CrossRef] [Green Version]
- Mellado, M.; Madrid, A.; Eña-Cortés, H.; López, R.; Jara, C.; Espinoza, L. Antioxidant Activity of Anthraquinones Isolated From Leaves Of Muehlenbeckia Hastulata(J.E. Sm.) Johnst (Polygonaceae). Chil. Chem. Soc. 2013, 58, 1767–1770. [Google Scholar] [CrossRef] [Green Version]
- Yang, T.-C.; Chao, H.-F.; Shi, L.-S.; Chang, T.-C.; Lin, H.-C.; Chang, W.-L. Alkaloids from Coptis chinensis root promote glucose uptake in C2C12 myotubes. Fitoterapia 2014, 93, 239–244. [Google Scholar] [CrossRef] [PubMed]


| Groups | Treatment |
|---|---|
| 1 | Fed with normal rat chow only (positive control) |
| 2 | Fed with 16% salt diet only (negative control) |
| 3 | Fed with 16% salt diet and 800 mg/kg of the poly-herbal extract once daily |
| 4 | Fed with 16% salt diet and 400 mg/kg of the poly-herbal extract once daily |
| 5 | Fed with 16% salt diet and 200 mg/kg of the poly-herbal extract once daily |
| Treatment | GSH (µmol/g) | GPX (µmol/g) | GST (µmol/g) |
|---|---|---|---|
| NRC | 2.77 ± 0.30 ab | 0.63 ± 0.04 bc | 5.90 ± 0.91 b |
| HSD only | 2.29 ± 0.44 ab | 0.55 ± 0.01 ab | 3.34 ± 0.54 a |
| HSD + 800 mg/kg PHE | 3.25 ± 0.38 b | 0.81 ± 0.07 d | 6.37 ± 0.81 b |
| HSD + 400 mg/kg PHE | 2.67 ± 0.08 ab | 0.73 ± 0.01 cd | 5.66 ± 0.55 b |
| HSD + 200 mg/kg PHE | 2.04 ± 0.23 a | 0.42 ± 0.05 a | 4.34 ± 0.54 ab |
| Treatment | GSH (µmol/g) | GPX (µmol/g) | GST (µmol/g) |
|---|---|---|---|
| NRC only | 1.61 ± 0.25 bc | 0.55 ± 0.02 b | 2.41 ± 0.39 b |
| HSD only | 0.91 ± 0.04 a | 0.31 ± 0.04 a | 0.50 ± 0.13 a |
| HSD + 800 mg/kg PHE | 1.68 ± 0.15 bc | 1.09 ± 0.03 d | 2.41 ± 0.39 b |
| HSD + 400 mg/kg PHE | 1.50 ± 0.16 bc | 0.76 ± 0.05 c | 1.39 ± 0.13 ab |
| HSD + 200 mg/kg PHE | 1.09 ± 0.02 ab | 0.76 ± 0.06 c | 0.50 ± 0.01 a |
| Treatment | GSH (µmol/g) | GPX (µmol/g) | GST (µmol/g) |
|---|---|---|---|
| NRC only | 2.77 ± 0.3 ab | 0.63 ± 0.04 b | 5.90 ± 0.91 b |
| HSD only | 1.93 ± 0.25 a | 0.51 ± 0.03 a | 3.34 ± 0.54 a |
| HSD + 800 mg/kg PHE | 3.25 ± 0.38 b | 0.71 ± 0.04 b | 6.37 ± 0.81 b |
| HSD + 400 mg/kg PHE | 2.67 ± 0.08 ab | 0.66 ± 0.05 b | 5.61 ± 0.55 b |
| HSD + 200 mg/kg PHE | 2.03 ± 0.23 a | 0.68 ± 0.04 b | 4.34 ± 0.54 ab |
| Treatment | HDL (mg/dL) | LDL (mg/dL) |
|---|---|---|
| NRC only | 6.63 ± 0.43 ab | 35.06 ± 1.97 c |
| HSD only | 4.91 ± 0.85 a | 163.29 ± 1.59 f |
| HSD + 800 mg/kg PHE | 22.83 ± 0.72 d | 9.67 ± 1.67 a |
| HSD + 400 mg/kg PHE | 21.99 ± 0.64 d | 27.25 ± 2.69 b |
| HSD + 200 mg/kg PHE | 12.09 ± 1.20 c | 89.30 ± 3.76 e |
| Retention Time | Identified Compounds | Peak Area % | |
|---|---|---|---|
| 1 | 2.651 | Arsenous acid, tris(trimethylsilyl)ester | 0.09 |
| 2 | 2.905 | 2,4-Cyclohexadien-1-one | 0.07 |
| 3 | 3.271 | Cyclotrisiloxane, hexamethyl- | 0.21 |
| 4 | 3.834 | 1,4-Bis(trimethylsilyl)benzene | 1.18 |
| 5 | 4.341 | Tris(tert-butyldimethylsilyloxy)arsane | 0.05 |
| 6 | 4.398 | 1,1,1,3,5,5,5-Heptamethyltrisiloxane | 0.06 |
| 7 | 4.764 | 4-Methyl-2-trimethylsilyloxy-acetophenone | 0.13 |
| 8 | 4.905 | 1,3,5,7-Cyclooctatetraene | 0.39 |
| 9 | 5.327 | Cyclotetrasiloxane, octamethyl- | 0.14 |
| 10 | 5.440 | Trans-4-Dimethylamino-4’-methoxych alcone | 0.39 |
| 11 | 5.834 | 1,1,3,3,5,5,7,7-Octamethyl-7-(2-methylpropoxy) tetrasiloxan-1-ol | 0.26 |
| 17 | 6.961 | 1,1,1,3,5,5,5Heptamethyltrisiloxane | 0.05 |
| 18 | 7.158 | Arsenous acid, tris(trimethylsilyl) ester | 0.04 |
| 19 | 7.468 | 1,2-Bis(trimethylsilyl)benzene | 0.11 |
| 20 | 7.722 | 1,1,1,3,5,5,5Heptamethyltrisiloxane 1H-Indole | 0.04 |
| 22 | 8.510 | Cyclopentasiloxane, decamethyl- | 1.22 |
| 23 | 8.736 | 5-Methyl-2-phenylindolizine | 0.12 |
| 24 | 9.017 | 3,3-Diisopropoxy-1,1,1,5,5,5-hexam ethyltrisiloxane. | 0.05 |
| 25 | 9.186 | 1,2,4Triazolo[1,5-a]pyrimidine-6-carboxylic acid | 0.04 |
| 26 | 9.327 | Silane | 0.10 |
| 27 | 9.863 | Octasiloxane, 1,1,3,3,5,5,7,7,9,9, 11,11,13,13,15,15-hexadecamethyl- | 0.23 |
| 28 | 10.144 | 4-Bromo-3-chloroaniline | 0.32 |
| 29 | 10.285 | Cyclohexasiloxane, dodecamethyl- | 1.47 |
| 30 | 10.651 | Heptasiloxane, 1,1,3,3,5,5,7,7,9,9,11,11,13,13-tetradecamethyl- | 0.54 |
| 31 | 10.961 | Alpha.-D-Ribofuranoside ((2-pyridy l)-2,3-O-isopropylidene-1-thio- | 1.28 |
| 32 | 11.384 | Coumarin | 1.01 |
| 33 | 11.609 | Cycloheptasiloxane, tetradecamethy1- | 1.85 |
| 34 | 11.947 | Anthracene, 9,10-diethyl-9,10-dihydro- | 0.38 |
| 35 | 12.313 | 3-Quinolinecarboxylic acid, 6,8-di fluoro-4-hydroxy-, ethyl ester | 1.15 |
| 36 | 12.595 | 2-Ethylacridine | 0.74 |
| 37 | 12.680 | Cyclooctasiloxane, hexadecamethyl- | 1.02 |
| 38 | 12.792 | 5,5’-Di(ethoxycarbonyl)-3,3’-dimethyl-4,4’-dipropyl-2,2’-dipyrrylmethane | 0.97 |
| 39 | 13.018 | Trans-3-Ethoxy-b-methyl-b-nitrostyrene | 1.58 |
| 40 | 13.187 | Corydaldine | 1.11 |
| 41 | 13.356 | Benzene, 1,1’-(1,2-cyclobutanediyl)bis-,trans- | 5.15 |
| 42 | 13.778 | Isopulegol | 1.78 |
| 43 | 13.947 | Bicyclo[4.1.0]hepta-2,4-diene, 2,3,4,5-tetraethyl-7,7-diphenyl- | 2.93 |
| 44 | 14.144 | 2-Methyl-7-phenylindole | 2.10 |
| 45 | 14.398 | 1H-Indole-2-carboxylic acid, 6-(4- ethoxyphenyl)-3-methyl-4-oxo-4,5,6,7-tetrahydro-, isopropyl ester | 4.10 |
| 46 | 14.539 | Scopoletin | 3.66 |
| 47 | 14.680 | Bicyclo[3.3.1]nonan-2-one,1-methyl-9-(1-methylethylidene)- | 2.45 |
| 48 | 14.933 | 2,4,6-Trimethylphenyl isothiocyanate | 1.79 |
| 49 | 15.074 | Deoxyqinghaosu | 8.46 |
| 50 | 15.271 | N-(2-Acetylcyclopentylidene)cyclohexylamine | 4.18 |
| 51 | 15.412 | Fluorenoneoxime | 2.58 |
| 52 | 15.750 | 6-Methoxy-2-hydroxyquinoxaline-4-oxide | 2.80 |
| 53 | 15.947 | Benzo[h]quinoline, 2,4-dimethyl- | 1.51 |
| 54 | 16.088 | Tris(tert-butyldimethylsilyloxy)arsane Propiophenone, 2’-(trimethylsiloxy)- | 1.87 |
| 55 | 16.257 | 9,10-Anthraquinone monohydrazone | 3.83 |
| 56 | 16.426 | 1,2-Benzisothiazol-3-amine tms | 2.02 |
| 57 | 17.215 | Benzene, 2-[(tert-butyldimethylsil yl)oxy]-1-isopropyl-4-methyl- | 8.83 |
| 58 | 17.863 | 1,2-Bis(trimethylsilyl)benzene | 2.10 |
| 59 | 18.229 | Tetrasiloxane, decamethyl- 1,4-Bis(trimethylsilyl)benzene | 1.49 |
| 60 | 18.595 | 2,3-Diphenylcyclopropyl)methylphenylsulfoxide, trans- | 3.59 |
| 61 | 18.764 | Trimethyl[4-(2-methyl-4-oxo-2-pent yl)phenoxy]silane | 0.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olorunnisola, O.S.; Adegbola, P.I.; Ajilore, B.S.; Akintola, O.A.; Fadahunsi, O.S. The Role of Poly-Herbal Extract in Sodium Chloride-Induced Oxidative Stress and Hyperlipidemia in Male Wistar Rats. Medicines 2021, 8, 25. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8060025
Olorunnisola OS, Adegbola PI, Ajilore BS, Akintola OA, Fadahunsi OS. The Role of Poly-Herbal Extract in Sodium Chloride-Induced Oxidative Stress and Hyperlipidemia in Male Wistar Rats. Medicines. 2021; 8(6):25. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8060025
Chicago/Turabian StyleOlorunnisola, Olubukola Sinbad, Peter Ifeoluwa Adegbola, Bamidele Stephen Ajilore, Olayemi Adebola Akintola, and Olumide Samuel Fadahunsi. 2021. "The Role of Poly-Herbal Extract in Sodium Chloride-Induced Oxidative Stress and Hyperlipidemia in Male Wistar Rats" Medicines 8, no. 6: 25. https://0-doi-org.brum.beds.ac.uk/10.3390/medicines8060025






