1. Introduction
Health and safety (H&S) in industries has now become important in most countries. However, the focus is generally on the safety component, i.e., avoiding accidents [
1], rather than long-term health [
2]. Existing methodologies for improving safety are primarily based on the risk methodologies [
3], normally by reducing the consequence of harm and likelihood of the occurrence. This is widely applied in risk management and related areas [
4]. There has been relatively less attention to long-term occupational health, other than via health monitoring and surveillance. The difficulty is the multiple overlapping health consequences that are difficult to separate, measure, and attribute to a source. Furthermore, many health problems are chronic; they may take a period to occur due to cumulative exposure, hence increasing the detection difficulty [
5]. Consequently, it is often difficult to conclusively identify the cause of health issues, and too late to change the work practices for that worker. At the time of exposure, workers may lack knowledge of long-term consequences, and thus not use protective systems effectively. Hence, there is a need for instruments and methodologies to measure the risk of harm, especially in the long-term H&S risk in the workplace, before it occurs. Examples of existing methods are the International Organization for Standardization (ISO) 31000 risk management standard [
6] with its many derivatives, and a variety of checklists and scoring methods (reviewed below). This paper explores a new way of looking at the subject, and proposes the concept of
Diminished Quality of Life (DQL) as a measure of occupational health. An instrument is developed to embody this concept. This may then be used to manage the minimization of harm, exposure monitoring, and the design of safe systems of work. The specific area under examination is the manufacturing industry, and the instrument was developed with this audience in mind. This was selected as representative of a variety of health risks, and employs many people.
4. Results
4.1. The Conceptual Model
The dominant paradigm for risk assessment is per the ISO 31000 process that partitions risk into consequence and the likelihood of that consequence. If we are to find better ways of incorporating the long-term health component into the assessment, then it will be necessary to re-conceptualise harm. Consequently, we developed a new conceptual framework, by starting with the biological consequences and working backwards to connect those causally to the hazards that might cause them, and how to represent them.
The hazards were classified by following a review of existing research. The objective was to address hazards for both health and safety, and with a special focus on the hazards that may result in long-term effects. Health and safety incident descriptions were identified for each hazard along with the corresponding biological consequences. The three steps in designing this conceptual model are shown in
Figure 1.
The literature review showed that each hazard has potentially multiple effects on a person’s health. For example, chemical exposure can have negative effects on a person’s body not only due to long-term exposure, but also by short term exposure, such as accidental contact. Chemical exposure can cause potential harm to a person’s health by cumulative exposure, for example, skin disease, respiratory system harm, and high or low blood pressure. It also can cause harm to the body by accidental contact, and, consequently, result in damage, such as acid burn.
Health needs to be treated differently to safety. This is because of their unique characteristics. Safety problems are related to accidents, and they can affect a person’s body immediately. By contrast, health problems are more likely to occur after a period of time, or by cumulative exposure with an associated accumulation/incubation period. Furthermore, compared to safety, some health problems can be hard to cure, or cannot be cured, and thus result in chronic issues. Therefore, we propose to classify hazards as either health or safety.
4.2. Health and Safety Hazards List
Based on the existing literature, manufacturing industry hazards are of two types:
Environmental hazards and
machinery hazards. A list of such health and safety hazards was aggregated from multiple sources, e.g., Health and Safety Executive (HSE), UK [
70], WorkSafe NZ [
71], and Occupational Safety and Health Administration US (OSHA), US [
68].
The environmental hazards in the manufacturing industry are grouped as chemical exposure, dust environment, light, noise, trips and falls, and temperature.
Chemical Exposure: Chemical exposure can result in an accident or a long-term health problem. Chemicals can come in contact with the skin and eyes, resulting in skin damage [
72] and eye injury [
73]. Chemicals can also cause respiratory system problems [
74]. Exposure to chemicals can be fatal [
75].
Dust: Machining operations can cause dust at work, such as cutting carbon and wood. This may result in breathing difficulties and lung disease [
76,
77], especially when inhaled for a long time [
78].
Light: Activities, such as cutting and welding, can have light issues associated with them. The consequence can be eye strain and short sightedness [
79]. The light in welding activities can be very strong, and lack of eye protection can result in blindness.
Noise: Noise is a general hazard in the manufacturing industry due to the nature of manufacturing operations [
80,
81]. The consequence of long term expose to relatively high noise levels can result in hearing loss [
20].
Slips, trips, and falls: Slips can be caused by inadequate cleaning, e.g., uncleaned and undried water on surfaces [
31]. Trips can be caused by unsecured equipment, e.g., cables [
82]. Falls from a height can be caused by loss of function of PPE, e.g., improper footwear [
83,
84]. The biological consequence of slips, trips, and falls can be bruises, abrasions, sprains, fracture, and even death [
85].
Temperature: Temperature can be uncomfortable in the manufacturing industry, as some products are created by using high or low temperature, e.g., tyres. High temperatures in the work environment can cause circulatory system diseases, e.g., blood pressure problems. Low temperatures can result in muscle fatigue [
86].
Machinery hazards in the manufacturing industry include cutting, crushing and squashing, electrical damage, heat and radiation, impact damage, wearing loose cloth, manual heavy loads, doing repetitive work, ventilation, vibration at work, and working in an uncomfortable position.
Cutting, crushing, and squashing: Manufacturing industry activities can result in cutting and squashing, for example, by operating machines (e.g., a lathe) and using hand tools (e.g., a hammer). The consequence of the associated hazards can be abrasion, small cuts, fracture, amputation [
87], and even death [
84].
Electrical damage: Electricity can result in serious harm to a worker in the manufacturing industry [
29,
88]. An electrical burn can cause skin damage [
89], and a serious electrical shock can cause paralysis and even death [
90].
Entrapment: Loose clothes and working with machines can result in machines jamming or clothing touching hot surfaces (resulting in burns), and slips and falls [
85]. This may then result in squashing, amputation, burns, and fractures.
Heat and radiation: Heat and radiation can result in burns due to fire, hot objects, and hot liquid [
30]. This can be fatal [
91,
92].
Infection: Infection is caused by bacteria and viruses [
93]. In factories, infection can be caused through multiple ways, for example, a wound caused by impact damage, or a cut caused by sharp edges. In meat and seafood process factories, infections may be also caused by zoonosis [
94].
Impact: Impact damage to a worker can be caused by machines and moving vehicles, such as forklifts [
95]. The biological outcome can be bruises, abrasions, sprains, fracture, paralysis, and even death.
Manual heavy loads: Manual heavy loads in the manufacturing industry can be caused by moving heavy products, and operating machines. A person who suddenly moves a heavy object can get muscle injury, resulting, for example, in back pain [
85]. Heavy manual work can result in musculoskeletal damage, such as tendinitis and fibromyalgia.
Repetitive work: Manufacturing work can be characterised by repetitive activities, such as packaging. Long term exposure to this hazard can result musculoskeletal damage [
12].
Ventilation: Fresh air provides a healthy working environment for workers, and this can be contributed by ventilation [
96]. Poor ventilation may result from lack of oxygen, and this can lead to dizziness; it may also lead to an uncomfortable temperature [
97,
98]. It may contribute to a lack of attention, and hence exposure to other hazards. Welding in confined spaces can be particularly dangerous.
Vibration: Vibration can be caused by machinery and equipment at work, e.g., drilling equipment [
99]. The biological outcome of this hazard can be musculoskeletal damage [
11].
Uncomfortable working position: Work in an uncomfortable and awkward position may happen when the height of the work surface is not appropriate for someone [
12]. It can happen when workers are asked to hold an object at an overhead height [
100]. This is an ergonomic issue and may result in muscle strain and musculoskeletal damage [
101].
A hazards list was created, combining both environmental hazards and machinery hazards. The various hazards were sorted alphabetically, and are shown in
Figure 2. This hazard list is considered to be comprehensive, but can be customised.
4.3. Biological Consequences
Health related biological outcomes in the manufacturing industry were identified based on the international classification of disease in occupational health (ICD) [
69] and the international classification of functioning, disability, and health (ICF). These are infectious diseases [
69], malignant diseases [
102], blood disease [
103,
104], mental and behavioral disorders [
105,
106], nervous system disease [
107], eye disease [
108,
109], ear disease [
110,
111], circulatory system disease [
112], respiratory system disease [
9], and musculoskeletal system disease [
12]. The incubation period can be very long, or may occur by cumulative exposure, hence they can be difficult to detect [
113]. Additionally, because of individual physique, the consequence of harm may be different. The consequences of health harm can be influenced by a number of factors, such as gender [
114] and age [
34,
115].
In contrast with health, safety accidents usually cause immediate personal harm to the human body. Transportation equipment, such as conveyors, forklifts, and trucks, may also result in impact damage to workers [
27]. The biological outcome of machinery accidents may result in amputation [
116], laceration [
117], fracture [
118], and even death [
119]. Other possible harms are cuts and bruises [
26]. Some other harms are caused by environmental accidents, such as trips and falls, chemicals [
120], and electrical discharges [
121]. Some of the environment accidents, like fire, can cause significant damage, even death [
122].
Once all potential biological consequences in the manufacturing industry were identified, a health consequences list was generated based on the literature, and this is presented in
Figure 3. We propose the consequence is different for different body parts. Hence, for example, amputation was divided into five categories: Arms, fingers, foots, hands, and legs. The various consequences list is presented by level. The application of the framework is limited to the second level. This is because further work is necessary to establish the lower level consequences with confidence.
4.4. Linking the Hazards to the Biological Consequences
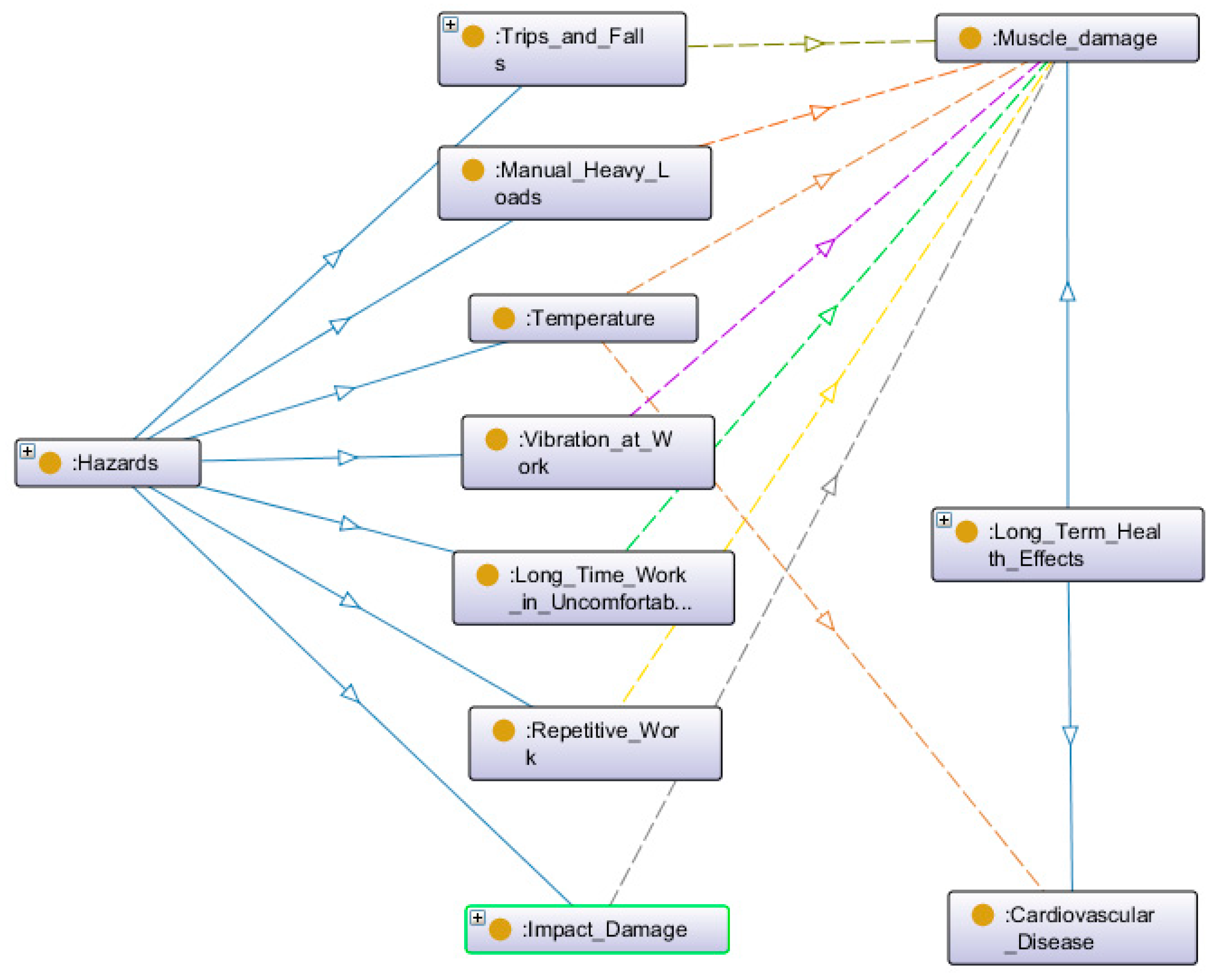
The relationships between hazards and biological consequence were then identified. The relationships are complex. A hazard can result in multiple consequences; a consequence can also be caused by different hazards. Therefore, an information methodology was adopted using an ontology. An ontology describes the relationship and hierarchy between each hazard and the corresponding biological consequence. Additionally, the ontology also focuses on processing and grouping similar consequences into categories. We applied Protégé software to map the lists of hazards and biological consequences. The relationship was then expressed by using mapping analysis. See
Figure 4 for an example of the relationship between safety hazards and muscle damage, and cardiovascular disease.
The benefit of using the ontology is that it imposes a systematic process for ensuring the coherence of the model. We found this helped ensure that biological consequences were less likely to be overlooked.
In practice, the way the ontology is expected to work is that the hazards would be identified in the workplace (e.g., ‘chemical exposure’), and the ontology would then automatically identify the associated biological consequences (e.g., skin disease, respiratory system problem, blood pressure problem, eye injury, skin damage). An occupational hygienist would identify the frequency of these consequences arising in the situation. Possibly, the ontology could also support decision-making at this latter step by providing default estimates. In the present work, the ontology is not fully automated in the software, instead the process requires manual input of data via a spreadsheet. Nonetheless, we believe that the overall architecture shown here should be feasible to deploy in the software.
Based on the result of the relationship map, we then developed a register to express the casualty of hazards and biological consequences, see
Figure 5 (H: Health; S: Safety.). The casualty was developed based on the existing literature.
4.5. Adoption of a Quality of Life Scale
Level of harm is a key factor in illustrating the negative effects to the human body. However, it is very hard for people to measure the level of harm. The first reason is that some health problems are chronic and this then results in uncertain consequences. Secondly, some health problems may have a long incubation period or affect the human body slowly, hence attribution to a specific time or event may be difficult. Hence, this may then result in uncertain consequences, weak protections, and late treatments. Thirdly, the level of harm is also dependent on a person’s physical ability. Therefore, we propose to use the Quality of Life (QOL) methodology to address the level of harm.
QOL was defined by the World Health Organisation (WHO) in 1948 as “
a state of complete physical, mental, and social well-being, and not merely the absence of disease” [
123]. There are many QOL measuring instruments developed by different researchers, e.g., the Karnofsky Performance Scale, Sickness Impact Profile, and linear analogue self-assessment (LASA) methods [
123]. However, these are focused on medical aspects, and QOL in the manufacturing industry are weakly applied and developed. The WHO also have a quality of life score, the WHO Disability Assessment Schedule (WHODAS 2.0) [
63]. We assessed this as more relevant to the situation of industrial harm. There are three different instruments developed by WHODAS, and we decided to use WHODAS 12-item instrument [
63]. This is more focused on physical effects than the other two instruments. It was developed to identify how much difficulty a person has in completing the tasks of daily living. The WHODAS questions are shown in
Appendix B. Each WHODAS 12-item has a 0 to 4 scale, see
Figure 6. The results are percentages, and are used to express the level of physical ability. A higher score indicates higher disability.
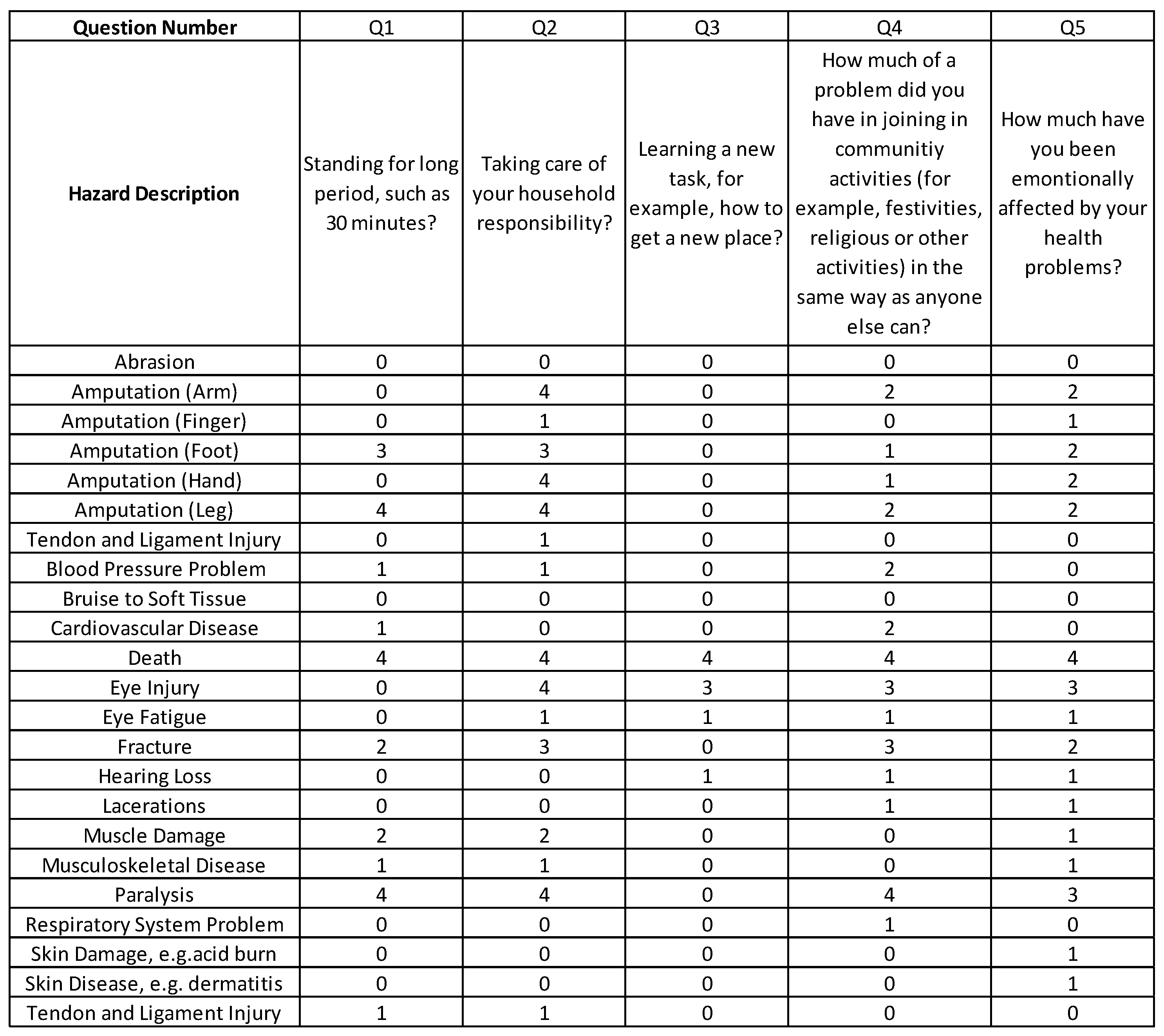
4.6. WHODAS Scores for Manufacturing
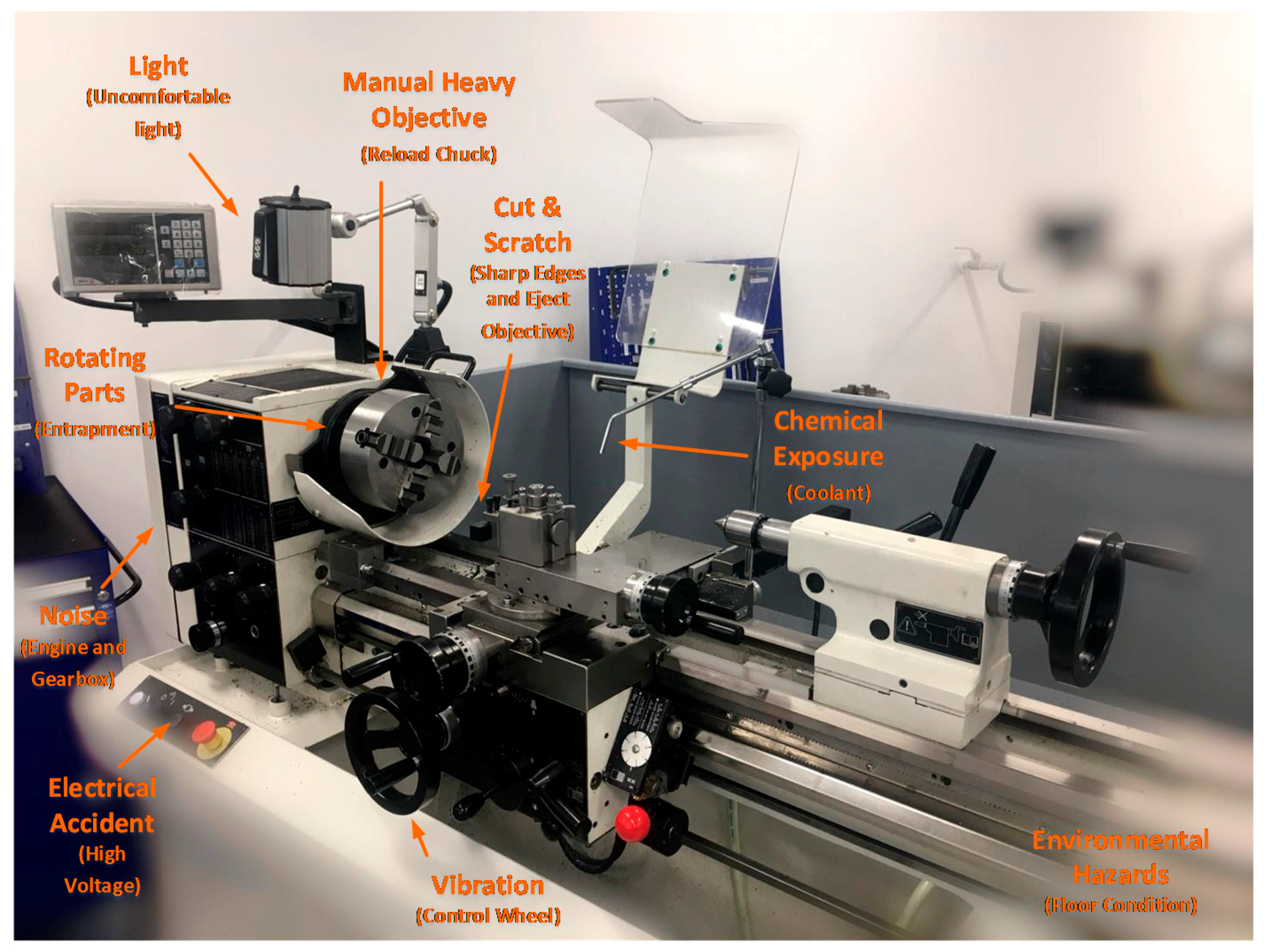
We then applied the WHODAS to a lathe work process, as representative of a common manufacturing industry activity. Potential hazards in operating a lathe were identified, see
Figure 7.
In this type of work, workers are exposed to both environmental hazards and machinery hazards. A typical environmental hazard here is hearing loss. Some other typical machinery hazards are cuts by the machine and contact with chemical products (e.g., coolant). The biological consequence for a cut may result in laceration and in extreme cases amputation; and the chemical exposure may potentially result in skin disease. We classified all potential hazards and their biological outcomes, and for each, we determined the WHODAS score. Representative data were used to demonstrate the principle. In this way, we determined the diminished long-term quality of life due to the exposure to say coolant. The WHODAS results for the lathe work are shown in
Figure 8, (see also
Appendix B).
4.7. Likelihood of an Incident Arising
Probability and frequency can be used to express the likelihood of an incident. Sherman Kent in 1964 presented the idea of Words to Estimate Probability (WEP) [
124]. This is widely used in likelihood descriptions. Some popular WEP words are ‘certain’, ‘possible’, and ‘impossible’. This has been applied to risk research, and the likelihood scales were developed using qualitative words [
60]. Sherman Kent also proposed that there are differences between “poets” (people preferring to use wordy descriptions in probability) and “mathematicians” (people preferring to use quantitative methods) [
125].
We propose to use a quantitative number to express the probability and frequency, instead of qualitative words. This is because we intend to get a numerical result in health and safety risk. A likelihood diagram was developed by the Central Intelligence Agency (CIA) in 2007 [
126], see
Figure 9. We adapted this, as further described below.
We developed and adopted a scale for the estimated frequency and likelihood by modifying the CIA scale in discussion with engineering technicians. The results are shown in
Figure 10.
4.8. Proposed Instrument for Diminished Quality of Life (DQL)
We now present a new concept that integrates all the above. We propose that health effects of industrial activities be measured as ‘diminished quality of life’ (DQL). DQL refers to the extent to which a hazard has a biological consequence that adversely affects a person’s quality of life much later in life. The DQL measurement is quantitative, ranging from 0 to 100. 0 refers to no negative effects on a person’s life, and 100 refers to a very bad outcome, like death.
DQL can be calculated in a four-step process. First is identifying the likelihood of incidents, see Section 4.5.1. Second is identifying the likelihood of a biological consequence. Third is identifying the level of harm: This is done through WHODAS, see Section 4.3.2. Finally, DQL can be calculated using Equation (1):
;
;
;
;
; and
.
We propose that DQL can be used for both long term health effects and short term safety accidents. It can potentially also be used in H&S management across other industries, such as construction. However, this paper is focused on DQL in the manufacturing industry. The DQL result of lathe operating has been addressed in
Appendix A.
4.9. Evaluation of Severity of Consequences for Quality of Life
After collecting the result of DQL, a method is proposed for workers to determine the overall outcome in health and safety. There is a need to determine thresholds for action, i.e., DQL scores that warrant treatment of the hazard. This is a difficult problem because the long-term biological consequences are poorly understood. Nonetheless, there is a need to develop guidelines for practitioners, so that they can target their finite resources towards appropriate interventions.
To determine the thresholds for action, we analysed the DQL result of lathe operating as representative of a typical material removing (cutting) process in manufacturing. It was noted that 51% of results were between 0-1. We inferred this as an acceptable score, on the basis that the lathe technology is widely used, and this level of residual risk appears to be accepted by industry: there appears to be an acceptance or assumption of risk at this level. We propose that items scoring 1 or lower are low level and may be inconsequential. They are indistinguishable from background risk factors in society generally. This category includes, for the lathe case, e.g., ‘Blood Pressure Problem’, and ‘Respiratory System Problem’. (In different situations, these may be more important.)
It was noted that 29% of DQL results were between 1-3 for the lathe. We propose that a DQL result between 1-3 is a moderate level. This applies in the lathe case where the current safety preventions are considered good. Some of the ‘Musculoskeletal Injury’ risks appear to be in this category for lathe work.
A further 20% of results were between 3-8. We propose a DQL result between 3-8 be considered a high level, and more attention should be given to implementation of treatments. For the lathe work, these were identified as hearing loss and eye injury.
Additionally, the DQL result can, in principle, be over 8, though no such levels were evident for the lathe process. Hence, we propose that a DQL result over 8 is at the extreme high level, and has an unacceptable risk, requiring urgent treatment.
It is acknowledged that these thresholds are subjective. The above strategy is summarized in
Figure 11, along with the recommended preventative mechanisms.
There are several advantages in adopting a DQL instrument. Firstly, through analysing the result of DQL, workers can get a better understanding of safety hazards and biological consequences, especially of the long-term health effects. Workers can also identify the DQL level and determine reasonable preventative mechanisms. This results in better recognition of health and safety at work, hence improving prevention and recovery treatments.
4.10. Health and Safety Measuring Instrument- DQL Instrument
The practical implementation of the DQL instrument may be achieved in a spreadsheet or table, see
Figure 12. The instrument consists of eight columns (A to H). Column A describes hazards in the workplace. Columns B is a description of the severity context and the current state. Column C is designed for a specific description of each hazard and relates to how someone could be harmed. Column D is for estimated frequency at work. Column E illustrates the corresponding biological consequence. Column F is the likelihood of the consequence. Column G is the corresponding WHODAS score. Column H is for calculating the DQL result, which is the product of columns D, F, and G.
This instrument is designed to be completed by engineering technologists, H&S officers, and occupational hygienists. Column B and Column D are designed for an engineering technologist to fill in. We assume that engineering technologists have a clear understanding of hazard identification and the frequency thereof. Column F is designed for H&S officers or occupational hygienists to fill in, as they are expected to have a good knowledge of occupational health and safety and also have the ability to present a reasonable likelihood based on analysing the incident reports.
For the full edition of the instrument with an application in lathe work, see
Appendix A. An extract is shown in
Figure 12. According to results of the application in lathe work, 51% of results were between 0-1 (Low Level), 29% of results were between 1-3 (Moderate Level), 20% of results were between 3-7 (High Level), and 0% of the results were over 8 (Extreme High level). We then found that the high level DQL results were associated with amputation, laceration, eye injury, hearing loss, and death. Clearly, these need to have preventative treatments applied, hence it would be recommended for inclusion in a safe-work plan. Note that some of these outcomes (such as hearing loss) are in the long-term harm category, while others (such as amputation) are in the immediate accident category.
5. Discussion
5.1. Summary
5.1.1. Health Consequences
In summary, the DQL measuring instrument presents a new way to manage health and safety in manufacturing industries, especially the health component. This is achieved by adapting the established WHODAS quality of life score to workplace health. Specifically, the method is to identify the likelihood of an exposure incident arising (as estimated by engineering technologists and H&S officers), followed by evaluation of the biological harm consequences. Those consequences are then scored by using the WHODAS 12-item inventory. The result is an assessment of the Diminished Quality of Life associated with a workplace hazard. This may then be used to manage the minimization of harm, exposure monitoring, and the design of safe systems of work.
In doing this, our premise is that the ‘health’ component of H&S does not always have immediate consequences, but rather effects occur at some indeterminate point in the future. Once the harm does occur, it can often be too late for full cure. We propose that for these hazards, the lack of any immediate harm and the indeterminateness of the consequences contributes to a worker inadvertently assuming a degree of personal risk. Hence, self-prevention is undermined by the worker’s perverse agency [
57].
5.1.2. Comparison between Risk Management and DQL Methods
We propose that the existing risk management methodology [
6], with its focus on consequence and likelihood, is adequate for safety accidents that have an immediate and tangible consequence, but less so for the long-term harm hazards. The conventional risk assessment process per ISO 31000 encapsulates the concept that the assessment first identifies the consequences, and then the likelihood of those consequences, and then combines them with a product relationship. It is the indeterminate nature of both the consequences and likelihood that limits the risk assessment method in these cases. The product of two uncertain variables further increases the uncertainty in the outcome. We propose that it is intrinsically difficult for industrial risk assessors to make these evaluations reliably. It is difficult for people to anticipate the consequences of the present exposure on their health at some remote point in the future.
Hence, we make the somewhat radical proposal that the risk management methodology is intrinsically unsuited for the harm category of hazards. Instead, we propose that it could be more useful to get people to think about how the hazard might decrease their future quality of life. In doing so, we have borrowed and adapted a validated quality of life instrument used in medicine and rehabilitation. In the DQL methodology, the outcome is measured as a diminished quality of life and is the product of the frequency of exposure, the likelihood of long and short term biological consequences arising, and the WHODAS score for those consequences. While these frequencies and likelihoods are also subjective, the use of the WHODAS provides a measure of consistency, and frames the cognition process in the hazard assessment to be future-focused.
We propose that the two methods are complementary—they achieve different things. In both cases, the results of applying the methodologies are numerical outcomes, which can usefully contribute to health and safety management. The conventional risk management methodology may be ideal for risks that can be reliably quantified, e.g., financial, insurance, technical systems. It is also a simple and useful, even if imprecise, method for assessing accident risk when using simple scales for the two axes. We propose that risk assessment is an important first analysis tool: It causes people to be mindful of the hazards in a situation, and encourages the deployment of preventative treatments. It also provides a means to do due diligence to legal requirements, such as [
42]. We suggest that methods based on quality of life, such as the DQL developed here, should be applied as a second stage of evaluation, as part of the continuous improvement process.
5.2. Original Contributions
This work makes several novel contributions. Firstly, it offers a systematic categorisation of health and safety hazards, and specifically addresses long-term health effects, including biological outcomes and their cause. This could potentially help workers better understand occupational health, and help managers provide safer work places.
Secondly, a conceptual framework has been developed around diminished quality of life to present health in a different way to the conventional risk management methodology. This has the potential to enrich the safety field, since health risks are otherwise difficult to analyse and manage. Thirdly, a methodology has been developed to provide a means to quantify DQL in an industrial setting. The DQL instrument not only addresses the accidental harm (environmental and physical) in the manufacturing industry, but also has a special focus on long-term health effects. The biological outcome and its cause are also addressed. The method relies on estimates that are feasible to obtain in the industry, hence it is not difficult to apply.
5.3. Implications for Practitioners
Health issues are under-represented in the safety literature compared to accidents, hence there is a need to develop an instrument to manage both health and safety. It is much easier for industry people to manage safety because an accident tends to have immediate consequences. By contrast, health problems are difficult to identify in the workplace, and some of the health problems require a period to occur or cumulative exposure. The DQL instrument presented here is focused on hazards and their biological consequences in the manufacturing industry. For its implementation, the methodology requires input from a number of industry professionals, such as an engineering technologist, H&S, and occupational hygienist/therapist. In principle, the methodology is applicable to other areas, such as construction, chemical and process engineering, agriculture, etc.
5.4. Limitations of the Work
The work has a number of limitations. One of these is the need for frequency and likelihood data, which is subjective. This is, similar to the subjective estimates needed for consequence and likelihood in the conventional risk assessment method. A second limitation is that we have used representative data to evaluate WHODAS scores. It could be interesting to see the variability between workers (and possibly across different cultures) to the WHODAS scores. A third limitation is that loops of causality have not been included in the work. Some factors (such as lighting and noise) cause fatigue, which may reduce concentration and increase the risk of accidents. A fourth limitation is that determination of an unacceptable threshold for the DQL score was set at >1, but this was our subjective evaluation. It is difficult to see how this score might be objectively determined.
The work was developed with industrial workers in mind, specifically manufacturing engineering. How well the method might apply to other areas has not been determined. Since the WHODAS is a not a sector-specific measure, it is possible that the DQL may be applicable more widely, but this would need to be verified.
5.5. Implications for Further Research
WHODAS scores for different stakeholders could be identified. This could involve developing a survey wherein respondents record the impact on their quality of life for each of the biological consequences identified. It may be necessary to simplify the list of biological consequences to avoid survey fatigue. It would be interesting to see if different groups, e.g., categorized by experience, appraised the consequences differently. A statistical approach may be useful here. A possible concurrent project could be to use qualitative research methods to determine why people made the responses they did. This might involve semi-structured interviews or semantic analysis. The DQL method could also be applied to other industries, such as construction.
Additionally, methodologies for control consequences at work need to be improved, especially in health aspects. Some potential barriers could be, for example, sound isolation (noise), ergonomics work station (manual work activity), and good quality PPE (chemical exposure). Hence, a potential research on efficient treatments for controlling health consequences at work may be valuable. However, some health consequences arise not only from the workplace, but rather individuals’ lifestyle choices (exercise, diet) and existing health conditions that occur outside of their workplace. Mental health needs to be considered as part of risk assessment too. Thus, we suggest there may be other potentially fruitful research to be undertaken on developing methods to provide a more holistic assessment of worker well-being.