Chronic Antibody-Mediated Liver Rejection: More than Meets the Eye
Abstract
:1. Introduction
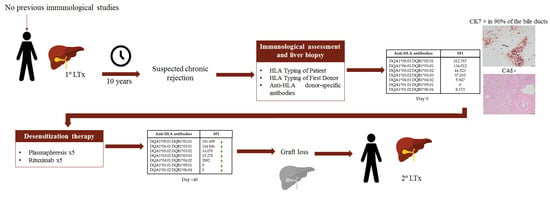
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board
Informed Consent
Data Availability Statement
Conflicts of Interest
References
- Wesson, R.N.; Etchill, E.W.; Garonzik-wang, J. Application and interpretation of histocompatibility data in liver transplantation. Curr. Opin. Organ Transplant. 2017, 22, 499–504. [Google Scholar] [CrossRef]
- Demetris, A.J.; Bellamy, C.; Hübscher, S.G.; O’Leary, J.; Randhawa, P.S.; Feng, S.; Neil, D.; Colvin, R.B.; McCaughan, G.; Fung, J.J.; et al. 2016 comprehensive update of the Banff working group on liver allograft pathology: Introduction of antibody-mediated rejection. Am. J. Transplant. 2016, 16, 2816–2835. [Google Scholar] [CrossRef]
- Muro, M. The endless history or search for the true role of alloantibodies in liver transplantation. Clin. Res. Hepatol. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Vionnet, J.; Sempoux, C.; Pascual, M.; Sánchez-Fueyo, A.; Colmenero, J. Donor-specific antibodies in liver transplantation. Gastroenterol. Hepatol. 2020, 43, 34–45. [Google Scholar] [CrossRef]
- Tambur, A.R.; Campbell, P.; Chong, A.S.; Feng, S.; Ford, M.L.; Gebel, H.; Gill, R.G.; Kelsoe, G.; Kosmoliaptsis, V.; Mannon, R.B.; et al. Sensitization in transplantation: Assessment of risk (STAR) 2019 Working Group Meeting Report. Am. J. Transplant. 2020, 20, 2652–2668. [Google Scholar] [CrossRef]
- Taner, T.; Stegall, M.D.; Heimbach, J.K. Antibody-mediated rejection in liver transplantation: Current controversies and future directions. Liver Transplant. 2014, 20, 514–527. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Yang, Y. Late and chronic antibody-mediated rejection: Main barrier to long term graft survival. Clin. Dev. Immunol. 2013, 2013, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demetris, A.J.; Murase, N.; Nakamura, K.; Iwaki, Y.; Yagihashi, A.; Valdivia, L.; Todo, S.; Iwatsuki, S.; Takaya, S.; Fung, J.J. Immunopathology of antibodies as effectors of orthotopic liver allograft rejection. Semin. Liver Dis. 1992, 12, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Ronca, V.; Wootton, G.; Milani, C.; Cain, O. The Immunological Basis of Liver Allograft Rejection. Front. Immunol. 2020, 11, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Del Bello, A.; Congy-jolivet, N.; Danjoux, M.; Muscari, F.; Esposito, L.; Cardeau-desangles, I.; Lavayssie, L.; Milongo, D.; Suc, B.; Duffas, J.P.; et al. De novo donor-specific anti-HLA antibodies mediated rejection in liver-transplant patients. Transpl. Int. 2015, 28, 1371–1382. [Google Scholar] [CrossRef]
- Legaz, I.; Boix, F.; López, M.; Alfaro, R.; Galián, J.A.; Llorente, S.; Campillo, J.A.; Botella, C.; Ramírez, P.; Sánchez-Bueno, F.; et al. Influence of Preformed Antibodies in Liver Transplantation. J. Clin. Med. 2020, 9, 708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valenzuela, N.M.; McNamara, J.T.; Reed, E.F. Antibody-mediated graft injury: Complement-dependent and complement-independent mechanisms. Curr. Opin. Organ Transplant. 2014, 19, 33–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.; Himmelfarb, E.A.; Sun, M.; Choi, E.K.; Fan, L.; Lai, J.; Kim, C.J.; Xu, H.; Wang, H.L. Immunostaining Patterns of Posttransplant Liver Biopsies Using 2 Anti-C4d Antibodies. Appl. Immunohistochem. Mol. Morphol. 2020, 28, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Sakashita, H.; Haga, H.; Ashihara, E.; Wen, M.; Tsuji, H.; Miyagawa-hayashino, A.; Egawa, H.; Takada, Y.; Maekawa, T. Significance of C4d staining in ABO-identical / compatible liver transplantation. Mod. Pathol. 2007, 20, 676–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fayek, S.A. The value of C4d deposit in post liver transplant liver biopsies. Transpl. Immunol. 2020, 27, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Bellizzi, A.M.; LeGallo, R.D.; Boyd, J.C.; Iezzoni, J.C. Hepatocyte cytokeratin 7 expression in chronic allograft rejection. Am. J. Clin. Pathol. 2011, 135, 238–244. [Google Scholar] [CrossRef] [Green Version]
- Neil, D.A.H.; Hubscher, S.G. Histologic and Biochemical Changes During the Evolution of Chronic Rejection of Liver Allografts. Hepatology. 2002, 35, 639–651. [Google Scholar] [CrossRef]
- Salazar, E.; Cohen, D.; Ipe, T.; Leveque, C. Therapeutic Plasma Exchange for Potential Human Leukocyte Antigen Antibody-Mediated Rejection in Liver Transplant Patients. Am. J. Clin. Pathol. 2017, 147, S163. [Google Scholar] [CrossRef]
- Kamar, N.; Lavayssière, L.; Muscari, F.; Selves, J.; Guilbeau-Frugier, C.; Cardeau, I.; Esposito, L.; Cointault, O.; Nogier, M.B.; Peron, J.M.; et al. Early plasmapheresis and rituximab for acute humoral rejection after ABO-compatible liver transplantation. World J. Gastroenterol. 2009, 15, 3426–3430. [Google Scholar] [CrossRef]
- Oguz, E.G.; Yildirim, T.; Merhametsiz, O.; Haspulat, A.; Ercan, Z.; Gursoy, K.; Bulut, C.; Akoglu, H.; Akdag, I.; Canbakan, B.; et al. Plasmapheresis in Chronic Active Antibody Mediated Rejection. Transplantation 2014, 98, 677. [Google Scholar] [CrossRef]
- Vuille-Lessard, É.; Bilodeau, M.; Willems, B.; Marleau, D.; Vincent, C.; Giard, J.; Villeneuve, J.; Soucy, G.; Nguyen, B.; Huard, G. A67 Antibody-mediated rejection after liver transplantation: A case series. J. Can. Assoc. Gastroenterol. 2019, 2, 134–135. [Google Scholar] [CrossRef]
- Koch, M.; Marget, M.; Sterneck, M.; Fischer, L.; Thude, H.; Nashan, B. Limited impact of pre-existing donor specific HLA-antibodies (DSA) on long term allograft survival after first adult liver transplantation. Hum. Immunol. 2018, 79, 545–549. [Google Scholar] [CrossRef] [PubMed]
- McCaughan, J.A.; Robertson, V.; Falconer, S.J.; Cryer, C.; Turner, D.M.; Oniscu, G.C. Preformed donor-specific HLA antibodies are associated with increased risk of early mortality after liver transplantation. Clin. Transplant. 2016, 30, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Kaneku, H.; Leary, J.G.O.; Taniguchi, M.; Susskind, B.M. Donor-Specific Human Leukocyte Antigen Antibodies of the Immunoglobulin G3 Subclass Are Associated With Chronic Rejection and Graft Loss After Liver Transplantation. Liver Transpl. 2012, 18, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Muro, M.; Moya-Quiles, M.R.; Mrowiec, A. Humoral Response in Liver Allograft Transplantation: A Review of the Role of Anti-Human Leukocyte Antigen (HLA) Antibodies. Curr. Protein Pept. Sci. 2016, 17, 776–784. [Google Scholar] [CrossRef]



| HLA Typing of Patient | A*01:01 A*30:02 B*49:01 B*50:02 C*06:02 C*07:01 DRB1*07:01 DRB1*08:01 DQA*02:01 DQA1*04:02 DQB1*02:01 DQB1*04:02 |
| HLA Typing of First Donor | A*30:02 A*26:01 B*18:01 B*38:01 C*05:01 C*12:03 DRB1*03:01 DRB1*14:01 DQB1*02:01 DQB1*05:03 (DQA1*01:01 DQA1*05:01) ∫ |
| HLA Typing of Second Donor | A*02:01 A*30:01 B*08:01 B*51:01 C*07:01 C*02:02 C*07:01 DRB1*03:01 DQB1*02:01 (DQA1*05:01) ∫ |
| Biochemical Parameters of Liver Function | Mean (Min–Max) |
|---|---|
| Aspartate transaminase (AST) | 146.9 U/L (76–261) |
| Alanine transaminase (ALT) | 87.6 U/L (59–114) |
| Bilirubin | 15.7 mg/dL (6.6–24.9) |
| Alkaline phosphatase (ALP) | 259 U/L (138–352) |
| Gamma-glutamyltransferase (GGT) | 62.1 (33–90) |
| SFI Units | MFI Units | Donor Antigens | CDC XM | FC XM |
|---|---|---|---|---|
| >100.000 | 4 | Forbidden | Probably positive | Positive |
| 100.000–40.000 | 4.000–1.500 | Risk | Probably negative | Probably positive |
| 40.000–20.000 | 1.500–800 | Undetermined | Negative | Probably negative |
| <20.000 | <800 | No Risk | Negative | Negative |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rita, C.G.; Iturrieta-Zuazo, I.; Ballester-González, R.; Alonso-Alarcón, N.; Moreno-Moreno, E.; Castañer-Alabau, J.L.; Nieto-Gañán, I. Chronic Antibody-Mediated Liver Rejection: More than Meets the Eye. Transplantology 2021, 2, 1-7. https://0-doi-org.brum.beds.ac.uk/10.3390/transplantology2010001
Rita CG, Iturrieta-Zuazo I, Ballester-González R, Alonso-Alarcón N, Moreno-Moreno E, Castañer-Alabau JL, Nieto-Gañán I. Chronic Antibody-Mediated Liver Rejection: More than Meets the Eye. Transplantology. 2021; 2(1):1-7. https://0-doi-org.brum.beds.ac.uk/10.3390/transplantology2010001
Chicago/Turabian StyleRita, Claudia Geraldine, Ignacio Iturrieta-Zuazo, Rubén Ballester-González, Nieves Alonso-Alarcón, Esther Moreno-Moreno, José Luis Castañer-Alabau, and Israel Nieto-Gañán. 2021. "Chronic Antibody-Mediated Liver Rejection: More than Meets the Eye" Transplantology 2, no. 1: 1-7. https://0-doi-org.brum.beds.ac.uk/10.3390/transplantology2010001