Neuroendocrine Tumors: Treatment and Management
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Therapy".
Viewed by 52070Editor
2. University Hospitals of Strasbourg Faculty of Medicine - University of Strasbourg Strasbourg, France
3. Molecular Imaging – DRHIM IPHC, UMR7178, CNRS/Unistra Strasbourg, France
Interests: Nuclear medicine, PET, Neuroendocrine tumors, Oncology, Infectious Diseases
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
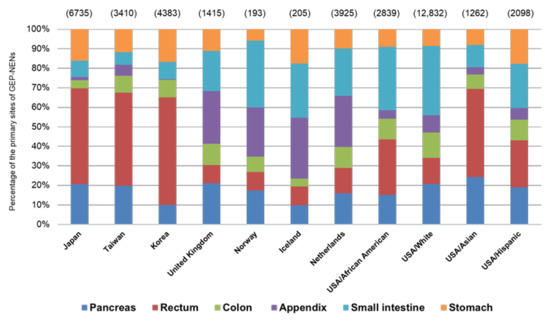
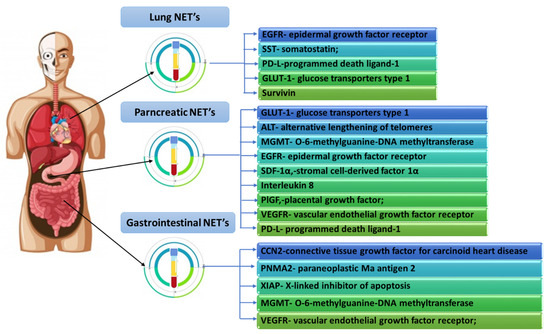
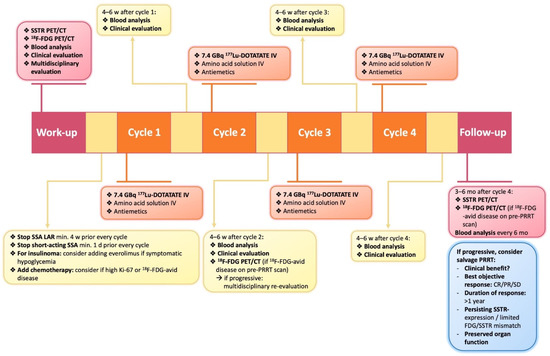
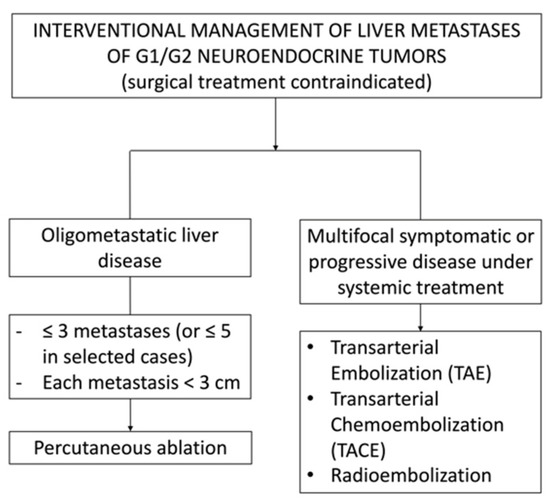
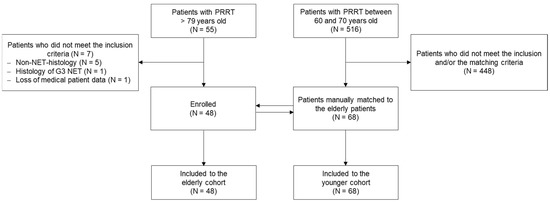
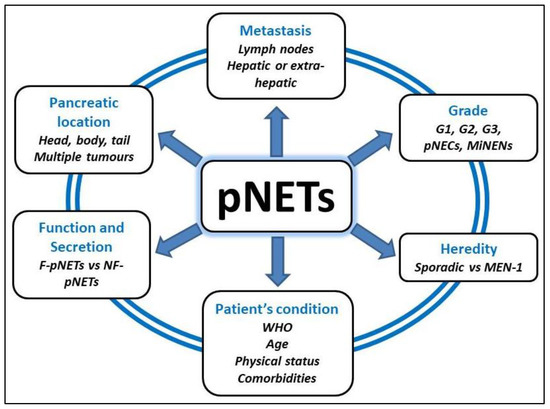
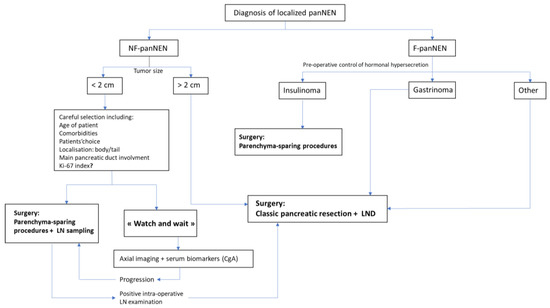
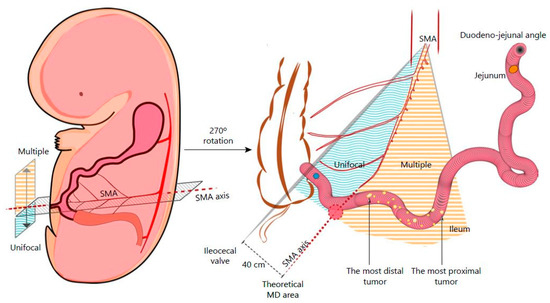
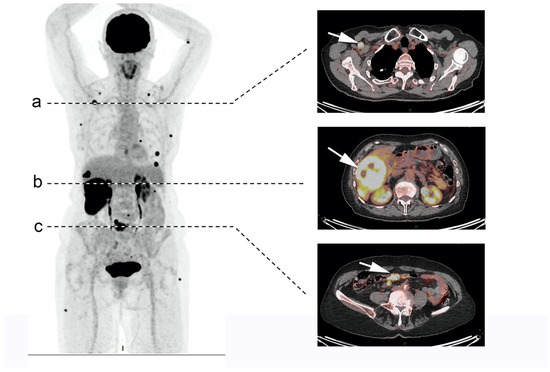
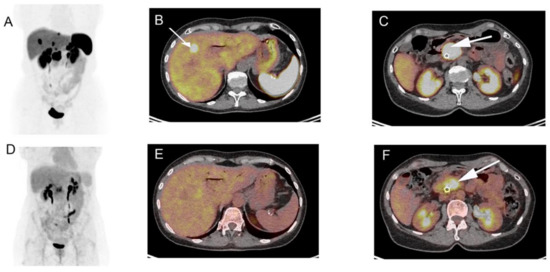
Neuroendocrine tumors (NET) are rare and heterogeneous epithelial neoplasms with neuroendocrine differentiation commonly originating from the gastrointestinal tract, pancreas, and lung. Patients with suspected or known NET are usually referred to a multidisciplinary skilled team for diagnostic evaluation, treatment, and follow-up. Whenever feasible, surgery is proposed for low-grade tumors. Multiple therapeutic options are available for unresectable advanced disease or metastatic disease, including medical treatment with cold somatostatin analogs, peptide receptor radionuclide therapy (PRRT), chemotherapy, and molecule-targeted therapies such as mammalian target of rapamycin (mTOR) inhibitors and antiangiogenic agents. Moreover, recent advances in understanding the genetic and epigenetic alterations in NET as well as the knowledge of proteomics and metabolomics tumoral features could make available novel targets for future therapeutic options and for the assessment of patient prognosis. In this Special Issue, a panel of internationally recognized experts in this field will focus on the current diagnostic approach, the several available therapeutic approaches, and the future directions for the management of patients with lung and gastroenteropancreatic NET.
Prof. Alessio Imperiale
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Neuroendocrine tumor
- pancreas, small bowel
- lung
- positron emission tomography
- surgery
- targeted therapy
- PRRT