New Insights into Prostate Cancer Diagnosis and Treatment
A topical collection in Current Oncology (ISSN 1718-7729). This collection belongs to the section "Genitourinary Oncology".
Viewed by 44157Editor
Topical Collection Information
Dear Colleagues,
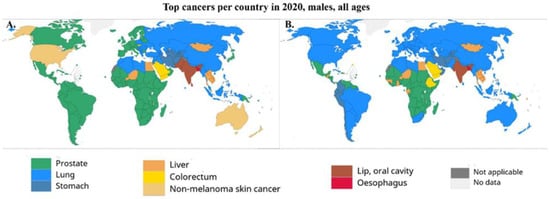
Prostate cancer (PCa) is the second most common cancer and the third leading cause of oncology-related death in men in the high-income countries. Curative therapy for PCa is surgical radical prostatectomy and/or local radiation therapy; however, approximately 5% to 20% of men will continue to have detectable or persistent levels of the tumor marker prostate-specific antigen (PSA) after primary treatment, and 27% to 53% will develop a PSA increase 5 years later in terms of biochemical recurrence.
Depending on tumor stage, the 5-year survival rate for these patients varies from 100% in early tumor stage to only 30% in patients with advanced cancer. Therefore, it is important to detect and accurately assess the stage of the disease as early as possible.
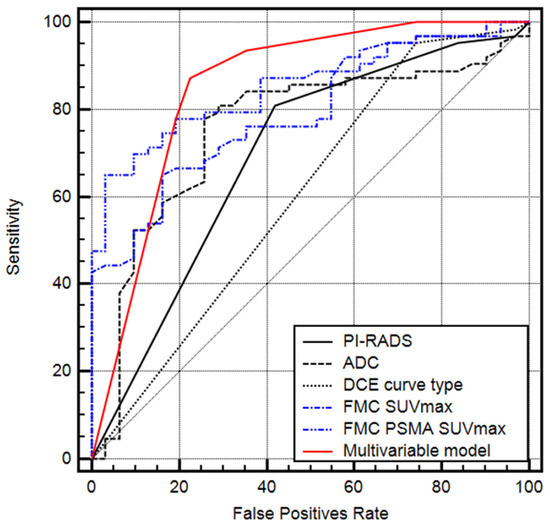
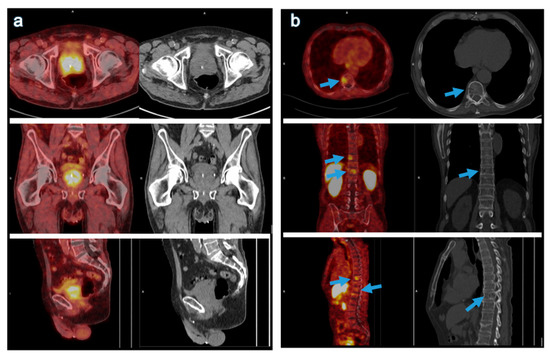
In this respect, prostate-specific membrane antigen (abbreviated as PSMA), which is normally expressed in all types of prostate tissue, including inflammatory, benign, and malignant prostate tissue, has recently become the focus of research. Their levels in patients with PCa and especially those with aggressive types and metastatic as well as castration-resistant PCa increase up to 1000-fold their normal levels and negatively correlate with androgen levels. Thus, these receptors are an exceptionally attractive theranostics molecule for the diagnosis and therapy of prostate tumor and its related metastases. They have subsequently emerged as the target of numerous diagnostic and therapeutic studies, highlighting the critical role of these receptors in the further therapeutic management of patients with prostate cancer.
Dear colleagues, I look forward to your interesting contributions and your valuable experiences with PSMA in the field of PCa.
Dr. Sazan Rasul
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Current Oncology is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- prostate cancer
- prostate-specific membrane antigen
- tumor staging
- PET-CT/MRI
- theranostics