Anti-Inflammatory and Anti-Oxidant Potential of the Root Extract and Constituents of Doronicum austriacum
Abstract
:1. Introduction
2. Results
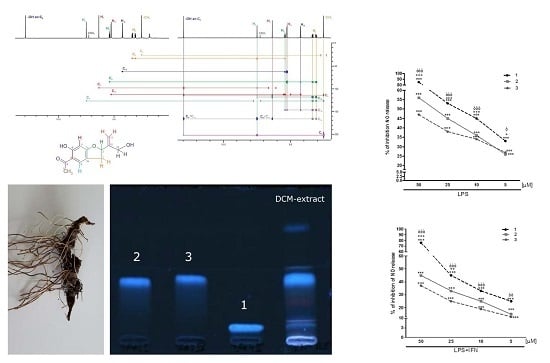
2.1. Identification of the Major Compounds
2.2. Anti-Inflammatory and Anti-Oxidant Potential of the D. austriacum Extract and Isolated Compounds in J774A.1 Macrophages and in C6 Astrocytes
3. Materials and Methods
3.1. Reagents
3.2. Cell Cultures
3.2.1. J774A.1 Murine Macrophages Cell Line
3.2.2. C6 Astroglial Cell Line
3.2.3. Antiproliferative Assay
3.2.4. Measurement of Intracellular ROS
3.2.5. Measurement of NO Release
3.2.6. iNOS Detection by Cytofluorimetry
3.2.7. Nitrotyrosine Detection by Confocal Microscopy
3.2.8. Data Analysis
3.2.9. Plant Material
3.2.10. Extract Preparation
3.2.11. Isolation
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- MacMicking, J.; Xie, Q.W.; Nathan, C. Nitric oxide and macrophage function. Annu. Rev. Immunol. 1997, 15, 323–350. [Google Scholar] [CrossRef] [PubMed]
- Pike, J.; Chandra, R.K. Effect of vitamin and trace element supplementation on immune indices in healthy elderly. Int. J. Vitam. Nutr. Res. 1995, 65, 117–121. [Google Scholar] [PubMed]
- Popolo, A.; Autore, G.; Pinto, A.; Marzocco, S. Oxidative stress in patients with cardiovascular disease and chronic renal failure. Free Radic. Res. 2013, 47, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.T.; Yu, J.; Grass, D.; de Beer, F.C.; Kindy, M.S. Inflammation-dependent cerebral deposition of serum amyloid a protein in a mouse model of amyloidosis. J. Neurosci. 2002, 22, 5900–5909. [Google Scholar] [PubMed]
- Frank-Cannon, T.C.; Alto, L.T.; McAlpine, F.E.; Tansey, M.G. Does neuroinflammation fan the flame in neurodegenerative diseases? Mol. Neurodegener. 2009, 4, 47. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.D., Jr.; Odunze, I.N. Oxygen free radicals and Parkinson’s disease. Free Radic. Biol. Med. 1991, 10, 161–169. [Google Scholar] [CrossRef]
- Smith, M.A.; Richey, P.L.; Taneda, S.; Kutty, R.K.; Sayre, L.M.; Monnier, V.M.; Perry, G. Advanced Maillard reaction end products, free radicals, and protein oxidation in Alzheimer’s disease. Ann. N. Y. Acad. Sci. 1994, 738, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Petersen, A.; Mani, K.; Brundin, P. Recent advances on the pathogenesis of Huntington’s disease. Exp. Neurol. 1999, 157, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Uttara, B.; Singh, A.V.; Zamboni, P.; Mahajan, R.T. Oxidative Stress and Neurodegenerative Diseases: A Review of Upstream and Downstream Antioxidant Therapeutic Options. Curr. Neuropharmacol. 2009, 7, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.V.; Hanna, P.M.; Mason, R.P. The origin of the hydroxyl radical oxygen in the Fenton Reaction. Free Radic. Biol. Med. 1997, 22, 885–888. [Google Scholar] [CrossRef]
- Hsieh, H.L.; Yang, C.M. Role of redox signaling in neuroinflammation and neurodegenerative diseases. Biomed. Res. Int. 2013, 2013, 484613. [Google Scholar] [CrossRef] [PubMed]
- Bohlmann, F.; Zdero, C. New Benzofuran Derivatives from Doronicum austriacum Jacq. Tetrahedron Lett. 1970, 41, 3575–3576. [Google Scholar] [CrossRef]
- Tabernaemontanus, J.T. New Vollkommen Kräuter-Buch, 1625. pp. 47–48. Available online: http://www.kraeuter.ch (accessed on 16 February 2017).
- Petričić, J.; Osmak, M.; Hadžija, M.; Kalodera, Z.; Slijepčević, M. Alkaloid concentrate from Doronicum austriacum inhibits the growth of mouse fibroblasts in vitro and the growth of mouse mammary carcinoma in vivo. Acta Pharm. Jugosl. 1991, 41, 169–173. [Google Scholar]
- Bohlmann, F.; Abraham, W.R. Ein neuer Sesquiterpenalkohol und andere Inhaltsstoffe aus Doronicum pardalianches. Phytochemistry 1979, 18, 668–671. [Google Scholar] [CrossRef]
- Bohlmann, F.; Grenz, M. Neue Tremeton-derivate aus Doronicum macrophyllum. Phytochemistry 1979, 18, 179–181. [Google Scholar] [CrossRef]
- Pelly, S.C.; Govender, S.; Fernandes, M.A.; Schmalz, H.G.; de Koning, C.B. Stereoselective syntheses of the 2-Isopropenyl-2,3-dihydrobenzofuran nucleus: Potential chiral building blocks for the syntheses of tremetone, hydroxytremetone, and rotenone. J. Org. Chem. 2007, 72, 2857–2864. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, M.; Magistretti, P.J. The role of astroglia in neuroprotection. Dialogues Clin. Neurosci. 2009, 11, 281–295. [Google Scholar] [PubMed]
- Schopfer, F.J.; Baker, P.R.; Freeman, B.A. NO-dependent protein nitration: A cell signaling event or an oxidative inflammatory response? Trends Biochem. Sci. 2003, 28, 646–654. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.Z.; Lee, S.T.; Collett, M.G.; Stegelmeier, B.L.; Green, B.T.; Buck, S.R.; Pfister, J.A. Toxicity of white snake-root (Ageratina altissima) and chemical extracts of white snake-root in goats. J. Agric. Food Chem. 2015, 63, 2092–2097. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.M.; DeGraw, J.I., Jr.; Shah, V.R.; Bonner, W.A. The synthesis and pharmacological action of tremetone. J. Med. Chem. 1963, 6, 315–319. [Google Scholar] [CrossRef]
- Pepe, G.; Sommella, E.; Manfra, M.; de Nisco, M.; Tenore, G.C.; Scopa, A.; Sofo, A.; Marzocco, S.; Adesso, S.; Novellino, T.; et al. Evaluation of anti-inflammatory activity and fast UHPLC-DAD-IT-TOF profiling of polyphenolic compounds extracted from green lettuce (Lactuca sativa L. var. Maravilla de Verano). Food Chem. 2015, 167, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Adesso, S.; Magnus, T.; Cuzzocrea, S.; Campolo, M.; Rissiek, B.; Paciello, O.; Autore, G.; Pinto, A.; Marzocco, S. Indoxyl sulfate affects glial function increasing oxidative stress and neuroinflammation in chronic kidney disease: Interaction between astrocytes and microglia. Front. Pharmacol. 2017, 8, 370. [Google Scholar] [CrossRef]
- Bianco, G.; Russo, R.; Marzocco, S.; Velotto, S.; Autore, G.; Severino, L. Modulation of macrophage activity by aflatoxins B1 and B2 and their metabolites aflatoxins M1 and M2. Toxicon 2012, 59, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Del Regno, M.; Adesso, S.; Popolo, A.; Quaroni, A.; Autore, G.; Severino, L.; Marzocco, S. Nivalenol induces oxidative stress and increases deoxynivalenol pro-oxidant effect in intestinal epithelial cells. Toxicol. Appl. Pharmacol. 2015, 285, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Marzocco, S.; Calabrone, L.; Adesso, S.; Larocca, M.; Franceschelli, S.; Autore, G.; Martelli, G.; Rossano, R. Anti-inflammatory activity of horseradish (Armoracia rusticana) root extracts in LPS-stimulated macrophages. Food Funct. 2015, 6, 3778–3788. [Google Scholar] [CrossRef] [PubMed]
- Bruhn, T.; Schaumloeffel, A.; Hemberger, Y.; Bringmann, G. SpecDis: Quantifying the comparison of calculated and experimental electronic circular dichroism spectra. Chirality 2013, 25, 243–249. [Google Scholar] [CrossRef] [PubMed]
Sample Availability: Samples of the compounds 1 to 3 are available from the authors. |






| Position | 1H-NMR Data of 1 | 13C-NMR Data of 1 | 1H-NMR Data of 2 | 13C-NMR Data of 2 | 1H-NMR Data of 3 | 13C-NMR Data of 3 |
|---|---|---|---|---|---|---|
| 2 | 5.40 t (8.6) | 85.3 d | 5.36 t (8.4) | 84.9 d | 5.36 t (8.4) | 84.9 d |
| 3 | Ha 3.36 ddd (0.9, 9.4, 15.4) Hb 3.09 ddd (1.3, 7.8, 15.3) | 33.6 t | Ha 3.36 ddd (0.8, 9.5, 15.2) Hb 3.10 ddd (1.1, 7.5, 15.3) | 33.6 t | Ha 3.35 ddd (0.8, 9.5, 15.2) Hb 3.10 ddd (1.2, 7.6, 15.4) | 33.7 t |
| 3a | --- | 118.5 s | --- | 118.3 s | --- | 118.7 s |
| 4 | 7.49 t (1.3) | 126.9 d | 7.50 t (1.3) | 126.7 d | 7.49 t (1.2) | 126.7 d |
| 5 | --- | 113.8 s | --- | 113.9 s | --- | 114.0 s |
| 6 | --- | 165.3 1 s | --- | 165.6 s | --- | 166.1 s |
| 7 | 6.36 s | 98.3 d | 6.37 s | 98.3 d | 6.37 s | 98.3 d |
| 7a | --- | 165.3 1 s | --- | 166.0 s | --- | 166.5 s |
| 8 | --- | 201.9 s | --- | 202.0 s | --- | 202.1 s |
| 9 | 2.53 s | 26.1 q | 2.53 s | 26.2 q | 2.53 s | 26.1 q |
| 10 | --- | 146.8 s | --- | 142.5 s | --- | 142.6 s |
| 11 | Ha 5.27 dq (2.1, 0.7) Hb 5.25 dt (1.7, 0.9) | 112.8 t | Ha 5.33 br s Hb 5.27 br s | 114.6 t | Ha 5.33 br s Hb 5.28 br s | 114.8 t |
| 12 | 4.25 s | 62.8 t | 4.67 dd (6.7, 13.6) | 63.4 t | 4.67 dd (7.8, 13.5) | 63.2 t |
| OH at C6 | 12.96 s | --- | 12.95 s | --- | 12.95 s | --- |
| 1’ | --- | 176.8 s | --- | 176.0 s | ||
| 2’ | 2.56 hept (7.0) | 33.9 d | 2.38 hex (7.0) | 41.0 d | ||
| 3’ | 1.16 d (7.0) | 18.7 q | Ha 1.67 m Hb 1.47 hept (7.0) | 26.6 t | ||
| 4’ | 1.16 d (7.0) | 18.7 q | 0.89 t (7.4) | 11.8 q | ||
| 5’ | 1.14 d (7.0) | 16.4 q |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marzocco, S.; Adesso, S.; Alilou, M.; Stuppner, H.; Schwaiger, S. Anti-Inflammatory and Anti-Oxidant Potential of the Root Extract and Constituents of Doronicum austriacum. Molecules 2017, 22, 1003. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules22061003
Marzocco S, Adesso S, Alilou M, Stuppner H, Schwaiger S. Anti-Inflammatory and Anti-Oxidant Potential of the Root Extract and Constituents of Doronicum austriacum. Molecules. 2017; 22(6):1003. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules22061003
Chicago/Turabian StyleMarzocco, Stefania, Simona Adesso, Mostafa Alilou, Hermann Stuppner, and Stefan Schwaiger. 2017. "Anti-Inflammatory and Anti-Oxidant Potential of the Root Extract and Constituents of Doronicum austriacum" Molecules 22, no. 6: 1003. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules22061003