Nanotechnology-Based Dressings for Wound Management
Abstract
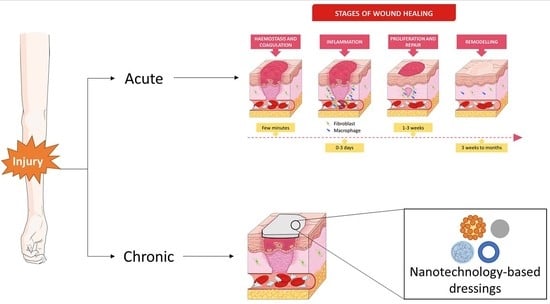
:1. Introduction
2. Physiology of Wound Healing
3. Dressing for Wound Treatment
3.1. Dressing’s Characteristics
3.2. Advanced Therapeutic Dressings
3.3. Biomaterials Used in the Development of Wound Dressings
3.4. Nanotechnology-Based Delivery Systems for Wound Healing
3.4.1. Nanoparticles
3.4.2. Polymeric Nanofibers
3.4.3. Nanohybrids
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Young, A.; McNaught, C.-E. The physiology of wound healing. Surgery 2011, 29, 475–479. [Google Scholar] [CrossRef]
- Pereira, R.F.; Bártolo, P.J. Traditional Therapies for Skin Wound Healing. Adv. Wound Care 2016, 5, 208–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Strodtbeck, F. Physiology of wound healing. Newborn Infant Nurs. Rev. 2001, 1, 43–52. [Google Scholar] [CrossRef]
- Beldon, P. Basic science of wound healing. Surgery 2010, 28, 409–412. [Google Scholar] [CrossRef]
- Groeber, F.; Holeiter, M.; Hampel, M.; Hinderer, S.; Schenke-Layland, K. Skin tissue engineering—In vivo and in vitro applications. Adv. Drug Deliv. Rev. 2011, 63, 352–366. [Google Scholar] [CrossRef]
- Abdelrahman, T.; Newton, H. Wound dressings: Principles and practice. Surgery 2011, 29, 491–495. [Google Scholar] [CrossRef]
- Ueno, C.; Hunt, T.K.; Hopf, H.W. Using Physiology to Improve Surgical Wound Outcomes. Plast. Reconstr. Surg. 2006, 117, 59S–71S. [Google Scholar] [CrossRef]
- Kapp, S.; Santamaria, N. The financial and quality-of-life cost to patients living with a chronic wound in the community. Int. Wound J. 2017, 14, 1108–1119. [Google Scholar] [CrossRef]
- Garcia-Orue, I.; Pedraz, J.L.; Hernandez, R.M.; Igartua, M. Nanotechnology-based delivery systems to release growth factors and other endogenous molecules for chronic wound healing. J. Drug Deliv. Sci. Technol. 2017, 42, 2–17. [Google Scholar] [CrossRef]
- Wattanakaroon, W.; Akanitkul, P.; Kaowkanya, W.; Phoudee, W. Albumin-natural rubber latex composite as a dermal wound dressing. Mater. Today Proc. 2017, 4, 6633–6640. [Google Scholar] [CrossRef]
- Ataide, J.A.; de Carvalho, N.M.; Rebelo, M.D.A.; Chaud, M.V.; Grotto, D.; Gerenutti, M.; Rai, M.; Mazzola, P.G.; Jozala, A.F. Bacterial Nanocellulose Loaded with Bromelain: Assessment of Antimicrobial, Antioxidant and Physical-Chemical Properties. Sci. Rep. 2017, 7, 18031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simões, D.; Miguel, S.P.; Ribeiro, M.P.; Coutinho, P.; Mendonça, A.G.; Correia, I.J. Recent advances on antimicrobial wound dressing: A review. Eur. J. Pharm. Biopharm. 2018, 127, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Pinese, C.; Jebors, S.; Stoebner, P.E.; Humblot, V.; Verdié, P.; Causse, L.; Garric, X.; Taillades, H.; Martinez, J.; Mehdi, A.; et al. Bioactive peptides grafted silicone dressings: A simple and specific method. Mater. Today Chem. 2017, 4, 73–83. [Google Scholar] [CrossRef]
- Andreu, V.; Mendoza, G.; Arruebo, M.; Irusta, S. Smart Dressings Based on Nanostructured Fibers Containing Natural Origin Antimicrobial, Anti-Inflammatory, and Regenerative Compounds. Materials 2015, 8, 5154–5193. [Google Scholar] [CrossRef]
- Aruan, N.M.; Sriyanti, I.; Edikresnha, D.; Suciati, T.; Munir, M.M.; Khairurrijal. Polyvinyl Alcohol/Soursop Leaves Extract Composite Nanofibers Synthesized Using Electrospinning Technique and their Potential as Antibacterial Wound Dressing. Procedia Eng. 2017, 170, 31–35. [Google Scholar] [CrossRef]
- Garcia-Orue, I.; Gainza, G.; Gutierrez, F.B.; Aguirre, J.J.; Evora, C.; Pedraz, J.L.; Hernandez, R.M.; Delgado, A.; Igartua, M. Novel nanofibrous dressings containing rhEGF and Aloe vera for wound healing applications. Int. J. Pharm. 2017, 523, 556–566. [Google Scholar] [CrossRef]
- Tummalapalli, M.; Berthet, M.; Verrier, B.; Deopura, B.L.; Alam, M.S.; Gupta, B. Composite wound dressings of pectin and gelatin with aloe vera and curcumin as bioactive agents. Int. J. Biol. Macromol. 2016, 82, 104–113. [Google Scholar] [CrossRef]
- Rajendran, N.K.; Kumar, S.S.D.; Houreld, N.N.; Abrahamse, H. A review on nanoparticle based treatment for wound healing. J. Drug Deliv. Sci. Technol. 2018, 44, 421–430. [Google Scholar] [CrossRef]
- Stoica, A.E.; Chircov, C.; Grumezescu, A.M. Nanomaterials for Wound Dressings: An Up-to-Date Overview. Molecules 2020, 25, 2699. [Google Scholar] [CrossRef]
- Kalashnikova, I.; Das, S.; Seal, S. Nanomaterials for wound healing: Scope and advancement. Nanomedicine 2015, 10, 2593–2612. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Thu, H.E.; Amjad, M.W.; Hussain, F.; Ahmed, T.A.; Khan, S. Exploring recent developments to improve antioxidant, anti-inflammatory and antimicrobial efficacy of curcumin: A review of new trends and future perspectives. Mater. Sci. Eng. C 2017, 77, 1316–1326. [Google Scholar] [CrossRef] [PubMed]
- VanDyke, D.; Kyriacopulos, P.; Yassini, B.; Wright, A.; Burkhart, E.; Jacek, S.; Pratt, M.; Peterson, C.R.; Rai, P. Nanoparticle Based Combination Treatments for Targeting Multiple Hallmarks of Cancer. Int. J. Nano Stud. Technol. 2016, S4, 1–18. [Google Scholar] [CrossRef]
- Lazarus, G.S.; Cooper, D.M.; Knighton, D.R.; Margolis, D.J.; Pecoraro, R.E.; Rodeheaver, G.; Robson, M.C. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch. Dermatol. 1994, 130, 489–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gottrup, F.; Agren, M.S.; Karlsmark, T. Models for use in wound healing research: A survey focusing on in vitro and in vivo adult soft tissue. Wound Repair Regen. Off. Publ. Wound Heal. Soc. Eur. Tissue Repair Soc. 2000, 8, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Martin, P. Wound healing—Aiming for perfect skin regeneration. Science 1997, 276, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.; Fronza, M.; Goettert, M.; Geller, F.; Luik, S.; Flores, E.M.M.; Bittencourt, C.F.; Zanetti, G.D.; Heinzmann, B.M.; Laufer, S.; et al. Biological studies on Brazilian plants used in wound healing. J. Ethnopharmacol. 2009, 122, 523–532. [Google Scholar] [CrossRef]
- Gurtner, G.C.; Werner, S.; Barrandon, Y.; Longaker, M.T. Wound repair and regeneration. Nature 2008, 453, 314–321. [Google Scholar] [CrossRef]
- Reinke, J.M.; Sorg, H. Wound Repair and Regeneration. Eur. Surg. Res. 2012, 49, 35–43. [Google Scholar] [CrossRef]
- Fonder, M.A.; Lazarus, G.S.; Cowan, D.A.; Aronson-Cook, B.; Kohli, A.R.; Mamelak, A.J. Treating the chronic wound: A practical approach to the care of nonhealing wounds and wound care dressings. J. Am. Acad. Dermatol. 2008, 58, 185–206. [Google Scholar] [CrossRef]
- Kumar, B.; Vijayakumar, M.; Govindarajan, R.; Pushpangadan, P. Ethnopharmacological approaches to wound healing—Exploring medicinal plants of India. J. Ethnopharmacol. 2007, 114, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Morton, L.M.; Phillips, T.J. Wound healing and treating wounds: Differential diagnosis and evaluation of chronic wounds. J. Am. Acad. Dermatol. 2016, 74, 589–605. [Google Scholar] [CrossRef] [PubMed]
- Oryan, A.; Alemzadeh, E. Effects of insulin on wound healing: A review of animal and human evidences. Life Sci. 2017, 174, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.; Harding, K. Wound healing. Medicine 2004, 32, 4–7. [Google Scholar] [CrossRef]
- Bryant, R.A.; Nix, D.P. Acute and Chronic Wounds: Current Management Concepts, 5th ed.; Mosby: St Louis, MO, USA, 2016; p. 648. [Google Scholar]
- Bailey, A.J.; Bazin, S.; Sims, T.J.; Le Lous, M.; Nicoletis, C.; Delaunay, A. Characterization of the collagen of human hypertrophic and normal scars. Biochim. Biophys. Acta-Protein Struct. 1975, 405, 412–421. [Google Scholar] [CrossRef]
- Schilling, J.A. Wound healing. Surg. Clin. N. Am. 1976, 56, 859–874. [Google Scholar] [CrossRef]
- Levenson, S.M.; Geever, E.F.; Crowley, L.V.; Oates, J.F.; Berard, C.W.; Rosen, H. Healing of Rat Skin Wounds. Ann. Surg. 1965, 161, 293–308. [Google Scholar] [CrossRef]
- Landén, N.X.; Li, D.; Ståhle, M. Transition from inflammation to proliferation: A critical step during wound healing. Cell. Mol. Life Sci. 2016, 73, 3861–3885. [Google Scholar] [CrossRef] [Green Version]
- Robson, M.C.; Steed, D.L.; Franz, M.G. Wound healing: Biologic features and approaches to maximize healing trajectories. Curr. Probl. Surg. 2001, 38, 72–140. [Google Scholar] [CrossRef]
- Werner, S.; Grose, R. Regulation of Wound Healing by Growth Factors and Cytokines. Physiol. Rev. 2003, 83, 835–870. [Google Scholar] [CrossRef]
- Frykberg, R.G.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, J.U.; Lee, S.W.; Pangeni, R.; Byun, Y.; Yoon, I.-S.; Park, J.W. Preparation and in vivo evaluation of cationic elastic liposomes comprising highly skin-permeable growth factors combined with hyaluronic acid for enhanced diabetic wound-healing therapy. Acta Biomater. 2017, 57, 197–215. [Google Scholar] [CrossRef]
- Winter, G.D. Formation of the Scab and the Rate of Epithelization of Superficial Wounds in the Skin of the Young Domestic Pig. Nature 1962, 193, 293–294. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.M. Optimizing wound healing. A practice within nursing’s domain. Nurs. Clin. N. Am. 1990, 25, 165–180. [Google Scholar] [CrossRef]
- Cuzzell, J.Z.; Stotts, N.A. Wound care. Trial & error yields to knowledge. Am. J. Nurs. 1990, 90, 53–60, 63. [Google Scholar]
- Winter, G.D.; Scales, J.T. Effect of Air Drying and Dressings on the Surface of a Wound. Nature 1963, 197, 91–92. [Google Scholar] [CrossRef]
- Salas Campos, L.; Fernandes Mansilla, M.; Martinez de la Chica, A.M. Topical chemotherapy for the treatment of burns. Rev. Enferm. 2005, 28, 67–70. [Google Scholar]
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.E.; Eccleston, G.M. Wound healing dressings and drug delivery systems: A review. J. Pharm. Sci. 2008, 97, 2892–2923. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressings—A review. BioMedicine 2015, 5, 22. [Google Scholar] [CrossRef]
- Fraser, J.F.; Cuttle, L.; Kempf, M.; Kimble, R.M. Cytotoxicity of topical antimicrobial agents used in burn wounds in Australasia. ANZ J. Surg. 2004, 74, 139–142. [Google Scholar] [CrossRef]
- Atiyeh, B.S.; Costagliola, M.; Hayek, S.N.; Dibo, S.A. Effect of silver on burn wound infection control and healing: Review of the literature. Burns 2007, 33, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Vowden, K.; Vowden, P. Wound dressings: Principles and practice. Surgery 2017, 35, 489–494. [Google Scholar] [CrossRef]
- Jayakumar, R.; Prabaharan, M.; Sudheesh Kumar, P.T.; Nair, S.V.; Tamura, H. Biomaterials based on chitin and chitosan in wound dressing applications. Biotechnol. Adv. 2011, 29, 322–337. [Google Scholar] [CrossRef] [PubMed]
- Abrigo, M.; McArthur, S.L.; Kingshott, P. Electrospun Nanofibers as Dressings for Chronic Wound Care: Advances, Challenges, and Future Prospects. Macromol. Biosci. 2014, 14, 772–792. [Google Scholar] [CrossRef]
- Ding, L.; Shan, X.; Zhao, X.; Zha, H.; Chen, X.; Wang, J.; Cai, C.; Wang, X.; Li, G.; Hao, J.; et al. Spongy bilayer dressing composed of chitosan–Ag nanoparticles and chitosan–Bletilla striata polysaccharide for wound healing applications. Carbohydr. Polym. 2017, 157, 1538–1547. [Google Scholar] [CrossRef]
- Seaman, S. Dressing selection in chronic wound management. J. Am. Podiatr. Med. Assoc. 2002, 92, 24–33. [Google Scholar] [CrossRef]
- Hajská, M.; Dragúňová, J.; Koller, J. Cytotoxicity testing of burn wound dressings: First results. Cell Tissue Bank. 2017, 18, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Sarabahi, S. Recent advances in topical wound care. Indian J. Plast. Surg. Off. Publ. Assoc. Plast. Surg. India 2012, 45, 379–387. [Google Scholar] [CrossRef]
- Jin, S.G.; Kim, K.S.; Yousaf, A.M.; Kim, D.W.; Jang, S.W.; Son, M.-W.; Kim, Y.H.; Yong, C.S.; Kim, J.O.; Choi, H.-G. Mechanical properties and in vivo healing evaluation of a novel Centella asiatica-loaded hydrocolloid wound dressing. Int. J. Pharm. 2015, 490, 240–247. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Kenawy, E.-R.S.; Chen, X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017, 8, 217–233. [Google Scholar] [CrossRef]
- Mulholland, E.J.; Dunne, N.; McCarthy, H.O. MicroRNA as Therapeutic Targets for Chronic Wound Healing. Mol. Ther.-Nucleic Acids 2017, 8, 46–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garg, T.; Rath, G.; Goyal, A.K. Biomaterials-based nanofiber scaffold: Targeted and controlled carrier for cell and drug delivery. J. Drug Target. 2015, 23, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Ikram, S. Chitosan Based Scaffolds and Their Applications in Wound Healing. Achiev. Life Sci. 2016, 10, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Ganesan, P. Natural and bio polymer curative films for wound dressing medical applications. Wound Med. 2017, 18, 33–40. [Google Scholar] [CrossRef]
- Khan, M.I.H.; Islam, J.M.M.; Kabir, W.; Rahman, A.; Mizan, M.; Rahman, M.F.; Amin, J.; Khan, M.A. Development of hydrocolloid Bi-layer dressing with bio-adhesive and non-adhesive properties. Mater. Sci. Eng. C 2016, 69, 609–615. [Google Scholar] [CrossRef]
- Karaki, N.; Aljawish, A.; Humeau, C.; Muniglia, L.; Jasniewski, J. Enzymatic modification of polysaccharides: Mechanisms, properties, and potential applications: A review. Enzym. Microb. Technol. 2016, 90, 1–18. [Google Scholar] [CrossRef]
- Singh, B.; Kumar, A. Radiation formation of functionalized polysaccharide-protein based skin mimicking semi- inter penetrating network for biomedical application. Int. J. Biol. Macromol. 2016, 92, 1136–1150. [Google Scholar] [CrossRef]
- Lohani, A.; Singh, G.; Bhattacharya, S.S.; Rama Hegde, R.; Verma, A. Tailored-interpenetrating polymer network beads of κ-carrageenan and sodium carboxymethyl cellulose for controlled drug delivery. J. Drug Deliv. Sci. Technol. 2016, 31, 53–64. [Google Scholar] [CrossRef]
- Mogoşanu, G.D.; Grumezescu, A.M. Natural and synthetic polymers for wounds and burns dressing. Int. J. Pharm. 2014, 463, 127–136. [Google Scholar] [CrossRef]
- Tavakoli, J. Physico-mechanical, morphological and biomedical properties of a novel natural wound dressing material. J. Mech. Behav. Biomed. Mater. 2017, 65, 373–382. [Google Scholar] [CrossRef]
- Tranquilan-Aranilla, C.; Barba, B.J.D.; Vista, J.R.M.; Abad, L.V. Hemostatic efficacy evaluation of radiation crosslinked carboxymethyl kappa-carrageenan and chitosan with varying degrees of substitution. Radiat. Phys. Chem. 2016, 124, 124–129. [Google Scholar] [CrossRef]
- Zia, K.M.; Tabasum, S.; Nasif, M.; Sultan, N.; Aslam, N.; Noreen, A.; Zuber, M. A review on synthesis, properties and applications of natural polymer based carrageenan blends and composites. Int. J. Biol. Macromol. 2017, 96, 282–301. [Google Scholar] [CrossRef] [PubMed]
- Miranda, O.J.; Srinivasan, G. Advanced trends in treatment of wounds. Curr. Sci. 2016, 111, 7. [Google Scholar] [CrossRef]
- Hazer, D.B.; Kılıçay, E.; Hazer, B. Poly(3-hydroxyalkanoate)s: Diversification and biomedical applications: A state of the art review. Mater. Sci. Eng. C 2012, 32, 637–647. [Google Scholar] [CrossRef]
- Broussard, K.C.; Powers, J.G. Wound Dressings: Selecting the Most Appropriate Type. Am. J. Clin. Dermatol. 2013, 14, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Boateng, J.; Catanzano, O. Advanced Therapeutic Dressings for Effective Wound Healing—A Review. J. Pharm. Sci. 2015, 104, 3653–3680. [Google Scholar] [CrossRef] [Green Version]
- Barnea, Y.; Weiss, J.; Gur, E. A review of the applications of the hydrofiber dressing with silver (Aquacel Ag) in wound care. Ther. Clin. Risk Manag. 2010, 6, 21–27. [Google Scholar] [CrossRef] [Green Version]
- Kaur, G.; Narayanan, G.; Garg, D.; Sachdev, A.; Matai, I. Biomaterials-Based Regenerative Strategies for Skin Tissue Wound Healing. ACS Appl. Bio Mater. 2022, 5, 2069–2106. [Google Scholar] [CrossRef]
- Bianchera, A.; Catanzano, O.; Boateng, J.; Elviri, L. The place of biomaterials in wound healing. In Therapeutic Dressings and Wound Healing Applications; Wiley: Hoboken, NJ, USA, 2020; pp. 337–366. [Google Scholar]
- Ijaola, A.O.; Akamo, D.O.; Damiri, F.; Akisin, C.J.; Bamidele, E.A.; Ajiboye, E.G.; Berrada, M.; Onyenokwe, V.O.; Yang, S.-Y.; Asmatulu, E. Polymeric biomaterials for wound healing applications: A comprehensive review. J. Biomater. Sci. Polym. Ed. 2022, 33, 1998–2050. [Google Scholar] [CrossRef]
- Momoh, F.U.; Boateng, J.S.; Richardson, S.C.W.; Chowdhry, B.Z.; Mitchell, J.C. Development and functional characterization of alginate dressing as potential protein delivery system for wound healing. Int. J. Biol. Macromol. 2015, 81, 137–150. [Google Scholar] [CrossRef] [Green Version]
- Duckworth, P.F.; Maddocks, S.E.; Rahatekar, S.S.; Barbour, M.E. Alginate films augmented with chlorhexidine hexametaphosphate particles provide sustained antimicrobial properties for application in wound care. J. Mater. Sci. Mater. Med. 2020, 31, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, X.; Liu, L.; An, T.; Xian, M.; Luckanagul, J.A.; Su, Z.; Lin, Y.; Wang, Q. A hydrogen sulfide-releasing alginate dressing for effective wound healing. Acta Biomater. 2020, 104, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Chen, J.; Shi, M.; Zhang, H.; Ma, P.X.; Guo, B. Electroactive anti-oxidant polyurethane elastomers with shape memory property as non-adherent wound dressing to enhance wound healing. Chem. Eng. J. 2019, 375, 121999. [Google Scholar] [CrossRef]
- Liu, X.; Niu, Y.; Chen, K.C.; Chen, S. Rapid hemostatic and mild polyurethane-urea foam wound dressing for promoting wound healing. Mater. Sci. Eng. C 2017, 71, 289–297. [Google Scholar] [CrossRef]
- Croisfelt, F.M.; Ataide, J.A.; Tundisi, L.L.; Cefali, L.C.; Rebelo, M.D.A.; Sánchez, J.L.D.; da Costa, T.G.; Lima, R.; Jozala, A.F.; Chaud, M.V.; et al. Characterization of PNIPAAm-co-AAm hydrogels for modified release of bromelain. Eur. Polym. J. 2018, 105, 48–54. [Google Scholar] [CrossRef]
- Jin, S.G.; Kim, K.S.; Kim, D.W.; Kim, D.S.; Seo, Y.G.; Go, T.G.; Youn, Y.S.; Kim, J.O.; Yong, C.S.; Choi, H.-G. Development of a novel sodium fusidate-loaded triple polymer hydrogel wound dressing: Mechanical properties and effects on wound repair. Int. J. Pharm. 2016, 497, 114–122. [Google Scholar] [CrossRef]
- Liu, X.; Wong, K.K.Y. Application of nanomedicine in wound healing. In Nanotechnology in Dermatology; Nasir, A., Friedman, A., Wang, S., Eds.; Springer: New York, NY, USA, 2013; pp. 221–229. [Google Scholar]
- Hamdan, S.; Pastar, I.; Drakulich, S.; Dikici, E.; Tomic-Canic, M.; Deo, S.; Daunert, S. Nanotechnology-Driven Therapeutic Interventions in Wound Healing: Potential Uses and Applications. ACS Cent. Sci. 2017, 3, 163–175. [Google Scholar] [CrossRef]
- Zhang, R.X.; Li, J.; Zhang, T.; Amini, M.A.; He, C.; Lu, B.; Ahmed, T.; Lip, H.; Rauth, A.M.; Wu, X.Y. Importance of integrating nanotechnology with pharmacology and physiology for innovative drug delivery and therapy—An illustration with firsthand examples. Acta Pharmacol. Sin. 2018, 39, 825–844. [Google Scholar] [CrossRef] [Green Version]
- Naraginti, S.; Kumari, P.L.; Das, R.K.; Sivakumar, A.; Patil, S.H.; Andhalkar, V.V. Amelioration of excision wounds by topical application of green synthesized, formulated silver and gold nanoparticles in albino Wistar rats. Mater. Sci. Eng. C 2016, 62, 293–300. [Google Scholar] [CrossRef]
- De Oliveira, D.M.; Menezes, D.B.; Andrade, L.R.; Lima, F.D.C.; Hollanda, L.; Zielinska, A.; Sanchez-Lopez, E.; Souto, E.B.; Severino, P. Silver nanoparticles obtained from Brazilian pepper extracts with synergistic anti-microbial effect: Production, characterization, hydrogel formulation, cell viability, and in vitro efficacy. Pharm. Dev. Technol. 2021, 26, 539–548. [Google Scholar] [CrossRef]
- Pannerselvam, B.; Dharmalingam Jothinathan, M.K.; Rajenderan, M.; Perumal, P.; Pudupalayam Thangavelu, K.; Kim, H.J.; Singh, V.; Rangarajulu, S.K. An in vitro study on the burn wound healing activity of cotton fabrics incorporated with phytosynthesized silver nanoparticles in male Wistar albino rats. Eur. J. Pharm. Sci. 2017, 100, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, K.R.; Koodali, R.T.; Manna, A.C. Size-Dependent Bacterial Growth Inhibition and Mechanism of Antibacterial Activity of Zinc Oxide Nanoparticles. Langmuir 2011, 27, 4020–4028. [Google Scholar] [CrossRef] [PubMed]
- El-Feky, G.S.; Sharaf, S.S.; El Shafei, A.; Hegazy, A.A. Using chitosan nanoparticles as drug carriers for the development of a silver sulfadiazine wound dressing. Carbohydr. Polym. 2017, 158, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Ataide, J.A.; Cefali, L.C.; Figueiredo, M.C.; Braga, L.E.D.O.; Ruiz, A.L.T.G.; Foglio, M.A.; Oliveira-Nascimento, L.; Mazzola, P.G. In vitro performance of free and encapsulated bromelain. Sci. Rep. 2021, 11, 10195. [Google Scholar] [CrossRef]
- Ataide, J.A.; Geraldes, D.C.; Gérios, E.F.; Bissaco, F.M.; Cefali, L.C.; Oliveira-Nascimento, L.; Mazzola, P.G. Freeze-dried chitosan nanoparticles to stabilize and deliver bromelain. J. Drug Deliv. Sci. Technol. 2021, 61, 102225. [Google Scholar] [CrossRef]
- Ataide, J.A.; Gerios, E.F.; Cefali, L.C.; Fernandes, A.R.; Teixeira, M.D.C.; Ferreira, N.R.; Tambourgi, E.B.; Jozala, A.F.; Chaud, M.V.; Oliveira-Nascimento, L.; et al. Effect of Polysaccharide Sources on the Physicochemical Properties of Bromelain-Chitosan Nanoparticles. Polymers 2019, 11, 1681. [Google Scholar] [CrossRef] [Green Version]
- Rosseto, H.C.; Toledo, L.D.A.S.D.; Francisco, L.M.B.D.; Esposito, E.; Lim, Y.; Valacchi, G.; Cortesi, R.; Bruschi, M.L. Nanostructured lipid systems modified with waste material of propolis for wound healing: Design, in vitro and in vivo evaluation. Colloids Surf. B Biointerfaces 2017, 158, 441–452. [Google Scholar] [CrossRef]
- Dos Santos, C.A.; dos Santos, G.R.; Soeiro, V.S.; dos Santos, J.R.; Rebelo, M.D.A.; Chaud, M.V.; Gerenutti, M.; Grotto, D.; Pandit, R.; Rai, M.; et al. Bacterial nanocellulose membranes combined with nisin: A strategy to prevent microbial growth. Cellulose 2018, 25, 6681–6689. [Google Scholar] [CrossRef]
- Dos Santos, G.R.; Soeiro, V.S.; Talarico, C.F.; Ataide, J.A.; Lopes, A.M.; Mazzola, P.G.; Oliveira, T.J.; Oliveira Junior, J.M.; Grotto, D.; Jozala, A.F. Bacterial Cellulose Membranes as Carriers for Nisin: Incorporation, Antimicrobial Activity, Cytotoxicity and Morphology. Polymers 2022, 14, 3497. [Google Scholar] [CrossRef]
- Huanbutta, K.; Sittikijyothin, W.; Sangnim, T. Development and Characterization of Bilayer Wound Healing Patch Nanofiber Fabricated by Electrospinning. J. Nano Res. 2019, 59, 46–56. [Google Scholar] [CrossRef]
- Sangnim, T.; Limmatvapirat, S.; Nunthanid, J.; Sriamornsak, P.; Sittikijyothin, W.; Wannachaiyasit, S.; Huanbutta, K. Design and characterization of clindamycin-loaded nanofiber patches composed of polyvinyl alcohol and tamarind seed gum and fabricated by electrohydrodynamic atomization. Asian J. Pharm. Sci. 2018, 13, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Diniz, F.R.; Maia, R.C.A.P.; Rannier Andrade, L.; Andrade, L.N.; Vinicius Chaud, M.; da Silva, C.F.; Corrêa, C.B.; de Albuquerque Junior, R.L.C.; Pereira da Costa, L.; Shin, S.R.; et al. Silver Nanoparticles-Composing Alginate/Gelatine Hydrogel Improves Wound Healing In Vivo. Nanomaterials 2020, 10, 390. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.T.S.; Lakshmanan, V.-K.; Anilkumar, T.V.; Ramya, C.; Reshmi, P.; Unnikrishnan, A.G.; Nair, S.V.; Jayakumar, R. Flexible and Microporous Chitosan Hydrogel/Nano ZnO Composite Bandages for Wound Dressing: In Vitro and In Vivo Evaluation. ACS Appl. Mater. Interfaces 2012, 4, 2618–2629. [Google Scholar] [CrossRef]
- Kumar, P.T.S.; Lakshmanan, V.-K.; Raj, M.; Biswas, R.; Hiroshi, T.; Nair, S.V.; Jayakumar, R. Evaluation of Wound Healing Potential of β-Chitin Hydrogel/Nano Zinc Oxide Composite Bandage. Pharm. Res. 2013, 30, 523–537. [Google Scholar] [CrossRef]
- Khorasani, M.T.; Joorabloo, A.; Adeli, H.; Mansoori-Moghadam, Z.; Moghaddam, A. Design and optimization of process parameters of polyvinyl (alcohol)/chitosan/nano zinc oxide hydrogels as wound healing materials. Carbohydr. Polym. 2019, 207, 542–554. [Google Scholar] [CrossRef] [PubMed]
- Khalid, A.; Khan, R.; Ul-Islam, M.; Khan, T.; Wahid, F. Bacterial cellulose-zinc oxide nanocomposites as a novel dressing system for burn wounds. Carbohydr. Polym. 2017, 164, 214–221. [Google Scholar] [CrossRef]
- Maneerung, T.; Tokura, S.; Rujiravanit, R. Impregnation of silver nanoparticles into bacterial cellulose for antimicrobial wound dressing. Carbohydr. Polym. 2008, 72, 43–51. [Google Scholar] [CrossRef]
- Augustine, R.; Malik, H.N.; Singhal, D.K.; Mukherjee, A.; Malakar, D.; Kalarikkal, N.; Thomas, S. Electrospun polycaprolactone/ZnO nanocomposite membranes as biomaterials with antibacterial and cell adhesion properties. J. Polym. Res. 2014, 21, 347. [Google Scholar] [CrossRef]
- Dhand, C.; Venkatesh, M.; Barathi, V.A.; Harini, S.; Bairagi, S.; Goh Tze Leng, E.; Muruganandham, N.; Low, K.Z.W.; Fazil, M.H.U.T.; Loh, X.J.; et al. Bio-inspired crosslinking and matrix-drug interactions for advanced wound dressings with long-term antimicrobial activity. Biomaterials 2017, 138, 153–168. [Google Scholar] [CrossRef]
- Sanchez-Lopez, E.; Gomes, D.; Esteruelas, G.; Bonilla, L.; Lopez-Machado, A.L.; Galindo, R.; Cano, A.; Espina, M.; Ettcheto, M.; Camins, A.; et al. Metal-Based Nanoparticles as Antimicrobial Agents: An Overview. Nanomaterials 2020, 10, 292. [Google Scholar] [CrossRef] [Green Version]
- Barui, A.K.; Veeriah, V.; Mukherjee, S.; Manna, J.; Patel, A.K.; Patra, S.; Pal, K.; Murali, S.; Rana, R.K.; Chatterjee, S.; et al. Zinc oxide nanoflowers make new blood vessels. Nanoscale 2012, 4, 7861–7869. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Han, Y.; Cui, M.; Tey, H.L.; Wang, L.-H.; Xu, C. ZnO nanoparticles as an antimicrobial tissue adhesive for skin wound closure. J. Mater. Chem. B 2017, 5, 4535–4541. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Macedo, A.S.; Dias-Ferreira, J.; Cano, A.; Zielinska, A.; Matos, C.M. Elastic and Ultradeformable Liposomes for Transdermal Delivery of Active Pharmaceutical Ingredients (APIs). Int. J. Mol. Sci. 2021, 22, 9743. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Doktorovova, S.; Zielinska, A.; Silva, A.M. Key production parameters for the development of solid lipid nanoparticles by high shear homogenization. Pharm. Dev. Technol. 2019, 24, 1181–1185. [Google Scholar] [CrossRef]
- Doktorovova, S.; Kovacevic, A.B.; Garcia, M.L.; Souto, E.B. Preclinical safety of solid lipid nanoparticles and nanostructured lipid carriers: Current evidence from in vitro and in vivo evaluation. Eur. J. Pharm. Biopharm. 2016, 108, 235–252. [Google Scholar] [CrossRef]
- Doktorovova, S.; Souto, E.B.; Silva, A.M. Nanotoxicology applied to solid lipid nanoparticles and nanostructured lipid carriers—A systematic review of in vitro data. Eur. J. Pharm. Biopharm. 2014, 87, 1–18. [Google Scholar] [CrossRef]
- Jain, S.; Patel, N.; Shah, M.K.; Khatri, P.; Vora, N. Recent Advances in Lipid-Based Vesicles and Particulate Carriers for Topical and Transdermal Application. J. Pharm. Sci. 2017, 106, 423–445. [Google Scholar] [CrossRef]
- Gelperina, S.; Kisich, K.; Iseman, M.D.; Heifets, L. The potential advantages of nanoparticle drug delivery systems in chemotherapy of tuberculosis. Am. J. Respir. Crit. Care Med. 2005, 172, 1487–1490. [Google Scholar] [CrossRef] [Green Version]
- Chantaburanan, T.; Teeranachaideekul, V.; Chantasart, D.; Jintapattanakit, A.; Junyaprasert, V.B. Effect of binary solid lipid matrix of wax and triglyceride on lipid crystallinity, drug-lipid interaction and drug release of ibuprofen-loaded solid lipid nanoparticles (SLN) for dermal delivery. J. Colloid Interface Sci. 2017, 504, 247–256. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Azadi, A.; Daneshamouz, S.; Mohammadi Samani, S. Cyproterone acetate-loaded solid lipid nanoparticles (SLNs) and nanostructured lipid carriers (NLCs): Preparation and optimization. Trends Pharm. Sci. 2017, 3, 275–286. [Google Scholar]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Potential of Nanoparticles as Permeation Enhancers and Targeted Delivery Options for Skin: Advantages and Disadvantages. Drug Des. Dev. Ther. 2020, 14, 3271–3289. [Google Scholar] [CrossRef] [PubMed]
- Abd, E.; Namjoshi, S.; Mohammed, Y.H.; Roberts, M.S.; Grice, J.E. Synergistic skin penetration enhancer and nanoemulsion formulations promote the human epidermal permeation of caffeine and naproxen. J. Pharm. Sci. 2016, 105, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Maghraby, G.M.E.; Williams, A.C.; Barry, B.W. Can drug-bearing liposomes penetrate intact skin? J. Pharm. Pharmacol. 2006, 58, 415–429. [Google Scholar] [CrossRef]
- Choi, M.; Maibach, H. Liposomes and niosomes as topical drug delivery systems. Skin Pharmacol. Physiol. 2005, 18, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Karuppuswamy, P.; Venugopal, J.R.; Navaneethan, B.; Laiva, A.L.; Sridhar, S.; Ramakrishna, S. Functionalized hybrid nanofibers to mimic native ECM for tissue engineering applications. Appl. Surf. Sci. 2014, 322, 162–168. [Google Scholar] [CrossRef]
- Bhaarathy, V.; Venugopal, J.; Gandhimathi, C.; Ponpandian, N.; Mangalaraj, D.; Ramakrishna, S. Biologically improved nanofibrous scaffolds for cardiac tissue engineering. Mater. Sci. Eng. C 2014, 44, 268–277. [Google Scholar] [CrossRef]
- Suganya, S.; Venugopal, J.; Ramakrishna, S.; Lakshmi, B.S.; Dev, V.R.G. Naturally derived biofunctional nanofibrous scaffold for skin tissue regeneration. Int. J. Biol. Macromol. 2014, 68, 135–143. [Google Scholar] [CrossRef]
- Jozala, A.F.; de Lencastre-Novaes, L.C.; Lopes, A.M.; de Carvalho Santos-Ebinuma, V.; Mazzola, P.G.; Pessoa-Jr, A.; Grotto, D.; Gerenutti, M.; Chaud, M.V. Bacterial nanocellulose production and application: A 10-year overview. Appl. Microbiol. Biotechnol. 2016, 100, 2063–2072. [Google Scholar] [CrossRef] [Green Version]
- Woo, K.M.; Jun, J.-H.; Chen, V.J.; Seo, J.; Baek, J.-H.; Ryoo, H.-M.; Kim, G.-S.; Somerman, M.J.; Ma, P.X. Nano-fibrous scaffolding promotes osteoblast differentiation and biomineralization. Biomaterials 2007, 28, 335–343. [Google Scholar] [CrossRef]
- Dickinson, L.E.; Gerecht, S. Engineered biopolymeric scaffolds for chronic wound healing. Front. Physiol. 2016, 7, 341. [Google Scholar] [CrossRef] [Green Version]
- Rošic, R.; Pelipenko, J.; Kristl, J.; Kocbek, P.; Baumgartner, S. Properties, engineering and applications of polymeric nanofibers: Current research and future advances. Chem. Biochem. Eng. Q. 2012, 26, 417–425. [Google Scholar]
- Kwon, I.K.; Kidoaki, S.; Matsuda, T. Electrospun nano-to microfiber fabrics made of biodegradable copolyesters: Structural characteristics, mechanical properties and cell adhesion potential. Biomaterials 2005, 26, 3929–3939. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Kotaki, M.; Inai, R.; Ramakrishna, S. Potential of nanofiber matrix as tissue-engineering scaffolds. Tissue Eng. 2005, 11, 101–109. [Google Scholar] [CrossRef]
- Turssi, C.P.; Ferracane, J.L.; Ferracane, L.L. Wear and fatigue behavior of nano-structured dental resin composites. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 78, 196–203. [Google Scholar] [CrossRef]
- Jung, M.; Sehr, K.; Klimek, J. Surface texture of four nanofilled and one hybrid composite after finishing. Oper. Dent. 2007, 32, 45–52. [Google Scholar] [CrossRef]
- Ergücü, Z.; Türkün, L.S.; Aladag, A. Color stability of nanocomposites polished with one-step systems. Oper. Dent. 2008, 33, 413–420. [Google Scholar] [CrossRef] [Green Version]
- Gaber, M.; Medhat, W.; Hany, M.; Saher, N.; Fang, J.-Y.; Elzoghby, A. Protein-lipid nanohybrids as emerging platforms for drug and gene delivery: Challenges and outcomes. J. Control. Release 2017, 254, 75–91. [Google Scholar] [CrossRef] [PubMed]



| Dressing Type | Definition | Main Characteristics | Advantages | Examples (References) |
|---|---|---|---|---|
| Alginate | Dressings made of calcium alginate, an anionic polysaccharide produced from brown seaweed | Calcium ions from dressing are exchanged with sodium ions from wound environment, forming a gel | Can absorb 15–20 times their weight in fluids; can be removed intact; considered long-term dressing | Release of therapeutic proteins [82]; containing chlorhexidine hexametaphosphate nanoparticles [83]; Sulfide-releasing property [84] |
| Films | Semipermeable dressings made from polyurethane and coated with an acrylic derivative adhesive | Transparent, gas and water vapour permeable | Allow easy wound monitoring (transparent dressing); can be changed only when necessary and removing cause simple and small trauma in wound region | Electroactive shape memory polyurethane-urea films [85] |
| Foams | Composed of polyurethane or silicone with a semi-occlusive outer layer | Outer layer is permeable to water vapour and serves as barrier for microorganisms’ infection, polyurethane center absorbs exudate | Able to create or maintain a moist environment; easy and nom-traumatic removal; can absorb and retain wound exudate | Hemostatic polyurethane-urea foams [86] |
| Hydrocolloids | Crosslinked polymer matrices with integrated adhesives and starches, such as cellulose, gelatin, pectin and guar | Occlusive and adhesive dressing, which form a gel upon contact with wound exudate, permeable to water vapour, allow debridement | Form gels in contact with wound exudate; capacity to promote wound debridement; long wear-time | Centella asiatica loaded hydrocolloid based on sodium alginate [60] |
| Hydrofiber | Contain carboxymethyl cellulose formed into textile fibers | Highly absorbent fibers, form gels upon exudate absorption, allow autolytic debridement | Can absorb 25 times its own weight; form gel when in contact with wound exudate; encourage autolytic debridement | Hydrofiber dressing with silver [78] |
| Hydrogels | Water-based products, designed as polymeric networks, comprised of up to 96% water | Clear to transparent, capable to absorb biological fluids, permeable to water and oxygen | Allow easy wound monitoring (transparent dressing); capable of absorbing biological fluids; maintain the area moisturized; promotes autolytic debridement; help cell proliferation and epithelization process; minimal or null trauma in their removal; permeable to water and oxygen | Hydrogels of PNIPAAm-co-Aam to release bromelain [87]; triple polymer hydrogel (chitosan, gelatin and PVA) loaded with moxifloxacin [88] |
| Nanotechnology-Based System | Description | Material | Active Loaded | Preparation Process | Study Type (References) |
|---|---|---|---|---|---|
| Nanoparticles | Inorganic nanoparticles | Silver and gold | None | Phytochemical assisted thermal reduction | In vivo [92] |
| Silver | None | Phytochemical assisted thermal reduction | In vitro [93] and in vivo [94] | ||
| Zinc oxide | None | Room temperature synthesis and solvothermal synthesis | In vitro [95] | ||
| Polymeric nanoparticles | Chitosan | Silver sulfadiazine | Ionotropic gelation | In vitro [96] | |
| Bromelain | Ionotropic gelation | In vitro [97,98,99] | |||
| Solid lipid nanoparticles | Poloxamer 188 and tristearin | Propolis | Stirring followed by ultrasonication | In vitro and in vivo [100] | |
| Polymeric nanofiber | Composite bilayer film | Polyvinyl alcohol (PVA) and gelatin/chitosan/polyethylene glycol (PEG) blend | None | solution casting and crosslinking agent | In vitro [66] |
| Membrane | Bacterial nanocellulose | Bromelain | Bacterial cultivation | In vitro [12] | |
| Nisin | Bacterial cultivation | In vitro [101,102] | |||
| Nanofiber | Polylactic-co-glycolic acid (PLGA) | Recombinant human epidermal growth factor and Aloe vera extract | Electrospinning | In vitro and in vivo [17] | |
| Polyvinyl alcohol (PVA) and tamarind seed gum | Clindamycin | Electrospinning | In vitro [103,104] | ||
| Nanohybrids | Hydrogel and nanoparticles | Alginate and gellatin hydrogel | Silver nanoparticles | Homogenization with mechanical stirrer | In vitro and in vivo [105] |
| Chitosan hydrogel | Zinc oxide nanoparticles | Nanoparticles: reduction with NaOH Hydrogel: pH change of chitosan solution Nanohydrid: homogeneization of NP and hydrogels followed by freeze-drying | In vitro and in vivo [106] | ||
| β-chitin hydrogel | Zinc oxide nanoparticles | Nanoparticles: reduction with NaOH Hydrogel: crosslink with CaCl2 Nanohydrid: homogeneization of NP and hydrogels followed by freeze-drying | In vitro and in vivo [107] | ||
| Polyvinyl alcohol (PVA) and chitosan | Zinc oxide nanoparticles | Freeze-thaw method | In vitro [108] | ||
| Chitosan and Bletilla striata polysaccharide | Chitosan-Ag nanoparticles | Hydrogel sponge: homogeneization followed by freeze-drying Nanoparticles: reduction followed by freeze-drying Nanohybrid: nanoparticles were crosslinked with genipin and frozen, followed by freeze-drying with sponges | In vitro and in vivo [56] | ||
| Membranes and nanoparticles | Bacterial nanocellulose membranes | Zinc oxide nanoparticles | Membranes: bacterial cultivation Nanohybrid: impregnation of ZnO NP | In vitro and in vivo [109] | |
| Bacterial nanocellulose | Silver nanoparticles | Membranes: bacterial cultivation Nanoparticles: silver nitrate reduction with sodium borohydride Nanohybrid: impregnation of silver nitrate | In vitro [110] | ||
| Nanofiber and nanoparticles | Polycaprolactone nanofibers | Zinc oxide nanoparticles | Electrospinning | In vitro [111] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ataide, J.A.; Zanchetta, B.; Santos, É.M.; Fava, A.L.M.; Alves, T.F.R.; Cefali, L.C.; Chaud, M.V.; Oliveira-Nascimento, L.; Souto, E.B.; Mazzola, P.G. Nanotechnology-Based Dressings for Wound Management. Pharmaceuticals 2022, 15, 1286. https://0-doi-org.brum.beds.ac.uk/10.3390/ph15101286
Ataide JA, Zanchetta B, Santos ÉM, Fava ALM, Alves TFR, Cefali LC, Chaud MV, Oliveira-Nascimento L, Souto EB, Mazzola PG. Nanotechnology-Based Dressings for Wound Management. Pharmaceuticals. 2022; 15(10):1286. https://0-doi-org.brum.beds.ac.uk/10.3390/ph15101286
Chicago/Turabian StyleAtaide, Janaína A., Beatriz Zanchetta, Érica M. Santos, Ana Laura M. Fava, Thais F. R. Alves, Letícia C. Cefali, Marco V. Chaud, Laura Oliveira-Nascimento, Eliana B. Souto, and Priscila G. Mazzola. 2022. "Nanotechnology-Based Dressings for Wound Management" Pharmaceuticals 15, no. 10: 1286. https://0-doi-org.brum.beds.ac.uk/10.3390/ph15101286