A Comprehensive Grading System for a Magnetic Sentinel Lymph Node Biopsy Procedure in Head and Neck Cancer Patients
Abstract
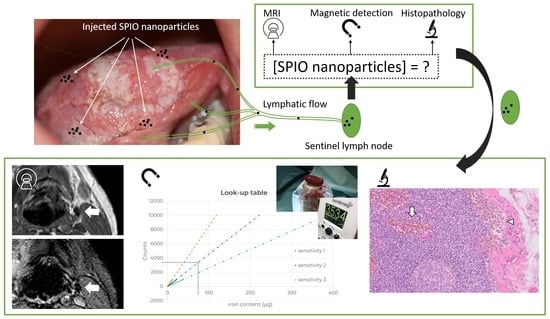
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Magnetic Resonance Imaging Grading
- T1-weighted (T1w) 3D fast field echo (TR/TE = 25/4.6 ms, flip angle 30°, voxel size 0.75 mm × 0.75 mm × 1.6 mm, FOV = 251–269);
- T2*-weighted (T2*w) fast field echo (TR/TE = 1700/18.41 ms, flip angle 18°, voxel size 0.62 mm × 0.62 mm × 3 mm, FOV = 247–267).
- 1: Internal spots of signal void
- 2: Confluence of internal spots of signal void, <25%
- 3: Partial (peripheral) signal void of the node, 25–75%
- 4: Complete signal void of the node, >75%
- 5: Blooming beyond border of the gland
2.2. Amount of Iron in Sentinel Lymph Nodes
2.3. Histopathology Grading
2.4. Data Analysis
3. Results
3.1. Magnetic Resonance Imaging Grading
3.2. Amount of Iron in Sentinel Lymph Nodes
3.3. Histopathology Grading
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Pt nr. | Tumor Stage | Total LNs | Injected Iron Dose (mg) | Interval | SLN nr. | Neck Level | Iron Content SLN (µg) | Cortical Grade | Medullar Grade | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I-MRI1 (hh:mm) | I-SLNB (hh:mm) | I-MRI2 (hh) | |||||||||
| 1 | cT2 | 29 | 22.4 | 00:24 | 15:57 | 672 | 1 | II | 116 | 1 | 3 |
| 2 | I | 51 | 1 | 4 | |||||||
| 3 | I | 124 | 3 | 3 | |||||||
| 4 | III | 37 | 2 | 3 | |||||||
| 5 & 6 1 | I 2 | 16 | 0 | 0 | |||||||
| 2 | cT1 | 32 | 22.4 | 00:22 | 16:31 | 672 | 1 | II | 95 | 2 | 4 |
| 2 | II | 80 | 2 | 4 | |||||||
| 3 | III | 121 | 4 | 4 | |||||||
| 4 | III | 183 | 4 | 4 | |||||||
| 3 | cT2 | 19 | 22.4 | 00:58 | 16:53 | 1009 | 1 | II | 30 | 1 | 4 |
| 2 | II | 227 | 2 | 4 | |||||||
| 3 | II | 22 | 2 | 3 | |||||||
| 4 | II | 35 | 4 | 4 | |||||||
| 5 3 | II | 59 | 2 | 4 | |||||||
| 6 | I | 64 | 3 | 4 | |||||||
| 4 | cT2 | 11 | 22.4 | 00:24 | 21:14 | 1176 | 1 | I | 32 | 3 | 2 |
| 2 | I | 115 | 1 | 4 | |||||||
| 5 | cT1 | 11 | 22.4 | 00:38 | 21:07 | 841 | 1 | II | 57 | 1 | 2 |
| 6 | cT1 | 4 | 11.2 | 01:41 | 05:17 | 561 | 1 | II | 136 | 3 | 4 |
| 7 | cT2 | 20 | 11.2 | 01:20 | 18:07 | 841 | 1 3 | II | 59 | 1 | 4 |
| 2 | II | 187 | 2 | 4 | |||||||
| 3 | I | 26 | 1 | 2 | |||||||
| 4 | I | 26 | 2 | 3 | |||||||
| 8 | cT1 | 25 | 11.2 | 01:09 | 04:06 | 656 | 1 3 | II | 82 | 2 | 2 |
References
- Gourin, C.; Conger, B.; Porubsky, E.; Sheils, W.; Bilodeau, P.; Coleman, T. The effect of occult nodal metastases on survival and regional control in patients with head and neck squamous cell carcinoma. Laryngoscope 2008, 118, 1191–1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Zinis, L.O.R.; Bolzoni, A.; Piazza, C.; Nicolai, P. Prevalence and localization of nodal metastases in squamous cell carcinoma of the oral cavity: Role and extension of neck dissection. Eur. Arch. Oto-Rhino-Laryngol. Head Neck 2006, 263, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- Giammarile, F.; Schilling, C.; Gnanasegaran, G.; Bal, C.; Oyen, W.J.G.; Rubello, D.; Schwarz, T.; Tartaglione, G.; Miller, R.N.; Paez, D.; et al. The EANM practical guidelines for sentinel lymph node localisation in oral cavity squamous cell carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 623–637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, J.; Candela, F.; Poddar, A. The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer 1990, 66, 109–113. [Google Scholar] [CrossRef]
- Thompson, C.F.; St. John, M.A.; Lawson, G.; Grogan, T.; Elashoff, D.; Mendelsohn, A.H. Diagnostic value of sentinel lymph node biopsy in head and neck cancer: A meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 2115–2122. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Wang, S.J.; Yang, X.; Peng, H. Diagnostic efficacy of sentinel lymph node biopsy in early oral squamous cell carcinoma: A meta-analysis of 66 studies. PLoS ONE 2017, 12, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Schilling, C.; Stoeckli, S.J.; Vigili, M.G.; de Bree, R.; Lai, S.Y.; Alvarez, J.; Christensen, A.; Cognetti, D.M.; D’Kruz, A.K.; Frerich, B.; et al. Surgical consensus guidelines on sentinel node biopsy (SNB) in patients with oral cancer. Head Neck 2019, 41, 2655–2664. [Google Scholar] [CrossRef]
- de Bree, R.; de Keizer, B.; Civantos, F.J.; Takes, R.P.; Rodrigo, J.P.; Hernandez-Prera, J.C.; Halmos, G.B.; Rinaldo, A.; Ferlito, A. What is the role of sentinel lymph node biopsy in the management of oral cancer in 2020? Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 3181–3191. [Google Scholar] [CrossRef]
- Johnson, C.B.; Boneti, C.; Korourian, S.; Adkins, L.; Klimberg, V.S. Intraoperative injection of subareolar or dermal radioisotope results in predictable identification of sentinel lymph nodes in breast cancer. Ann. Surg. 2011, 254, 612–618. [Google Scholar] [CrossRef]
- Zada, A.; Peek, M.C.L.; Ahmed, M.; Anninga, B.; Baker, R.; Kusakabe, M.; Sekino, M.; Klaase, J.M.; ten Haken, B.; Douek, M. Meta-analysis of sentinel lymph node biopsy in breast cancer using the magnetic technique. Br. J. Surg. 2016, 103, 1409–1419. [Google Scholar] [CrossRef]
- Alvarado, M.D.; Mittendorf, E.A.; Teshome, M.; Thompson, A.M.; Bold, R.J.; Gittleman, M.A.; Beitsch, P.D.; Blair, A.L.; Kivilaid, K.; Harmer, Q.J.; et al. SentimagIC: A Non-inferiority Trial Comparing Superparamagnetic Iron Oxide Versus Technetium-99m and Blue Dye in the Detection of Axillary Sentinel Nodes in Patients with Early-Stage Breast Cancer. Ann. Surg. Oncol. 2019, 26, 3510–3516. [Google Scholar] [CrossRef] [PubMed]
- Winter, A.; Woenkhaus, J.; Wawroschek, F. A novel method for intraoperative sentinel lymph node detection in prostate cancer patients using superparamagnetic iron oxide nanoparticles and a handheld magnetometer: The initial clinical experience. Ann. Surg. Oncol. 2014, 21, 4390–4396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baena Fustegueras, J.A.; Gonzalez, F.H.; Caldero, S.G.; de la Fuente Juarez, M.C.; Lopez, S.R.; Riu, F.R.; Mestres Petit, N.; Álvarez, P.M.; Lecube Torelló, A.; Matias-Guiu, X.; et al. Magnetic detection of sentinel lymph node in papillary thyroid carcinoma: The MAGIC-PAT study results. Eur. J. Surg. Oncol. 2019, 45, 1175–1181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernando, J.; Aguirre, P.; Aguilar-Salvatierra, A.; Leizaola-Cardesa, I.O.; Bidaguren, A.; Gomez-Moreno, G. Magnetic detection of sentinel nodes in oral squamous cell carcinoma by means of superparamagnetic iron oxide contrast. J. Surg. Oncol. 2019, 121, 244–248. [Google Scholar] [CrossRef]
- Nieuwenhuis, E.R.; Kolenaar, B.; van Bemmel, A.J.M.; Hof, J.J.; van Baarlen, J.; Christenhusz, A.; Pouw, J.J.; ten Haken, B.; Alic, L.; de Bree, R. A complete magnetic sentinel lymph node biopsy procedure in oral cancer patients: A pilot study. Oral Oncol. 2021, 121, 105464. [Google Scholar] [CrossRef]
- Mizokami, D.; Kosuda, S.; Tomifuji, M.; Araki, K.; Yamashita, T.; Shinmoto, H.; Shiotani, A. Superparamagnetic iron oxide-enhanced interstitial magnetic resonance lymphography to detect a sentinel lymph node in tongue cancer patients. Acta Otolaryngol. 2013, 133, 418–423. [Google Scholar] [CrossRef]
- Mahieu, R.; de Maar, J.S.; Nieuwenhuis, E.R.; Deckers, R.; Moonen, C.; Alic, L.; ten Haken, B.; de Keizer, B.; de Bree, R. New developments in imaging for sentinel lymph node biopsy in early-stage oral cavity squamous cell carcinoma. Cancers 2020, 12, 3055. [Google Scholar] [CrossRef]
- Winter, A.; Kowald, T.; Engels, S.; Wawroschek, F. Magnetic resonance sentinel lymph node imaging and magnetometer-guided intraoperative detection in prostate cancer using superparamagnetic iron oxide nanoparticles. Int. J. Nanomed. 2018, 13, 6689–6698. [Google Scholar] [CrossRef] [Green Version]
- Aribal, E.; Çelik, L.; Yilmaz, C.; Demirkiran, C.; Guner, D.C. Effects of iron oxide particles on MRI and mammography in breast cancer patients after a sentinel lymph node biopsy with paramagnetic tracers. Clin. Imaging 2021, 75, 22–26. [Google Scholar] [CrossRef]
- Nieuwenhuis, E.R.; Christenhusz, A.; Alic, L. Look-up table (LUT) for Sentimag and Sienna, relation between magnetic readout (counts) and iron content. 4TU.ResearchData 2021. [Google Scholar] [CrossRef]
- Byers, R.M.; Wolf, P.F.; Ballantyne, A.J. Rationale for Elective Modified. Head Neck Surg. 1988, 10, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Tartaglione, G.; Stoeckli, S.J.; de Bree, R.; Schilling, C.; Flach, G.B.; Bakholdt, V.; Sorensen, J.A.; Bilde, A.; von Buchwald, C.; Lawson, G.; et al. Sentinel node in oral cancer: The nuclear medicine aspects. A survey from the sentinel European node trial. Clin. Nucl. Med. 2016, 41, 534–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Den Toom, I.J.; Mahieu, R.; van Rooij, R.; van Es, R.J.J.; Hobbelink, M.G.G.; Krijger, G.C.; Tijink, B.M.; de Keizer, B.; de Bree, R. Sentinel lymph node detection in oral cancer: A within-patient comparison between [99mTc]Tc-tilmanocept and [99mTc]Tc-nanocolloid. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Sekino, M.; Kuwahata, A.; Ookubo, T.; Shiozawa, M.; Ohashi, K.; Kaneko, M.; Saito, I.; Inoue, Y.; Ohsaki, H.; Takei, H.; et al. Handheld magnetic probe with permanent magnet and Hall sensor for identifying sentinel lymph nodes in breast cancer patients. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Waddington, W.A.; Keshtgar, M.R.S.; Taylor, I.; Lakhani, S.R.; Short, M.D.; Ell, P.J. Original article Radiation safety of the sentinel lymph node technique in breast cancer. Eur. J. Nucl. Med. 2000, 27, 377–391. [Google Scholar] [CrossRef]
- Mirzaei, N.; Katsarelias, D.; Zaar, P.; Johansson, I.; Leonhardt, H.; Wärnberg, F.; Olofsson Bagge, R. Sentinel lymph node localization and staging with a low-dose of superparamagnetic iron oxide (SPIO) enhanced MRI and magnetometer in patients with cutaneous melanoma of the extremity-The MAGMEN feasibility study. Eur. J. Surg. Oncol. 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Anninga, B.; Ahmed, M.; Van Hemelrijck, M.; Pouw, J.J.; Westbroek, D.; Pinder, S.; ten Haken, B.; Pankhurst, Q.; Douek, M. Magnetic sentinel lymph node biopsy and localization properties of a magnetic tracer in an in vivo porcine model. Breast Cancer Res. Treat. 2013, 141, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Houpeau, J.-L.; Chauvet, M.-P.; Guillemin, F.; Bendavid-Athias, C.; Charitansky, H.; Kramar, A.; Giard, S. Sentinel lymph node identification using superparamagnetic iron oxide particles versus radioisotope: The French Sentimag feasibility trial. J. Surg. Oncol 2016, 113, 501–507. [Google Scholar] [CrossRef]
- Atula, T.; Shoaib, T.; Ross, G.L.; Gray, H.W.; Soutar, D.S. How many sentinel nodes should be harvested in oral squamous cell carcinoma? Eur. Arch. Oto-Rhino-Laryngol. 2008, 265, 19–23. [Google Scholar] [CrossRef] [Green Version]
- Pouw, J.J.; Ahmed, M.; Anninga, B.; Schuurman, K.; Pinder, S.E.; van Hemelrijck, M.; Pankhurst, Q.A.; Douek, M.; ten Haken, B. Comparison of three magnetic nanoparticle tracers for sentinel lymph node biopsy in an in vivo porcine model. Int. J. Nanomed. 2015, 10, 1235–1243. [Google Scholar] [CrossRef] [Green Version]
- Schauer, A.J.; Becker, W.; Reiser, M.; Possinger, K. Specific developments in sentinel node labeling using 99mTc-colloids. In The Sentinel Lymph Node Concept; Heilmann, U., McHugh, W., Pfaff, U., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 59–69. [Google Scholar]
- Johnson, L.; Pinder, S.E.; Douek, M. Deposition of superparamagnetic iron-oxide nanoparticles in axillary sentinel lymph nodes following subcutaneous injection. Histopathology 2013, 62, 481–486. [Google Scholar] [CrossRef] [PubMed]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nieuwenhuis, E.R.; Kolenaar, B.; Hof, J.J.; van Baarlen, J.; van Bemmel, A.J.M.; Christenhusz, A.; Scheenen, T.W.J.; ten Haken, B.; de Bree, R.; Alic, L. A Comprehensive Grading System for a Magnetic Sentinel Lymph Node Biopsy Procedure in Head and Neck Cancer Patients. Cancers 2022, 14, 678. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14030678
Nieuwenhuis ER, Kolenaar B, Hof JJ, van Baarlen J, van Bemmel AJM, Christenhusz A, Scheenen TWJ, ten Haken B, de Bree R, Alic L. A Comprehensive Grading System for a Magnetic Sentinel Lymph Node Biopsy Procedure in Head and Neck Cancer Patients. Cancers. 2022; 14(3):678. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14030678
Chicago/Turabian StyleNieuwenhuis, Eliane R., Barry Kolenaar, Jurrit J. Hof, Joop van Baarlen, Alexander J. M. van Bemmel, Anke Christenhusz, Tom W. J. Scheenen, Bernard ten Haken, Remco de Bree, and Lejla Alic. 2022. "A Comprehensive Grading System for a Magnetic Sentinel Lymph Node Biopsy Procedure in Head and Neck Cancer Patients" Cancers 14, no. 3: 678. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14030678