Elevated Plasma Levels of Mature Brain-Derived Neurotrophic Factor in Major Depressive Disorder Patients with Higher Suicidal Ideation
Abstract
:1. Introduction
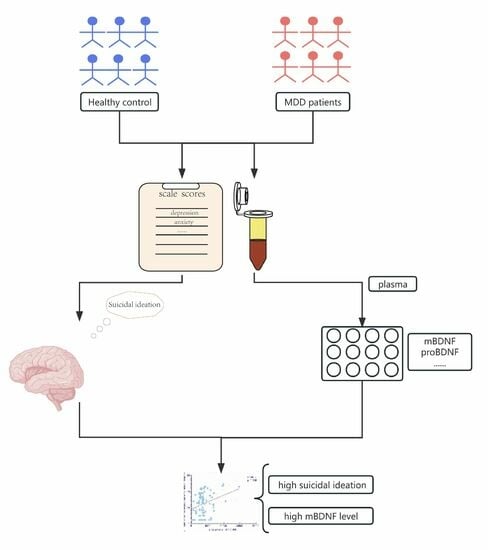
2. Materials and Methods
2.1. Subjects
2.2. Symptom Assessment
2.3. Measurements
2.4. Data Analysis
2.5. Ethics
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Increased mBDNF in MDD Patients with High and Low Suicidal Ideation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vahia, I.V.; Jeste, D.V.; Reynolds, C.F., 3rd. Older Adults and the Mental Health Effects of COVID-19. JAMA 2020, 324, 2253. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed]
- Depression and Other Common Mental Disorders; WHO: Geneva, Switzerland, 2017; p. 24.
- Malhi, G.S.; Mann, J.J. Depression. Lancet 2018, 392, 2299–2312. [Google Scholar] [CrossRef]
- Fazel, S.; Runeson, B. Suicide. N. Engl. J. Med. 2020, 382, 266–274. [Google Scholar] [CrossRef] [PubMed]
- De Vincenti, A.P.; Ríos, A.S.; Paratcha, G.; Ledda, F. Mechanisms That Modulate and Diversify BDNF Functions: Implications for Hippocampal Synaptic Plasticity. Front. Cell. Neurosci. 2019, 13, 135. [Google Scholar] [CrossRef]
- Binder, D.K.; Scharfman, H.E. Brain-derived neurotrophic factor. Growth Factors 2004, 22, 123–131. [Google Scholar] [CrossRef]
- Deinhardt, K.; Chao, M.V. Shaping neurons: Long and short range effects of mature and proBDNF signalling upon neuronal structure. Neuropharmacology 2013, 76, 603–609. [Google Scholar] [CrossRef]
- Numakawa, T.; Suzuki, S.; Kumamaru, E.; Adachi, N.; Richards, M.; Kunugi, H. BDNF function and intracellular signaling in neurons. Histol. Histopathol. 2010, 25, 237–258. [Google Scholar]
- Behl, T.; Rana, T.; Alotaibi, G.H.; Shamsuzzaman, M.; Naqvi, M.; Sehgal, A.; Singh, S.; Sharma, N.; Almoshari, Y.; Abdellatif, A.A.; et al. Polyphenols inhibiting MAPK signalling pathway mediated oxidative stress and inflammation in depression. Biomed. Pharmacother. 2022, 146, 112545. [Google Scholar] [CrossRef]
- Rana, T.; Behl, T.; Sehgal, A.; Singh, S.; Sharma, N.; Abdeen, A.; Ibrahim, S.F.; Mani, V.; Iqbal, M.S.; Bhatia, S.; et al. Exploring the role of neuropeptides in depression and anxiety. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2021, 114, 110478. [Google Scholar] [CrossRef]
- Teng, K.K.; Felice, S.; Kim, T.; Hempstead, B.L. Understanding proneurotrophin actions: Recent advances and challenges. Dev. Neurobiol. 2010, 70, 350–359. [Google Scholar] [CrossRef]
- Chen, L.; Li, X.-S.; Zheng, G.-E.; Xie, G.-J.; Cheng, Y. Peripheral blood BDNF-TrkB signaling in first-episode, drug-free patients with major depressive disorder and schizophrenia. Neurosci. Lett. 2019, 714, 134618. [Google Scholar] [CrossRef]
- Molendijk, M.L.; Spinhoven, P.; Polak, M.; Bus, B.A.A.; Penninx, B.W.J.H.; Elzinga, B.M. Serum BDNF concentrations as peripheral manifestations of depression: Evidence from a systematic review and meta-analyses on 179 associations (N = 9484). Mol. Psychiatry 2013, 19, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Elfving, B.; Buttenschøn, H.N.; Foldager, L.; Poulsen, P.H.; Andersen, J.H.; Grynderup, M.B.; Hansen, M.; Kolstad, H.A.; Kaerlev, L.; Mikkelsen, S.; et al. Depression, the Val66Met polymorphism, age, and gender influence the serum BDNF level. J. Psychiatr. Res. 2012, 46, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Skibinska, M.; Groszewska, A.; Kapelski, P.; Rajewska-Rager, A.; Pawlak, J.; Dmitrzak-Weglarz, M.; Szczepankiewicz, A.; Twarowska-Hauser, J. Val66Met functional polymorphism and serum protein level of brain-derived neurotrophic factor (BDNF) in acute episode of schizophrenia and depression. Pharmacol. Rep. 2018, 70, 55–59. [Google Scholar] [CrossRef]
- Ryan, K.M.; Dunne, R.; McLoughlin, D.M. BDNF plasma levels and genotype in depression and the response to electroconvulsive therapy. Brain Stimul. 2018, 11, 1123–1131. [Google Scholar] [CrossRef]
- Yoshida, T.; Ishikawa, M.; Niitsu, T.; Nakazato, M.; Watanabe, H.; Shiraishi, T.; Shiina, A.; Hashimoto, T.; Kanahara, N.; Hasegawa, T.; et al. Decreased Serum Levels of Mature Brain-Derived Neurotrophic Factor (BDNF), but Not Its Precursor proBDNF, in Patients with Major Depressive Disorder. PLoS ONE 2012, 7, e42676. [Google Scholar] [CrossRef]
- Gelle, T.; Samey, R.A.; Plansont, B.; Bessette, B.; Jauberteau-Marchan, M.-O.; Lalloué, F.; Girard, M. BDNF and pro-BDNF in serum and exosomes in major depression: Evolution after antidepressant treatment. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2020, 109, 110229. [Google Scholar] [CrossRef]
- Maes, M. Evidence for an immune response in major depression: A review and hypothesis. Prog. Neuro Psychopharmacol. Biol. Psychiatry 1995, 19, 11–38. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.H.; Raison, C.L. The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 2015, 16, 22–34. [Google Scholar] [CrossRef]
- Beurel, E.; Toups, M.; Nemeroff, C.B. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron 2020, 107, 234–256. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Willemsen, G.; Owen, N.; Flower, L.; Mohamed-Ali, V. Acute mental stress elicits delayed increases in circulating inflammatory cytokine levels. Clin. Sci. 2001, 101, 185–192. [Google Scholar] [CrossRef]
- Grippo, A.J.; Sullivan, N.R.; Damjanoska, K.J.; Crane, J.W.; Carrasco, G.A.; Shi, J.; Chen, Z.; Garcia, F.; Muma, N.A.; van de Kar, L.D. Chronic mild stress induces behavioral and physiological changes, and may alter serotonin 1A receptor function, in male and cycling female rats. Psychopharmacology 2004, 179, 769–780. [Google Scholar] [CrossRef] [PubMed]
- You, Z.; Luo, C.; Zhang, W.; Chen, Y.; He, J.; Zhao, Q.; Zuo, R.; Wu, Y. Pro- and anti-inflammatory cytokines expression in rat’s brain and spleen exposed to chronic mild stress: Involvement in depression. Behav. Brain Res. 2011, 225, 135–141. [Google Scholar] [CrossRef]
- Liu, W.; Sheng, H.; Xu, Y.; Liu, Y.; Lu, J.; Ni, X. Swimming exercise ameliorates depression-like behavior in chronically stressed rats: Relevant to proinflammatory cytokines and IDO activation. Behav. Brain Res. 2013, 242, 110–116. [Google Scholar] [CrossRef]
- Bartolomucci, A.; Palanza, P.; Sacerdote, P.; Ceresini, G.; Chirieleison, A.; Panerai, A.; Parmigiani, S. Individual housing induces altered immuno-endocrine responses to psychological stress in male mice. Psychoneuroendocrinology 2002, 28, 540–558. [Google Scholar] [CrossRef]
- Möller, M.; Du Preez, J.L.; Viljoen, F.P.; Berk, M.; Emsley, R.; Harvey, B.H. Social isolation rearing induces mitochondrial, immunological, neurochemical and behavioural deficits in rats, and is reversed by clozapine or N-acetyl cysteine. Brain Behav. Immun. 2013, 30, 156–167. [Google Scholar] [CrossRef]
- Chourbaji, S.; Urani, A.; Inta, I.; Sanchis-Segura, C.; Brandwein, C.; Zink, M.; Schwaninger, M.; Gass, P. IL-6 knockout mice exhibit resistance to stress-induced development of depression-like behaviors. Neurobiol. Dis. 2006, 23, 587–594. [Google Scholar] [CrossRef]
- Song, C.; Zhang, X.Y.; Manku, M. Increased Phospholipase A2 Activity and Inflammatory Response But Decreased Nerve Growth Factor Expression in the Olfactory Bulbectomized Rat Model of Depression: Effects of Chronic Ethyl-Eicosapentaenoate Treatment. J. Neurosci. 2009, 29, 14–22. [Google Scholar] [CrossRef]
- Gómez-Lázaro, E.; Arregi, A.; Beitia, G.; Vegas, O.; Azpiroz, A.; Garmendia, L. Individual differences in chronically defeated male mice: Behavioral, endocrine, immune, and neurotrophic changes as markers of vulnerability to the effects of stress. Stress 2011, 14, 537–548. [Google Scholar] [CrossRef]
- Patki, G.; Solanki, N.; Atrooz, F.; Allam, F.; Salim, S. Depression, anxiety-like behavior and memory impairment are associated with increased oxidative stress and inflammation in a rat model of social stress. Brain Res. 2013, 1539, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Yu, H.-Y.; Shen, X.-F.; Gao, Z.-Q.; Yang, C.; Yang, J.-J.; Zhang, G.-F. The rapid antidepressant effect of ketamine in rats is associated with down-regulation of pro-inflammatory cytokines in the hippocampus. Upsala J. Med. Sci. 2015, 120, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Young, J.J.; Bruno, D.; Pomara, N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J. Affect. Disord. 2014, 169, 15–20. [Google Scholar] [CrossRef]
- Raison, C.L.; Borisov, A.S.; Majer, M.; Drake, D.F.; Pagnoni, G.; Woolwine, B.J.; Vogt, G.J.; Massung, B.; Miller, A.H. Activation of Central Nervous System Inflammatory Pathways by Interferon-Alpha: Relationship to Monoamines and Depression. Biol. Psychiatry 2009, 65, 296–303. [Google Scholar] [CrossRef]
- Raison, C.L.; Capuron, L.; Miller, A.H. Cytokines sing the blues: Inflammation and the pathogenesis of depression. Trends Immunol. 2006, 27, 24–31. [Google Scholar] [CrossRef]
- Goldsmith, D.R.; Rapaport, M.H.; Miller, B.J. A meta-analysis of blood cytokine network alterations in psychiatric patients: Comparisons between schizophrenia, bipolar disorder and depression. Mol. Psychiatry 2016, 21, 1696–1709. [Google Scholar] [CrossRef] [PubMed]
- Köhler, C.A.; Freitas, T.H.; Maes, M.; De Andrade, N.Q.; Liu, C.S.; Fernandes, B.S.; Stubbs, B.; Solmi, M.; Veronese, N.; Herrmann, N.; et al. Peripheral cytokine and chemokine alterations in depression: A meta-analysis of 82 studies. Acta Psychiatr. Scand. 2017, 135, 373–387. [Google Scholar] [CrossRef]
- Ng, A.; Tam, W.W.; Zhang, M.W.; Ho, C.S.; Husain, S.F.; McIntyre, R.S.; Ho, R.C. IL-1β, IL-6, TNF- α and CRP in Elderly Patients with Depression or Alzheimer’s disease: Systematic Review and Meta-Analysis. Sci. Rep. 2018, 8, 12050. [Google Scholar] [CrossRef]
- Valkanova, V.; Ebmeier, K.P.; Allan, C.L. CRP, IL-6 and depression: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2013, 150, 736–744. [Google Scholar] [CrossRef]
- Desseilles, M.; Perroud, N.; Guillaume, S.; Jaussent, I.; Genty, C.; Malafosse, A.; Courtet, P. Is it valid to measure suicidal ideation by depression rating scales? J. Affect. Disord. 2012, 136, 398–404. [Google Scholar] [CrossRef]
- Li, H.; Lu, J.; Li, S.; Huang, B.; Shi, G.; Mou, T.; Xu, Y. Increased Hypocretin (Orexin) Plasma Level in Depression, Bipolar Disorder Patients. Front. Psychiatry 2021, 12, 676336. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Manual for the Beck Scale for Suicide Ideation; Psychological Corporation: San Antonio, TX, USA, 1991. [Google Scholar]
- de Beurs, D.P.; Fokkema, M.; de Groot, M.H.; de Keijser, J.; Kerkhof, A.J. Longitudinal measurement invariance of the Beck Scale for Suicide Ideation. Psychiatry Res. 2015, 225, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.T., Jr.; McCrae, R.R. Domains and facets: Hierarchical personality assessment using the revised NEO personality inventory. J. Pers. Assess. 1995, 64, 21–50. [Google Scholar] [CrossRef] [PubMed]
- Schutter, N.; Koorevaar, L.; Holwerda, T.J.; Stek, M.L.; Dekker, J.; Comijs, H.C. ‘Big Five’ personality characteristics are associated with loneliness but not with social network size in older adults, irrespective of depression. Int. Psychogeriatr. 2020, 32, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Bostwick, J.M.; Pankratz, V.S.; Levenson, J.L.; Young, R.C.; Mulsant, B.H.; Sajatovic, M.; Gildengers, A.G.; Gyulai, L.; Al Jurdi, R.K.; Beyer, J.; et al. Affective Disorders and Suicide Risk: A Reexamination. Am. J. Psychiatry 2000, 157, 1925–1932. [Google Scholar] [CrossRef]
- Osby, U.; Brandt, L.; Correia, N.; Ekbom, A.; Sparén, P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch. Gen. Psychiatry 2001, 58, 844–850. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Dilsaver, S.C. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other axis I disorders. Biol. Psychiatry 1996, 39, 896–899. [Google Scholar] [CrossRef]
- Eisen, R.B.; Perera, S.; Banfield, L.; Anglin, R.; Minuzzi, L.; Samaan, Z. Association between BDNF levels and suicidal behaviour: A systematic review and meta-analysis. Syst. Rev. 2015, 4, 187. [Google Scholar] [CrossRef]
- Grah, M.; Mihanovic, M.; Ruljancic, N.; Restek-Petrovic, B.; Molnar, S.; Jelavic, S. Brain-derived neurotrophic factor as a suicide factor in mental disorders. Acta Neuropsychiatr. 2013, 26, 356–363. [Google Scholar] [CrossRef]
- Rana, T.; Behl, T.; Sehgal, A.; Srivastava, P.; Bungau, S. Unfolding the Role of BDNF as a Biomarker for Treatment of Depression. J. Mol. Neurosci. 2020, 71, 2008–2021. [Google Scholar] [CrossRef]
- Li, H.-Y.; Zhu, M.-Z.; Yuan, X.-R.; Guo, Z.-X.; Pan, Y.-D.; Li, Y.-Q.; Zhu, X.-H. A thalamic-primary auditory cortex circuit mediates resilience to stress. Cell 2023, 186, 1352–1368.e18. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Wu, G.W.; Reus, V.I.; Hough, C.M.; Lindqvist, D.; Westrin, Å.; Nier, B.M.; Wolkowitz, O.M.; Mellon, S.H. Low serum brain-derived neurotrophic factor is associated with suicidal ideation in major depressive disorder. Psychiatry Res. 2019, 273, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-K.; Lee, H.-P.; Won, S.-D.; Park, E.-Y.; Lee, H.-Y.; Lee, B.-H.; Lee, S.-W.; Yoon, D.; Han, C.; Kim, D.-J.; et al. Low plasma BDNF is associated with suicidal behavior in major depression. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2006, 31, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Dawood, T.; Anderson, J.; Barton, D.; Lambert, E.; Esler, M.; Hotchkin, E.; Haikerwal, D.; Kaye, D.; Lambert, G. Reduced overflow of BDNF from the brain is linked with suicide risk in depressive illness. Mol. Psychiatry 2007, 12, 981–983. [Google Scholar] [CrossRef]
- Salas-Magaña, M.; Tovilla-Zárate, C.A.; González-Castro, T.B.; Juárez-Rojop, I.E.; López-Narváez, M.L.; Rodríguez-Pérez, J.M.; Bello, J.R. Decrease in brain-derived neurotrophic factor at plasma level but not in serum concentrations in suicide behavior: A systematic review and meta-analysis. Brain Behav. 2017, 7, e00706. [Google Scholar] [CrossRef]
- Moreira, F.P.; Borges, C.J.; Wiener, C.D.; da Silva, P.M.; Portela, L.V.; Lara, D.R.; da Silva, R.A.; Souza, L.D.d.M.; Jansen, K.; Oses, J.P. Serum brain-derived neurotrophic factor levels in subjects with major depressive disorder with previous suicide attempt: A population-based study. Psychiatry Res. 2018, 262, 500–504. [Google Scholar] [CrossRef]
- Park, Y.-M.; Lee, B.-H.; Um, T.H.; Kim, S. Serum BDNF Levels in Relation to Illness Severity, Suicide Attempts, and Central Serotonin Activity in Patients with Major Depressive Disorder: A Pilot Study. PLoS ONE 2014, 9, e91061. [Google Scholar] [CrossRef]
- Pinheiro, R.T.; Pinheiro, K.A.T.; Coelho, F.M.d.C.; Quevedo, L.d.; Gazal, M.; da Silva, R.A.; Giovenardi, M.; Lucion, A.B.; de Souza, D.O.; Portela, L.V.; et al. Brain-Derived Neurotrophic Factor Levels in Women with Postpartum Affective Disorder and Suicidality. Neurochem. Res. 2012, 37, 2229–2234. [Google Scholar] [CrossRef]
- Hartig, J.; Neme, B. BDNF-related mutations in major depressive disorder: A systematic review. Acta Neuropsychiatr. 2023, 35, 5–26. [Google Scholar] [CrossRef]
- Ferrer, A.; Labad, J.; Salvat-Pujol, N.; Barrachina, M.; Costas, J.; Urretavizcaya, M.; Arriba-Arnau, A.; Crespo, J.M.; Soriano-Mas, C.; Carracedo, A.; et al. BDNF genetic variants and methylation: Effects on cognition in major depressive disorder. Transl. Psychiatry. 2019, 9, 265. [Google Scholar] [CrossRef]
- Lee, B.-H.; Kim, Y.-K. BDNF mRNA expression of peripheral blood mononuclear cells was decreased in depressive patients who had or had not recently attempted suicide. J. Affect. Disord. 2010, 125, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Cefis, M.; Prigent-Tessier, A.; Quirié, A.; Pernet, N.; Marie, C.; Garnier, P. The effect of exercise on memory and BDNF signaling is dependent on intensity. Anat. Embryol. 2019, 224, 1975–1985. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Du, X.; Yin, G.; Zhang, Y.; Li, X.; Cai, J.; Huang, X.; Ning, Y.; Soares, J.C.; Wu, F.; et al. Effects of smoking on cognition and BDNF levels in a male Chinese population: Relationship with BDNF Val66Met polymorphism. Sci. Rep. 2019, 9, 217. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | MDD + HSI (n = 43) | MDD + LSI (n = 40) | CON (n = 93) | p |
|---|---|---|---|---|
| % Males (n) | 37.2 (16) | 35.0 (14) | 43.0 (40) | 0.638 |
| Age (y), mean (SD) | 26.44 (6.77) | 27.98 (6.94) | 27.58 (7.69) | 0.566 |
| Education (y), mean (SD) | 14.21 (2.24) | 14.88 (1.77) | 14.92 (1.81) | 0.194 |
| Illness duration (m), mean (SD) | 2.45 (2.92) | 1.86 (2.05) | 0.970 | |
| Relapse time (n) | 1.53 (0.86) | 1.42 (0.89) | 0.321 | |
| Onset age (y) | 24.35 (6.94) | 25.97 (6.26) | 0.272 | |
| HAMD-17 score, mean (SD) | 24.53 (4.70) | 23.48 (4.18) | 2.28 (2.53) | <0.001 ab |
| Anxiety/somatization, mean (SD) | 8.30 (1.94) | 7.26 (1.90) | 1.11 (1.31) | <0.001 abc |
| Cognitive disorder, mean (SD) | 5.58 (1.43) | 3.75 (1.72) | 0.13 (0.37) | <0.001 abc |
| Psychomotor retardation, mean (SD) | 7.49 (1.88) | 7.58 (1.78) | 046 (0.93) | <0.001 ab |
| Sleep disorder, mean (SD) | 3.56 (1.59) | 3.38 (1.58) | 0.38 (0.90) | <0.001 ab |
| Weight, mean (SD) | 0.65 (0.90) | 0.48 (0.85) | 0.05 (0.31) | <0.001 ab |
| Neuroticism, mean (SD) | 41.12 (6.74) | 42.10 (6.05) | 27.02 (6.61) | <0.001 ab |
| Extraversion, mean (SD) | 28.23 (7.62) | 30.65 (6.74) | 40.11 (6.44) | <0.001 ab |
| Conscientiousness, mean (SD) | 38.14 (7.94) | 38.80 (7.12) | 43.56 (5.49) | <0.001 ab |
| Agreeableness, mean (SD) | 40.56 (5.84) | 42.15 (5.54) | 43.28 (4.62) | 0.023 ab |
| Openness, mean (SD) | 35.05 (6.89) | 38.03 (5.25) | 39.19 (4.89) | 0.001 abc |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
| |
| |
| |
| |
|
| Plasma Peptide | MDD + HSI (n = 43) | MDD + LSI (n = 40) | CON (n = 93) | p | ES (HSI vs. LSI) | ES (HSI vs. CON) | ES (LSI vs. CON) |
|---|---|---|---|---|---|---|---|
| mBDNF, mean (SD) | 8900.82 (5488.47) | 6157.71 (2965.86) | 3508.85 (3590.37) | <0.001 abc | 0.30 | 0.50 | 0.37 |
| proBDNF, mean (SD) | 2011.14 (2317.79) | 1076.08 (1643.96) | 3236.87 (2832.83) | <0.001 ab | 0.23 | −0.23 | −0.42 |
| TrkB, mean (SD) | 5620.79 (1350.27) | 5721.11 (1201.44) | 6435.37 (1387.59) | <0.001 ab | −0.04 | −0.29 | −0.27 |
| tpA, mean (SD) | 1865.83 (945.97) | 1986.40 (780.20) | 1526.29 (767.85) | <0.001 ab | −0.07 | 0.19 | 0.28 |
| IL-1β, mean (SD) | 722.32 (341.67) | 847.86 (877.17) | 295.25 (125.54) | <0.001 ab | −0.09 | 0.64 | 0.40 |
| IL-6, mean (SD) | 783.01 (500.53) | 996.71 (711.76) | 712.08 (521.99) | 0.021 ab | −0.17 | 0.07 | 0.22 |
| TNF, mean (SD) | 473.34 (216.04) | 532.12 (196.36) | 533.93 (286.75) | 0.492 | −0.14 | -0.12 | −0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; Zhao, M.; Jiang, C.; Zhao, H.; Wu, C.; Li, Y.; Zhang, S.; Xu, P.; Mou, T.; Xu, Y.; et al. Elevated Plasma Levels of Mature Brain-Derived Neurotrophic Factor in Major Depressive Disorder Patients with Higher Suicidal Ideation. Brain Sci. 2023, 13, 1223. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci13081223
Li H, Zhao M, Jiang C, Zhao H, Wu C, Li Y, Zhang S, Xu P, Mou T, Xu Y, et al. Elevated Plasma Levels of Mature Brain-Derived Neurotrophic Factor in Major Depressive Disorder Patients with Higher Suicidal Ideation. Brain Sciences. 2023; 13(8):1223. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci13081223
Chicago/Turabian StyleLi, Haimei, Miaomiao Zhao, Chaonan Jiang, Haoyang Zhao, Congchong Wu, Ying Li, Shiyi Zhang, Pengfeng Xu, Tingting Mou, Yi Xu, and et al. 2023. "Elevated Plasma Levels of Mature Brain-Derived Neurotrophic Factor in Major Depressive Disorder Patients with Higher Suicidal Ideation" Brain Sciences 13, no. 8: 1223. https://0-doi-org.brum.beds.ac.uk/10.3390/brainsci13081223