Impact of EcSOD Perturbations in Cancer Progression
Abstract
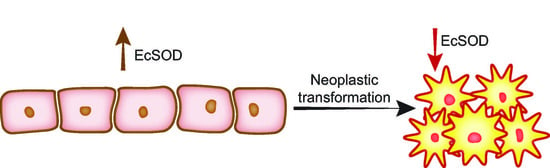
:1. Reactive Oxygen Species (ROS)
2. EcSOD
2.1. EcSOD Expression
2.2. EcSOD and Disease
2.3. EcSOD and Cancer
2.4. Hypermethylation of EcSOD
2.5. Single Nucleotide Polymorphisms
2.6. Phenotypic Effects of EcSOD Expression
3. SOD Mimetics in Cancer Therapy
SOD Mimetics and Pharmacological Ascorbate
4. Summary
Funding
Data Availability Statement
Conflicts of Interest
References
- Suzuki, Y.J.; Forman, H.J.; Sevanian, A. Oxidants as Stimulators of Signal Transduction. Free. Radic. Biol. Med. 1997, 22, 269–285. [Google Scholar] [CrossRef]
- Thannickal, V.J.; Fanburg, B.L. Reactive oxygen species in cell signaling. Am. J. Physiol. Cell. Mol. Physiol. 2000, 279, L1005–L1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heyworth, P.G.; Cross, A.R.; Curnutte, J.T. Chronic granulomatous disease. Curr. Opin. Immunol. 2003, 15, 578–584. [Google Scholar] [CrossRef]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.; Mazur, M.; Telser, J. Free radicals and antioxidants in normal physio-logical functions and human disease. Int. J. Biochem. Cell Biol. 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Kinnula, V.L.; Crapo, J.D. Superoxide dismutases in malignant cells and human tumors. Free. Radic. Biol. Med. 2004, 36, 718–744. [Google Scholar] [CrossRef] [PubMed]
- Mccord, J.M.; Fridovich, I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar] [CrossRef]
- Weisiger, R.A.; Fridovich, I. Mitochondrial superoxide simutase. Site of synthesis and intramitochondrial localization. J. Biol. Chem. 1973, 248, 4793–4796. [Google Scholar] [CrossRef]
- Marklund, S.L.; Holme, E.; Hellner, L. Superoxide dismutase in extracellular fluids. Clin. Chim. Acta 1982, 126, 41–51. [Google Scholar] [CrossRef]
- Oberley, L.W.; Buettner, G. Role of superoxide dismutase in cancer: A review. Cancer Res. 1979, 39, 1141–1149. [Google Scholar]
- Hendrickson, D.J.; Fisher, J.H.; Jones, C.; Ho, Y.-S. Regional localization of human extracellular superoxide dismutase gene to 4pter-q. Genomics 1990, 8, 736–738. [Google Scholar] [CrossRef]
- Zelko, I.N.; Mariani, T.J.; Folz, R.J. Superoxide dismutase multigene family: A comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic. Biol. Med. 2002, 33, 337–349. [Google Scholar] [CrossRef]
- Marklund, S.L. Extracellular superoxide dismutase in human tissues and human cell lines. J. Clin. Investig. 1984, 74, 1398–1403. [Google Scholar] [CrossRef] [PubMed]
- Marklund, S.L. Extracellular superoxide dismutase and other superoxide dismutase isoenzymes in tissues from nine mamma-lian species. Biochem. J. 1984, 222, 649–655. [Google Scholar] [CrossRef] [Green Version]
- Folz, R.J.; Crapo, J.D. Extracellular Superoxide Dismutase (SOD3): Tissue-Specific Expression, Genomic Characterization, and Computer-Assisted Sequence Analysis of the Human EC SOD Gene. Genomics 1994, 22, 162–171. [Google Scholar] [CrossRef]
- Uhlén, M.; Fagerberg, L.; Hallström, B.M.; Lindskog, C.; Oksvold, P.; Mardinoglu, A.; Sivertsson, A.; Kampf, C.; Sjöstedt, E.; Asplund, A.; et al. Tissue-based map of the human proteome. Science 2015, 347, 1260419. [Google Scholar] [CrossRef]
- The Human Protein Atlas. Available online: https://www.proteinatlas.org/ENSG00000109610-SOD3/tissue (accessed on 15 July 2021).
- Sandström, J.; Carlsson, L.; Marklund, S.L.; Edlund, T. The heparin-binding domain of extracellular superoxide dismutase C and formation of variants with reduced heparin affinity. J. Biol. Chem. 1992, 267, 18205–18209. [Google Scholar] [CrossRef]
- Yan, Z.; Spaulding, H.R. Extracellular superoxide dismutase, a molecular transducer of health benefits of exercise. Redox Biol. 2020, 32, 101508. [Google Scholar] [CrossRef]
- Sandstrom, J.; Nilsson, P.; Karlsson, K.; Marklund, S.L. 10-fold increase in human plasma extracellular superoxide dis-mutase content caused by a mutation in heparin-binding domain. J. Biol. Chem. 1994, 269, 19163–19166. [Google Scholar] [CrossRef]
- Karlsson, K.; Edlund, A.; Sandstrom, J.; Marklund, S.L. Proteolytic modification of the heparin-binding affinity of extra-cellular superoxide dismutase. Biochem. J. 1993, 290, 623–626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandstrom, J.; Karlsson, K.; Edlund, T.; Marklund, S.L. Heparin-affinity patterns and composition of extracellular super-oxide dismutase in human plasma and tissues. Biochem. J. 1993, 294, 853–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karlsson, K.; Sandström, J.; Edlund, A.; Marklund, S.L. Turnover of extracellular-superoxide dismutase in tissues. Lab. Investig. 1994, 70, 705–710. [Google Scholar] [PubMed]
- Fukai, T.; Siegfried, M.R.; Ushio-Fukai, M.; Cheng, Y.; Kojda, G.; Harrison, D.G. Regulation of the vascular extracellular superoxide dismutase by nitric oxide and exercise training. J. Clin. Investig. 2000, 105, 1631–1639. [Google Scholar] [CrossRef] [Green Version]
- Fukai, T.; Siegfried, M.R.; Ushio-Fukai, M.; Griendling, K.K.; Harrison, D.G. Modulation of extracellular superoxide dis-mutase expression by angiotensin II and hypertension. Circ. Res. 1999, 85, 23–28. [Google Scholar] [CrossRef] [Green Version]
- Adachi, T.; Hara, H.; Yamada, H.; Yamazaki, N.; Yamamoto, M.; Sugiyama, T.; Futenma, A.; Katagiri, Y. Hepa-rin-stimulated expression of extracellular-superoxide dismutase in human fibroblasts. Atherosclerosis 2001, 159, 307–312. [Google Scholar] [CrossRef]
- Strålin, P.; Marklund, S.L. Multiple cytokines regulate the expression of extracellular superoxide dismutase in human vascular smooth muscle cells. Atherosclerosis 2000, 151, 433–441. [Google Scholar] [CrossRef]
- Strehlow, K.; Rotter, S.; Wassmann, S.; Adam, O.; Grohe, C.; Laufs, K.; Bohm, M.; Nickenig, G. Modulation of anti-oxidant enzyme expression and function by estrogen. Circ. Res. 2003, 93, 170–177. [Google Scholar] [CrossRef]
- Itoh, S.; Ozumi, K.; Kim, H.W.; Nakagawa, O.; McKinney, R.D.; Folz, R.J.; Zelko, I.N.; Ushio-Fukai, M.; Fukai, T. Novel mechanism for regulation of extracellular SOD transcription and activity by copper: Role of antioxidant. Free. Radic. Biol. Med. 2009, 46, 95–104. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.L.; Adachi, T.; Sim, A.S.; Wilcken, D.E. Plasma extracellular superoxide dismutase levels in an Australian popu-lation with coronary artery disease. Arterioscler. Thromb. Vasc. Biol. 1998, 18, 1915–1921. [Google Scholar] [CrossRef] [Green Version]
- Gongora, M.C.; Qin, Z.; Laude, K.; Kim, H.W.; McCann, L.; Folz, J.R.; Dikalov, S.; Fukai, T.; Harrison, D.G. Role of Extracellular Superoxide Dismutase in Hypertension. Hypertension 2006, 48, 473–481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, O.; Marklund, S.L.; Geiger, H.; Pedrazzini, T.; Busse, R.; Brandes, R.P. Extracellular superoxide dismutase is a major determinant of nitric oxide bioavailability: In vivo and ex vivo evidence from ecSOD-deficient mice. Circ. Res. 2003, 93, 622–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, M.N.; Zhang, Y.; Codipilly, C.; Zaghloul, N.; Patel, D.; Wolin, M.; Miller, E.J. Extracellular superoxide dis-mutase overexpression can reverse the course of hypoxia-induced pulmonary hypertension. Mol. Med. 2012, 18, 38–46. [Google Scholar] [CrossRef]
- Wedgwood, S.; Lakshminrusimha, S.; Fukai, T.; Russell, J.A.; Schumacker, P.T.; Steinhorn, R.H. Hydrogen Peroxide Regulates Extracellular Superoxide Dismutase Activity and Expression in Neonatal Pulmonary Hypertension. Antioxid. Redox Signal. 2011, 15, 1497–1506. [Google Scholar] [CrossRef]
- Yao, H.; Arunachalam, G.; Hwang, J.-W.; Chung, S.; Sundar, I.K.; Kinnula, V.L.; Crapo, J.D.; Rahman, I. Extracellular superoxide dismutase protects against pulmonary emphysema by attenuating oxidative fragmentation of ECM. Proc. Natl. Acad. Sci. USA 2010, 107, 15571–15576. [Google Scholar] [CrossRef] [Green Version]
- Svensk, A.M.; Soini, Y.; Paakko, P.; Hiravikoski, P.; Kinnula, V.L. Differential expression of superoxide dismutases in lung cancer. Am. J. Clin. Pathol. 2004, 122, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Yoo, D.G.; Song, Y.J.; Cho, E.J.; Lee, S.K.; Park, J.B.; Yu, J.H.; Lim, S.P.; Kim, J.M.; Jeon, B.H. Alteration of APE1/ref-1 expression in non-small cell lung cancer: The implications of impaired extracellular superoxide dismutase and catalase anti-oxidant systems. Lung Cancer 2008, 60, 277–284. [Google Scholar] [CrossRef]
- Teoh-Fitzgerald, M.L.; Fitzgerald, M.P.; Jensen, T.J.; Futscher, B.W.; Domann, F.E. Genetic and Epigenetic Inactivation of Extracellular Superoxide Dismutase Promotes an Invasive Phenotype in Human Lung Cancer by Disrupting ECM Homeostasis. Mol. Cancer Res. 2012, 10, 40–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzgerald, M.P.; Zhong, W.; Askeland, R.W.; Domann, F.E. Epigenetic reprogramming governs EcSOD expression during human mammary epithelial cell differentiation, tumorigenesis and metastasis. Oncogene 2013, 33, 358–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Leary, B.R.; Fath, M.; Bellizzi, A.; Hrabe, J.; Button, A.M.; Allen, B.; Case, A.; Altekruse, S.; Wagner, B.A.; Buettner, G.; et al. Loss of SOD3 (EcSOD) Expression Promotes an Aggressive Phenotype in Human Pancreatic Ductal Adenocarcinoma. Clin. Cancer Res. 2015, 21, 1741–1751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hubackova, M.; Vaclavikova, R.; Ehrlichova, M.; Mrhalova, M.; Kodet, R.; Kubackova, K.; Vrana, D.; Gut, I.; Soucek, P. Association of superoxide dismutases and NAD(P)H quinone oxidoreductases with prognosis of patients with breast car-cinomas. Int. J. Cancer 2012, 130, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Laatikainen, L.E.; Castellone, M.D.; Hebrant, A.; Hoste, C.; Cantisani, M.C.; Laurila, J.P.; Salvatore, G.; Salerno, P.; Basolo, F.; Nasman, J.; et al. Extracellular superoxide dismutase is a thyroid dif-ferentiation marker down-regulated in cancer. Endocr. Relat. Cancer 2010, 17, 785–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parascandolo, A.; Rappa, F.; Cappello, F.; Kim, J.; Cantu, D.A.; Chen, H.; Mazzoccoli, G.; Hematti, P.; Castellone, M.D.; Salvatore, M.; et al. Extracellular Superoxide Dismutase Expression in Papillary Thyroid Cancer Mesen-chymal Stem/Stromal Cells Modulates Cancer Cell Growth and Migration. Sci. Rep. 2017, 7, 41416. [Google Scholar] [CrossRef] [Green Version]
- Soini, Y.; Kallio, J.P.; Hirvikoski, P.; Helin, H.; Kellokumpu-Lehtinen, P.; Tammela, T.L.J.; Peltoniemi, M.; Martikainen, P.M.; Kinnula, L.V. Antioxidant enzymes in renal cell carcinoma. Histol. Histopathol. 2006, 21, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Fattman, C.L.; Schaefer, L.M.; Oury, T.D. Extracellular superoxide dismutase in biology and medicine. Free. Radic. Biol. Med. 2003, 35, 236–256. [Google Scholar] [CrossRef]
- Naushad, S.M.; Reddy, C.A.; Rupasree, Y.; Pavani, A.; Digumarti, R.R.; Gottumukkala, S.R.; Kuppusamy, P.; Kutala, V.K. Cross-Talk between One-Carbon Metabolism and Xenobiotic Metabolism: Implications on Oxidative DNA Damage and Susceptibility to Breast Cancer. Cell Biochem. Biophys. 2011, 61, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Griess, B.; Klinkebiel, D.; Kueh, A.; Desler, M.; Cowan, K.; Fitzgerald, M.; Teoh-Fitzgerald, M. Association ofSOD3 promoter DNA methylation with its down-regulation in breast carcinomas. Epigenetics 2020, 15, 1325–1335. [Google Scholar] [CrossRef]
- Mohelnikova-Duchonova, B.; Marsakova, L.; Vrana, D.; Holcatova, I.; Ryska, M.; Smerhovsky, Z.; Slamova, A.; Schejbalova, M.; Soucek, P. Superoxide dismutase and nicotinamide adenine dinucleotide phosphate: Quinone oxidoreductase polymorphisms and pancreatic cancer risk. Pancreas 2011, 40, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Xie, W.; Regan, M.M.; King, I.B.; Stampfer, M.J.; Kantoff, P.W.; Oh, W.K.; Chan, J.M. Single-nucleotide polymorphisms within the antioxidant defence system and associations with aggressive prostate cancer. BJU Int. 2010, 107, 126–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, D.; Lee, K.-M.; Park, S.K.; Berndt, S.I.; Peters, U.; Reding, D.; Chatterjee, N.; Welch, R.; Chanock, S.; Huang, W.-Y.; et al. Functional Variant of Manganese Superoxide Dismutase (SOD2 V16A) Polymorphism Is Associated with Prostate Cancer Risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Study. Cancer Epidemiol. Biomark. Prev. 2007, 16, 1581–1586. [Google Scholar] [CrossRef] [Green Version]
- Rajaraman, P.; Hutchinson, A.; Rothman, N.; Black, P.M.; Fine, H.A.; Loeffler, J.S.; Selker, R.G.; Shapiro, W.R.; Linet, M.S.; Inskip, P.D. Oxidative response gene polymorphisms and risk of adult brain tumors. Neuro-Oncology 2008, 10, 709–715. [Google Scholar] [CrossRef] [Green Version]
- Du, J.; Nelson, E.S.; Simons, A.L.; Olney, K.E.; Moser, J.C.; Schrock, H.; Wagner, B.A.; Buettner, G.; Smith, B.J.; Teoh, M.L.; et al. Regulation of pancreatic cancer growth by superoxide. Mol. Carcinog. 2012, 52, 555–567. [Google Scholar] [CrossRef] [Green Version]
- Teoh, M.L.; Sun, W.; Smith, B.J.; Oberley, L.W.; Cullen, J. Modulation of Reactive Oxygen Species in Pancreatic Cancer. Clin. Cancer Res. 2007, 13, 7441–7450. [Google Scholar] [CrossRef] [Green Version]
- Deng, X.; Ewton, D.Z.; Friedman, E. Mirk/Dyrk1B Maintains the Viability of Quiescent Pancreatic Cancer Cells by Reducing Levels of Reactive Oxygen Species. Cancer Res. 2009, 69, 3317–3324. [Google Scholar] [CrossRef] [Green Version]
- Sibenaller, Z.A.; Welsh, J.L.; Du, C.; Witmer, J.R.; Schrock, H.E.; Du, J.; Buettner, G.R.; Goswami, P.C.; Cieslak, J.A., 3rd; Cullen, J.J. Extracellular superoxide dismutase suppresses hypoxia-inducible factor-1alpha in pancreatic cancer. Free Radic. Biol. Med. 2014, 69, 357–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basu, A.; Drame, A.; Muñoz, R.; Gijsbers, R.; Debyser, Z.; De Leon, M.; Casiano, C.A. Pathway specific gene expression profiling reveals oxidative stress genes potentially regulated by transcription co-activator LEDGF/p75 in prostate cancer cells. Prostate 2011, 72, 597–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaiswing, L.; Zhong, W.; Cullen, J.; Oberley, L.W.; Oberley, T.D. Extracellular Redox State Regulates Features Associated with Prostate Cancer Cell Invasion. Cancer Res. 2008, 68, 5820–5826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teoh, M.L.T.; Fitzgerald, M.P.; Oberley, L.W.; Domann, F.E. Overexpression of Extracellular Superoxide Dismutase Attenuates Heparanase Expression and Inhibits Breast Carcinoma Cell Growth and Invasion. Cancer Res. 2009, 69, 6355–6363. [Google Scholar] [CrossRef] [Green Version]
- Golden, B.O.; Griess, B.; Mir, S.; Fitzgerald, M.; Kuperwasser, C.; Domann, F.; Teoh-Fitzgerald, M. Extracellular su-peroxide dismutase inhibits hepatocyte growth factor-mediated breast cancer-fibroblast interactions. Oncotarget 2017, 8, 107390–107408. [Google Scholar] [CrossRef] [Green Version]
- Wheeler, M.D.; Smutney, O.M.; Samulski, R.J. Secretion of extracellular superoxide dismutase from muscle transduced with recombinant adenovirus inhibits the growth of B16 melanomas in mice. Mol. Cancer Res. 2003, 1, 871–881. [Google Scholar]
- Saed, G.M.; Ali-Fehmi, R.; Jiang, Z.L.; Fletcher, N.M.; Diamond, M.P.; Abu-Soud, H.M.; Munkarah, A.R. Myeloperox-idase serves as a redox switch that regulates apoptosis in epithelial ovarian cancer. Gynecol. Oncol. 2010, 116, 276–281. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Z.; Fletcher, N.M.; Ali-Fehmi, R.; Diamond, M.P.; Abu-Soud, H.M.; Munkarah, A.R.; Saed, G.M. Modulation of redox signaling promotes apoptosis in epithelial ovarian cancer cells. Gynecol. Oncol. 2011, 122, 418–423. [Google Scholar] [CrossRef] [Green Version]
- Messerli, S.M.; Schaefer, A.M.; Zhuang, Y.; Soltys, B.J.; Keime, N.; Jin, J.; Ma, L.; Hsia, C.J.C.; Miskimins, W.K. Use of Antimetastatic SOD3-Mimetic Albumin as a Primer in Triple Negative Breast Cancer. J. Oncol. 2019, 2019, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Saed, G.M.; Fletcher, N.M.; Jiang, Z.L.; Abu-Soud, H.M.; Diamond, M.P. Dichloroacetate Induces Apoptosis of Epithelial Ovarian Cancer Cells Through a Mechanism Involving Modulation of Oxidative Stress. Reprod. Sci. 2011, 18, 1253–1261. [Google Scholar] [CrossRef]
- Wang, C.-A.; Harrell, J.C.; Iwanaga, R.; Jedlicka, P.; Ford, H.L. Vascular endothelial growth factor C promotes breast cancer progression via a novel antioxidant mechanism that involves regulation of superoxide dismutase. Breast Cancer Res. 2014, 16, 462. [Google Scholar] [CrossRef] [Green Version]
- Mira, E.; Carmona-Rodríguez, L.; Pérez-Villamil, B.; Casas, J.; Fernández-Aceñero, M.J.; Martinez-Rey, D.; Martín-González, P.; Heras-Murillo, I.; Cabezas, M.P.; Tardáguila, M.; et al. SOD3 improves the tumor response to chemotherapy by stabilizing endothelial HIF-2α. Nat. Commun. 2018, 9, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carmona-Rodríguez, L.; Martínez-Rey, D.; Fernández-Aceñero, M.J.; González-Martín, A.; Cabezas, M.P.; Rodriguez-Rodriguez, N.; Pérez-Villamil, B.; Sáez, M.E.; Díaz-Rubio, E.; Mira, E.; et al. SOD3 induces a HIF-2α-dependent program in endothelial cells that provides a selective signal for tumor infiltration by T cells. J. Immunother. Cancer 2020, 8, e000432. [Google Scholar] [CrossRef] [PubMed]
- Takenaga, M.; Igarashi, R.; Ochiai, A.; Mizushima, Y. Effect of lecithinized superoxide dismutase (PC-SOD) on experimental pulmonary metastasis in mice. Free Radic. Biol. Med. 1999, 26, 1117–1125. [Google Scholar] [CrossRef]
- Vickers, S.M.; MacMillan-Crow, L.A.; Green, M.; Ellis, C.; Thompson, J.A. Association of Increased Immunostaining for Inducible Nitric Oxide Synthase and Nitrotyrosine With Fibroblast Growth Factor Transformation in Pancreatic Cancer. Arch. Surg. 1999, 134, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Kato, H.; Miyazaki, T.; Yoshikawa, M.; Nakajima, M.; Fukai, Y.; Tajima, K.; Masuda, N.; Tsutsumi, S.; Tsukada, K.; Nakajima, T.; et al. Nitrotyrosine in esophageal squamous cell carcinoma and relevance to p53 expression. Cancer Lett. 2000, 153, 121–127. [Google Scholar] [CrossRef]
- Chatterjee, A.; Zhu, Y.; Tong, Q.; Kosmacek, E.A.; Lichter, E.Z.; Oberley-Deegan, R.E. The Addition of Manganese Porphyrins during Radiation Inhibits Prostate Cancer Growth and Simultaneously Protects Normal Prostate Tissue from Radiation Damage. Antioxidants 2018, 7, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shrishrimal, S.; Kosmacek, E.A.; Chatterjee, A.; Tyson, M.J.; Oberley-Deegan, R.E. The SOD Mimic, MnTE-2-PyP, Protects from Chronic Fibrosis and Inflammation in Irradiated Normal Pelvic Tissues. Antioxidants 2017, 6, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cline, J.M.; Dugan, G.; Bourland, J.D.; Perry, D.L.; Stitzel, J.D.; Weaver, A.A.; Jiang, C.; Tovmasyan, A.; Owzar, K.; Spasojevic, I.; et al. Post-Irradiation Treatment with a Superoxide Dismutase Mimic, MnTnHex-2-PyP5+, Mitigates Radiation Injury in the Lungs of Non-Human Primates after Whole-Thorax Exposure to Ionizing Radiation. Antioxidants 2018, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Anderson, C.M.; Lee, C.M.; Saunders, D.P.; Curtis, A.; Dunlap, N.; Nangia, C.; Lee, A.S.; Gordon, S.M.; Kovoor, P.; Arevalo-Araujo, R.; et al. Phase IIb, Randomized, Double-Blind Trial of GC4419 Versus Placebo to Reduce Severe Oral Mucositis Due to Concurrent Radiotherapy and Cisplatin For Head and Neck Cancer. J. Clin. Oncol. 2019, 37, 3256–3265. [Google Scholar] [CrossRef]
- Du, J.; Martin, S.M.; Levine, M.; Wagner, B.A.; Buettner, G.; Wang, S.-H.; Taghiyev, A.F.; Du, C.; Knudson, C.M.; Cullen, J.J. Mechanisms of Ascorbate-Induced Cytotoxicity in Pancreatic Cancer. Clin. Cancer Res. 2010, 16, 509–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, M.S.; Wilkes, J.G.; Schroeder, S.R.; Buettner, G.R.; Wagner, B.A.; Du, J.; Gibson-Corley, K.; O’Leary, B.R.; Spitz, D.R.; Buatti, J.M.; et al. Pharmacologic Ascorbate Reduces Radiation-Induced Normal Tissue Toxicity and Enhances Tumor Radiosensitization in Pancreatic Cancer. Cancer Res. 2018, 78, 6838–6851. [Google Scholar] [CrossRef] [Green Version]
- Welsh, J.L.; Wagner, B.A.; van’t Erve, T.J.; Zehr, P.S.; Berg, D.J.; Halfdanarson, T.R.; Yee, N.S.; Bodeker, K.L.; Du, J.; Roberts, L.J., 2nd; et al. Pharmacological ascorbate with gemcitabine for the control of metastatic and node-positive pancreatic cancer (PACMAN): Results from a phase I clinical trial. Cancer Chemother. Pharm. 2013, 71, 765–775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, M.S.; O’Leary, B.R.; Wilkes, J.G.; Gibson, A.R.; Wagner, B.A.; Du, J.; Sarsour, E.; Hwang, R.F.; Buettner, G.R.; Cullen, J.J. Enhanced Pharmacological Ascorbate Oxidation Radiosensitizes Pancreatic Cancer. Radiat. Res. 2018, 191, 43–51. [Google Scholar] [CrossRef]
- Batinić-Haberle, I.; Reboucas, J.; Spasojević, I. Superoxide Dismutase Mimics: Chemistry, Pharmacology, and Therapeutic Potential. Antioxid. Redox Signal. 2010, 13, 877–918. [Google Scholar] [CrossRef] [Green Version]
- Rawal, M.; Schroeder, S.R.; Wagner, B.A.; Cushing, C.; Welsh, J.L.; Button, A.; Du, J.; Sibenaller, Z.A.; Buettner, G.; Cullen, J.J. Manganoporphyrins Increase Ascorbate-Induced Cytotoxicity by Enhancing H2O2 Generation. Cancer Res. 2013, 73, 5232–5241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heer, C.D.; Davis, A.B.; Riffe, D.B.; Wagner, B.A.; Falls, K.C.; Allen, B.G.; Buettner, G.R.; Beardsley, R.A.; Riley, D.P.; Spitz, D.R. Superoxide Dismutase Mimetic GC4419 Enhances the Oxidation of Pharmacological Ascorbate and Its Anticancer Effects in an H2O2-Dependent Manner. Antioxidants 2018, 7, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, A.R.; O’Leary, B.R.; Du, J.; Sarsour, E.; Kalen, A.L.; Wagner, B.A.; Stolwijk, J.M.; Falls-Hubert, K.C.; Alexander, M.S.; Carroll, R.S.; et al. Dual Oxidase-Induced Sustained Generation of Hydrogen Peroxide Contributes to Pharmacologic Ascorbate-Induced Cytotoxicity. Cancer Res. 2020, 80, 1401–1413. [Google Scholar] [CrossRef]





| Tissue | Growth/Proliferation | Cell Types | Model | Other Effects | Reference |
|---|---|---|---|---|---|
| Pancreas | Decreased doubling time, tumor growth | Mia PaCa-2, BxPC-3 | In vitro—adenoviral overexpression, In vivo—intratumoral injection with adenoviral constructs | Teoh/Cullen 2007 [52] | |
| Pancreas | Decreased doubling time, tumor growth | Mia PaCa-2, H6c7 | In vitro—adenoviral overexpression, In vivo—intratumoral injection with adenoviral constructs | Du/Cullen 2012 [51] | |
| Pancreas | Increased indirectly; survival of quiescent cells | SU86.86, Panc-1 | In vitro | Loss of EcSOD correlated with decreased survival of quiescent cells | Deng 2009 [53] |
| Pancreas | Decreased doubling time, tumor growth | Mia PaCa-2, BxPC-3 | In vitro—stable cell overexpression, In vivo—subcutaneous injection with stably overexpressing cells | EcSOD overexpression decreased invasive capacity. Loss of EcSOD correlated with worsened disease biology | O’Leary 2015 [39] |
| Pancreas | Decreased tumor growth | Mia PaCa-2 | In vivo—intratumoral injection with adenoviral constructs | EcSOD overexpression suppressed VEGF levels | Sibenallar 2014 [54] |
| Prostate | NA | PC3 | qPCR gene microarray | EcSOD expression increased/decreased corresponding to LEDGF expression | Basu 2011 [55] |
| Prostate | NA | DU145, PC-3, WPEI-NB26 | In vitro—adenoviral overexpression | Overexpressed EcSOD decreased cell invasiveness | Chaiswing 2008 [56] |
| Breast | Decreased doubling time, clonogenic survival | MDA-MB231, MDA-MB 435 | In vitro—adenoviral overexpression | Decreased invasive capacity (matrigel) | Teoh/Domann 2009 [57] |
| Breast | NA | Human breast tissue samples | Increase in hypermethylation of EcSOD promoter in breast ca | Naushad 2011 [45] | |
| Breast | NA | Human breast tissue samples | Decreased EcSOD in tumor vs. normal; higher expression in lower grade tumor samples | Hubackova 2012 [40] | |
| Breast | NA | Decreased EcSOD in mRNA and protein in tumor vs. normal; inverse correlation with clinical stages of cancer | Teoh 2014 [38] | ||
| Breast | NA | MDA-MB231, MDA-MB468, RMF | In vitro—MDA-MB231 overexpressing EcSOD cell line | EcSOD overexpression suppresses oncogenic cancer-fibroblast interaction | Golden 2017 [58] |
| Breast | NA | Human breast tissue samples | Pyrosequencing analysis in breast carcinoma samples | Increase in methylation status of EcSOD promoter in tumor vs. normal tissue | Griess 2020 [46] |
| Lung | Decreased clonogenic survival | HAE, A549, MRC-5, NCI-H1975 & H1650; lung tissue samples | In vitro—adenoviral overexpression | Decreased invasive capacity (matrigel) | Teoh 2012 [37] |
| Lung | NA | Human lung ca tissue samples | Decreased EcSOD in tumor vs. normal | Yoo 2008 [36] | |
| Lung | NA | Human lung ca tissue samples | Decreased EcSOD in tumor vs. normal | Svensk 2004 [35] | |
| Melanoma | No change | B16-F1 | In vitro—adenoviral overexpression; In vivo—tumor xenografts | Decreased tumor size with EcSOD overexpression. | Wheeler 2003 [59] |
| Thyroid | NA | PC C13, RET/PTC1, PC E1A, COS-7 | Transformed rat thyroid cell lines, Human thyroid DNA array | NA | Laukkanen 2010 [41] |
| Thyroid | Stromal SOD3 increased cancer cell growth | Mesenchymal stem/stromal cells isolated from human papillary thyroid cancer | qPCR expression of SOD3 measured in normal thyroid stromal cells and papillary thyroid cancer stromal cells | Increased SOD3 expression in cancer mesenchymal stem/stromal cells vs. normal MSCs | Parascandolo 2017 [42] |
| Ovarian | NA | SKOV-3, MDAH-2774 | In vitro—DCA administration, shifting cell metabolism from anaerobic to aerobic | Increased apoptosis and increased EcSOD | Saed 2010 [60] |
| Ovarian | NA | SKOV-3 MDAH-2774 | In vitro—DCI administration, inhibiting NADPH oxidase production of ROS | Increased apoptosis and decreased EcSOD | Jiang 2011 [61] |
| Renal | Increased apoptosis and proliferation with higher EcSOD expression | Human RCC samples | NA | NA | Soini 2006 [43] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Leary, B.R.; Carroll, R.S.; Steers, G.J.; Hrabe, J.; Domann, F.E.; Cullen, J.J. Impact of EcSOD Perturbations in Cancer Progression. Antioxidants 2021, 10, 1219. https://0-doi-org.brum.beds.ac.uk/10.3390/antiox10081219
O’Leary BR, Carroll RS, Steers GJ, Hrabe J, Domann FE, Cullen JJ. Impact of EcSOD Perturbations in Cancer Progression. Antioxidants. 2021; 10(8):1219. https://0-doi-org.brum.beds.ac.uk/10.3390/antiox10081219
Chicago/Turabian StyleO’Leary, Brianne R., Rory S. Carroll, Garett J. Steers, Jennifer Hrabe, Frederick E. Domann, and Joseph J. Cullen. 2021. "Impact of EcSOD Perturbations in Cancer Progression" Antioxidants 10, no. 8: 1219. https://0-doi-org.brum.beds.ac.uk/10.3390/antiox10081219