Depression and Complicated Grief, and Associated Factors, of Bereaved Family Members of Patients Who Died of Malignant Pleural Mesothelioma in Japan
Abstract
:1. Introduction
2. Methods
2.1. Study Design, Participants, and Setting
2.2. Outcomes
2.3. Instruments
2.3.1. Information of the Patients and Bereaved Family Members
2.3.2. Depression
2.3.3. Complicated Grief (CG)
2.3.4. Achievement of Good Death (GDI)
2.3.5. Quality of End-of-Life Care (CES)
2.3.6. Missing Data
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Characteristics of Malignant Pleural Mesothelioma Patients and Bereaved Family Members
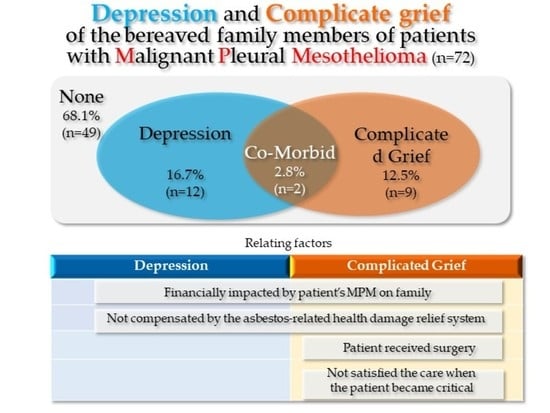
3.2. Depression and Complicated Grief and among Bereaved Family Members
3.3. Correlation between the Total Scores of the PHQ-9, BGQ, GDI, and CES
3.4. Factors Associated with Depression
3.5. Factors Associated with BGQ Total Score
4. Discussion
4.1. Implications of Care
4.2. Implications for Further Research
4.3. Representativeness of the General Population of Bereaved Family Members of MPM Patients
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shear, M.K. Complicated grief. N. Engl. J. Med. 2015, 372, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, D.; Miyashita, M.; Nakajima, S.; Ito, M.; Kato, M.; Kim, Y. Prevalence and determinants of complicated grief in general population. J. Affect. Disord. 2010, 127, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, M.; Sakaguchi, Y.; Morita, T.; Ogawa, A.; Fujisawa, D.; Kizawa, Y.; Miyashita, M. Factors associated with possible complicated grief and major depressive disorders. Psycho-Oncology 2018, 27, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Carver, C.S.; Spiegel, D.; Mitchell, H.R.; Cannady, R.S. Role of family caregivers’ self-perceived preparedness for the death of the cancer patient in long-term adjustment to bereavement. Psycho-Oncology 2017, 26, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, M.; Sakaguchi, Y.; Igarashi, N.; Morita, T.; Shima, Y.; Miyashita, M. Effects of financial status on major depressive disorder and complicated grief among bereaved family members of patients with cancer. Psycho-Oncology 2021, 30, 844–852. [Google Scholar] [CrossRef]
- Nakajima, S.; Masaya, I.; Akemi, S.; Takako, K. Complicated grief in those bereaved by violent death: The effects of post-traumatic stress disorder on complicated grief. Dialogues Clin. Neurosci. 2012, 14, 210. [Google Scholar] [CrossRef]
- Shear, K.M.; Jackson, C.T.; Essock, S.M.; Donahue, S.A.; Felton, C.J. Screening for complicated grief among Project Liberty service recipients 18 months after 11 September 2001. Psychiatr. Serv. 2006, 57, 1291–1297. [Google Scholar] [CrossRef]
- Burke, L.A.; Neimeyer, R.A.; McDevitt-Murphy, M.E. African American homicide bereavement: Aspects of social support that predict complicated grief, PTSD, and depression. OMEGA-J. Death Dying 2010, 611, 24. [Google Scholar] [CrossRef]
- Wen, F.H.; Prigerson, H.G.; Chou, W.C.; Chen, J.S.; Chang, W.C.; Hsu, M.H.; Tang, S.T. Prolonged grief disorder and depression are distinguishable syndromes: A latent transition analysis for bereaved family caregivers of cancer patients. Psycho-Oncology 2022, 1–8. [Google Scholar] [CrossRef]
- van Zandwijk, N.; Clarke, C.; Henderson, D.; Musk, A.W.; Fong, K.; Nowak, A.; Loneragan, R.; McCaughan, B.; Boyer, M.; Feigen, M.; et al. Guidelines for the diagnosis and treatment of malignant pleural mesothelioma. J. Thorac. Dis. 2013, 5, E254. [Google Scholar] [CrossRef]
- Furuya, S.; Takahashi, K. Experience of Japan in achieving a total ban on asbestos. Int. J. Environ. Res. Public Health 2017, 14, 1261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zha, L.; Kitamura, Y.; Kitamura, T.; Liu, R.; Shima, M.; Kurumatani, N.; Sobue, T. Population-based cohort study on health effects of asbestos exposure in Japan. Cancer Sci. 2019, 110, 1076–1084. [Google Scholar] [CrossRef] [Green Version]
- Sawanyawisuth, K.; Furuya, S.; Park, E.K.; Myong, J.P.; Ramos-Bonilla, J.P.; Ochir, O.C.; Takahashi, K. Compensation for asbestos-related diseases in Japan: Utilization of standard classifications of industry and occupations. Asian Pac. J. Cancer Prev. 2017, 18, 1779. [Google Scholar] [CrossRef] [PubMed]
- Japan Ministry of Health Law. Yearly Changes (from 1995 to 2020) in Number of Deaths from Mesothelioma by Prefecture (20 Major Cities Re-listed) (based on Vital Statistics (Final Data)). 2021. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/tokusyu/chuuhisyu20/dl/chuuhisyu.pdf (accessed on 10 May 2022).
- Chouaid, C.; Assié, J.B.; Andujar, P.; Blein, C.; Tournier, C.; Vainchtock, A.; Pairon, J.C. Determinants of malignant pleural mesothelioma survival and burden of disease in France: A national cohort analysis. Cancer Med. 2018, 7, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Gemba, K.; Fujimoto, N.; Aoe, K.; Kato, K.; Takeshima, Y.; Inai, K.; Kishimoto, T. Treatment and survival analyses of malignant mesothelioma in Japan. Acta Oncol. 2013, 52, 803–808. [Google Scholar] [CrossRef] [Green Version]
- Kang, M.S.; Lee, S.S.; Kwon, S.C.; Huh, D.A.; Lee, Y.J. Survival of Korean Patients with Malignant Pleural Mesothelioma Compensated for the Asbestos Injury Relief. Appl. Sci. 2021, 11, 9713. [Google Scholar] [CrossRef]
- Amin, W.; Linkov, F.; Landsittel, D.P.; Silverstein, J.C.; Bshara, W.; Gaudioso, C.; Becich, M.J. Factors influencing malignant mesothelioma survival: A retrospective review of the National Mesothelioma Virtual Bank cohort. F1000Research 2018, 7, 1184. [Google Scholar] [CrossRef]
- Bibby, A.C.; Tsim, S.; Kanellakis, N.; Ball, H.; Talbot, D.C.; Blyth, K.G.; Maskell, N.A.; Psallidas, I. Malignant pleural mesothelioma: An update on investigation, diagnosis and treatment. Eur. Respir. Rev. 2016, 25, 472–486. [Google Scholar] [CrossRef] [Green Version]
- Mercadante, S.; Degiovanni, D.; Casuccio, A. Symptom burden in mesothelioma patients admitted to home palliative care. Curr. Med. Res. Opin. 2016, 32, 1985–1988. [Google Scholar] [CrossRef]
- Breen, L.J.; Huseini, T.; Same, A.; Peddle-McIntyre, C.J.; Lee, Y.G. Living with Mesothelioma: A Systematic Review of Patient and Caregiver Psychosocial Support Needs. Patient Educ. Couns. 2022, 105, 1904–1916. [Google Scholar] [CrossRef]
- Guglielmucci, F.; Franzoi, I.G.; Bonafede, M.; Borgogno, F.V.; Grosso, F.; Granieri, A. The less I think about it, the better I feel”: A thematic analysis of the subjective experience of malignant mesothelioma patients and their caregivers. Front. Psychol. 2018, 9, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonafede, M.; Granieri, A.; Binazzi, A.; Mensi, C.; Grosso, F.; Santoro, G.; Guglielmucci, F. Psychological distress after a diagnosis of malignant mesothelioma in a group of patients and Caregivers at the National Priority Contaminated Site of Casale Monferrato. Int. J. Environ. Res. Public Health 2020, 17, 4353. [Google Scholar] [CrossRef] [PubMed]
- Girgis, S.; Smith, A.B.; Lambert, S.; Waller, A.; Girgis, A. “It sort of hit me like a baseball bat between the eyes”: A qualitative study of the psychosocial experiences of mesothelioma patients and carers. Supportive Care Cancer 2019, 27, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Nagamatsu, Y.; Horiuchi, S.; Natori, Y. The stages and difficulties of patients with malignant pleural mesothelioma. J. Hum. Care Stud. 2012, 12, 69–81. [Google Scholar]
- Nagamatsu, Y.; Oze, I.; Aoe, K.; Hotta, K.; Kato, K.; Nakagawa, J.; Hara, K.; Kishimoto, T.; Fujimoto, N. Quality of life of survivors of malignant pleural mesothelioma in Japan: A cross sectional study. BMC Cancer 2018, 18, 350. [Google Scholar] [CrossRef] [Green Version]
- Shear, M.K.; Simon, N.; Wall, M.; Zisook, S.; Neimeyer, R.; Duan, N.; Reynolds, C.; Lebowitz, B.; Sung, S.; Ghesquiere, A.; et al. Complicated grief and related bereavement issues for DSM-5. Depress. Anxiety 2011, 28, 103–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagamatsu, Y.; Sakyo, Y.; Barroga, E.; Koni, R.; Natori, Y.; Miyashita, M. Bereaved Family Members’ Perspectives of Good Death and Quality of End-of-Life Care for Malignant Pleural Mesothelioma Patients: A Cross-Sectional Study. J. Clin. Med. 2022, 11, 541. [Google Scholar] [CrossRef]
- Thekkumpurath, P.; Walker, J.; Butcher, I.; Hodges, L.; Kleiboer, A.; O’Connor, M.; Wall, L.; Murray, G.; Kroenke, K.; Sharpe, M. Screening for major depression in cancer outpatients. The diagnostic accuracy of the 9-item Patient Health Questionnaire. Cancer 2011, 117, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Wittkampf, K.A.; Naeije, L.; Schene, A.H.; Huyser, J.; Van Weert, H.C. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: A systematic review. Gen. Hosp. Psychiatry 2007, 29, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Muramatsu, K.; Kamijima, K.; Yoshida, M.; Otsubo, T.; Miyaoka, H.; Muramatsu, Y.; Gejyo, F. The patient health questionnaire, Japanese version: Validity according to the mini-international neuropsychiatric interview–plus. Psychol. Rep. 2007, 101, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Nakajima, S.; Fujisawa, D.; Miyashita, M.; Kim, Y.; Shear, M.K.; Ghesquiere, A.; Wall, M.M. Brief measure for screening complicated grief: Reliability and discriminant validity. PLoS ONE 2012, 7, e31209. [Google Scholar] [CrossRef] [PubMed]
- Miyashita, M.; Morita, T.; Sato, K.; Hirai, K.; Shima, Y.; Uchitomi, Y. Good death inventory: A measure for evaluating good death from the bereaved family member’s perspective. J. Pain Symptom Manag. 2008, 35, 486–498. [Google Scholar] [CrossRef] [PubMed]
- Miyashita, M.; Aoyama, M.; Nakahata, M.; Yamada, Y.; Abe, M.; Yanagihara, K.; Morita, T. Development the Care Evaluation Scale Version 2.0: A modified version of a measure for bereaved family members to evaluate the structure and process of palliative care for cancer patient. BMC Palliat Care. 2017, 16, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiratsuka, R.; Aoyama, M.; Masukawa, K.; Shimizu, Y.; Hamano, J.; Sakaguchi, Y.; Miyashita, M. The association of family functioning with possible major depressive disorders and complicated grief among bereaved family members of patients with cancer: Results from the J-HOPE4 study, a nationwide cross-sectional follow-up survey in Japan: Family function association with depression. J. Pain Symptom Manag. 2021, 62, 1154–1164. [Google Scholar] [CrossRef]
- Mizuno, Y.; Kishimoto, J.; Asukai, N. A nationwide random sampling survey of potential complicated grief in Japan. Death Stud. 2012, 36, 447–461. [Google Scholar] [CrossRef]
- Shinada, K.; Kohno, T.; Fukuda, K.; Higashitani, M.; Kawamatsu, N.; Kitai, T.; Mizuno, A. Depression and complicated grief in bereaved caregivers in cardiovascular diseases: Prevalence and determinants. BMJ Supportive Palliat. Care 2021. [Google Scholar] [CrossRef]
- Ueda, T.; Fujita, G.; Yanagita, T.; Kaise, C.; Sato, M. Risk factors for mental health problems and complicated grief in bereaved families of motor vehicle accident victims. Jpn. J. Psychol. 2017, 87, 569–578. [Google Scholar] [CrossRef] [Green Version]
- Aoyama, M. Grief, Depression, Insomnia and Alcohol Consumption Among Bereaved Family Members of Cancer Patients. In The Japan Hospis and Palliative Care Evaluation Study 3; Miyashita, M., Tsuneto, S., Shima, Y., Eds.; Hospice Foundation: Osaka, Japan, 2016; pp. 29–37. [Google Scholar]
- Kramer, B.J.; Kavanaugh, M.; Trentham-Dietz, A.; Walsh, M.; Yonker, J.A. Complicated grief symptoms in caregivers of persons with lung cancer: The role of family conflict, intrapsychic strains, and hospice utilization. OMEGA-J. Death Dying 2011, 62, 201–220. [Google Scholar] [CrossRef] [Green Version]
- Komischke-Konnerup, K.B.; Zachariae, R.; Johannsen, M.; Nielsen, L.D.; O’Connor, M. Co-occurrence of prolonged grief symptoms and symptoms of depression, anxiety, and posttraumatic stress in bereaved adults: A systematic review and meta-analysis. J. Affect. Disord. Rep. 2021, 4, 100140. [Google Scholar] [CrossRef]
- Wright, A.A.; Keating, N.L.; Balboni, T.A.; Matulonis, U.A.; Block, S.D.; Prigerson, H.G. Place of death: Correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J. Clin. Oncol. 2010, 28, 4457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ball, H.; Moore, S.; Leary, A. A systematic literature review comparing the psychological care needs of patients with mesothelioma and advanced lung cancer. Eur. J. Oncol. Nurs. 2016, 25, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Ott, C.H. The impact of complicated grief on mental and physical health at various points in the bereavement process. Death Stud. 2003, 27, 249–272. [Google Scholar] [CrossRef]
- Sugarbaker, D.J.; Jaklitsch, M.T.; Bueno, R. Prevention, early detection, and management of complications after 328 consecutive extrapleural pneumonectomies. J. Thorac. Cardiovasc. Surg. 2004, 128, 138–146. [Google Scholar] [CrossRef] [Green Version]
- Ploenes, T.; Osei-Agyemang, T.; Krohn, A. Changes in lung function after surgery for mesothelioma. Asian Cardiovasc. Thorac. Ann. 2013, 21, 48–55. [Google Scholar] [CrossRef]
- Papaspyros, S.; Papaspyros, S. Surgical management of malignant pleural mesothelioma: Impact of surgery on survival and quality of life—relation to chemotherapy, radiotherapy, and alternative therapies. IRSN Surg. 2014, 817203. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi, S.; Cardillo, G.; Zirafa, C.C.; Carleo, F.; Facciolo, F.; Fontanini, G.; Melfi, F. Surgery for malignant pleural mesothelioma: An international guidelines review. J. Thorac. Dis. 2018, 10 (Suppl. 2), S285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, Y.W.; Huang, C.T.; Yin, S.M.; Huang, Y.C.; Chien, C.H.; Chuang, H.Y. Determinants of complicated grief in caregivers who cared for terminal cancer patients. Supportive Care Cancer 2010, 18, 1321–1327. [Google Scholar] [CrossRef]
- Hensley, P.L. Treatment of bereavement-related depression and traumatic grief. J. Affect. Disord. 2006, 92, 117–124. [Google Scholar] [CrossRef]
- Stroebe, M.; Schut, H.; Stroebe, W. 2007 Health outcomes of bereavement. Lancet 2007, 370, 1960–1973. [Google Scholar] [CrossRef]
- Shear, K.; Frank, E.; Houck, P.R.; Reynolds, C.F., III. Treatment of complicated grief: A randomizedcontrolled trial. JAMA 2005, 293, 2601–2608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zisook, S.; Shuchter, S.R. Treatment of the depressions of bereavement. Am. Behav. Sci. 2001, 44, 782–797. [Google Scholar] [CrossRef]
- Wetherell, J.L. Complicated grief therapy as a new treatment approach. Dialogues Clin. Neurosci. 2022, 14, 159–166. [Google Scholar] [CrossRef]
- Vanderwerker, L.C.; Prigerson, H.G. Social support and technological connectedness as protective factors in bereavement. J. Loss Trauma 2004, 9, 45–57. [Google Scholar] [CrossRef]
- Melhem, N.M.; Moritz, G.; Walker, M.; Shear, M.K.; Brent, D. Phenomenology and correlates of complicated grief in children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 493–499. [Google Scholar] [CrossRef]
- Schulz, R.; Boerner, K.; Klinger, J.; Rosen, J. Preparedness for death and adjustment to bereavement among caregivers of recently placed nursing home residents. J. Palliat. Med. 2015, 18, 127–133. [Google Scholar] [CrossRef] [Green Version]

| Patients | n | % | ||
|---|---|---|---|---|
| Sex | Men | 59 | 81.9 | |
| Women | 13 | 18.1 | ||
| Source of asbestos exposure | Occupation | 49 | 68.1 | |
| Neighboring factory | 17 | 23.6 | ||
| School | 1 | 1.4 | ||
| Family | 1 | 1.4 | ||
| Unknown | 4 | 5.4 | ||
| Treatment | Surgery | 14 | 19.4 | |
| (includes multiple treatments) | Extrapleural pneumonectomy | 12 | 16.7 | |
| Pleurectomy decoration | 2 | 2.8 | ||
| Chemotherapy | 51 | 70.8 | ||
| Radiotherapy | 15 | 20.8 | ||
| Palliative care | 41 | 56.9 | ||
| Compensation | Worker’s accident compensation insurance | 47 | 65.3 | |
| (some had both types) | Asbestos-related health-damage relief system | 56 | 77.8 | |
| Place of death | Respiratory ward | 35 | 48.6 | |
| Palliative care unit/hospice | 24 | 33.3 | ||
| Home | 10 | 13.9 | ||
| Other | 3 | 4.2 | ||
| Age at diagnosis (years) | Range: | 36–92 | Mean ± SD | 66.9 ± 9.6 |
| Survival (months) | 0.5–69 | 14.5 ± 14.1 | ||
| Bereaved family members | n | % | ||
| Sex | Men | 15 | 20.8 | |
| Women | 57 | 79.2 | ||
| Relationship with patient | Spouse | 52 | 72.2 | |
| Child | 20 | 17.8 | ||
| Experience of end-of-life discussion with patient | Yes | 27 | 37.5 | |
| No | 44 | 61.1 | ||
| Timing of patient’s death | Much sooner than expected | 31 | 43.1 | |
| Sooner than expected | 25 | 34.7 | ||
| Moderate | 9 | 12.5 | ||
| Later than expected | 5 | 6.9 | ||
| Much later than expected | 2 | 2.8 | ||
| Satisfaction with care: | Satisfied | 29 | 40.3 | |
| On diagnosis | Not satisfied | 43 | 59.7 | |
| When patient became critical | Satisfied | 31 | 38.9 | |
| Not satisfied | 41 | 61.1 | ||
| When patient died | Satisfied | 47 | 65.3 | |
| Not satisfied | 25 | 34.7 | ||
| Financial impact of patient’s | Significant impact | 12 | 16.7 | |
| MPM on family | Some impact | 15 | 20.8 | |
| Moderate impact | 20 | 27.8 | ||
| Minor impact | 15 | 20.8 | ||
| No impact | 10 | 13.9 | ||
| Level of anger toward asbestos | Very angry | 56 | 77.8 | |
| Angry | 11 | 15.3 | ||
| Moderately angry | 4 | 5.6 | ||
| Slightly angry | 1 | 1.4 | ||
| Not angry at all | 0 | 0 | ||
| Age (in years) | Range: | 32–82 | Mean ± SD | 62.5 ± 12.2 |
| Time since bereavement (months) | 9–110 | 45.2 ± 27.2 | ||
| Variable | Estimated Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Family financially impacted by patient’s MPM | 2.569 | 1.316–5.015 | 0.006 |
| Not compensated by the asbestos-related health-damage relief system | 7.334 | 1.401–38.374 | 0.018 |
| Variable | Estimated Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Family financially impacted by patient’s MPM | 3.278 | 1.250–8.596 | 0.016 |
| Not compensated by the asbestos-related health-damage relief system | 19.210 | 1.609–229.392 | 0.020 |
| Received surgery | 11.301 | 1.256–101.649 | 0.030 |
| Not satisfied with the care given when the patient became critical | 13.626 | 1.213–153.009 | 0.034 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagamatsu, Y.; Sakyo, Y.; Barroga, E.; Koni, R.; Natori, Y.; Miyashita, M. Depression and Complicated Grief, and Associated Factors, of Bereaved Family Members of Patients Who Died of Malignant Pleural Mesothelioma in Japan. J. Clin. Med. 2022, 11, 3380. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm11123380
Nagamatsu Y, Sakyo Y, Barroga E, Koni R, Natori Y, Miyashita M. Depression and Complicated Grief, and Associated Factors, of Bereaved Family Members of Patients Who Died of Malignant Pleural Mesothelioma in Japan. Journal of Clinical Medicine. 2022; 11(12):3380. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm11123380
Chicago/Turabian StyleNagamatsu, Yasuko, Yumi Sakyo, Edward Barroga, Riwa Koni, Yuji Natori, and Mitsunori Miyashita. 2022. "Depression and Complicated Grief, and Associated Factors, of Bereaved Family Members of Patients Who Died of Malignant Pleural Mesothelioma in Japan" Journal of Clinical Medicine 11, no. 12: 3380. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm11123380