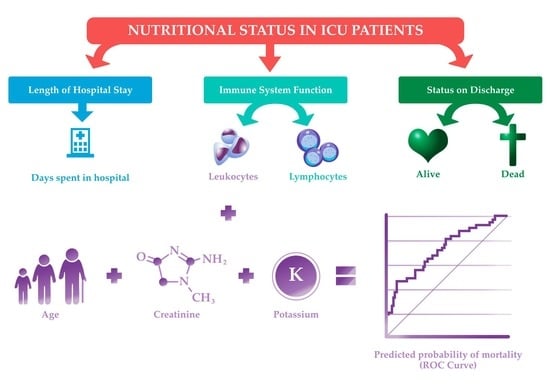
Nutritional State, Immunological and Biochemical Parameters, and Mortality in the ICU: An Analytical Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Population, and Sample
2.2. Elegibity Criteria
2.3. Variables and Measurement
2.4. Ethical Aspects
2.5. Statistical Analysis
3. Results
3.1. Descriptive Profile of ICU Patients
3.2. Factors Associated with Hospital Stay
3.3. Factors Associated with Immunological Function
3.4. Factors Associated with Vital Situation
3.5. Multivariate Analysis of ICU Mortality
4. Discussion
4.1. Prevalence of Diseases upon Admission and Mortality in the ICU
4.2. Diseases upon Admission and Lymphocytosis during ICU Stay
4.3. Nutritional State, Hospital Stay, and Immunological Function
4.4. Nutritional State and Leukocyte Count in Mortality
4.5. Multivariate Analysis of ICU Mortality
4.6. Study Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burgos, R. Disease-related malnutrition. Nutr. Hosp. Supl. 2013, 6, 10–23. [Google Scholar]
- Pérez, D.; Molina, R.; Gutiérrez, A.; Larrahondo, H. Evaluation of the Nutritional state of the critical patients in the intensive care ward of the hospital “Hermanos Ameijeiras”. Rev. Cuba. De Med. Intensiv. Y Emerg. 2014, 13, 374–387. [Google Scholar]
- Acosta, J.; Gómez, U.; Ruiz, S. Nutritional Assessment of the severely ill patient. Nutr. Hosp. 2005, 20 (Suppl. S2), 5–8. [Google Scholar]
- Rajendram, R.; Khan, M.F. The use of Nutritional screening tools in the intensive therapy unit. Anesth. Pain Intensive Care 2019, 23, 231–236. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, F.; Schuetz, P.; Bounoure, L.; Austin, P.; Ballesteros-Pomar, M.; Cederholm, T.; Fletcher, J.; Laviano, A.; Norman, K.; Poulia, K.-A.; et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin. Nutr. 2018, 37, 336–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [Green Version]
- Álvarez-Hernández, J.; Planas Vila, M.; León-Sanz, M.; García de Lorenzo, A.; Celaya-Pérez, S.; García-Lorda, P.; Araujo, K.; Sarto Guerri, B.; PREDyCES Researchers. Prevalence and costs of malnutrition in hospitalized patients; the PREDyCES Study. Nutr. Hosp. 2012, 27, 1049–1059. [Google Scholar] [CrossRef] [Green Version]
- Hudson, L.; Chittams, J.; Griffith, C.; Compher, C. Malnutrition identified by academy of nutrition and dietetics/American society for parenteral and enteral nutrition is associated with more 30-day readmissions, greater hospital mortality, and longer hospital stays: A retrospective analysis of nutrition assessment data in a major medical center. JPEN J. Parenter. Enter. Nutr. 2018, 42, 892e7. [Google Scholar] [CrossRef]
- Vallejo, K.P.; Martínez, C.M.; Adames, A.A.M.; Fuchs-Tarlovsky, V.; Nogales, G.C.C.; Paz, R.E.R.; Perman, M.I.; Correia, M.I.T.D.; Waitzberg, D.L. Current clinical nutrition practices in critically ill patients in Latin America: A multinational observational study. Crit. Care 2017, 21, 227. [Google Scholar] [CrossRef] [Green Version]
- Illera, D.; Rivera, G.; Orozco, A.; Montenegro, V.; Orlando, C. Perfil epidemiológico y factores de riesgo en pacientes de la Unidad de Cuidados Intensivos, Hospital San José, Popayán. Rev. Fac. Cienc. de la Salud 2015, 17, 14–19. [Google Scholar]
- Sánchez-Hurtado, L.A.; Tejeda-Huezo, B.C.; Gómez-Flores, S.S.; Esquivel-Chávez, A.; Cano-Oviedo, A.A.; Baltazar-Torres, J. Elderly patients in a Mexican intensive care unit: A retrospective análisis. Med. Intensiva. 2018, 42, 258–260. [Google Scholar] [CrossRef] [PubMed]
- Savastano, L.; Cremaschi, F.; Benito, O. Análisis de la mortalidad en la Unidad de Cuidados Intensivos del Hospital Central de Mendoza, Argentina. Rev. Médica Univ. 2009, 5, 73–75. [Google Scholar]
- Gutiérrez, N.; Rienzo, A.; Holguin, H.; Cardozo, J.; Arias, J.; Beltrán, D.; Pérez, A. Estado nutricional de pacientes en dos centros hospitalarios de Villavicencio, Colombia 2015. Rev. Investig. Andin. 2016, 18, 1709–1728. [Google Scholar] [CrossRef] [Green Version]
- Domínguez-Berrueta, M.; Martín, A.; Pérez, M. Analysis of the nutritional parameters and adjustment of the requirements of the initial parenteral nutrition in post-surgical critically ill patients. Nutr. Hosp. 2014, 29, 402–410. [Google Scholar] [CrossRef]
- Valero, M.; Díez, L.; El Kadaoui, N.; Jiménez, A.; Rodríguez, H.; León, M. Are the tools recommended by ASPEN and ESPEN comparable for assessing the nutritional status? Nutr. Hosp. 2005, 20, 259–267. [Google Scholar]
- Loser, C. Malnutrition in Hospital: The clinical and economic implication. Dtsch. Arztbel. Int. 2010, 107, 911–917. [Google Scholar] [CrossRef]
- Montoya, S.; Múnera, N. Effect to early Nutritional intervention in the aoutcome of patients at risk clinical nutrition. Nutr. Hosp. 2014, 29, 427–436. [Google Scholar] [CrossRef]
- Colombia. Ministerio de Salud y Protección Social. Resolución Número 3280 del 2018, Política Integral de Atención en Salud. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-3280-de-2018.pdf (accessed on 17 April 2022).
- Nachvak, S.; Hedayati, S.; Hejazi, N.; Motamedi-Motlagh, A.; Abdollahzad, H. Nutritional care and balance of energy in patients hospitalized in Iranian intensive care units. Nutr. Clin. Métab. 2018, 32, 122–128. [Google Scholar] [CrossRef]
- Rosenthal, V.D.; Duszynska, W.; Ider, B.-E.; Gurskis, V.; Al-Ruzzieh, M.A.; Myatra, S.N.; Gupta, D.; Belkebir, S.; Upadhyay, N.; Zand, F.; et al. International nosocomial infection control consortium (INICC) report, data summary of 45 countries for 2013–2018, adult and pediatric units, device-associated module. Am. J. Infect. Control. 2021, 49, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Tejedor, A.; Cabre-Pericas Ll Martin-Delgado, M.; Leal-Micharet, A.; Algora-Weber, A. Evolution and prognosis of long intensive care unit stay patients suffering a deterioration: A multicenter study. J. Crit. Care 2015, 30, 654.e1–654.e7. [Google Scholar] [CrossRef]
- Shi, Y.; Yang, C.; Chen, L.; Cheng, M.; Xie, W. Predictive value of neutrophil-to-lymphocyte and platelet ratio in in-hospital mortality in septic patients. Heliyon 2022, 8, e11498. [Google Scholar] [CrossRef]
- Gameiro, J.; Fonseca, J.A.; Dias, J.M.; Milho, J.; Rosa, R.; Jorge, S.; Lopes, J.A. Neutrophil, lymphocyte and platelet ratio as a predictor of postoperative acute kidney injury in major abdominal surgery. BMC Nephrol. 2018, 19, 320. [Google Scholar] [CrossRef]
- Chang-Hoon, K.; Dhong, J.; Yoon, P.; Jungil, B.; Youn, C.; Won, K.; Jae-Hyon, B. Neutrophil, Lymphocyte, and Platelet Counts and Acute Kidney Injury After Cardiovascular Surgery. J. Cardiothorac. Vasc. Anesth. 2018, 32, 212–222. [Google Scholar] [CrossRef]
- Yun, C.; Jiyoung, L.; Ji, P.; Do-Gyun, H.; Eunji, H.; In Kyong, Y. Late Mortality Prediction of Neutrophil-to- Lymphocyte and Platelet Ratio in Patients with Trauma Who Underwent Emergency Surgery: A Retrospective Study. J. Surg. Res. 2021, 267, 755–761 ISSN 0022. [Google Scholar] [CrossRef]
- Lew Ch Yung, G.; Cheung, K.; Chua, A.; Chong, M.; Miller, M. Association between malnutrition and 28-day mortality and intensive care length-of-stay in the critically ill: A prospective cohort study. Nutrients 2017, 10, 10. [Google Scholar] [CrossRef] [Green Version]
- Gong, M.; Bajwa, E.; Thompson, B.; Christiani, D. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax 2010, 65, 44–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonseca-González, G.; Suárez-Cuenca, J.; Flores Alcántar, M.; Garro-Almendro, A. Distribución del índice neutrófilo/linfocito en diferentes fenotipos metabólicos de obesidad. Rev. Mex. Endocrinol. Metabol. Nutr. 2018, 5, 13–20. [Google Scholar]
- Herishanu, Y.; Rogowski, O.; Polliack, A.; Marilus, R. Leukocytosis in obese individuals: Possible link in patients with unexplained persistent neutrophilia. Eur. J. Haematol. 2006, 76, 516–520. [Google Scholar] [CrossRef]
- Wierdsma, N.J.; Kruizenga, H.M.; Konings, L.A.; Krebbers, D.; Jorissen, J.R.; Joosten, M.-H.I.; van Aken, L.H.; Tan, F.M.; van Bodegraven, A.A.; Soeters, M.R.; et al. Poor Nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission. Clin. Nutr. ESPEN 2021, 43, 369–376. [Google Scholar] [CrossRef]
- Service, E.; Anwar, F. Nutritional management in critically ill trauma patients is challenging. Trauma 2016, 18, 231–236. [Google Scholar] [CrossRef]
- Mukhopadhyay, A.; Henry, J.; Ong, V.; Leong, C.; Teh, A.L.; van Dam, R.; Kowitlawakul, Y. Association of modified NUTRIC score with 28—Day mortality in critically ill patients. Clin. Nutr. 2017, 36, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Maryam, S.; Azizollah, P.; Joana, N.; Nicola, V.; Narges, R.; Afrooz, J.; Mahboobe, H. The importance of nutritional status on clinical outcomes among both ICU and Non-ICU patients with COVID-19. Clin. Nutr. ESPEN 2022, 49, 225–231. [Google Scholar] [CrossRef]
- O’Brien, J.; Gales, C.; Pescado, R.; Ancukiewicz, M.; Kramer, A. Excess body weight is not independently associated with out- come in mechanically ventilated patients with acute lung injury. Ann. Intern. Med. 2004, 140, 338–345. [Google Scholar] [CrossRef]
- Tremblay, A.; Bandi, V. Impact of body mass index on outcomes following critical care. Chest 2003, 123, 1202–1207. [Google Scholar] [CrossRef]
- Frat, J.-P.; Gissot, V.; Ragot, S.; Desachy, A.; Runge, I.; Lebert, C.; Robert, R.; the Association des Réanimateurs du Centre-Ouest (ARCO) study group. Impact of obesity in mechanically ventilated patients: A prospective study. Intensive Care Med. 2008, 34, 1991–1998. [Google Scholar] [CrossRef]
- Akinnusi, M.; Pineda, L.; El Solh, A. Effect of obesity on intensive care morbidity and mortality: A meta-analysis. Crit. Care Med. 2008, 36, 151–158. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Li, Z.; Yang, T.; Wang, M.; Xi, X. Is body mass index associated with outcomes of mechanically ventilated adult patients in intensive critical units? A systematic review and meta-analysis. PLoS ONE 2018, 13, e0198669. [Google Scholar] [CrossRef] [Green Version]
- Tocalini, P.; Vicente, A.; Amoza, R.; Reid, C.G.; Cura, A.; Tozzi, W.; Villarruel, M.; Esperón, F.; Alí, M.; Novo, M.; et al. Association between obesity and mortality in adult patients receiving invasive mechanical ventilation: A systematic review and meta—Analysis. Med. Intensiva. 2020, 44, 18–26. [Google Scholar] [CrossRef]
- Abete, I.; Lu, Y.; Lassale, C.; Verschuren, M.; Van der Schouw, Y.; Bueno-de-Mesquita, B. White cell counts in relation to mortality in a general population of cohort study in the Netherlands: A mediating effect or not? BMJ Open. 2019, 9, e030949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvear-Vega, S.; Canteros-Gatica, J. Performance evaluation of APACHE II and SAPS III in an intensive care unit. Rev. Salud Pública. 2018, 20, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, F.; Yılmaz, A.S.; Ersoy, I.; Demir, M.; Orhan, H. Predictive outcomes of APACHE II and expanded SAPS II mortality scoring systems in coronary care unit. Int. J. Cardiol. 2023, 371, 427–431. [Google Scholar] [CrossRef] [PubMed]

| Variables |
Total (±SD) (n)% |
Women (n = 66) (±SD) (n)% |
Men (n = 48) (±SD) (n)% | p |
|---|---|---|---|---|
| Age | 62.38 (±17.63) | 61.52 (±17.41) | 63.56 (±18.04) | 0.543 |
| Type of nutritional support | ||||
| Oral feeding | (78) 68.4% | (48) 72.7% | (30) 62.5% | 0.296 |
| Enteral nutritional support | (31) 27.2% | (17) 25.8% | (14) 29.2% | |
| Parenteral nutritional support | (4) 3.5% | (1) 1.5% | (3) 6.3% | |
| Mixed nutritional support | (1) 0.9% | (0) | (1) 2.1% | |
| Nutritional state | ||||
| Low weight | (20) 17.5% | (10) 15.2% | (10) 20.8% | 0.725 |
| Normal weight | (33) 29% | (20) 30.3% | (13) 27.1% | |
| Overweight/obesity | (61) 53.5% | (36) 54.5% | (25) 52.1% | |
| Immunological and biochemical functions | ||||
| Leukocytes (×103/uL) | 18.33 (±36.10) | 19.40 (±42.67) | 16.85 (±24.75) | 0.352 |
| Normal-range leukocytes | (46) 40.4% | (27) 40.9% | (19) 39.6% | 0.484 |
| Leukocytosis | (54) 47.4% | (29) 43.9% | 25) 52.1% | |
| Leukopenia | (14) 12.3% | (10) 15.2% | (4) 8.3% | |
| Lymphocytes (%) | 15.16 (±11.49) | 15.28 (±10.43) | 15.01 (±12.91) | 0.635 |
| Normal-range lymphocytes | (37) 32.5% | (24) 36.4% | (13) 27.1% | 0.434 |
| Lymphocytosis | (3) 2.6% | (1) 1.5% | (2) 4.2% | |
| Lymphopenia | (74) 64.9% | (41) 62.1% | (33) 68.8% | |
| Creatinine (mg/dL) | 1.61 (±2.70) | 1.60 (±2.95) | 1.63 (±2.35) | 0.948 |
| Potassium (mEq/L) | 4.10 (±0.71) | 4.08 (±0.77) | 4.13 (±0.63) | 0.685 |
| Disease upon admission | ||||
| Circulatory and respiratory diseases | (36) 31.6% | (20) 55.6% | (16) 44.4% | 0.381 |
| Neoplastic diseases | (34) 29.8% | (17) 50% | (17) 50% | |
| Other diseases | (28) 24.6% | (20) 71.4% | (8) 28.6% | |
| Infectious diseases | (16) 14% | (9) 56.3% | (7) 43.8% | |
| Vital situation | ||||
| Deceased | (43) 37.7% | (25) 58.1% | (18) 41.9% | 0.967 |
| Alive | (71) 62.3% | (41) 57.8% | (30) 42.3% | |
| Hospital stay (days) | 23.96 (±23.85) | 24.08 (±23.50) | 23.81 (±24.56) | 0.954 |
| Variables |
Hospital Stay (Days) (±SD) | p |
|---|---|---|
| Age | Rho 0.016 | 0.868 |
| Disease upon admission | ||
| Circulatory and respiratory diseases | 17.81 (±19.17) | 0.042 |
| Neoplastic diseases | 33.26 (±29.22) | |
| Other diseases | 22.96 (±22.89) | |
| Infectious diseases | 19.81 (±17.25) | |
| Nutritional state | ||
| Low weight | 20.80 (±21.74) | 0.601 |
| Normal weight | 27.24 (±22.66) | |
| Overweight/obesity | 23.23 (±25.25) | |
| Immunological function | ||
| leukocytes (×103/uL) | Rho −0.040 | 0.669 |
| Normal-range leukocytes | 18.89 (±18.29) | 0.168 |
| Leukocytosis | 27.83 (±26.63) | |
| Leukopenia | 25.71 (±27.14) | |
| lymphocytes (%) | Rho −0.063 | 0.502 |
| Normal-range lymphocytes | 17.41 (±17.72) | 0.040 |
| Lymphocytosis | 47.33 (±49.31) | |
| Lymphopenia | 26.30 (±24.68) | |
| Variables |
Normal-Range Leukocytes (±SD) (n)% |
Leukocytosis (±SD) (n)% |
Leukopenia (±SD) (n)% | p |
|---|---|---|---|---|
| Age | 66.33 (±15.46) | 58.44 (±19.18) | 64.57 (±15.77) | 0.073 |
| Life course classification | ||||
| Youth | (1) 11.1% | (8) 88.9% | (0) 0% | 0.121 |
| Adults | (15) 39.5% | (17) 44.7% | (6) 15.8% | |
| Elderly | (30) 44.8% | (29) 43.3% | (8) 11.9% | |
| Disease upon admission | ||||
| Circulatory and respiratory diseases | (21) 58.3% | (11) 30.6% | (4) 11.1% | 0.216 |
| Neoplastic diseases | (11) 32.4% | (19) 55.9% | (4) 11.8% | |
| Other diseases | (10) 35.7% | (15) 53.6% | (3) 10.7% | |
| Infectious diseases | (4)25% | (9) 56.3% | (3) 18.8% | |
| Nutritional state | ||||
| Low weight | (6) 30% | (7) 35% | (7) 35% | 0.018 |
| Normal weight | (13) 39.4% | (17) 51.5% | (3) 9.1% | |
| Overweight/obesity | (27) 44.3% | (30) 49.2% | (4) 6.6% | |
| Variables |
Deceased (±SD) (n)% |
Alive (±SD) (n)% | p |
|---|---|---|---|
| Age | 66.26 (±17.08) | 60.03 (±17.66) | 0.067 |
| Life course | |||
| Youth | (2) 22.2% | (7) 77.8% | 0.571 |
| Adults | (14) 36.8% | (24) 63.2% | |
| Elderly | (27) 40.3% | (40) 59.7% | |
| Disease upon admission | |||
| Circulatory and respiratory diseases | (12) 33.3% | (24) 66.7% | 0.512 |
| Neoplastic diseases | (15) 44.1% | (19) 55.9% | |
| Other diseases | (12) 42.9% | (16) 57.1% | |
| Infectious diseases | (4) 25% | (12) 75% | |
| Nutritional state | |||
| Low weight | (11) 55% | (9) 45% | 0.157 |
| Normal weight | (13) 39.4% | (20) 60.6% | |
| Overweight/obesity | (19) 31.1% | (42) 68.9% | |
| Immunological function | |||
| Leukocytes (×103/uL) | 27.82 (±56.83) | 12.58 (±8.79) | 0.028 |
| Normal-range leukocytes | (12) 26.1% | (34) 73.9% | 0.066 |
| Leukocytosis | (23) 42.6% | (31) 57.4% | |
| Leukopenia | (8) 57.1% | (6) 42.9% | |
| Hospital stay (days) | 21.95 (±20.94) | 25.18 (±25.51) | 0.486 |
| Raw Estimation (Unadjusted) | Adjusted Estimation | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Alive (n = 71) | Deceased (n = 43) | OR | 95% CI | p | OR | 95% CI | p |
| Age (years) | 60.3 (17.66) | 66.26 (17.08) | 1.022 | 0.998–1.046 | 0.070 | 1.029 | 1.003–1.055 | 0.028 |
| Leukocytes | 12.58 (8.79) | 27.82 (56.83) | 1.017 | 0.997–1.038 | 0.099 | 1.024 | 1.000–1.048 | 0.048 |
| Creatinine | 1.82 (3.26) | 1.27 (1.34) | 0.911 | 0.760–1.093 | 0.317 | 0.747 | 0.566–0.985 | 0.039 |
| Potassium | 4.02 (0.66) | 4.24 (0.79) | 1.575 | 0.916–2.707 | 0.100 | 2.946 | 1.364–6.361 | 0.006 |
| Diagnostic accuracy of the associative model | ||||||||
| Cox and Snell R Square | 0.170 | |||||||
| Nagelkerke R Square | 0.231 | |||||||
| Hosmer–Lemeshow test | 0.065 | |||||||
| Sensitivity | 76.9% | |||||||
| Specificity | 73.9% | |||||||
| Validity index | 74.6% | |||||||
| +predictive value | 46.5% | |||||||
| −predictive value | 91.5% | |||||||
| Prevalence | 22.8% | |||||||
| Youden’s index | 72.3% | |||||||
| +likelihood ratio | 2.95 | |||||||
| −likelihood ratio | 0.30 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz Chavarro, B.C.; Romero-Saldaña, M.; Assis Reveiz, J.K.; Molina-Recio, G. Nutritional State, Immunological and Biochemical Parameters, and Mortality in the ICU: An Analytical Study. J. Clin. Med. 2023, 12, 4177. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12134177
Díaz Chavarro BC, Romero-Saldaña M, Assis Reveiz JK, Molina-Recio G. Nutritional State, Immunological and Biochemical Parameters, and Mortality in the ICU: An Analytical Study. Journal of Clinical Medicine. 2023; 12(13):4177. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12134177
Chicago/Turabian StyleDíaz Chavarro, Blanca Cecilia, Manuel Romero-Saldaña, Jorge Karim Assis Reveiz, and Guillermo Molina-Recio. 2023. "Nutritional State, Immunological and Biochemical Parameters, and Mortality in the ICU: An Analytical Study" Journal of Clinical Medicine 12, no. 13: 4177. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12134177